Introduction
The World Health Organization has declared the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreak a pandemic disease, given its spreading in more than 100 countries worldwide, infecting over 185,000 people and killing more than 7000. Now, the epicentre of the infection has moved from China to Europe. In Italy, the number of infected patients closely follows an exponential trend, with the risk of reaching the saturation of intensive care units soon.
Cardiovascular diseases (CVDs) and cardiovascular (CV) risk factors, such as hypertension, are the most common cause of death worldwide. It is not surprising that hypertension is very common among patients who died as a consequence (or co-cause) of SARS-CoV-2 disease (coronavirus disease 2019 (COVID-19)). Data from the China epidemic and the COVID-19 deaths show that most of those patients were old and commonly affected by CVD. A retrospective cohort study on clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China, found that non-survivors had a mean age of 69 years and hypertension was the most common comorbidity (48%), followed by diabetes mellitus (31%) and coronary heart disease (24%).1 In Italy, the Italian Health Institute (Istituto Superiore di Sanità-ISS) on 17 March 2020 reported 2003 patients who died with COVID-19. They had a mean age of 79.5 years and a mean of 2.7 comorbidities. Similarly to what was observed in Chinese population, the more prevalent comorbidities were arterial hypertension (76.1%), ischaemic heart disease (33.0%) and diabetes mellitus (35.5%) (www.iss.it). A high prevalence of hypertension is also present in patients who died after Middle East respiratory syndrome (MERS)-coronavirus (CoV) and influenza virus infections, indicating that this comorbidity is not specific for COVID-19 patients, but most likely represents a confounder related to the high prevalence of hypertension and CVD among older adults. It is not known if a specific link between these CV conditions and SARS-CoV-2 infection does exist.
On the other hand, after the confirmation of the key role played by angiotensin-converting enzyme 2 (ACE2) in SARS-CoV-2 cell entry,2 some authors have drawn attention to the possible risks associated with the administration of ACE inhibitors (ACE-Is) and angiotensin II type 1 receptor blockers (ARBs), also suggesting a change in anti-hypertensive therapies, given their capacity to increase ACE2 levels in some tissues such as the myocardium, with a consequent hypothetical greater susceptibility to SARS-CoV-2 infection and higher risk for severe disease.3,4 However, as some scientific societies promptly stated (European Society of Cardiology (ESC) Council on Hypertension5 and Heart Failure Society of America/American College of Cardiology/American Heart Association),6 it is crucial not to draw hasty conclusions from simple deductions not supported by experimental data, as in the published comments cited above.3,4 Here, we briefly discuss about the role of ACE2 in the CV system and in acute respiratory syndromes, in order to deepen understanding of this controversial situation.
Pathophysiology of renin–angiotensin–aldosterone system and ACE2 in CV homeostasis
The renin–angiotensin–aldosterone system (RAAS) plays a central role in the homeostatic control of the CV and renal systems and in regulating fluid volume and blood pressure. The RAAS blockade represents a cornerstone of the therapy of arterial hypertension and its related CV sequelae, such as ischaemic heart disease and heart failure (HF).
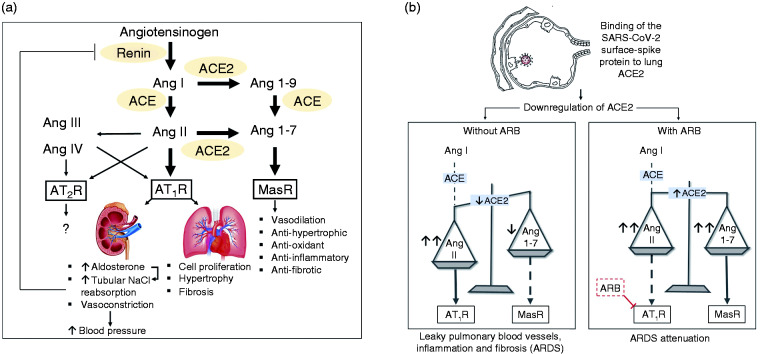
The RAAS consists of a cascade of both systemic and tissue enzymatic reactions, resulting in generation of angiotensin (Ang) II. In the first place, renin, a proteinase released by the kidneys, cleaves angiotensinogen to produce Ang I, both locally and in the circulation, which is then hydrolysed by the widespread endothelial angiotensin-converting enzyme (ACE), producing the octapeptide Ang II. This biologically active peptide binds Ang II type 1 and type 2 receptors (AT1R and AT2R). After binding the AT1R, Ang II stimulates aldosterone secretion and promotes salt and water reabsorption, vasoconstriction, inflammation and oxidative stress. This picture had been further enriched by the discovery of ACE2 in 2000.7 This is a type I transmembrane metallocarboxypeptidase, with homology to ACE, that cleaves Ang I into a nonapeptide (Ang 1-9), that binds AT2R, and Ang II into a heptapeptide (Ang 1-7), that binds an endogenous orphan Mas receptor (MasR), thus playing a central role in counterbalancing RAAS activation, resulting in CV protection. Ang 1-9 can also be rapidly changed into Ang 1-7 by the classical ACE activity. In conclusion, decreased ACE2 activity leads to activation of the Ang II-AT1R axis, contributing to progression of CV disease, while increased ACE2 activity leads to activation of ACE2-Ang 1-9-AT2R but mostly ACE2-Ang 1-7-MasR axes, contributing to protection against CV disease (Figure 1(a)). ACE2-Ang 1-7 pathway has also a key protective role against HF.
Figure 1.
(a) Schematic of the renin-angiotensin system counterbalanced by the angiotensin-converting enzyme 2 (ACE2)-angiotensin (Ang) 1-7-Mas axis. Note the role of angiotensin-converting enzyme (ACE) also in the conversion of Ang 1-9 to Ang 1-7. (b) Evidence-based hypothesis of the protective role of Ang II type 1 receptor blockers (ARBs) in pulmonary conditions potentially leading to acute respiratory distress syndrome (ARDS). ACE inhibitors (ACE-Is) are also likely to exert protective effects by reducing Ang II synthesis, but since ACE-Is also reduce the conversion of Ang 1-9 to Ang 1-7, they might hypothetically lessen the protective effects of a more intense Mas stimulation by higher concentrations of Ang 1-7.
AT1R: angiotensin II type 1 receptor; AT2R: angiotensin II type 2 receptor; MasR: Mas receptor; SARS-CoV-2: severe acute respiratory syndrome coronavirus 2.
Initially thought to be expressed only in limited organs (mainly heart and kidney), ACE2 was later found to be expressed in several other tissues, including lungs,8 exerting its key roles in maintaining homeostasis of the body, counterbalancing excessive RAAS activity.
Role of ACE2 in acute respiratory syndromes
While ACE is detectable in the entire capillary network of the alveoli in human lungs, ACE2 is produced mainly in Clara cells and type II alveolar epithelial cells,8 and epithelial injury is crucial for the development of acute respiratory distress syndrome (ARDS) in humans. Very consistent experimental data has been reproduced in different animal models which showed that an imbalance between classical RAAS and ACE2 activity is likely to promote and accelerate lung injury. The ACE-Ang II-AT1R axis induces pulmonary vasoconstriction and increase vascular permeability resulting in pulmonary ‘leaky’ vessels with secondary production of inflammatory cytokines, acceleration of apoptosis in alveolar epithelial cells and promotion of extracellular matrix synthesis with human lung fibrosis.9 On the contrary, Ang 1-7 was found to improve oxygenation, reduce inflammation and attenuate lung fibrosis in acute lung injury, a noteworthy factor in protecting against ARDS-related poor prognosis.10 Indeed, the use of an ARB or ACE-I, through reduction of Ang II-AT1R stimulation and the induced increase of ACE2, has been effective in decreasing lung injury in animal models of ARDS,11 and the use of human recombinant ACE2 could also be promising, although the interaction between RAAS and ARDS needs to be further elucidated. In 2003, ACE2 returned to the limelight following the discovery that it serves as a receptor for the binding of the SARS coronavirus. Now, it has just been confirmed that is also used as a receptor by the SARS-CoV-2 virus.2 However, it is not just the gateway for the virus. In fact, previous studies found that ACE2 can protect lungs from severe acute injury in mice, while the Ang II-AT1R axis promotes lung disease, leading to leaky pulmonary blood vessels, and impairs lung function.12 Furthermore, previous studies on SARS and MERS showed that the binding of the viral surface-spike protein to ACE2 leads to its downregulation, through its internalization and, perhaps, its shedding.12 The downregulation of ACE2 results in a hyper-effective Ang II-AT1R axis that increases pulmonary vascular damage and leakage, promoting the development of ARDS. Indeed, experimental SARS-CoV infections of wild-type mice in vivo lead to reduced ACE2 expression in the lungs, suggesting that reduced ACE2 expression might have a role in SARS-CoV-mediated severe acute lung pathologies. Importantly, after the AT1R blockade up-regulating ACE2, the acute severe lung injury in spike-Fc-treated mice was attenuated. Furthermore, AT1R blockade also led to attenuated pulmonary oedema. Therefore, SARS-CoV infections are likely to exaggerate acute lung failure through dysregulation of the RAAS and this process can be attenuated by the AT1R blockade12 (Figure 1(b)). However, whether SARS-CoV-2 also induces ACE2 downregulation is yet to be determined. Meanwhile, a controversy has arisen on the role of the ACE-I and ARB in SARS-CoV-2 entry and the consequent susceptibility and severity of COVID-19, due to their property of ACE2 overexpression. But no data have been published on this topic, whereas the evidence for the protective role of ARB at least is well-founded.
Conclusion
Hasty speculation on a negative relationship between COVID-19 and RAAS blockers could be dangerous3,4 and is not justified by our knowledge. To date, no data from randomised clinical trials or even large observational studies are available to support the discontinuation of ACE-I or ARB in COVID-19 patients and there is no evidence that these drugs can improve or worsen SARS-CoV-2 lung invasion and COVID-19 course. Therefore, hypertensive patients, especially if having CVD and high CV risk, should continue to take their drugs with high adherence to the prescribed therapies. At the same time, the administration of ACE-Is or ARBs aiming at preventing COVID-19 or lowering the disease severity is not supported by conclusive data. However, some authors have hypothesised a protective role of ARBs, especially losartan and telmisartan that strongly bind to the AT1R, against the spread and mortality from SARS-CoV-2 infection,13 given the mechanisms described above.
What is certain is that the use of an ACE-I/ARB in patients affected by hypertension, diabetes mellitus and the most prevalent CV diseases, such as ischaemic heart disease and HF, is associated with lower risk of death, even in the oldest patients hospitalised for acute medical conditions.14 Therefore, their discontinuation due to speculative observations could be harmful and lead to higher rates of CV deaths, especially in older COVID-19 patients, in which CV comorbidities are likely to strongly affect mortality. Several scientific societies have just made appropriate statements regarding the importance of taking ACE-I/ARB medication as per indications, in order not to put millions of patients affected by hypertension and related CVD at further risk5,6 Furthermore, at present, given the lack of data it is not recommended to discontinue these drugs because of the COVID-19. On the contrary, several experimental animal models suggest exactly the opposite, with ARBs found to limit lung damage in ARDS.11
At the same time, we feel there is urgency to provide solid evidence on the therapeutic and prognostic role of anti-hypertensive therapy in COVID-19 patients because both positive and negative effects would have important pragmatic implications, given the rapid spread of the infection globally.
Author contribution
RS, FG and FS contributed to the conception or design of the work. RS, FG, CDP, PG and FS contributed to the acquisition, analysis or interpretation of data for the work. RS, FG, CDP and FS drafted the manuscript. RS, FG and PG critically revised the manuscript. All gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship and/or publication of this article.
References
- 1. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020; 395: 1054–1062. [DOI] [PMC free article] [PubMed]
- 2. Yan R, Zhang Y, Li Y, et al. Structural basis for the recognition of the SARS-CoV-2 by full-length human ACE2. Science 2020; 367: 1444–1448. [DOI] [PMC free article] [PubMed]
- 3. Zheng YY, Ma YT, Zhang JY, et al. COVID-19 and the cardiovascular system. Nat Rev Cardiol. Epub ahead of print 5 March 2020. DOI: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed]
- 4. Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020; 8: e21. [DOI] [PMC free article] [PubMed]
- 5.De Simone G, Chair, ESC Council on Hypertension; On behalf of the Nucleus Members. Position Statement of the ESC Council on Hypertension on ACE-Inhibitors and Angiotensin Receptor Blockers. https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang (accessed 13 March 2020).
- 6.Bozkurt B, Kovacs R and Harrington B. HFSA/ACC/AHA Statement Addresses Concerns Re: Using RAAS Antagonists in COVID-19. https://www.acc.org/latest-in-cardiology/articles/2020/03/17/08/59/hfsa-acc-aha-statement-addresses-concerns-re-using-raas-antagonists-in-covid-19 (accessed 17 March 2020). [DOI] [PMC free article] [PubMed]
- 7. Donoghue M, Hsieh F, Baronas E, et al. A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1-9. Circ Res 2000; 87: E1–E9. [DOI] [PubMed] [Google Scholar]
- 8. Wiener RS, Cao YX, Hinds A, et al. Angiotensin converting enzyme 2 is primarily epithelial and is developmentally regulated in the mouse lung. J Cell Biochem 2007; 101: 1278–1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Uhal BD, Li X, Piasecki CC, et al. Angiotensin signalling in pulmonary fibrosis. Int J Biochem Cell Biol 2012; 44: 465–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zambelli V, Bellani G, Borsa R, et al. Angiotensin-(1-7) improves oxygenation, while reducing cellular infiltrate and fibrosis in experimental acute respiratory distress syndrome. Intensive Care Med Exp 2015; 3: 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shen L, Mo H, Cai L, et al. Losartan prevents sepsis-induced acute lung injury and decreases activation of nuclear factor kappa B and mitogen-activated protein kinases. Shock 2009; 31: 500–506. [DOI] [PubMed] [Google Scholar]
- 12. Imai Y, Kuba K, Rao S, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature 2005; 436: 112–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Phadke MA and Saunik S. Use of angiotensin receptor blockers such as Telmisartan, Losartsan in nCoV Wuhan Corona Virus infections – Novel mode of treatment. BMJ 2020; 368: m406.
- 14. Spannella F, Giulietti F, Balietti P, et al. Renin-angiotensin system blockers and statins are associated with lower in-hospital mortality in very elderly hypertensives. J Am Med Dir Assoc 2018; 19: 342–347. [DOI] [PubMed] [Google Scholar]