Abstract
Background
On 13 March 2020, the Danish authorities imposed extensive nationwide lockdown measures to prevent the spread of the coronavirus disease 2019 (COVID-19) and reallocated limited healthcare resources. We investigated mortality rates, overall and according to location, in patients with established cardiovascular disease before, during, and after these lockdown measures.
Methods and results
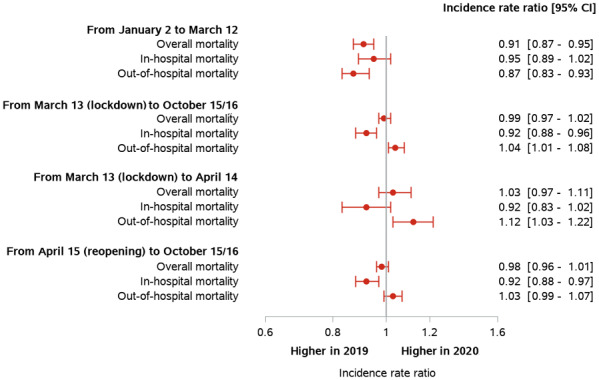
Using Danish nationwide registries, we identified a dynamic cohort comprising all Danish citizens with cardiovascular disease (i.e. a history of ischaemic heart disease, ischaemic stroke, heart failure, atrial fibrillation, or peripheral artery disease) alive on 2 January 2019 and 2020. The cohort was followed from 2 January 2019/2020 until death or 16/15 October 2019/2020. The cohort comprised 340 392 and 347 136 patients with cardiovascular disease in 2019 and 2020, respectively. The overall, in-hospital, and out-of-hospital mortality rate in 2020 before lockdown was significantly lower compared with the same period in 2019 [adjusted incidence rate ratio (IRR) 0.91, 95% confidence interval (CI) CI 0.87–0.95; IRR 0.95, 95% CI 0.89–1.02; and IRR 0.87, 95% CI 0.83–0.93, respectively]. The overall mortality rate during and after lockdown was not significantly different compared with the same period in 2019 (IRR 0.99, 95% CI 0.97–1.02). However, the in-hospital mortality rate was lower and out-of-hospital mortality rate higher during and after lockdown compared with the same period in 2019 (in-hospital, IRR 0.92, 95% CI 0.88–0.96; out-of-hospital, IRR 1.04, 95% CI1.01–1.08). These trends were consistent irrespective of sex and age.
Conclusions
Among patients with established cardiovascular disease, the in-hospital mortality rate was lower and out-of-hospital mortality rate higher during lockdown compared with the same period in the preceding year, irrespective of age and sex.
Keywords: COVID-19, Mortality, Cardiovascular disease
Graphical Abstract
Introduction
Governments worldwide have imposed comprehensive strategies to prevent the rapid spread of the coronavirus disease 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and to alleviate the increasing burden on healthcare systems and providers.1 Such strategies include extensive societal lockdown and reorganization of healthcare systems. Compared with many other countries, the rates of laboratory-confirmed COVID-19 cases and COVID-19 related deaths have been low in Denmark.2 Thus, as of 16 October 2020, Denmark, with a population of 5.8 million people, had a total of 35 291 cases and 679 deaths.2,3 However, these mitigation strategies, which were implemented in Denmark on 13 March 2020, may have a detrimental effect on medical care of other and more prevalent medical conditions and may, for example, affect optimal treatment delivery to patients with acute or established cardiovascular diseases. Another consequence may also be that some individuals experiencing symptoms suggestive of acute cardiovascular conditions or clinical deterioration in established cardiovascular diseases may be more likely to stay at home, and perhaps seek alternative care, rather than attending emergency departments due to fear of acquiring COVID-19.4–16 While the detrimental impact of these widespread strategies has been suggested, longitudinal data in patients with established cardiovascular disease are lacking. Specifically, whether, and to what extent, a lockdown strategy and reorganization of the healthcare system, as well as the pandemic itself, have impacted mortality rates and location of death in patients with established cardiovascular diseases has not been examined. Given that established cardiovascular diseases constitute a leading cause of global morbidity and mortality17,18 and necessitate optimal medical care and regular evaluation, such knowledge is of great importance and will shed light on another possible collateral effect of a lockdown strategy and reorganization of the healthcare system.
We performed a nationwide registry-based cohort study to investigate all-cause mortality rates, overall and according to location of death, in patients with established cardiovascular disease, including ischaemic heart disease, ischaemic stroke, heart failure, atrial fibrillation, and peripheral artery disease, before, during, and after the lockdown of Danish society and reorganization of the healthcare system due to the COVID-19 pandemic.
Methods
The COVID-19 lockdown and reopening in Denmark
On 13 March 2020, the Danish authorities imposed extensive nationwide lockdown measures to prevent the spread of COVID-19, including closure of Danish borders, schools, and daycare facilities, and sending home all employees working in non-essential jobs in the public sector. On 18 March 2020, these measures were further extended to include a ban of gatherings of >10 people.19 The Danish healthcare system was also reorganized, outpatient visits were converted to telemedicine or cancelled, whenever possible, and elective, non-vital procedures were cancelled or postponed. On 6 April, the Danish authorities announced that the government would commence a gradual and controlled reopening of Danish society. The first phase of reopening of Danish society included reopening of schools for younger pupils (15 April) and liberal professions (20 April).19 The second phase included reopening of restaurants and cafes (18 May), schools for older pupils (18 May), cultural and recreational activities (i.e. museums, theatres, and outdoor parks), and research institutions (27 May).19 The third phase included an easing of the ban of gatherings to 50 people (8 June) and allowed all public sector employees to return to work in person (15 June).19
Data sources
In Denmark, all citizens are assigned a unique and personal identification number, which allows accurate linkage of nationwide administrative registries at an individual level. For this study, data from several nationwide administrative registries were obtained. The Danish National Patient Registry contains information on all hospital admissions and outpatient contacts according to the International Classification of Diseases (ICD).20 The Danish National Prescription Registry holds detailed information on dispensing date, strength, and quantity on all claimed drug prescriptions in Denmark.21 The Danish Civil Registration System comprises data on birth date, sex, and vital status [i.e. whether a person is alive and resident in Denmark, disappeared (persons whose residence is unknown to Danish authorities), emigrated, or dead, along with the date of these events].22 Statistics Denmark holds data on education, household income, and marital status.23,24 The Danish registries are validated and of high quality, and have been described in detail previously.20–24
Study population
The study population comprised all Danish citizens with cardiovascular disease who were ≥18 years old and alive on 2 January 2019. The study cohort was dynamic; thus, patients with cardiovascular disease could also enter the study cohort on 2 January 2020 if they were ≥18 years old and alive on this date. The index date for patients who were part of the dynamic cohort in 2019 and 2020 was 2 January 2019 and 2 January 2020, respectively. Established cardiovascular disease was defined as an in-hospital or outpatient diagnosis code of ischaemic heart disease, ischaemic stroke, heart failure, atrial fibrillation, or peripheral artery disease (for ICD codes, see Supplementary material online, Table S1) within 10 years prior to inclusion. These diagnoses have previously been validated with high positive predictive values in the Danish National Patient Registry.25,26
Follow-up and outcomes
The dynamic cohort was followed from the date of inclusion until death or end of follow-up, whichever came first. As 2020 was a leap year and to ensure a similar potential follow-up period, patients included in 2019 and 2020 were followed until 16 October 2019 and 15 October 2020, respectively. The primary outcome was all-cause mortality. Secondary outcomes were in-hospital all-cause mortality and out-of-hospital all-cause mortality. In-hospital mortality was defined as date of death during a hospital admission. Conversely, out-of-hospital mortality was defined as date of death not during a hospital admission.
The rates of outcomes were also examined for each subgroup of patients with established cardiovascular disease (i.e. ischaemic heart disease, ischaemic stroke, heart failure, atrial fibrillation, and peripheral artery disease). The rates of outcomes were also examined in patients with established cardiovascular disease according to sex and age categories (<60 years, 60–79 years, and ≥80 years). Finally, we assessed the total number of cardiovascular admissions (and not only the first during the study period) in patients with established cardiovascular disease. Cardiovascular admissions were defined as any primary of secondary in-hospital diagnosis code of diseases of the circulatory system (ICD-10 code category I) with an overnight stay.
Covariates
Comorbidity was obtained using in-hospital and outpatient diagnosis codes up to 10 years prior to inclusion, i.e. 2 January in 2019 and 2020, respectively (for ICD-10 codes, see Supplementary material online, Table S1). Patients with hypertension were identified using claimed drug prescriptions as described previously.27,28 To quantify the burden of comorbidities, the Charlson Comorbidity Index was calculated as described previously.26 Pharmacotherapy at baseline was defined as claimed prescriptions within 180 days prior to inclusion (for ATC codes, see Supplementary material online, Table S2). The highest level of completed education was classified in accordance with the International Standard Classification of Education. Duration of cardiovascular disease was determined using the date of the first diagnosis code of ischaemic heart disease, ischaemic stroke, heart failure, or peripheral artery disease within 10 years prior to inclusion and graded in years.
Statistics
Baseline characteristics according to inclusion year were reported as frequencies with percentages or medians with 25th–75th percentiles, and differences were tested with the χ2 test for categorical variables and the Mann–Whitney test for continuous variables. In addition, characteristics of patients with an in-hospital and out-of-hospital death, respectively, during lockdown at the time of death in 2019 and 2020 were reported. Rates of overall, in-hospital, and out-of-hospital mortality per 1000 person-years were calculated for each of the 41 weeks in 2019 and 2020 and reported with 95% exact Poisson confidence intervals (CIs). Mortality rate ratios with 95% CIs were calculated using adjusted Poisson regression models for each of the 41 weeks, with the weeks in 2019 as reference. In addition, mortality rate ratios with 95% CIs were calculated using adjusted Cox regression models before (between 2 January and 12 March), during [between 13 March (i.e. the date of the initiation of the Danish COVID-19 lockdown and healthcare reorganization) and 14 April], and after lockdown (between 15 April (i.e. the date of the first phase of reopening) and 15/16 October], with 2019 as reference. All models were adjusted for age modelled as linear spline with two knots at 60 and 80 years, sex, education, living alone, duration of cardiovascular disease (categorial variable), a history of ischaemic heart disease, ischaemic stroke, peripheral artery disease, diabetes mellitus, heart failure, atrial fibrillation, hypertension, malignancy, chronic kidney disease, chronic obstructive pulmonary disease, and liver disease. All statistical analyses were performed with SAS statistical software (SAS 9.4, SAS Institute, Cary, NC, USA) and R (version 3.6.1, The R Foundation).29 The level of statistical significance was set at 5%.
Ethics
In Denmark, registry-based studies that are conducted for the sole purpose of statistics and scientific research do not require ethical approval or informed consent by law. However, the study is approved by the institute responsible for the data [the Capital Region of Denmark (approval number: P-2019-191)] in accordance with the General Data Protection Regulation.
Results
The dynamic cohort comprised 340 392 Danish citizens with cardiovascular disease who were 18 years of age or older and alive on 2 January 2019 and 2 January 2020, respectively. In total, 308 081 (88.7%) who were part of the cohort in 2020 were also part of the cohort in 2019. Patients in 2019 and 2020 were comparable with respect to age, sex, socioeconomic status, comorbidities, and concomitant medical treatment (Table 1).
Table 1.
Baseline characteristics of the study population
| 2019 cohort (n = 340 392) | 2020 cohort (n = 347 136) | |
|---|---|---|
| Demographics | ||
| Age, median (25th–75th percentile) | 71 (62–79) | 72 (62–79) |
| Age, n (%) | ||
| <60 years | 70 133 (20.6) | 69 165 (19.9) |
| 60–79 years | 190 732 (56.0) | 194 899 (56.1) |
| ≥80 years | 79 527 (23.4) | 83 072 (23.9) |
| Male, n (%) | 202 005 (59.3) | 206 991 (59.6) |
| Socioeconomic status | ||
| Education, n (%) | ||
| ISCED 0–2 | 126 298 (37.1) | 125 854 (36.3) |
| ISCED 3 | 140 556 (41.3) | 144 799 (41.7) |
| ISCED 5–6 | 55 142 (16.2) | 57 335 (16.5) |
| ISCED 7–8 | 18 396 (5.4) | 19 148 (5.5) |
| Living alone, n (%) | 134 334 (39.5) | 132 344 (38.1) |
| Comorbidities, n (%) | ||
| Ischaemic heart disease | 125 882 (37.0) | 124 108 (35.8) |
| Ischaemic stroke | 50 674 (14.9) | 53 661 (15.5) |
| Heart failure | 37 777 (11.1) | 42 008 (12.1) |
| Atrial fibrillation | 101 383 (29.8) | 107 200 (30.9) |
| Peripheral artery disease | 18 595 (5.5) | 18 142 (5.2) |
| Hypertension | 171 035 (50.2) | 176 082 (50.7) |
| Diabetes | 28 506 (8.4) | 26 958 (7.8) |
| Malignancy | 32 671 (9.6) | 33 497 (9.6) |
| Chronic kidney disease | 13 889 (4.1) | 14 988 (4.3) |
| Chronic obstructive pulmonary disease | 18 599 (5.5) | 19 082 (5.5) |
| Liver disease | 4560 (1.3) | 4860 (1.4) |
| Charlson Comorbidity Index | ||
| 0 | 138 887 (40.8) | 139 904 (40.3) |
| 1 | 111 004 (32.6) | 114 118 (32.9) |
| 2 | 29 215 (8.6) | 30 337 (8.7) |
| ≥3 | 61 286 (18.0) | 62 777 (18.1) |
| Concomitant medical treatment, n (%) | ||
| Lipid-lowering drugs | 186 989 (54.9) | 193 090 (55.6) |
| Aspirin | 104 940 (30.8) | 102 103 (29.4) |
| ADP receptor inhibitors | 61 556 (18.1) | 63 955 (18.4) |
| Oral anticoagulants | 110 278 (32.4) | 118 367 (34.1) |
| Beta-blockers | 158 066 (46.4) | 161 521 (46.5) |
| Calcium channel blockers | 81 727 (24.0) | 86 450 (24.9) |
| RAAS inhibitors | 154 794 (45.5) | 161 329 (46.5) |
RAAS, renin–angiotensin–aldosterone system; ISCED, International Standard Classification of Education.
ISCED 0–2, early childhood, primary education, and lower secondary education; ISCED 3, general upper secondary education and vocational upper secondary education (ISCED 4 does not exist in Denmark); ISCED 5–6, short-cycle tertiary, medium-length tertiary, and Bachelor’s-level education or equivalent; ISCED 7–8, second-cycle, Master’s level or equivalent and PhD level.
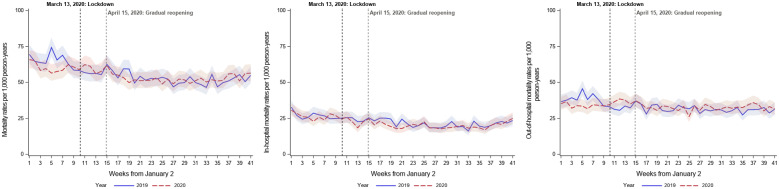
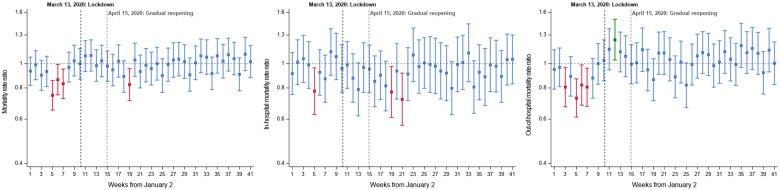
Overall mortality
In total, 14 660 (4.3%) and 14 743 (4.2%) patients died during the study period in 2019 and 2020, respectively. The weekly mortality rates per 1000 person-years from 2 January in 2019 and 2020, respectively are shown in Figure 1A, and Figure 2A displays the weekly adjusted mortality rate ratios in 2020 compared with 2019. The overall mortality rate before13 March was significantly lower in 2020 compared with 2019 [adjusted incidence rate ratio (IRR) 0.91, 95% CI 0.87–0.95]. The overall mortality rate between 13 March (lockdown) and 15/16 October (end of follow-up) was not significantly different in 2020 compared with 2019 (adjusted IRR 0.99, 95% CI 0.97–1.02). Likewise, the mortality rates between 13 March (lockdown) and 14 April and between 15 April (first phase of reopening) and 15/16 October (end of follow-up) were not significantly different in 2020 compared with 2019.
Figure 1.
Weekly mortality rates from 2 January in 2019 and 2020.
(A) Overall mortality; (B) in-hospital mortality; and (C) out-of-hospital mortality.
Figure 2.
Weekly adjusted mortality rate ratios in 2020 compared with 2019.
(A) Overall mortality; (B) in-hospital mortality; and (C) out-of-hospital mortality. Green indicates a significantly increased mortality rate in 2020 compared with 2019. Red indicates a significantly decreased mortality rate in 2020 compared with 2019.
In-hospital and out-of-hospital mortality
Table S3 in the Suppplementary material online displays the characteristics of patients with an in-hospital death between 13 March (lockdown) and 15/16 October (end of follow-up) in 2019 and 2020. Compared with patients who died during hospital admission in 2019, those who died during hospital admission in 2020 were less often living alone (55.6% vs. 51.0%, P-value <0.001) and more often had a history of atrial fibrillation (38.4% vs. 41.2%, P-value 0.01).
The weekly unadjusted in-hospital mortality rates per 1000 person-years from 2 January in 2019 and 2020, respectively, are shown in Figure 1B, and Figure 2B displays the weekly adjusted in-hospital mortality rate ratios in 2020 compared with 2019. The in-hospital mortality rate before 13 March was not significantly lower in 2020 compared with 2019 (adjusted IRR 0.95, 95% CI 0.89–1.02). However, the in-hospital mortality between 13 March (lockdown) and 15/16 October (end of follow-up) was significantly lower in 2020 compared with 2019 (adjusted IRR 0.92, 95% CI 0.88–0.96), with a similar trend between 13 March (lockdown) and 14 April and between 15 April (first phase of reopening) and 15/16 October (end of follow-up).
The characteristics of patients with an out-of-hospital death between 13 March (lockdown) and1 5/16 October (end of follow-up) at the time of death in 2019 and 2020 are shown in Supplementary material online, Table S4. Patients who died out of hospital in 2020 were less often living alone (65.9% vs. 62.0%, P-value <0.001, more often had heart failure (21.1% vs. 22.9%, P-value 0.02, and less often had peripheral artery disease (10.3% vs. 9.1%, P-value 0.02) and diabetes (11.4% versus 10.2%, P-value 0.04) than those who died out of hospital in 2019. The weekly unadjusted out-of-hospital mortality rates per 1000 person-years from 2 January in 2019 and 2020, respectively, are shown in Figure 1C, and Figure 2C displays the weekly adjusted out-of-hospital mortality rate ratios in 2020 compared with 2019. The out-of-hospital mortality rate before 13 March was significantly lower in 2020 compared with 2019 (adjusted IRR 0.87, 95% CI 0.83–0.93). However, the out-of-hospital mortality rate between 13 March (lockdown) and 15/16 October (end of follow-up) was significantly higher in 2020 compared with 2019 (adjusted IRR 1.04, 95% CI, 1.01–1.08), with a similar trend between 13 March (lockdown) and 14 April, and between 15 April (first phase of reopening) and 15/16 October (end of follow-up).
Sex and age
Adjusted IRRs for mortality before and after 13 March in 2020 compared with 2019 according to subgroups are shown in Supplementary material online, Table S5. In both men and women, there was a trend towards a lower in-hospital mortality rate and a trend towards a higher out-of-hospital mortality rate after 13 March in 2020 compared with 2019. A similar trend was seen in patients aged 60–79 years and ≥80 years. In patients ≤60 years, the in-hospital or out-of-hospital mortality rates were not significantly different in 2020 compared with 2019.
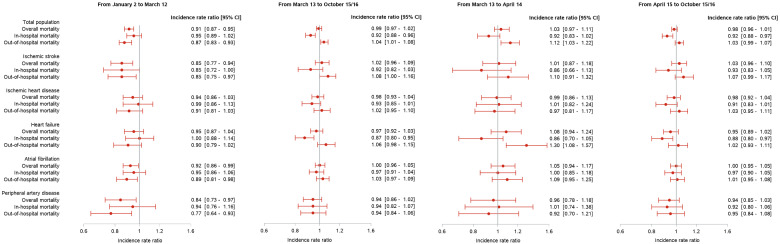
Subgroups of cardiovascular diseases
Adjusted IRRs for mortality before and after 13 March in 2020 compared with 2019 according to subgroups are shown in Figure 3. Between 13 March (lockdown) and 15/16 October (end of follow-up), the overall mortality rate in all subgroups was not significantly different in 2020 compared with 2019. However, there was a trend towards a lower in-hospital mortality rate after 13 March in 2020 compared with 2019 in all subgroups, though this was only statistically significant in patients with heart failure. Likewise, there was a trend towards a higher out-of-hospital mortality rate after 13 March in 2020 compared with 2019 in all subgroups, apart from peripheral artery disease, though this was not statistically significant. Overall, there was a similar trend between 13 March (lockdown) and 14 April and between 15 April (first phase of reopening) and 15/16 October (end of follow-up).
Figure 3.
Adjusted incidence rate ratios for mortality before, during, and after lockdown in 2020 compared with 2019 overall and according to subgroups.
13 March 2020: lockdown.
15 April 2020: first phase of reopening.
Cardiovascular admissions
The total number of cardiovascular admissions during the first 4 weeks after 13 March was lower in 2020 compared with 2019 (Figure 4). After the gradual reopening, the total number of cardiovascular admissions increased and returned to numbers similar to those observed in 2019.
Figure 4.
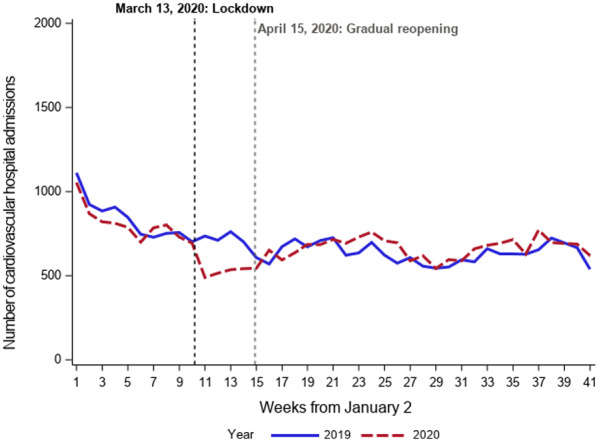
Total number of cardiovascular admissions from 2 January in 2019 and 2020.
Discussion
In this Danish nationwide cohort study, we investigated all-cause mortality rates, overall and according to location of death, in patients with established cardiovascular diseases before, during, and after the lockdown of Danish society and reorganization of the healthcare system due to the COVID-19 pandemic. This study yielded the following major findings: first, the mortality rate in patients with established cardiovascular diseases during lockdown and reopening of Danish society was not significantly different compared with the same period in the preceding year. Second, the in-hospital mortality rate was significantly lower and the out-of-hospital mortality rate significantly higher during lockdown and reopening of Danish society compared with the same period in the preceding year. Third, these findings were consistent across subgroups of cardiovascular diseases.
Although the COVID-19 pandemic is an unprecedented threat to global health in recent time,1 reports of potential collateral effects of the widespread strategies to prevent the rapid spread of SARS-CoV-2 and to alleviate the burden on healthcare systems are emerging. For example, several countries, including the USA, Italy, France, Austria, and Denmark, have observed a substantial decline in hospital admissions for acute cardiovascular diseases, such as acute coronary syndrome, stroke, new-onset atrial fibrillation, and decompensated heart failure, and a considerable proportion of excess deaths not attributed to COVID-19 during the ongoing pandemic.4–16,30,31 There has also been concern that the societal lockdown and reorganization of healthcare systems with reduced routine care may confer an increase in deaths not due to COVID-19 in patients with established cardiovascular diseases. However, whether the potential collateral effects of the COVID-19 lockdown may extend to patients with established cardiovascular diseases has not been investigated. In our nationwide study, we did not observe an increased mortality rate in patients with established cardiovascular diseases during lockdown and reopening of Danish society compared with the same period in the preceding year, and this finding was consistent across all subgroups of established cardiovascular diseases. This finding is also in keeping with a previous study, in which we found that the overall mortality rate in the general population during weeks 1–27 in 2020 was not higher than the mortality rates in the same period in 2015–2019 in Denmark.32 However, this is in contrast to the findings from many other countries.30,31 Although we can only speculate on this finding, it is possible that the implementation of timely, and comprehensive, lockdown measures and subsequent low burden of COVID-19 may in part explain the absence of excess mortality in the general population as well as in patients with chronic cardiovascular diseases. While our findings apparently do not suggest any collateral effects of the lockdown strategy on the care of patients with cardiovascular diseases, further data are needed to establish the long-term impact on the prognosis in these patients.
In Denmark, professional medical societies and patient associations have issued statements and developed tools to increase recognition of symptoms of acute cardiovascular diseases, including stroke and acute coronary syndrome, in the general population and to underline the importance of immediate contact with emergency medical services should such symptoms occur.33,34 Moreover, telehealth has been increasingly adopted in primary and secondary healthcare sectors during the pandemic.6,35 Interestingly, this study demonstrated a marked difference in location of death. While the overall mortality rate in patients with established cardiovascular diseases during lockdown and reopening of Danish society was not different from that of the preceding year, a decrease in the rate of in-hospital mortality and a corresponding increase in the rate of out-of-hospital mortality was observed compared with the same period in 2019. This difference in location of death was evident across all subgroups of established cardiovascular diseases, particularly heart failure. It is therefore important to try to better understand why the overall mortality rate was similar during lockdown compared with the same period in the preceding year despite a substantial change in location of death. It may reflect an increased reluctance of patients with established cardiovascular diseases, particularly those with terminal illness and end-stage disease, to contact emergency medical services and seek medical care due to the message from governments worldwide to stay at home, the fear of acquiring COVID-19 in hospital, or perhaps to avoid adding to an overburdened healthcare system. As patients with established cardiovascular disease are more susceptible to becoming infected with SARS-CoV-2 and have a higher case-fatality rate compared with COVID-19 patients without cardiovascular disease,36–42 these patients are likely to be even more reluctant to contact emergency medical services and to seek medical care. This is in line with recent studies which suggest that the number of hospital admissions for cardiovascular diseases in general have decreased during the COVID-19 pandemic.4–16 An interesting observation was that the incidence rate for out-of-hospital mortality seemed to increase before the implementation of lockdown measures (i.e. from week 8 in 2020 compared with 2019). This finding further supports the notion that the observed changes in mortality patterns are not due to lockdown measures alone, but also reflect an increased reluctance towards seeking medical care due to the message from governments worldwide to stay at home or the fear of acquiring COVID-19 in hospital. What are the potential implications of our findings? We believe that our findings suggest that the message from governments worldwide to stay at home should be more nuanced and reinforce the necessity of a clear public health message to patients experiencing symptoms suggestive of acute cardiovascular conditions or clinical deterioration in established cardiovascular diseases to still seek emergency medical services rather than to stay at home or seek alternative care. Further studies are needed to confirm these findings and to clarify the causes of such changes.
Another interesting finding of this study was the decrease in the overall mortality rate in the first months of 2020 prior to lockdown compared with the same period in the preceding year. The explanations for this observation are not clear and we can only speculate on this finding. However, a substantial decrease in the number of cases with a positive test for influenza in Denmark was observed in the 2020 season compared with the 2019 season (7575 vs. 11 645 positive cases in Denmark, with a population of 5.8 million people)43 and it is possible that this may, in part, contribute to the observed lower mortality rate in 2020 compared with 2019.
Strengths and limitations
In the present study, we used data from complete and unselected nationwide administrative registries, which enables us to examine trends in mortality on a nationwide scale. The Danish healthcare system, funded by taxes, provides equal access to healthcare services for all residents regardless of socioeconomic or insurance status. The findings of this study, however, should be viewed in the context of a number of limitations. The observational nature precludes the assessment of causal inference. Thus, we report associations and not cause–effect relationships. Likewise, the possibility of residual confounding cannot be excluded despite adjustment for potential confounders. Data on important clinical parameters, such as cardiovascular disease severity, symptoms, and laboratory (e.g. estimated glomerular fraction and natriuretic peptides) and echocardiographic measurements, and utilization of visiting nurse services or palliative care initiatives were not available. Likewise, data on COVID-19 status among patients who died were not available. However, the burden of COVID-19 was relatively small in Denmark compared with other European countries and the USA. In Denmark, deaths must be registered within 2 weeks after their occurrence. However, we addressed this potential issue by terminating follow-up on 15 October 2020, despite the fact that data on mortality were available until Mid November 2020. In addition, data on cause of death were not available for this study as the Danish Registry of Causes of Death is currently updated until the end of 2018. Finally, the impact of the societal lockdown and healthcare system reorganization in Denmark with 5.8 million citizens, a universal healthcare system, and high socioeconomic status may not be generalizable to larger countries with less uniform healthcare systems and low socioeconomic status.
Conclusions
Among patients with established cardiovascular disease, the mortality rate during lockdown and reopening of Danish society was similar compared with the same period in the preceding year. However, the in-hospital mortality rate was lower, and the out-of-hospital mortality rate was higher during lockdown and reopening of Danish society compared with the same period in the preceding year.
Supplementary material
Supplementary material is available at European Heart Journal online.
Conflict of interest: T.B.-S. reports personal fees from Amgen, Sanofi Pasteur, and Novartis, and grants from Sanofi Pasteur and GE Healthcare outside the submitted work; L.K. reports personal fees from speakers honoraria from Novo Nordisk, Novartis, Boehringer, and AstraZeneca, outside the submitted work; the other authors have no conflicts of interest to declare.
Supplementary Material
References
- 1. World Health Organization; 2020.WHO Director-General’s opening remarks at the media briefing on COVID-19 – 3 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---3-march-2020. (17 April 2020)
- 2. OVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/map.html (6 November 2020)
- 3. Statens Serum Institut. Overvågningdata for covid-19 i Danmark og Europa. https://covid19.ssi.dk/overvagningsdata (6 November 2020)
- 4. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J 2020;41:1852–1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. De Filippo O, D’Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, Secco GG, Campo G, Gallone G, Verardi R, Gaido L, Iannaccone M, Galvani M, Ugo F, Barbero U, Infantino V, Olivotti L, Mennuni M, Gili S, Infusino F, Vercellino M, Zucchetti O, Casella G, Giammaria M, Boccuzzi G, Tolomeo P, Doronzo B, Senatore G, Grosso Marra W, Rognoni A, Trabattoni D, Franchin L, Borin A, Bruno F, Galluzzo A, Gambino A, Nicolino A, Truffa Giachet A, Sardella G, Fedele F, Monticone S, Montefusco A, Omedè P, Pennone M, Patti G, Mancone M, De Ferrari GM. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med 2020;383:88–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Holt A, Gislason GH, Schou M, Zareini B, Biering-Sørensen T, Phelps M, Kragholm K, Andersson C, Fosbøl EL, Hansen ML, Gerds TA, Køber L, Torp-Pedersen C, Lamberts M. New-onset atrial fibrillation: incidence, characteristics, and related events following a national COVID-19 lockdown of 5.6 million people. Eur Heart J 2020;41:3072–3079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tsivgoulis G, Tsivgoulis G, Katsanos AH, Ornello R, Sacco S. Ischemic stroke epidemiology during the COVID-19 pandemic: navigating uncharted waters with changing tides. Stroke 2020;51:1924–1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mesnier J, Cottin Y, Coste P, Ferrari E, Schiele F, Lemesle G, Thuaire C, Angoulvant D, Cayla G, Bouleti C, Gallet de Saint Aurin R, Goube P, Lhermusier T, Dillinger JG, Paganelli F, Saib A, Prunier F, Vanzetto G, Dubreuil O, Puymirat E, Boccara F, Eltchaninoff H, Cachanado M, Rousseau A, Drouet E, Steg PG, Simon T, Danchin N. Hospital admissions for acute myocardial infarction before and after lockdown according to regional prevalence of COVID-19 and patient profile in France: a registry study. Lancet Public Health 2020;5:e536–e542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP, Mancone M, Mercuro G, Muscoli S, Nodari S, Pedrinelli R, Sinagra G, Indolfi C, Società Italiana di Cardiologia and the CCU Academy investigators group. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J 2020;41:2083–2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, Dixon S, Rade JJ, Tannenbaum M, Chambers J, Huang PP, Henry TD. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 2020;75:2871–2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, Sung S-H, Ambrosy AP, Sidney S, Go AS. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med 2020;383:691–693. [DOI] [PubMed] [Google Scholar]
- 12. European Stroke Organisation. Likely increase in the risk of death or disability from stroke during the COVID-19 pandemic. https://eso-stroke.org/eso/likely-increase-in-the-risk-of-death-or-disability-from-stroke-during-the-covid-19-pandemic/ (17 April 2020)
- 13. Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of Covid-19 on stroke evaluation in the United States. N Engl J Med 2020;383:400–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pandey AS, Daou BJ, Tsai JP, Zaidi SF, Salahuddin H, Gemmete JJ, Oliver MJ, Singer J, Elder TA, Mbabuike N, Adel JG, Gujrati Y, Adeel Saleemi M, Siddiqui FM, Elias AE, Rehman MF, Marin H, Chebl AB, Kole M, Wilseck JM, Kazmierczak CD, Mick JM, Majjhoo AQ, Naravetla BR, Rayes M, Luqman AW, Richards BF, Kelkar P, Burgess R, Thompson BG, Chaudhary N, Mazaris PA, Qahwash O, Razak MA, Jumaa MA; Michigan Stroke Treatment Improvement Collaborative (MISTIC). COVID-19 pandemic—the bystander effect on stroke care in Michigan. Neurosurgery 2020;87:E397–E399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Siegler JE, Heslin ME, Thau L, Smith A, Jovin TG. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis 2020;29:104953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Andersson C, Andersson C, Gerds T, Fosbøl E, Phelps M, Andersen J, Lamberts M, Holt A, Butt JH, Madelaire C, Gislason G, Gislason G, Gislason G, Torp-Pedersen C, Torp-Pedersen C, Køber L, Schou M. Incidence of new-onset and worsening heart failure before and after the COVID-19 epidemic lockdown in Denmark: a nationwide cohort study. Circ Heart Fail 2020;13:e007274. [DOI] [PubMed] [Google Scholar]
- 17. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1736–1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, Ahmed M, Aksut B, Alam T, Alam K, Alla F, Alvis-Guzman N, Amrock S, Ansari H, Ärnlöv J, Asayesh H, Atey TM, Avila-Burgos L, Awasthi A, Banerjee A, Barac A, Bärnighausen T, Barregard L, Bedi N, Belay Ketema E, Bennett D, Berhe G, Bhutta Z, Bitew S, Carapetis J, Carrero JJ, Malta DC, Castañeda-Orjuela CA, Castillo-Rivas J, Catalá-López F, Choi JY, Christensen H, Cirillo M, Cooper L Jr, Criqui M, Cundiff D, Damasceno A, Dandona L, Dandona R, Davletov K, Dharmaratne S, Dorairaj P, Dubey M, Ehrenkranz R, El Sayed Zaki M, Faraon EJA, Esteghamati A, Farid T, Farvid M, Feigin V, Ding EL, Fowkes G, Gebrehiwot T, Gillum R, Gold A, Gona P, Gupta R, Habtewold TD, Hafezi-Nejad N, Hailu T, Hailu GB, Hankey G, Hassen HY, Abate KH, Havmoeller R, Hay SI, Horino M, Hotez PJ, Jacobsen K, James S, Javanbakht M, Jeemon P, John D, Jonas J, Kalkonde Y, Karimkhani C, Kasaeian A, Khader Y, Khan A, Khang YH, Khera S, Khoja AT, Khubchandani J, Kim D, Kolte D, Kosen S, Krohn KJ, Kumar GA, Kwan GF, Lal DK, Larsson A, Linn S, Lopez A, Lotufo PA, El Razek HMA, Malekzadeh R, Mazidi M, Meier T, Meles KG, Mensah G, Meretoja A, Mezgebe H, Miller T, Mirrakhimov E, Mohammed S, Moran AE, Musa KI, Narula J, Neal B, Ngalesoni F, Nguyen G, Obermeyer CM, Owolabi M, Patton G, Pedro J, Qato D, Qorbani M, Rahimi K, Rai RK, Rawaf S, Ribeiro A, Safiri S, Salomon JA, Santos I, Santric Milicevic M, Sartorius B, Schutte A, Sepanlou S, Shaikh MA, Shin MJ, Shishehbor M, Shore H, Silva DAS, Sobngwi E, Stranges S, Swaminathan S, Tabarés-Seisdedos R, Tadele Atnafu N, Tesfay F, Thakur JS, Thrift A, Topor-Madry R, Truelsen T, Tyrovolas S, Ukwaja KN, Uthman O, Vasankari T, Vlassov V, Vollset SE, Wakayo T, Watkins D, Weintraub R, Werdecker A, Westerman R, Wiysonge CS, Wolfe C, Workicho A, Xu G, Yano Y, Yip P, Yonemoto N, Younis M, Yu C, Vos T, Naghavi M, Murray C. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol 2017;70:1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. COVID-19 in Denmark and border crossing – Information from the Danish authorities about coronavirus/COVID-19. https://politi.dk/en/coronavirus-in-denmark (1 October 2020)
- 20. Lynge E, Sandegaard JL, Rebolj M. The Danish national patient register. Scand J Public Health 2011;39:30–33. [DOI] [PubMed] [Google Scholar]
- 21. Wallach Kildemoes H, Toft Sørensen H, Hallas J. The Danish national prescription registry. Scand J Public Health 2011;39:38–41. [DOI] [PubMed] [Google Scholar]
- 22. Pedersen CB. The Danish civil registration system. Scand J Public Health 2011;39:22–25. [DOI] [PubMed] [Google Scholar]
- 23. Jensen VM, Rasmussen AW. Danish education registers. Scand J Public Health 2011;39:91–94. [DOI] [PubMed] [Google Scholar]
- 24. Baadsgaard M, Quitzau J. Danish registers on personal income and transfer payments. Scand J Public Health 2011;39:103–105. [DOI] [PubMed] [Google Scholar]
- 25. Sundbøll J, Adelborg K, Munch T, Frøslev T, Sørensen HT, Bøtker HE, Schmidt M. Positive predictive value of cardiovascular diagnoses in the Danish National Patient Registry: a validation study. BMJ Open 2016;6:e012832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Thygesen SK, Christiansen CF, Christensen S, Lash TL, Sørensen HT. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol 2011;11:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Schramm TK, Gislason GH, Køber L, Rasmussen S, Rasmussen JN, Abildstrøm SZ, Hansen ML, Folke F, Buch P, Madsen M, Vaag A, Torp-Pedersen C. Diabetes patients requiring glucose-lowering therapy and nondiabetics with a prior myocardial infarction carry the same cardiovascular risk: a population study of 3.3 million people. Circulation 2008;117:1945–1954. [DOI] [PubMed] [Google Scholar]
- 28. Olesen JB, Lip GYH, Hansen ML, Hansen PR, Tolstrup JS, Lindhardsen J, Selmer C, Ahlehoff O, Olsen AMS, Gislason GH, Torp-Pedersen C. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ 2011;342:320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. R Core Team. R Core Team 2014 R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing. https://www.R-project.org/. [Google Scholar]
- 30. Rossen LM, Branum AM, Ahmad FB, Sutton P, Anderson RN. Excess deaths associated with COVID-19, by age and race and ethnicity—United States, January 26–October 3, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1522–1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bilinski A, Emanuel EJ. COVID-19 and excess all-cause mortality in the US and 18 comparison countries. JAMA 2020;324:2100–2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mills EHA, Møller AL, Gnesin F, Zylyftari N, Broccia M, Jensen B, Schou M, Fosbøl EL, Køber L, Andersen MP, Phelps M, Gerds T, Torp-Pedersen C. National all-cause mortality during the COVID-19 pandemic: a Danish registry-based study. Eur J Epidemiol 2020;35:1007–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Vi skal ikke tro, at alle andre sygdomme er forsvundet, fordi der er corona. 2020. https://hjerteforeningen.dk/2020/03/vi-skal-ikke-tro-at-alle-andre-sygdomme-er-forsvundet-fordi-der-er-corona/ (11 November 2020)
- 34. Danish Resuscitation Council. Covid-19 epidemien gør det ekstra vigtigt at holde øje med hinanden og reagere akut ved tegn på stroke. 2020. https://twitter.com/Resus_DK/status/1247804200974553096 (11 November 2020)
- 35. Sundhedsstyrelsen. COVID-19: Monitorering af aktivitet i sundhedsvæsenet. Beskrivelse af udviklingen i aktivitet i sundhedsvæsenet under COVID-19. 2020.
- 36. Nishiga M, Wang DW, Han Y, Lewis DB, Wu JC. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol 2020;17:543–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020;323:1239–1242. [DOI] [PubMed] [Google Scholar]
- 38. Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R, Adamo M, Ammirati E, Sinagra G, Lombardi CM, Metra M. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:819–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, Liu L, Shan H, Lei C, Hui DSC, Du B, Li L, Zeng G, Yuen K-Y, Chen R, Tang C, Wang T, Chen P, Xiang J, Li S, Wang J, Liang Z, Peng Y, Wei L, Liu Y, Hu Y, Peng P, Wang J, Liu J, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol 2020;17:259–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Statens Serum institut. Influenzasæsonen – opgørelse over sygdomsforekomst 2019/20. https://www.ssi.dk/sygdomme-beredskab-og-forskning/sygdomsovervaagning/i/influenzasaesonen—opgoerelse-over-sygdomsforekomst-2019–20
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.