Abstract
Background
Healthcare workers have been overexposed to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) during the current pandemic, but there is little information on the impact of SARS-CoV-2 on nephrologists. The aim of this study was to assess SARS-CoV-2 infections in nephrologists in the first and second pandemic waves, describing risk factors and clinical features.
Methods
This national survey was sent to Spanish nephrologists. Epidemiological data, comorbidities and medications were collected and compared between infected and non-infected nephrologists. Symptoms, prescribed treatments and outcomes are described for infected nephrologists.
Results
Three hundred and twenty-seven nephrologists (66% female, age 46 ± 11 years) completed the survey. Of them, 62 (19%) were infected by SARS-CoV-2. Infection was detected by real-time reverse transcription-polymerase chain reaction in the 37 symptomatic patients (62%) and by serological tests in 25 (38%) asymptomatic individuals. Five (8%) of the infected nephrologists were hospitalized. Contrary to the general population, most infections occurred during the first pandemic wave and, specifically, during the first month, when personal protective equipment (PPE) shortages were more severe. Factors associated with infection in univariate analysis were younger age (P = 0.004), work in non-nephrology departments (P = 0.045), higher exposure to coronavirus disease 2019 patients (P < 0.001), lack of appropriate PPE (P < 0.001) and non-O ABO blood group. In an adjusted multivariate model, only lack of appropriate PPE remained predictive of infection [hazard ratio 3.5 (95% confidence interval 1.9–6.8), P < 0.0001].
Conclusions
SARS-CoV-2 infection was frequent among nephrologists, was frequently diagnosed late and was associated with working conditions.
Keywords: COVID-19, healthcare worker, nephrologist, personal protective equipment, SARS-CoV-2
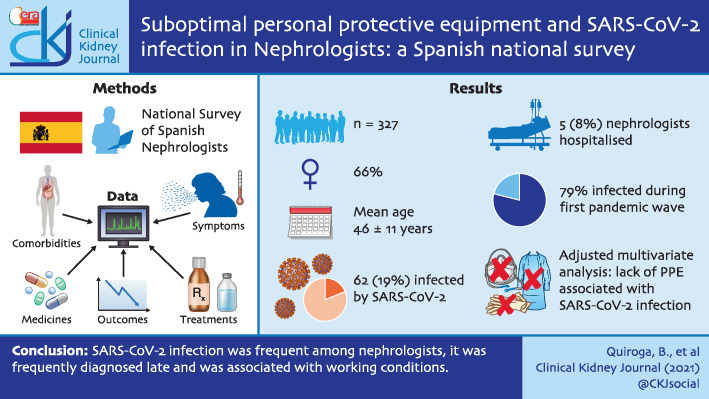
Graphical Abstract
INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has impacted the world, causing a new disease called coronavirus disease 2019 (COVID-19) [1]. One of the main characteristics of SARS-CoV-2 is its high infectivity, which has contributed to worldwide spread. To avoid exponential transmission, several countries established strict lockdowns for their population. However, essential workers [including healthcare workers (HCWs)] were not affected by this measure and were requested to keep working. Despite the need for adequate personal protective equipment (PPE), this was not guaranteed in many countries, especially during the first wave [2, 3].
The first COVID-19 case was declared in Spain on 31 January 2020, and since then, Spain has been one of the countries most affected by the pandemic [4]. More than 20% of all the COVID-19 cases have been among HCWs [5].
Nephrologists have been at the front line during the SARS-CoV-2 pandemic. In addition to the usual care of hospitalized patients, they have had to assist dialysis patients continuously. Haemodialysis patients are at high risk for infection and severe infection due to immune deficiency, healthcare frequentation and collective transport [6, 7]. Thus, during the pandemic, they have attended hospital at least thrice weekly for renal replacement therapy, needing nephrologists for care of infected and uninfected patients. Haemodialysis patients have had one of the highest infection and mortality rates during the COVID-19 pandemic [8, 9]. Therefore, and because of work in COVID-19 teams, nephrologists have been highly exposed to SARS-CoV-2. Very few studies have focused on SARS-CoV-2 infection among HCWs, and no data are available about SARS-CoV-2 infection among nephrologists.
The aim of this national survey was to assess the frequency of SARS-CoV-2 infection among Spanish nephrologists, investigating potential risk factors and clinical characteristics.
MATERIALS AND METHODS
Spanish nephrologists were invited by the Spanish Society of Nephrology to participate in an online anonymous survey to assess the frequency of SARS-CoV-2 infection. Nephrologists were sent an e-mail from the Secretary of the Spanish Society of Nephrology with a link to the survey. Using an online electronic questionnaire of 30 closed questions, nephrologists were asked about their infection situation [real-time reverse transcription-polymerase chain reaction (rRT-PCR) in nasopharyngeal swabs and serum immunoglobulin (Ig) M and IgG antibodies (serology test)] and the date. Medical information including demographic data (sex, age and body mass index), blood group, comorbidities (hypertension, diabetes mellitus, dyslipidaemia, hypothyroidism, chronic kidney disease) and usual treatment with renin–angiotensin–aldosterone blockers were also collected. Deadline for answering the survey was 1 November 2020. Although from the epidemiological point of view there is not a formal definition of the COVID-19 waves and how we define them is arbitrary, we considered the first pandemic wave until 31 May 2020 and the second wave from 1 June 2020 until 30 October 2020, based on the number of infections reported in Spain and the morphology of the incidence curves as per World Health Organization data (https://covid19.who.int/region/euro/country/es; 8 December 2020, date last accessed).
Participants were asked about working conditions, including the total number of weeks worked during the pandemic, requirement to work in non-nephrology departments (COVID-19 wards), place of work (hospital, dialysis centre or both), exposure to COVID-19 patients (defined as the percentage of the total working days during the pandemic used to attend COVID-19 patients) and on-call shifts. They were also asked whether they considered the available PPE to be adequate. The definition of adequate PPE was not defined a priori since it may depend on the actual working conditions of each individual nephrologist and they are well-trained healthcare professionals who could knowledgeably characterize the adequateness of PPE for each individual task.
For infected nephrologists, symptoms, chest X-ray and treatments were collected. They were also asked about the need for hospitalization and intensive care and the length of stay in the hospital. Subjectively, we collected the nephrologists' opinion on the possibility of being a SARS-CoV-2 spreading vector for family members.
The study was approved by the Ethical Committee of the Hospital Universitario de la Princesa (Madrid, Spain) with number 13/20.
Statistics
Values are expressed as mean ± standard deviation or median (interquartile range) depending on their distribution assessed by the Kolmogorov–Smirnov test. Subjects were divided into two groups regarding their infection status (ever SARS-CoV-2 infected or never infected). We compared several variables between the two groups using Chi-square or t-test for parametric variables and Fisher test or Mann–Whitney test for non-parametric variables. We created a variable to determine the working time during the pandemic expressed in weeks and another to estimate the exposure to SARS-CoV-2. Exposure to SARS-CoV-2 is expressed as percentage of time over the pandemic, considering a 'COVID-19 exposed day' as a day in which contact with COVID-19 patients occurred at least once. Independent predictors for infection were assessed using logistic regression including variables with P < 0.1 in univariate analysis and confounders.
All statistical analyses were performed with SPSS 24.0 (SPSS, Inc., Chicago, IL, USA). P-values <0.05 were considered statistically significant.
RESULTS
Baseline characteristics
The survey was sent electronically to 2255 members of the Spanish Society of Nephology [346 (15%) of them were not active], 953 (42%) opened the e-mail and 327 (15%) completed it. Of them, 217 (66%) were women and the mean age was 46 ± 11 years. Baseline characteristics are shown in Table 1 and Supplementary data, Table S1.
Table 1.
Baseline characteristics in SARS-Cov-2-infected and -non-infected nephrologists
| [AQ] | Total (n = 327) |
Infected (n = 62) |
Non-infected (n = 265) |
P-value |
|---|---|---|---|---|
| Sex (female), n (%) | 217 (66) | 43 (69) | 174 (66) | 0.579 |
| Age (years)a | 46 ± 11 | 42 ± 12 | 46 ± 10 | 0.004 |
| Hypertension, n (%) | 27 (8) | 3 (5) | 24 (9) | 0.277 |
| Diabetes mellitus, n (%) | 4 (1) | 0 (0) | 4 (1) | 0.330 |
| Dyslipidaemia, n (%) | 49 (15) | 8 (13) | 41 (15) | 0.610 |
| Hypothyroidism, n (%) | 18 (5%) | 1 (2) | 17 (6) | 0.136 |
| Body mass index (kg/m2)a | 24 ± 4 | 23 ± 3 | 24 ± 4 | 0.059 |
| ABO blood group, n (%)b | 0.014 | |||
| A or AB | 163 (51) | 33 (56) |
130 (50) |
|
| B | 33 (10) | 11 (19) |
22 (8) |
|
| O | 124 (39) | 15 (25) | 109 (42) | |
| Rh blood group (positive), n (%) | 251 (78) | 46 (78) | 205 (79) | 0.922 |
| Chronic kidney disease, n (%) | ||||
| eGFR <60 mL/min/1.73 m2 | 1 (<1) | 0 (0) | 1 (<1) | 0.628 |
| Albuminuria >30 mg/g urinary creatinine | 1 (<1) | 0 (0) | 1 (<1) | 0.640 |
| RAAS blockers, n (%) | 23 (7) | 2 (3) | 21 (8) | 0.191 |
| Working time during the pandemic, n (%) | 0.751 | |||
| <10 weeks | 13 (4) | 1 (2) |
12 (4) |
|
| 10–20 weeks | 10 (3) | 2 (3) |
8 (3) |
|
| 21–30 weeks | 108 (33) | 20 (32) |
88 (33) |
|
| >30 weeks | 196 (60) | 39 (62) | 157 (59) | |
| Work in non-nephrology units, n (%) | 122 (37) | 30 (48) | 92 (35) | 0.045 |
| Place of usual work, n (%) | 0.894 | |||
| Hospital | 291 (89) | 55 (89) |
236 (89) |
|
| Dialysis centre | 23 (7) | 5 (8) |
18 (7) |
|
| Both | 13 (4) | 2 (3) | 11 (4) | |
| On-call shifts n, % | 243 (74) | 46 (74) | 197 (74) | 0.981 |
| Exposure to COVID-19 patients, n (%)c | <0.001 | |||
| 0–25% | 204 (62) | 26 (42) |
179 (67) |
|
| 26–50% | 52 (16) | 14 (23) |
38 (14) |
|
| 51–75% | 29 (9) | 5 (8) |
24 (9) |
|
| 76–100% | 42 (13) | 17 (27) | 25 (9) | |
| Lack of appropriate PPE, n (%)d | 144 (44) | 43 (69) | 101 (38) | <0.001 |
Mean ± standard deviation.
Per cent of total working period.
Personal opinion of the nephrologist.
Complete blood group data is expressed in Supplementary data, Table S1.
GFR, estimated glomerular filtration rate; RAAS, renin–angiotensin–aldosterone system.
Factors associated with infection by SARS-CoV-2
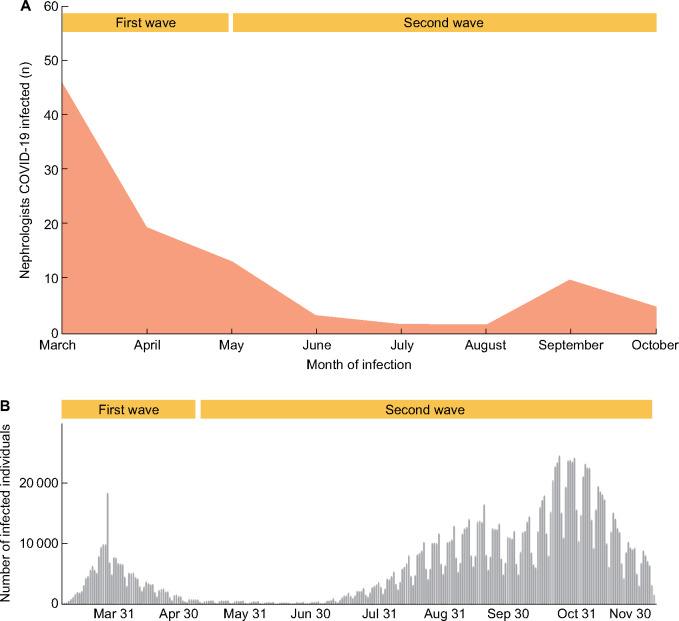
Sixty-two nephrologists (19%) were infected by SARS-CoV-2. A higher proportion of nephrologists were infected by SARS-CoV-2 in the first pandemic wave (48, 79%) than in the second wave (14, 21%; Figure 1A). In fact, most were infected during the first month of the pandemic. This was contrary to the general population data, which disclosed a much higher frequency of diagnosed SARS-CoV-2 infection during the second pandemic wave (Figure 1B). Infection was detected using rRT-PCR in 37 patients (62%) and serological tests in 25 (38%). All nephrologists diagnosed by rRT-PCR were symptomatic.
FIGURE 1:
COVID-19 pandemic in Spain. (A) Number of SARS-CoV-2-infected nephrologists as per the present survey. The number of nephrologists infected per month is represented, with data points connected by straight lines. (B) Number of SARS-CoV-2 infections in Spain. Weekly number of infected individual represented as per the World Health Organization (https://covid19.who.int/region/euro/country/es; 8 December 2020, date last accessed).
Table 1 shows baseline characteristics for SARS-CoV-2-infected and -non-infected nephrologists. Infected nephrologists were younger (P = 0.004) and had a lower frequency of ABO group O (see also Supplementary data, Table S1). In addition, SARS-CoV-2 infection affected more frequently nephrologists that were required to work in non-nephrology departments, usually COVID-19 wards (P = 0.045), and those with higher exposure to COVID-19 patients (P < 0.001; Table 1). The lack of appropriate PPE was more frequent in SARS-CoV-2-infected nephrologists (P < 0.001). A multivariate model confirmed the independent predictor value for lack of appropriate PPE for COVID-19 infection [hazard ratio 3.5 (95% confidence interval 1.9–6.8), P < 0.0001] after adjusting for age, sex, blood group, working in a non-nephrology department and exposure to COVID-19 (Table 2).
Table 2.
Logistic regression of predictors for SARS-CoV-2 infection in nephrologists
| HR (95% CI) | P-value | |
|---|---|---|
| Age (per year) | 2.7 (0.9–1.0) | 0.09 |
| Sex (female) | 1.0 (0.5–1.9) | 0.97 |
| Lack of appropriate PPE | 3.5 (1.9–6.8) | <0.001 |
| ABO blood group (O versus others) | 0.6 (0.3–1.2) | 0.14 |
| Exposure to COVID-19 patients (per 25% increase) | 1.0 (0.7–1.6) | 0.88 |
| Work in non-nephrology units | 1.4 (0.7–2.5) | 0.31 |
HR, hazard ratio; 95% CI, 95% confidence interval.
Symptoms and chest X-ray findings
Among 62 SARS-CoV-2-infected nephrologists, 29 (47%) developed fever, 30 (48%) had cough, 20 (32%) diarrhoea, 36 (60%) myalgia, 25 (44%) anosmia and 28 (40%) dysgeusia. Chest X-ray revealed unilateral infiltrates in seven (11%) nephrologists and bilateral in five (8%).
Treatments and outcomes
Among 62 SARS-CoV-2-infected nephrologists, 16 (26%) received azithromycin, 15 (24%) hydroxychloroquine, 5 (8%) corticosteroids, 1 (2%) remdesivir, 4 (6%) anticoagulants and none tocilizumab. Thirty-nine (63%) patients did not receive any specific treatment. Azithromycin and hydroxychloroquine were administered to infected nephrologists only during the first wave. Among individuals receiving corticosteroids, four were infected in the first wave and one in the second wave. Only one of the four who received anticoagulants was infected in the second wave.
Five nephrologists (8%) needed hospitalization, but none required admission to an intensive care unit. Hospitalized nephrologists were older than those who stayed at home (57 ± 6 versus 40 ± 11 years, P < 0.001). More frequent symptoms in hospitalized patients were fever (100% versus 44%, P = 0.016) and diarrhoea (80 versus 29%, P = 0.021). All hospitalized subjects presented X-ray chest infiltrates (in two cases were unilateral and in three bilateral; 100% versus 14%, P < 0.001 versus non-hospitalized nephrologists). Those hospitalized were more likely to receive azithromycin (80% versus 22%, P = 0.006), hydroxychloroquine (80% versus 21%, P = 0.004), corticosteroids (80% versus 2%, P < 0.001), anticoagulants (80% versus 0%, P < 0.001) and remdesivir (25% versus 0%, P < 0.001). The median length of hospitalization was 12 (5–12) days.
Thirteen patients (21%) thought they had infected a family member and 41 (66%) requested a sick leave.
DISCUSSION
Our study shows the relevant impact of SARS-CoV-2 infection among nephrologists and will help define policy for future pandemics. Thus, it highlights the need to provide healthcare personnel, including those a priori potentially considered as lower risk, with adequate PPE. Thus, the data are consistent with acquisition of the infection during work, illustrating the poor preparedness of the Spanish healthcare system during the first wave of the pandemic and raising questions regarding the monitoring of healthcare personnel, since approximately one-third of infected doctors were unaware of the infection and may have continued to work while infected, exposing colleagues, patients and family alike to the risk of infection.
Professional exposure to SARS-CoV-2 under unprotected conditions has several serious consequences. First, the health consequences of acute COVID-19 infection that may lead to hospitalization and death. Indeed, deaths among Spanish nephrologists have been documented. Secondly, sick leave (41% of infected individuals in our series) increases the workload for colleagues, with a potential negative impact on job performance and mental health [10]. Thirdly, the possibility of developing persistent symptoms under the post-COVID-19 syndrome [11]. Fourthly, the spread of SARS-CoV-2 to colleagues, patients and family members, especially for those with undiagnosed disease. Our data show that up to 21% of the surveyed nephrologists thought they had infected a family member. Social distancing to mitigate the spread of the virus was, in many cases, impossible for HCWs.
During the pandemic, most HCWs in severely hit areas such as Madrid were forced to change their working conditions. Most of the changes related to work in COVID-19 wards at a point when up to 90% of hospitalized patients were COVID-19 patients in some centres. Nephrologists that were required to work in non-nephrology departments were more likely to be infected by SARS-CoV-2. In addition, independently from the medical department where the nephrologists worked, SARS-CoV-2-infected nephrologists had a higher exposure to COVID-19 patients. In this regard, nephrology services changed their organization and probably asked younger HCWs to work in COVID-19 areas, as they were theoretically more protected against the infection complications. In addition, no differences were found on infection rates between in-hospital and in-centre dialysis units, as previously reported in patient-based studies, showing that the preventive measures (when available) were followed by all the professionals independently of the working place [12].
Interestingly, even in this relative small sample, ABO blood group O was associated with lower frequency of SARS-CoV-2, confirming prior reports of susceptibility to SARS-CoV-2 infection [13].
Regarding treatments, temporal differences were found. Thus, by the second wave, it had become clear that azithromycin and hydroxychloroquine were useless, and only corticosteroids or anticoagulants were used [14].
Most infected nephrologists of our series had mild COVID-19 and only five (8%) needed hospitalization. Interestingly, criteria for admission may have differed from usual criteria. As an example, two nephrologists with bilateral infiltrates in chest X-ray were not hospitalized. The reason is unclear, and may range from saturated hospital beds, limiting admission to clearly hypoxic patients, to self-control at home, especially in subjects at low-risk for complications [15]. As expected, hospitalization was more frequent in older nephrologists.
This study has some limitations. First, it relied on an online national survey and not all invited subjects participated. However, a large sample size was obtained that allowed the observation of differences between groups. Secondly, some questions assessed subjective thoughts. The adequacy of PPEs did not have exact predefined criteria, as the concept of adequacy may differ for different clinical circumstances. Thus, we relied on the professional assessment of nephrologists. However, the response fits well with our personal experiences: during the first wave, surgical masks were locked in some centres and requesting one required providing personal identification and a phone number, as well as having a ‘good’ reason why it should be needed; PPE95 masks were not available outside COVID-19 wards and were limited to one per person per week. In this regard, a majority of nephrologists were infected during the first wave, and specifically in March, the month when the lack of PPE was most noticeable. Thirdly, as it is a survey, we do not have information regarding laboratory values and we could not include symptomatic nephrologists with a false-negative test. Finally, unfortunately, some colleagues died during this pandemic and we do not have these data. In this regard, this manuscript is a tribute to them. By contrast, SARS-CoV-2-infected individuals may have been more prone to complete the survey.
In conclusion, nephrologists have been importantly affected during the SARS-CoV-2 pandemic. The main risk factor for SARS-CoV-2 infection was the use of inadequate PPE. In this regard, the epidemiology of COVID-19 in nephrologists was the opposite of that in the general population and was characterized by a higher peak during the first pandemic wave, when the shortage of PPE was more severe. Overall, these data are consistent with acquisition of SARS-CoV-2 infection in the line of duty, and send a strong message to health authorities regarding the need to prepare for future once-in-a-century events to guarantee the safety of healthcare personnel, their patients and their families.
SUPPLEMENTARY DATA
Supplementary data are available at ckj online.
Supplementary Material
ACKNOWLEDGEMENTS
We want to thank all the nephrologists who have completed this survey and the Spanish Society of Nephrology for facilitating its realization. This study is a tribute to all the healthcare workers who have died due to COVID-19 in the exercise of their profession.
FUNDING
This work has not received any financial support of any kind (public, private or non-profit entity).
AUTHORS’ CONTRIBUTIONS
B.Q. was responsible for conception and design, acquisition of data, analysis and interpretation of data and drafting the manuscript. A.O. and P.d.S. were responsible for conception and design, interpretation of data and revised the manuscript. E.S.-A. was responsible for conception and design, and acquisition of data, and revised the manuscript.
CONFLICT OF INTEREST STATEMENT
None declared. The results presented in this paper have not been published previously in whole or part, except in abstract format.
REFERENCES
- 1. Zhu N, Zhang D, Wang W. et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382: 727–733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ortega R, Gonzalez M, Nozari A. et al. Personal protective equipment and Covid-19. N Engl J Med 2020; 382: e105. [DOI] [PubMed] [Google Scholar]
- 3. Carriazo S, Kanbay M, Ortiz A.. Kidney disease and electrolytes in COVID-19: more than meets the eye. Clin Kidney J 2020; 13: 274–280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Spiteri G, Fielding J, Diercke M. et al. First cases of coronavirus disease 2019 (COVID-19) in the WHO European Region, 24 January to 21 February 2020. Euro Surveill 2020; 25: 2000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Equipo COVID-19. RENAVE/CNE/CNM (ISCIII). Informe sobre la situación de COVID-19 en personal sanitario en España, 2020. https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Paginas/InformesCOVID-19.aspx (8 December 2020, date last accessed)
- 6. Syed-Ahmed M, Narayanan M.. Immune dysfunction and risk of infection in chronic kidney disease. Adv Chronic Kidney Dis 2019; 26: 8–15 [DOI] [PubMed] [Google Scholar]
- 7. Rincón A, Moreso F, López-Herradón A. et al. The keys to control a COVID-19 outbreak in a haemodialysis unit. Clin Kidney J 2020; 13: 542–549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Goicoechea M, Sánchez Cámara LA, Macías N. et al. COVID-19: clinical course and outcomes of 36 hemodialysis patients in Spain. Kidney Int 2020; 98: 27–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Williamson EJ, Walker AJ, Bhaskaran K. et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020; 584: 430–436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. El-Hage W, Hingray C, Lemogne C. et al. Health professionals facing the coronavirus disease 2019 (COVID-19) pandemic: What are the mental health risks? Encephale 2020; 46: S73–S80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Demeco A, Marotta N, Barletta M. et al. Rehabilitation of patients post-COVID-19 infection: a literature review. J Int Med Res 2020; 48: 030006052094838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sánchez-Álvarez JE, Pérez Fontán M, Jiménez Martín C. et al. SARS-CoV-2 infection in patients on renal replacement therapy. Report of the COVID-19 Registry of the Spanish Society of Nephrology (SEN). Nefrologia 2020; 40: 272–278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhao J, Yang Y, Huang H. et al. Relationship between the ABO blood group and the COVID-19 susceptibility. Clin Infect Dis 2020; ciaa1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Group RC, Horby P, Mafham M. et al. Effect of hydroxychloroquine in hospitalized patients with Covid-19. N Engl J Med 2020; 383: 2030–2040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Guille C, Sen S.. Prescription drug use and self-prescription among training physicians. Arch Intern Med 2012; 172: 371–372 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.