Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may cause acute kidney injury and thrombosis in patients with coronavirus disease 2019 (COVID-19) [1]. Postmortem studies have shown venous thromboembolism in addition to thrombotic microangiopathy (TMA), endothelial swelling and diffuse microvascular thrombosis consistent with complement fragment deposits in the endothelium [2]. Also, the complement system plays a central role in the pathology of TMA. The successful use of complement inhibitors in a COVID-19 patient with TMA has not been reported previously. In this report we present a COVID-19 patient with TMA who was treated with eculizumab.
A 34-year-old man was admitted to the hospital with symptoms of blurred vision. Two years ago he was diagnosed with primary hypertension and treated with ramipril. His blood pressure was 240/90 mmHg and grade 4 hypertensive retinopathy was detected in the ophthalmic examination. Laboratory data included haemoglobin 14.4 g/dL, platelets 28 700/mm3, leucocytes 4590/mm3, serum creatinine 433 µmol/L, lactate dehydrogenase 1271 U/L and haptoglobin 3 mg/dL. C3 and C4 levels were normaland the direct Coombs test was negative. Urinalysis detected 2.2 g of protein/day. Schistocytes were seen in the peripheral blood smear. Secondary haemostasis tests were in the normal range. TMA was diagnosed and computed tomography of the chest showed unilateral, multifocal and peripheral ground-glass pneumonic infiltrates. Nasopharyngeal swabs were positive for SARS-COV-2 using real-time reverse transcriptase polymerase chain reaction. Glyceryl trinitrate was used for hypertension and hydroxychloroquine with azithromycin was initiated for COVID-19 treatment during hospitalization. After normalization of hypertension, the TMA did not resolve. Disintegrin and metalloproteinase with thrombospondin motifs 13 levels were in the normal range. Anti-cardiolipin, anti-β2-glycoprotein, lupus anticoagulant and anti-nuclear antibodies were negative. The patient was started on eculizumab at 900 mg/week for 4 weeks. He was discharged on Day 15 in good condition. After that, the thrombocytopenia resolved and serum creatinine decreased to 106 µmol/L during outpatient follow-up (Figure 1).
FIGURE 1.
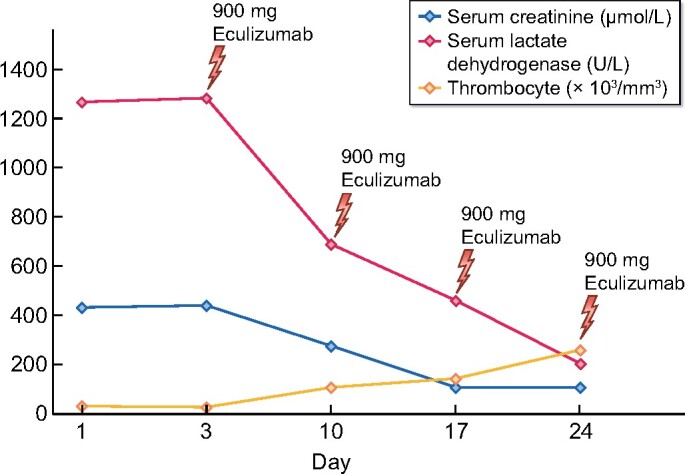
The course of the laboratory results during COVID-19 treatment.
TMA is one of the rare causes of acute kidney injury in COVID-19 patients [3]. TMA can occur in COVID-19 patients due to infections, certain medications and autoimmune disorders [4]. In our patient, we could not perform a renal biopsy because of the patient’s refusal and severe thrombocytopenia. Also, TMA can be associated with COVID-19 after the exclusion of other causes. In addition, his medical history and physical examination were not notable for rheumatologic diseases. However, we could not make a further assessment of the diagnosis of rheumatological disorders and atypical haemolytic uraemic syndrome due to tests that could not be performed for logistical reasons.
TMA can be confused with macrophage activation syndrome and diffuse intravascular coagulation in COVID-19 [5]. Early diagnosis and treatment are essential because of the different treatment strategies. Therefore peripheral blood smear and secondary haemostasis tests are useful in COVID-19 patients presenting with thrombocytopenia. Also, early diagnosis and treatment may reduce morbidity and mortality.
FUNDING
The authors declare no sources of funding for this study.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICAL APPROVAL
This article does not contain any studies with human participants or animals performed by any of the authors.
PATIENT CONSENT
Written informed consent was obtained from the patient.
REFERENCES
- 1. Merrill JT, Erkan D, Winakur J. et al. Emerging evidence of a COVID-19 thrombotic syndrome has treatment implications. Nat Rev Rheumatol 2020; 16: 581–589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Su H, Yang M, Wan C. et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int 2020; 98: 219–227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jhaveri KD, Meir LR, Flores Chang BS. et al. Thrombotic microangiopathy in a patient with COVID-19. Kidney Int 2020; 98: 509–512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ville S, Bot SLE, Chapelet-Debout A. et al. Atypical HUS relapse triggered by COVID-19 Kidney Int 2021; 99: 267–268 [DOI] [PMC free article] [PubMed]
- 5. Iba T, Levy JH, Levi M. et al. The unique characteristics of COVID-19 coagulopathy. Crit Care 2020; 24: 360. [DOI] [PMC free article] [PubMed] [Google Scholar]


