Editor
Coronavirus Disease 2019 (COVID-19) has infected millions people worldwide with hundreds of thousands dead1. As healthcare systems prepared to cope with the pandemic, surgical services made significant adjustments to what would be considered standard of care. Changes included turning surgical theatres into additional critical-care units, postponing non-urgent, non-cancer procedures, and redeploying staff to other medical specialties. Decisions were made in the absence of data to help guide the rapidly evolving processes and conclusions. Thus, there has never been a greater requirement for more research to inform surgical practice. In this study, an international collaboration was gathered to determine the most pressing COVID-19 related surgical research priorities in a modified Delphi process2.
A modified Delphi process was undertaken as previously described2,3. Participants were asked to submit and prioritise questions based on relevance and answerability. They were from multiple countries and backgrounds including heathcare professionals, patients, and clinical scientists. The study was endorsed by the Association of Surgeons of Great Britain and Ireland (ASGBI); Association of Upper Gastrointestinal Surgery of Great Britain and Ireland (AUGIS); Indian Association of Gastrointestinal Endosurgeons (IAGES); Pancreatic Society of Great Britain and Ireland (PSGBI); Society of American Gastrointestinal and Endoscopic Surgeons (SAGES); Sociedad Espanola de Investigaciones Quirurgicas (SEIQ) and World Society of Emergency Surgery (WSES).
Phase I: Participants were invited by twitter to submit questions across the spectrum of “Surgery in the COVID-19 pandemic” via surveymonkey. Members of endorsing societies were also invited via email. Questions were, reviewed, amended and categorized. Phase II: Participants prioritised Phase 1 questions on a Likert Scale (5 — highest research priority). The survey remained open for 72 hours, with the question order randomly assigned. Results were reviewed by a blinded steering committee and questions scoring a weighted mean ≥ 3·8 were included in phase III. Phase III: Participants performed a final round of prioritization over a further 72-hour period. Results were reviewed in the same manner as phase II. The criteria for inclusion in the final list of prioritised research questions was a mean score of ≥4·0, a score of 1 or 2 by <10%, and 4 or 5 by >70% of respondents.
A total of 510 research questions were submitted by 130 participants during Phase I with a median of 4 questions (range 1-10). Submissions were from predominantly general surgeons but included clinical scientists, patients, and other medical specialties from 25 countries (Fig. 1a). Following review by the steering committee, 96 questions were progressed for prioritisation in phase II.
Fig. 1.
Maps showing location of stakeholders' responses during each phase. A) Phase 1 responses, summarized in country location (left panel) and by continent and specialty (right panel) B) Phase II responses, summarized in country location (left panel) and by continent and specialty (right panel) C) Phase III responses, summarized in country location (left panel) and by continent and specialty (right panel)
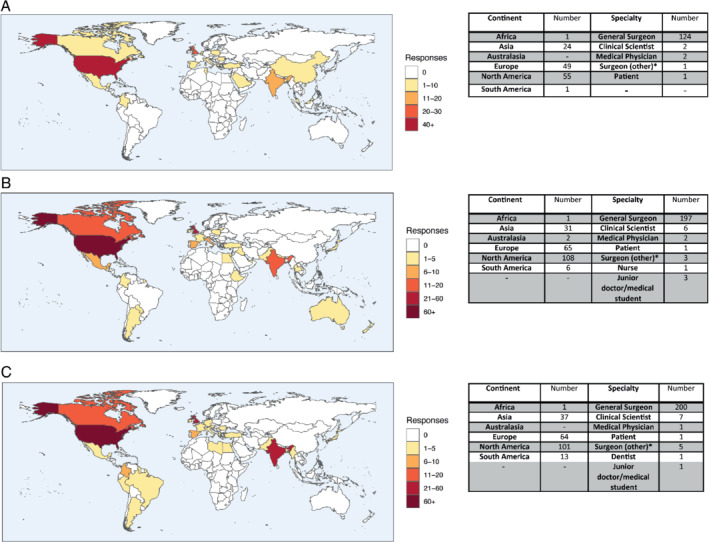
*Surgeons (other): Trauma and Orthopaedics, Paediatric, Plastic, Urology, Obstetrics and gynaecology.
Two-hundred and thirteen participants prioritised the questions in phase II, with a 90·6% completion rate. These were predominantly general surgeons from 34 countries (Fig. 1b). Thirty-nine questions were progressed for prioristisation in round III. Questions were prioritized by 216 stakeholders from 26 countries, with a 90·3% completion rate in phase III (Fig. 1c). At the end of phase III, 13 questions met the criteria to be defined as a high research priority (Table 1). Thirty-eight participated in at least two of the three phases throughout the Delphi process.
Table 1.
Final list of prioritized research questions
| Category | Questions |
|---|---|
| Theatre environment and technical consideration | Are SARS-CoV-2 particles aerosolized during endoscopy, laparoscopy or open surgery? |
| Theatre environment and technical consideration | What are the most effective methods for preventing the spread of SARS-CoV-2 during aerosol generating procedures? |
| Theatre environment and technical consideration | What are the risks of SARS-CoV-2 aerosol generation in the use of electrocautery devices during the COVID-19 pandemic? |
| Theatre environment and technical consideration | What are the safest approaches to protect the theatre team from COVID-19 transmission during open and laparoscopic surgery? |
| Laparoscopy | Is laparoscopy an aerosol generating procedure, and if so what precautions should be taken before, during and after laparoscopic surgery? |
| Laparoscopy | What is the risk of SARS-CoV-2 virus transmission during laparoscopic/MIS surgery? |
| Protective Equipment | What personal protective equipment should be donned by the operating team undertaking a surgical procedure (open, laparoscopic or robotic) during the COVID-19 pandemic? |
| Elective Surgery | Should all patients undergoing elective surgical procedures be tested for COVID-19 prior to surgery and how should they be screened? |
| General | Are COVID-19 positive patients at risk of transmitting the SARS-CoV-2 virus to the healthcare team through bodily fluids or aerosolized particles? |
| General | Does the presence of SARS-CoV-2 antibodies confer protection from reinfection? |
| General | Is there an increased incidence of perioperative complications in COVID-19 positive patients following surgery (e.g. SSI, VTE/PE)? |
| General | What are the principal factors influencing mortality in COVID-19 surgical patients? |
| General | What is the impact of COVID-19 infection on surgical outcomes? |
The COVID-19 pandemic has had a significant impact on global surgical activity which will persist for an unknown period of time4. There was some repetition in the 13 final questions such that further research could be condensed down to five key areas: virus aerosolization during surgery; effective personal protective equipment (PPE); pre-operative screening; antibodies/immunity; viral infection and surgical outcomes. A safe strategy to facilitate surgery is fundamental to the patient and staff safety5,6. There are limitations to the results presented here including that countries with high response rates were those nations in which the surgical societies supported the study. Lower response rates were noted from certain countries where the virus first emerged.
References
- 1. World Health Organization . Coronavirus Disease 2019 (COVID-19) Situation Report — 121. WHO: Geneva. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200520-covid-19-sitrep-121.pdf?sfvrsn=c4be2ec6_2. [Google Scholar]
- 2. Wilson MS, Blencowe NS, Boyle C, Knight SR, Petty R, Vohra RSet al. . A modified Delphi process to establish future research priorities in malignant oesophagogastric surgery. Surgeon 2019; 10.1016/j.surge.2019.11.003 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 3. Knight SR, Pathak S, Christie A, Jones L, Rees J, Davies Het al. . Use of a modified Delphi approach to develop research priorities in HPB surgery across the United Kingdom. HPB (Oxford) 2019; 21: 1446–1452. [DOI] [PubMed] [Google Scholar]
- 4. COVIDSurg Collaborative . Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg 2020; 10.1002/bjs.11746 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Abdelrahman T, Beamish AJ, Brown C, Egan RJ, Evans T, Ryan Harper Eet al. . Surgery during the COVID-19 pandemic: operating room suggestions from an international Delphi process. Br J Surg 2020; 10.1002/bjs.11747 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]


