Editor
The COVID-19 outbreak greatly impacted surgical activities. Restrictions were imposed globally based on precautionary principle.
Little is known of the nosocomial risk for COVID-negative patients undergoing surgery, nor the risk of operating on COVID patients during the epidemic1.
We reviewed patients who underwent surgery in an academic hospital in the particularly affected Paris area during the 4 initial weeks of surgical restrictions, encompassing the epidemic peak.
This study was approved by the Institutional Review Board. All patients who received a surgical procedure during the study period were included. The clinical situation was updated at least 3 weeks after the procedure.
Patients were considered positive when the reverse transcription Polymerase Chain reaction was positive or the pathognomonic computed tomography scanner signs2 were found. The data collected included patients demographic information, dates of admission/discharge, post-hospitalization orientation, comorbidities, date of surgery, department, type of intervention, emergency and oncological indications, type of anesthesia, pre/post operative COVID-19 tests, post-operative symptoms, COVID-19 specific intensive care unit (ICU) admission/death, symptoms among patients surroundings.
Population
472 patients received 524 procedures between 13th March and 9th April 2020. Twenty-four (5 per cent) patients were lost of follow-up. Median time from surgery to status update was 35 days (range: 21-55). Patients' characteristics are presented in Table 1.
Table 1.
Patients characteristics: entire cohort, preoperative COVID, non-COVID patients, postoperative COVID patients and comparison between non-COVID vs. postoperative COVID patients
| Population | Total 472 (24 lost follow-up) | Preoperative COVID 13 | Non COVID 439 | Postoperative COVID 20 | Non COVID vs Postoperative COVID p-value |
|---|---|---|---|---|---|
| Gender ratio F/M | 189/283 (0·67) | 2/11 (0·18) | 177/262 (0·67) | 10/10 (1) | 0·529 |
| Age in years median (IQL) | 64 (50-74) | 71 (58-77) | 63 (49-74) | 78 (66-87) | <0·001 |
| BMI in kg/m 2 median | 25 (22-18) | 26 (26-28) | 25 (22-28) | 26(24-28) | 0·527 |
| Comorbidities | |||||
| Obesity | 71 (16·9) | 0 (0·0) | 68 (17·3) | 3 (21·4) | 0·967 |
| High Blood Pressure | 199 (42·9) | 7 (53·8) | 180 (41·8) | 12 (60·0) | 0·269 |
| Diabetes | 96 (20·8) | 4 (30·8) | 86 (20·0) | 6 (30·0) | 0·427 |
| Chronic Respiratory Failure | 21 (4·6) | 0 (0·0) | 21 (4·9) | 0 (0·0) | 0·581 |
| Chronic Cardiac Failure | 41 (8·9) | 0 (0·0) | 36 (8·4) | 5 (25·0) | 0·04 |
| Chronic Kidney Failure | 66 (14·2) | 3 (23·1) | 56 (13·0) | 7 (35·0) | 0·02 |
| Immunodeficiency | 61 (13·2) | 0 (0·0) | 60 (14·0) | 1 (5·0) | 0·492 |
| Length of Hospital Stay in days Median (IQL) | 5 (2-12) | 8 (4-18) | 5 (2-11) | 15 (6-28) | 0·365 |
| Emergency Indications | 195 (41·3) | 8 (61·5) | 177 (40·3) | 10 (50·0) | 0·529 |
| Oncologic Indications | 149 (31·6) | 3 (23·1) | 141 (32·1) | 5 (25·0) | 0·672 |
| Department | 0·591 | ||||
| Cardiac | 1 (0·2) | 0 (0·0) | 1 (0·2) | 0 (0·0) | |
| Gastroenterology | 120 (25·4) | 3 (23·1) | 111 (25·3) | 6 (30·0) | |
| Neurosurgery | 36 (7·6) | 1 (7·7) | 32 (7·3) | 3 (15·0) | |
| Orthopedic | 74 (15·7) | 1 (7·7) | 70 (15·9) | 3 (15·0) | |
| Urology | 63 (13·3) | 4 (30·8) | 57 (13·0) | 2 (10·0) | |
| Visceral | 49 (10·4) | 0 (0·0) | 49 (11·2) | 0 (0·0) | |
| Vascular | 49 (10·4) | 1 (7·7) | 44 (10·0) | 4 (20·0) | |
| Plastic surgery | 77 (16·3) | 2 (15·4) | 73 (16·6) | 2 (10·0) | |
| Other | 3 (0·6) | 1 (7·7) | 2 (0·5) | 0 (0·0) | |
| Type of Anesthesia | 0·283 | ||||
| General | 341 (72·2) | 12 (92·3) | 318 (72·4) | 11 (55·0) | |
| Spinal | 11 (2·3) | 0 (0·0) | 10 (2·3) | 1 (5·0) | |
| Local | 113 (23·9) | 1 (7·7) | 104 (23·7) | 8 (40·0) | |
| COVID specific Intensive Care Unit Admission | 5 (2·1) | 4 (57·1) | 0 (0·0) | 1 (5·0) | |
| COVID specific Death | 3 (1·3) | 0 (0·0) | 0 (0·0) | 3 (15·0) |
COVID-19 before surgery
135/472 (29 per cent) patients had a pre-operative COVID-19. This rate increased along the 4-week period (figure 1). Thirteen (10 per cent) were positive: 3 were pre-diagnosed ICU patients requiring surgery: 2 remained 31 and 36 days after surgery, 1 was discharged; 10 (7 per cent) were detected with a pre-operative test. One patient was admitted to ICU the day after surgery and discharged from hospital after 9 days. All of the 10 patients diagnosed from systematic tests were discharged, 4 developed symptoms but did not require ICU. No patient died.
Fig. 1.
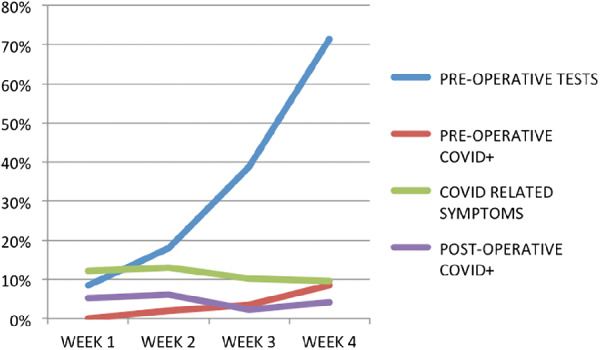
Weekly description of the surgical population: pre-operative test rates (blue), pre-operative COVID-confirmed rates (red), post-operative COVID-related symptoms rates (green), postoperative COVID-confirmed rates (purple)
COVID-19 after surgery
54/448 (12 per cent) of patients developed COVID-19-related symptoms at a median time of 8 days post-surgery. Thirty-three were tested: 16 were positive. Sixty-nine asymptomatic patients received a post-operative test, 4 were positive. Overall, 20 patients from 101 tested had a confirmed COVID-19 after surgery. Positive postoperative test rate was 20 per cent, shifting from 6 per cent for asymptomatic patients to 48 per cent in case of symptoms. Within these 20 patients, 1 (0·5 per cent) was admitted in ICU 5 days after surgery. Three (15 per cent) patients died of COVID-19 (7, 15, 15 days after surgery). The overall post-operative COVID-19 specific ICU admission/death were respectively 0·2 per cent/0·7 per cent. COVID patients were significantly older (78 vs. 64 years old; p < 0·001), had more chronic kidney (35 per cent vs. 13 per cent; p = 0·02) and chronic cardiac failure (25 per cent vs. 8 per cent; p = 0·04) compared to COVID negative patients. There was no significant difference regarding other variables (Table 1).
Evolution of preoperative COVID-19 negative population
122 patients were negative on systematic preoperative tests. Four (3 per cent) were lost of follow-up; 17/118 (14 per cent) developed COVID related symptoms at a median time of 11 days post-surgery. Fourteen were tested: 4 positive cases. Overall, 39 were tested postoperatively after a negative preoperative test, 5/39 (13 per cent) were positive (1 asymptomatic patient). None died or required ICU.
This study is the first to report on COVID-19 epidemic peak specific risk in a comprehensive surgical population.
Firstly, the COVID-19 specific death rate is limited but real (0·7 per cent). Surgeries during the epidemic should be maintained for emergencies and cancer-related surgeries. Secondly, the COVID-19 specific ICU admission rate was low (0·2 per cent). This point should reassure fears of adding stress to overwhelmed ICU. Thirdly, the contaminated population was significantly older, with more chronic kidney and cardiac failures. Alternatives to surgery should be particularly considered when possible for these specific populations. Our results are consistent with recent reports (3-5).
The burden of surgery for COVID patients, with no death, looks better than the recent Lei et al study reporting a mortality rate of 20·5 per cent1.
Among the patients who received both pre/post surgery tests, 13 per cent turned positive. The concomitant national lockdown made extra-hospital contamination unlikely in this subgroup.
References
- 1. Lei S, Jiang F, Su W, Chen C, Chen J, Mei W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine 2020; 10.1016/j.eclinm.2020.100331 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Han R, Huang L, Jiang H, Dong J, Peng H, Zhang D. Early Clinical and CT Manifestations of Coronavirus Disease 2019 (COVID-19) Pneumonia. AJR Am J Roentgenol 2020; 10.2214/ajr.20.22961 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 3. Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents 2020; 10.1016/j.ijantimicag.2020.105924 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet Lond Engl 2020; 395: 507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhao XY, Xu XX, Yin HS, Hu QM, Xiong T, Tang YY, et al. Clinical characteristics of patients with 2019 coronavirus disease in a non-Wuhan area of Hubei Province, China: a retrospective study. BMC Infect Dis 2020; 10.1186/s12879-020-05010-w [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]


