Background:
Intraneural ganglion cysts are nonneoplastic mucinous cysts that form by the accumulation of thick mucinous fluid in the epineurium of peripheral nerves. Symptoms arise from mechanical compression of adjacent nerve fascicles from the intraneural ganglion cyst, and include local or radiating pain, paresthesias, weakness, and muscle atrophy.
Methods:
Retrospective review of three cases of symptomatic intraneural ganglion cysts affecting the upper and lower extremity.
Results:
In our cases, the intraneural ganglion cysts were completely decompressed with resection of the articular branches, leading to improvement in the patient’s symptoms.
Conclusions:
Treatment of intraneural ganglion cysts requires an understanding of the underlying anatomy and pathophysiology; accurate early diagnosis is important and can lead to timely treatment and better outcomes.
INTRODUCTION
Intraneural ganglion cysts are nonneoplastic mucinous cysts formed by the accumulation of thick mucinous fluid in the epineurium of peripheral nerves with most found in para-articular or articular locations.1–3
The most commonly affected nerve in the body is the common peroneal nerve, and in the upper extremity, the most frequently affected nerves are the ulnar and radial nerves.1–6
Symptoms arise from mechanical compression of adjacent nerve fascicles from the intraneural ganglion cyst, and include local or radiating pain, paresthesias, weakness, and muscle atrophy.2
MRI is the study of choice for diagnosis of an intraneural ganglion cyst.5–14 It is important to distinguish this condition from other possible causes of peripheral neuropathy and compression because early diagnosis can facilitate timely treatment and better outcomes.
We describe 3 cases of successful treatment of symptomatic intraneural ganglion cysts of the upper and lower extremity.
CASE 1
The patient was a 16 year-old right-hand dominant adolescent boy with a right dorsal wrist mass of 3 years duration. Although initially soft, the mass progressively became firmer and tender to palpation. Paresthesias were reported and exacerbated with writing and physical activity. MRI revealed a lobulated mass with peripheral enhancement in the subcutaneous tissues overlying the dorsal aspect of the distal metaphysis of the radius.
Given the patient’s clinical presentation, an excisional biopsy was planned. Using a longitudinal incision over the mass on the radial border of the dorsal wrist, a cystic mass containing clear fluid was immediately identified. This was determined to be an intraneural ganglion cyst encompassing 2 dorsal branches of the superficial radial nerve, with a chain-of-beads configuration measuring 2–3 cm in length. The remainder of the superficial radial nerve was intact with a normal appearance.
Upon distal dissection, the intraneural ganglion cyst was found to communicate with a cyst stalk arising from the 3–4 intercompartmental septum between the third and fourth extensor compartments. The third and fourth extensor compartments were opened to retract the adjacent tendons and to follow the cyst stalk to its origin from the radiocarpal joint. The cyst was resected, and the cyst stalk was spread widely at its base, creating a dorsal wrist arthrotomy and revealing hypertrophic synovium within the radiocarpal joint. An articular branch of the superficial radial nerve was visualized within the stalk of the cyst. This articular branch was presumed to be the portal of entry for cyst fluid into the superficial radial nerve and was transected to prevent recurrence of the intraneural ganglion cyst. An adjacent posterior interosseous nerve branch was also transected to minimize potential cyst recurrence. Due to the inextricable nature of the cyst in the proximal portion of the involved superficial radial nerve branches, those branches were divided further proximally in the normal part of the nerve, crushed, cauterized, and buried into the flexor carpi radialis muscle. Histologic examination confirmed the diagnosis of intraneural ganglion cyst. The patient had a successful postoperative course with complete resolution of symptoms, without any cyst recurrence noted at 6 years postoperatively.
CASE 2
The patient was a 52 year-old right-hand dominant man who presented with an 11-week history of left foot drop. The patient also had occasional pain at the popliteal fossa, anterior leg, and lateral leg, as well as the dorsal aspect of the foot and ankle. The patient reported two prior similar episodes of foot drop, in the same extremity, with full spontaneous recovery.
On physical examination, the patient had paresthesias along the cutaneous distributions of the deep and superficial peroneal nerves. A Tinel’s sign was positive at the dorsal ankle and foot, and over the distal course of the deep peroneal nerve in the foot. The scratch collapse test was positive at the fibular neck, and the anterior crural septum.
Diagnostic workup, including MRI of the spine, did not provide a definitive etiology for the patient’s clinical presentation. Electromyography showed no detectable motor unit potentials of the tibialis anterior and extensor hallucis longus muscles.
Based on the clinical presentation and physical examination, a surgical decompression of the common peroneal nerve at the fibular neck was planned.13 At surgery, an oblique incision was made over the course of the common peroneal nerve at the fibular neck, and the nerve caliber was enlarged in appearance.
A lucency on the cephalic aspect of the common peroneal nerve was noted, indicating the presence of an intraneural ganglion cyst. The articular branch of the deep peroneal nerve was identified and also found to contain intraneural fluid, which we presumed to be in communication with the more proximal intraneural fluid initially seen in the common peroneal nerve proximal to the fibular neck.
The intraneural ganglion cyst was scored with a knife over a nonfascicular region, and the ganglion cyst fluid was expressed. The articular branch of the deep peroneal nerve was transected at its entry to the proximal tibiofibular joint to prevent recurrence of the intraneural ganglion cyst. A lacrimal probe was then passed distally: (1) from the main portion of the cyst in the common peroneal nerve at the site of decompression, (2) into the articular branch of the deep peroneal nerve, and (3) out through a small fistulous opening at the distal transected end of the articular branch. This maneuver confirmed that the main portion of the common peroneal nerve intraneural ganglion cyst, proximal to the fibular neck, was contiguous with the articular branch of the deep peroneal nerve. The common peroneal nerve was fully decompressed along its course at the fibular neck, and the intraneural cyst was unroofed and emptied of fluid along its length.
Postoperatively, 11 months after common peroneal nerve decompression and intraneural ganglion cyst treatment, the patient recovered substantial ankle dorsiflexion strength and became independent of his ankle-foot orthosis.
CASE 3
A 55-year-old patient presented with sudden left foot drop associated with numbness and severe pain to the lateral side of the ankle and dorsal aspect of the foot.
On physical examination, the patient had paresthesias along the cutaneous distribution of the deep peroneal nerve. Distal sensation was otherwise intact. Tinel’s sign was negative at the dorsal foot, dorsal ankle, tarsal tunnel, lateral leg, and over the anterior and lateral compartments of the leg. MRI showed a cystic structure in the articular branch of the peroneal nerve with denervation changes in the tibialis anterior muscle.
Common peroneal nerve decompression with concurrent intraneural ganglion cyst treatment was planned. An oblique incision was made over the course of the common peroneal nerve at the fibular neck. The common peroneal nerve and intraneural ganglion cyst were immediately identified. The deep peroneal nerve was notably dilated and filled with fluid upon its entry into the anterior compartment of the leg. Next, the cyst-containing articular branch of the deep peroneal nerve was visualized, where it supplied the superior tibiofibular joint. The joint was distracted to reveal the origin of the intraneural ganglion cyst. Proximally, the cyst was unroofed in a nonfascicular region of the nerve. The chain-of-beads cystic structures noted distally within the nerve were meticulously dissected and unroofed while preserving all of the surrounding nerve fascicles. Finally, the articular branch was transected where it entered the superior tibiofibular joint. Histologic examination confirmed that this was an intraneural ganglion cyst.
Three weeks following decompression of the common peroneal nerve and treatment of the intraneural ganglion cyst, the patient reported substantial improvement in ambulation. Sensation to light touch remained intact in the superficial peroneal, deep peroneal, and sural nerve distributions. At 8 months follow-up, the patient had full ankle dorsiflexion strength without pain.
DISCUSSION
The etiology of intraneural ganglion cysts has been controversial. In recent years, the articular/synovial theory has become widely accepted. According to this theory, cysts are formed when synovial fluid escapes from a capsular defect of a joint and spreads along the epineurium of an attached nerve branch.1 In all of our cases, involvement of articular nerve branches was noted intraoperatively, supporting the articular/synovial theory. However, close examination proximally along the parent nerve trunk and distally along other branches arising from the same parent nerve trunk should be performed, as more than 1 intraneural ganglion cyst can be found along the course of a parent nerve trunk and its branches due to antegrade and retrograde intraneural communication of ganglion cysts as theorized by the “cross-over” principle described by Spinner et al.15 This distal-proximal-distal path for ingress of the intraneural ganglion cyst fluid is clearly demonstrated in Case 2 above, as the cyst fluid is presumed to arise from the proximal tibiofibular joint, traveling (1) proximally along the articular branch into the common peroneal nerve, and (2) distally along the deep peroneal nerve branch into the motor fascicle to tibialis anterior.
Intraneural ganglion cysts can mimic the clinical presentation of patients with other causes of peripheral neuropathy or even vasculopathic claudication in some cases.11 This is due to compression of the peripheral nerve containing the intraneural ganglion cyst, with (1) extrinsic compression due to overlying structures tightening over the enlarged cystic nerve, and (2) intrinsic compression due to local stretching and compression of adjacent nerve fascicles by the expanding intraneural cyst. In 2 of our cases, patients presented with a focal neurological deficit (foot drop) due to the intraneural ganglion cyst. This presentation parallels similar reports in the literature.12
Many patients report sudden sharp neuropathic pain, which they often describe as a “lightning-strike” or “tearing” type of intense electrical sensation, shortly before their first notice of the palpable/visible mass of the cyst or before the first onset of neuropathic changes like numbness or weakness. This likely represents the initial extension of ganglion cyst fluid from the joint space into the nerve structure.
Ultrasound is a suitable diagnostic tool for pinpointing intraneural ganglion cysts. However, ultrasound examination is highly examiner-dependent and smaller lesions can be missed when using this technique as a primary diagnostic modality. MRI is preferred for diagnosis of intraneural ganglion cysts, as it provides detailed characterization of the associated anatomy. The complete extent of the lesion can be precisely determined, and the nerve fascicles can be shown in greater detail. In addition, the consequences of muscle denervation can be effectively visualized.5
Surgical management is the mainstay for patients with symptomatic intraneural ganglion cyst. Multiple surgical options have been described, including ultrasound-guided aspiration, cyst resection, neurolysis, and articular branch disconnection. With the articular/synovial theory becoming the most widely accepted theory, the most commonly reported operative approach to treat cyst symptoms and prevent intraneural recurrence has been cyst decompression and articular branch disconnection.7
Historically, surgical management has led to disappointing outcomes and high rates of recurrence, which have been estimated at 11%.7 Desy et al. reported a recurrence rate of 13% following isolated cyst decompression without articular branch disconnection. Articular branch ligation or disconnection led to an improved 6% recurrence rate, and no intraneural recurrence was observed after surgical procedures that addressed the adjacent joint.7–9 In our cases, the intraneural ganglion cysts were completely decompressed with resection of the articular branches, leading to improvement in ankle dorsiflexion strength and relief of pain. Debridement of the adjacent superior tibiofibular joint was not performed due to the preference of the consulting orthopedic surgeon.
In summary, intraneural ganglion cysts can cause debilitating pain and weakness, and prompt diagnosis and treatment leads to improved outcomes. A thorough understanding of the pathophysiology and clinical course of this entity allows for individualized and efficacious surgical intervention.
Fig. 1.
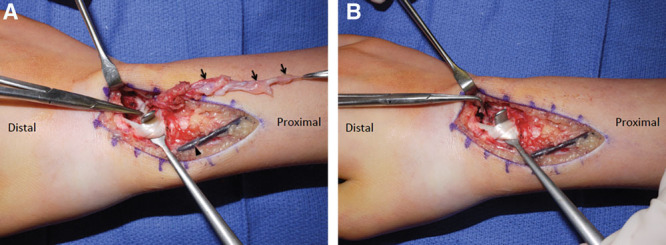
Case 1. A, The involved nerve branches have been transected proximally to their branch point from the main trunk of the superficial radial nerve (proximal clamp). Intraneural ganglion cysts are clearly visualized in a chain-of-beads pattern along the nerve branches (arrows). The base of the cyst at the dorsal radiocarpal joint capsule is indicated by the distal clamp. The extensor pollicis longus and radial wrist extensor tendons are reflected radially for visualization of the cyst base, and the cephalic vein (arrowhead) indicates the approximate course of the main trunk of the superficial radial nerve. B, A small nerve branch (clamp) was visualized running with the cyst stalk into the dorsal radiocarpal joint capsule. The stalk has already been excised and opened at its base.
Fig. 2.
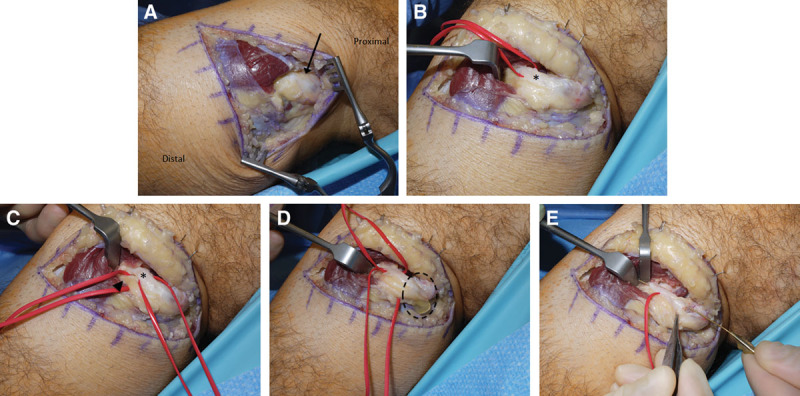
Case 2. A, A cystic dilation (arrow) was immediately visualized upon dissection of the left common peroneal nerve. B, The articular branch (asterisk) of the peroneal nerve was dissected at the cephalic aspect of the deep peroneal nerve and noted to be occupied by cyst fluid. C, The motor branch (arrowhead) to the tibialis anterior was distinct from the articular branch (asterisk), but was also found to be full of cyst fluid. The motor branch was left fully intact, but was decompressed by releasing adjacent compressive structures and by draining the main cyst body (Fig. 2D). D, The main body of the cyst was decompressed proximally, with return of typical ganglion cyst fluid (dotted circle). E, Following transection of the articular branch at its insertion to the superior tibiofibular joint, we demonstrated continuity between the main body of the cyst and the distal transected end of the articular branch by passing a lacrimal probe through the intraneural cyst track. The articular branch was transected to eliminate the pathway for ingress of intraneural cyst fluid.
Fig. 3.
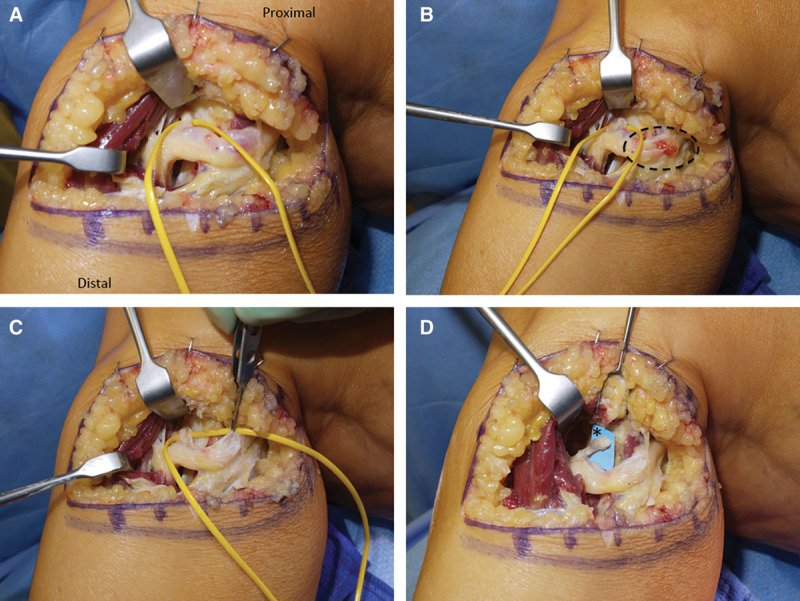
Case 3. A, The left peroneal nerve was decompressed and noted to contain an intraneural ganglion cyst. The articular branch (vessel loop) to the superior tibiofibular joint was dissected and found to contain cyst fluid. B, The cyst decompression was begun proximally, with return of cyst fluid (dotted circle). The cyst was noted to be continuous with the intraneural fluid of the articular branch distally (vessel loop). C, The course of the cyst was decompressed distally through the terminal segment of the articular branch. D, The articular branch was transected distally at its insertion, and the distal transected end (asterisk) was reflected laterally into the peroneus musculature.
Footnotes
Published online 16 February 2021.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Desy NM, Wang H, Elshiekh MA, et al. Intraneural ganglion cysts: A systematic review and reinterpretation of the world’s literature. J Neurosurg. 2016;125:615–630. [DOI] [PubMed] [Google Scholar]
- 2.Buckley CE, Tong E, Spence LD, et al. Intraneural ganglion cyst involving the tibial nerve—a case report. BJR Case Rep. 2017;3:20160116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fricke T, Schmitt AD, Jansen O. Intraneural ganglion cysts of the lower limb. Rofo. 2019;191:732–738. [DOI] [PubMed] [Google Scholar]
- 4.Wilson TJ, Hebert-Blouin MN, Murthy NS, et al. The nearly invisible intraneural cyst: A new and emerging part of the spectrum. Neurosurg Focus 2017;42:E10. [DOI] [PubMed] [Google Scholar]
- 5.Silveira CRS, Vieira CGM, Pereira BM, et al. Cystic degeneration of the tibial nerve: Magnetic resonance neurography and sonography appearances of an intraneural ganglion cyst. Skeletal Radiol. 2017;46:1763–1767. [DOI] [PubMed] [Google Scholar]
- 6.Spinner RJ, Mikami Y, Desy NM, et al. Superficial radial intraneural ganglion cysts at the wrist. Acta Neurochir (Wien). 2020;160;2479–2484. [DOI] [PubMed] [Google Scholar]
- 7.Desy NM, Lipinski LJ, Tanaka S, et al. Recurrent intraneural ganglion cysts: Pathoanatomic patterns and treatment implications. Clin Anat. 2015;28:1058–1069. [DOI] [PubMed] [Google Scholar]
- 8.Lisovski V, Minderis M. Intraneural ganglion cyst: A case report and a review of the literature. Acta Med Litu. 2019;26:147–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spinner RJ, Atkinson JL, Scheithauer BW, et al. Peroneal intraneural ganglia: The importance of the articular branch: Clinical series. J Neurosurg. 2003;99:319–329. [DOI] [PubMed] [Google Scholar]
- 10.Gillenwater J, Cheng J, Mackinnon SE. Evaluation of the scratch collapse test in peroneal nerve compression. Plast Reconstr Surg. 2011;128:933–939. [DOI] [PubMed] [Google Scholar]
- 11.Ozden R, Uruc V, Kalaci A, et al. Compression of common peroneal nerve caused by an extraneural ganglion cyst mimicking intermittent claudication. J Brachial Plex Peripher Nerve Inj. 2013;8:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park SH, Do HK, Jo GY. Compressive peroneal neuropathy by an intraneural ganglion cyst combined with L5 radiculopathy. A case report. Medicine(Baltimore). 2019;98:e17865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kao DS, Cheng J. Peripheral neuropathy: Surgical approaches simplified for the imagers. Semi Musculoskelet Radiol. 2015:19:121– 12–9. [DOI] [PubMed] [Google Scholar]
- 14.Vibhor W, John F, Jonathan C, et al. Intraneural ganglion cyst at the wrist presenting as radial neuropathy. Ann Med Health Sci Res. 2017;7:20–22. [Google Scholar]
- 15.Spinner RJ, Amrami KK, Wang H, et al. Cross-over: A generalizable phenomenon necessary for secondary intraneural ganglion cyst formation. Clin Anat. 2008;21:111–118. [DOI] [PubMed] [Google Scholar]


