Abstract
Objectives
Coronavirus disease 19 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is associated with diverse clinical, including hematologic, abnormalities. We describe peripheral blood and bone marrow findings in deceased and living patients with COVID-19.
Methods
We examined bone marrows from 20 autopsies and 2 living patients with COVID-19 using H&E-stained slides and immunohistochemical stains. Clinical history and laboratory values were reviewed. HScore was calculated to estimate risk of hemophagocytic lymphohistocytosis (HLH).
Results
The deceased patients included 12 men and 8 women (aged 32 to >89 years; median, 63 years). Hematologic abnormalities included frequent neutrophilic leukocytosis, lymphopenia, anemia, and thrombocytopenia; one patient showed striking erythrocytosis. The bone marrows were all normocellular to hypercellular, most showing maturing trilineage hematopoiesis with myeloid left shift. In all 19 evaluable bone marrows, hemophagocytic histiocytes were identified. The HScore for secondary HLH ranged from 35 to 269 (median, 125; >169 in 5 patients). Coinfections were identified in 6 patients. In 2 living patients, bone marrow showed maturing trilineage hematopoiesis, including one showing few hemophagocytic histiocytes.
Conclusions
Peripheral blood from deceased patients with COVID-19 frequently showed neutrophilic leukocytosis, lymphopenia, and, rarely, secondary polycythemia; hemophagocytosis was common in their bone marrow. Consistent with other studies, we provide histopathologic evidence of secondary HLH development in patients with COVID-19.
Keywords: COVID-19, SARS-CoV-2, CBC, Peripheral blood, Bone marrow, Hemophagocytosis, Coronavirus
Key Points.
• We noted a high incidence of hemophagocytosis in the bone marrow from patients with coronavirus disease 2019 (COVID-19) who underwent autopsy (100% of 19 evaluable marrows).
• Common hematologic abnormalities in patients with fatal COVID-19 included neutrophilic leukocytosis, lymphopenia, and anemia.
• Our findings provide histopathologic data to support secondary hemophagocytic lymphohistiocytosis as one of the manifestations of COVID-19.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the agent that causes coronavirus disease 2019 (COVID-19), represents a severe and ongoing threat to public health worldwide.1 Much focus on COVID-19, both clinically and histopathologically, has centered on patients with acute respiratory failure and corresponding diffuse alveolar damage of their lungs.2,3 Although there is still much to learn regarding the pulmonary consequences of COVID-19, comparatively little is known about the effects of COVID-19 on other tissues. Several studies have described findings in the peripheral blood and/or bone marrow, but the spectrum of hematologic findings remains to be defined.4-7
Immune dysfunction has been implicated in the morbidity and mortality of affected patients.8,9 Recent studies discussing the hyperinflammatory state of patients who test positive for COVID-19 have noted an overproduction of cytokines, which may correlate with secondary hemophagocytic lymphohistiocytosis (HLH).8,9 Understanding changes in the bone marrow of affected individuals is of particular importance given these clinical concerns about HLH. In this report, we describe the hematologic and histopathologic findings in the bone marrow of 20 patients who died of COVID-19 and in 2 living patients infected by SARS-CoV-2. A striking finding at autopsy was the frequent presence of marrow hemophagocytosis.
Materials and Methods
This study was approved by our hospital’s institutional review board. This is a single-center retrospective study of 22 patients who tested positive for COVID-19 at our institution from March to July 2020 who had bone marrow available for histopathologic examination. The bone marrows from 2 surgical specimens and the first 20 consecutive autopsies of patients positive for COVID-19 from March to April 2020 were evaluated. Nasopharyngeal swabs were taken premortem during hospitalization or postmortem in the case of deaths that occurred outside our institution and were analyzed using real-time reverse transcription polymerase chain reaction. Normal values used for hematologic parameters were as established at our institution: WBC count, 4.5 to 11 × 109/L; hemoglobin, 13.5 to 17.5 g/dL; hematocrit, 41 to 53 L/L; platelets, 150 to 400 × 109/L; absolute neutrophil count (ANC), 1.8 to 7.7 × 109/L; and absolute lymphocyte count (ALC), 1 to 4.8 × 109/L. Postmortem examination was performed on 20 patients; the bone marrow was obtained from rib squeeze.10,11
For purposes of comparison, we collected the bone marrow at the time of autopsy from 10 patients who tested negative for COVID-19; the bone marrow was obtained from rib squeeze. The autopsy cases were performed by the same prosecutor during a 2-week period. All 10 patients tested negative for COVID-19 premortem at least once within the 2 weeks before death, and 7 of the 10 patients tested negative for COVID-19 twice within the 2 weeks before death. The patients were selected solely based on their negative COVID-19 status with no additional clinical information provided to the reviewer at the time of histologic review.
Additional bone marrow samples from 2 living patients who tested positive for COVID-19, obtained during clinical care, were also examined, one from a below-the-knee amputation and one from the sternum during treatment of a pericardial effusion. The formalin-fixed paraffin-embedded tissues were sectioned in 5 μm onto glass slides and stained using H&E. The bone marrow was evaluated for overall cellularity; myeloid-to-erythroid ratio; overall appearance of myeloid cells, erythroid cells, and megakaryocytes; presence and extent of hemophagocytosis; and any additional findings such as the presence of lymphoid aggregates. Immunohistochemical staining for CD68 was performed to highlight the macrophages. Selected cases were evaluated with antibodies to E-cadherin, CD71, glycophorin, myeloperoxidase, CD61, CD20, CD3, CD5, LEF1, and cyclin D1 to highlight hematologic elements Table 1. The patients’ electronic medical records were retrospectively reviewed, and demographic information, laboratory data, clinical presentation, hospital course, and comorbidities were documented. We assessed the patients’ risk for secondary HLH by calculating their HScore, which provides numerical point values for each of the following 9 variables: (1) known immunosuppression, (2) high temperature, and (3) organomegaly; laboratory values for (4) triglycerides, (5) ferritin, (6) serum glutamic oxaloacetic transaminase, and (7) fibrinogen; (8) cytopenia(s); and (9) the histologic presence of hemophagocytosis in the bone marrow.12 We used an HScore of greater than or equal to 169 as our cutoff value, which corresponds to sensitivity of 93% and specificity of 86% for the diagnosis of HLH.12 Statistical analysis including 2-tailed paired t tests and the Fisher exact test was performed using GraphPad Prism version 5.02 (GraphPad Software), with significance defined as P < .05.
Table 1.
Antibody Clones Used for Immunohistochemical Stains
| Antigen | Vendor, Dilution, Clone |
| CD68 | Biocare, RTU, clone KP1 |
| E-cadherin | Leica, RTU, clone 36B5 |
| CD71 | Bio SB, RTU, clone 10F11 |
| Glycophorin | Dako, 1:500, clone Ref40f |
| MPO | Leica, RTU, clone 59A5 |
| CD61 | Leica, RTU, clone 2f2 |
| CD20 | Leica, 1:100, clone L26 |
| CD3 | Leica, RTU, clone LN10 |
| CD5 | Leica, RTU, clone 4C7 |
| LEF1 | Bio SB, RTU, clone ep310 |
| Cyclin D1 | Leica, RTU, clone ep12 |
RTU, ready to use.
Results
Peripheral blood and bone marrow from the first 20 consecutive patients who tested positive for COVID-19 and underwent postmortem examination were evaluated. There were 12 men and 8 women, with an age range of 32 to more than 89 years (median, 63 years). There were 11 White non-Hispanic patients, 8 Hispanic patients, and 1 Black non-Hispanic patient. The cohort showed the following comorbidities: 80% with hypertension, 50% with diabetes, 25% with asthma, and 15% with immunosuppression (renal transplant, methotrexate use for psoriasis, and chronic prednisone use for sarcoidosis). The body mass index (BMI) ranged from 19.8 to 69.3 (median, 32.7); 14 (70%) of 20 patients were obese (with BMI >30). Six of 20 patients were former smokers, whereas the other 14 were never smokers; there were no current smokers in the cohort. One patient had chronic lymphocytic leukemia (CLL) Table 2. All 20 patients were admitted with hypoxemic respiratory failure and/or fever, accompanied by altered mental status in 15 cases and clinical findings of meningo-encephalitis including seizures in 1 case. Three patients died at outside facilities, with details of their presentation not available. Duration of hospitalization before death ranged from less than 1 day to 15 days. The principal cause of death in all 17 in-house cases was hypoxemic respiratory failure. Three patients died at outside facilities and were transferred following death to our institution for autopsy; although cause of death was not provided, the autopsy findings in these 3 patients were all consistent with respiratory failure.
Table 2.
Clinical Data for 20 Autopsied Patients Who Tested Positive for COVID-19
| Characteristic | Result |
|---|---|
| Age, range, median, y | 32 to >89, 63 |
| Male, No. (%) | 12 (60) |
| Female, No. (%) | 8 (40) |
| Ethnicity, No. (%) | |
| White, non-Hispanic | 11 (55) |
| Hispanic | 8 (40) |
| Black | 1 (5) |
| Comorbidities, No. (%) | |
| Hypertension | 16 (80) |
| Diabetes mellitus, type 2 | 10 (50) |
| BMI, range (median) | 19.8-69.3 (32.7)a |
| Asthma | 5 (25) |
| Immunosuppression | 3 (15)b |
| Malignancy | 3 (15)c |
| Other | 4 (20)d |
BMI, body mass index.
a70% obese (BMI > 30).
bMethotrexate for psoriasis, 1 patient; renal transplant, 1 patient; chronic prednisone for sarcoidosis, 1 patient.
cMetastatic urothelial carcinoma, 1 patient; metastatic ovarian serous carcinoma, 1 patient; chronic lymphocytic leukemia, 1 patient.
dLatent tuberculosis, 1 patient; chronic kidney disease, 3 patients.
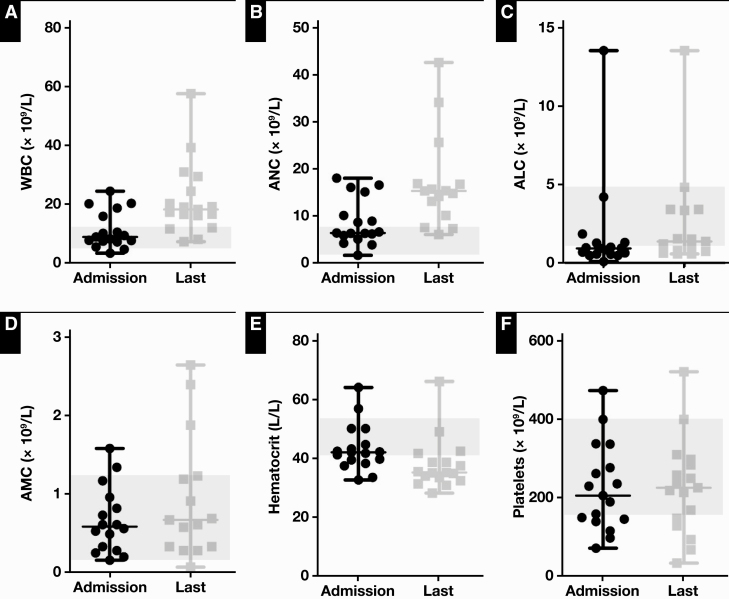
Complete blood counts (CBC) were obtained during hospitalization in 17 patients with autopsy Table 3. Their hematologic abnormalities are summarized in Figure 1 and included leukocytosis in 5 patients on admission (WBC count, 15.8-24.4 × 109/L; median, 20.1 × 109/L) and in 15 patients on their last CBC (WBC count, 11.6-57.4 × 109/L; median, 19.0 × 109/L), elevated neutrophils in 7 patients on admission (ANC, 8.66-18.03 × 109/L; median, 15.1 × 109/L) and in 12 patients on their last CBC (ANC, 10.11-42.5 × 109/L; median, 15.5 × 109/L), lymphopenia in 11 patients on admission (ALC, 0.09-0.97 × 109/L; median, 0.65 × 109/L) and in 5 patients on their last CBC (ALC, 0.58-0.79 × 109/L; median, 0.63 × 109/L), anemia in 6 patients on admission (hematocrit, 32.7-39.8 L/L; median, 38.0 L/L) and in 13 patients on their last CBC (hematocrit, 28.2-38.7 L/L; median, 34.9 L/L), and thrombocytopenia in 6 patients on admission (platelets, 71-149 × 109/L; median, 127 × 109/L) and in 4 patients on their last CBC (platelets, 67-147 × 109/L; median, 110 × 109/L). One patient had leukopenia and neutropenia on admission (WBC count, 3.3 × 109/L; ANC, 1.7 × 109/L); no patient had leukopenia or neutropenia on their last CBC. One patient had thrombocytosis (platelets, 472 × 109/L) on admission, and another had thrombocytosis (platelets, 520 × 109/L) in the last CBC. A two-tailed paired t-test comparison of the patients’ first and last CBCs revealed that there was a statistically significant increase in WBC count (mean, 10.21 × 109/L; 95% confidence interval [CI], 3.85-16.57 × 109/L; P = .0036) and ANC (mean, 8.77 × 109/L; 95% CI, 3.26-14.28 × 109/L; P = .0042) and significant reduction in hematocrit (mean, 5.59 L/L; 95% CI, 2.75-8.43 L/L; P = .0007).
Table 3.
Clinical and Laboratory Data, Including Parameters of the HScore for Deceased Patients Who Tested Positive for COVID-19
| Patient | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | |
| Clinical data | ||||||||||||||||||||
| Age, y | 76 | 76 | 59 | 60 | 66 | 56 | 76 | 33 | 75 | 32 | 72 | 48 | 40 | 87 | 89 | 45 | >89 | 85 | 44 | 57 |
| Sex | F | M | M | F | M | M | F | M | F | F | M | M | M | M | F | F | M | M | F | M |
| Race/ethnicity | W | W | W | H | H | H | W | W | H | H | W | H | H | W | W | B | W | W | W | H |
| BMI | 38.9 | 35.4 | 34.4 | 35.3 | 37.1 | 31.6 | 32.5 | 28.6 | 31.7 | 61.0 | 21.5 | 30.6 | 45.8 | 27.1 | 23.0 | 69.3 | 19.8 | 32.8 | 44.8 | 30.0 |
| Known coinfection | No | No | No | Yes | No | Yes | Yes | Yes | No | No | NA | Yes | No | No | No | NA | NA | Yes | No | No |
| CBC values, initial and final | ||||||||||||||||||||
| WBC, initial, × 109/L | 7.69 | 10.02 | 9.30 | 5.43 | 10.41 | 4.66 | 15.8 | 8.81 | 20.24 | 18.66 | NA | 8.18 | 7.62 | 3.32 | 24.38 | NA | NA | 7.16 | 20.12 | 7.43 |
| WBC, final, × 109/L | 8.00 | 19.11 | 57.43 | 16.54 | 20.17 | 11.95 | 16.08 | 18.96 | 18.17 | 30.87 | NA | 11.55 | 39.19 | 7.26 | 24.38 | NA | NA | 17.21 | 29.4 | 16.48 |
| HGB, initial, g/dL | 13.9 | 14.8 | 13.5 | 13.3 | 13.4 | 16.5 | 17.9 | 12.5 | 16.0 | 10.1 | NA | 11.8 | 15.3 | 10.9 | 14.2 | NA | NA | 13.9 | 20.3 | 14.1 |
| HGB, final, g/dL | 12.8 | 11.3 | 9.9 | 11.8 | 11.4 | 9.7 | 14.9 | 10.9 | 13.3 | 11.4 | NA | 11.3 | 11.4 | 9.9 | 14.2 | NA | NA | 11.1 | 21.2 | 8.2 |
| HCT, initial, L/L | 43.2 | 42.2 | 38.3 | 39.8 | 41.2 | 50.1 | 56.9 | 37.5 | 50.1 | 32.7 | NA | 39.5 | 44.7 | 33.6 | 42.4 | NA | NA | 41.8 | 64.1 | 42.1 |
| HCT, final, L/L | 38.7 | 35.1 | 31.4 | 35.5 | 34.9 | 32.4 | 49.0 | 33.5 | 41.7 | 37.5 | NA | 38.7 | 35.2 | 30.9 | 42.4 | NA | NA | 34.0 | 66.1 | 28.1 |
| PLT, initial, × 109/L | 140 | 229 | 139 | 158 | 261 | 71 | 276 | 115 | 145 | 337 | NA | 472 | 189 | 205 | 399 | NA | NA | 97 | 336 | 235 |
| PLT, final, × 109/L | 168 | 520 | 257 | 33 | 225 | 147 | 218 | 128 | 67 | 213 | NA | 93 | 249 | 283 | 399 | NA | NA | 240 | 297 | 309 |
| ANC, initial, × 109/L | 6.15 | 8.88 | 8.66 | 4.18 | 5.05 | 3.85 | 15.1 | 6.29 | 16.55 | 16.05 | NA | 6.58 | 6.27 | 1.65 | 10.11 | NA | NA | 6.34 | 18.03 | 5.81 |
| ANC, final, × 109/L | 7.33 | 15.35 | 42.50 | 15.68 | 16.72 | NA | 14.78 | 15.32 | 16.84 | 25.62 | NA | 7.53 | 34.1 | 6.04 | 10.11 | NA | NA | 14.16 | NA | 13.12 |
| ALC, initial, × 109/L | 1.27 | 0.09 | 0.48 | 0.93 | 4.21 | 0.48 | 0.55 | 0.94 | 1.84 | 1.31 | NA | 0.65 | 0.83 | 0.97 | 13.5 | NA | NA | 0.57 | 0.71 | 1.03 |
| ALC, final, × 109/L | 0.63 | 1.03 | 4.82 | 0.58 | 1.55 | NA | 0.58 | 1.37 | 0.79 | 3.42 | NA | 3.34 | 3.41 | 0.74 | 13.5 | NA | NA | 1.22 | NA | 1.52 |
| HScore parameters | ||||||||||||||||||||
| Underlying immunosuppression | Yes | No | No | No | No | Yes | No | No | No | No | Yes | No | No | No | No | No | No | No | No | No |
| Temperature, maximum, °C | 39.3 | 39.6 | 37 | 40.1 | 39.1 | 42.4 | 37.5 | 40.4 | 37.7 | 39.5 | NA | 40 | 39.9 | 37.2 | 37.5 | NA | NA | 38.1 | 37.8 | 39.9 |
| Organomegaly | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No |
| Cytopenia, lineagesa | 0 | 0 | 0 | 1 | 0 | 3 | 0 | 1 | 1 | 0 | NA | 1 | 0 | 1 | 0 | NA | NA | 1 | 0 | 1 |
| Ferritin, ng/mL | 675 | 758 | 1,619 | 25,018 | 5,182 | 7,689 | 4,398 | 798 | 942 | 413 | NA | 2,768 | 3,961 | 351 | 1,064 | NA | NA | 464 | 690 | 664 |
| Triglycerides, mmoles/L | NA | 4 | 8 | 5 | 13 | 14 | NA | NA | 2 | 14 | NA | 5 | 6 | 1 | NA | NA | NA | 6 | 0 | 3 |
| Fibrinogen, g/L | NA | 12.41 | 13.35 | 6.06 | 10.08 | 6.51 | NA | 6.41 | 5.66 | 7.1 | NA | 7.61 | 11.2 | 8.55 | NA | NA | NA | 9.63 | 7.33 | 6.54 |
| AST, IU/L | 42 | 121 | 229 | 1,977 | 1,553 | 206 | 72 | 68 | 180 | 53 | NA | 87 | 205 | 26 | NA | NA | NA | 71 | 42 | 306 |
| Hemophagocytosis | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NAb | Yes | Yes | Yes | Yes | Yes | Yes |
| HScore | 105 | 147 | 118 | 217 | 186 | 269 | 89 | 103 | 98 | 132 | 53 | 202 | 202 | 0 | 35 | 35 | 35 | 54 | 54 | 147 |
ALC, absolute lymphocyte count; ANC, absolute neutrophil count; AST, glutamic oxaloacetic transaminase; B, Black; H, Hispanic; HCT, hematocrit; HGB, hemoglobin; NA, not available; W, White.
aDefined as hemoglobin <9.2 g/dL, WBC <5 × 109/L, platelets <110 × 109/L; evaluated over the course of hospitalization.
bMarrow too necrotic for evaluation.
Figure 1.
Hematologic data on admission and last CBC before death for the 17 patients with in-house autopsy. Gray bar demonstrates normal range for WBC count (P = .0036) (A), absolute neutrophil count (ANC; P = .0042) (B), absolute lymphocyte count (ALC) (C), absolute monocyte count (AMC) (D), hematocrit (P = .0007) (E), and platelets (F).
The patient with a history of CLL had an absolute lymphocytosis consistent with persistent CLL. One patient had erythrocytosis (admission hemoglobin/hematocrit, 20.3 g/dL/64.1 L/L) as well as a neutrophilic leukocytosis and died less than 24 hours after admission, with the last CBC showing hemoglobin/hematocrit of 21.2 g/dL/66.1 L/L; erythropoietin was elevated at 45.5. CBC had been normal 4 months before admission. During hospitalization, the patient’s physical examination noted moist mucous membranes, and no concerns for dehydration were noted. Five patients had giant platelets on peripheral smear. Plasma cells were identified on the peripheral smears for 2 patients.
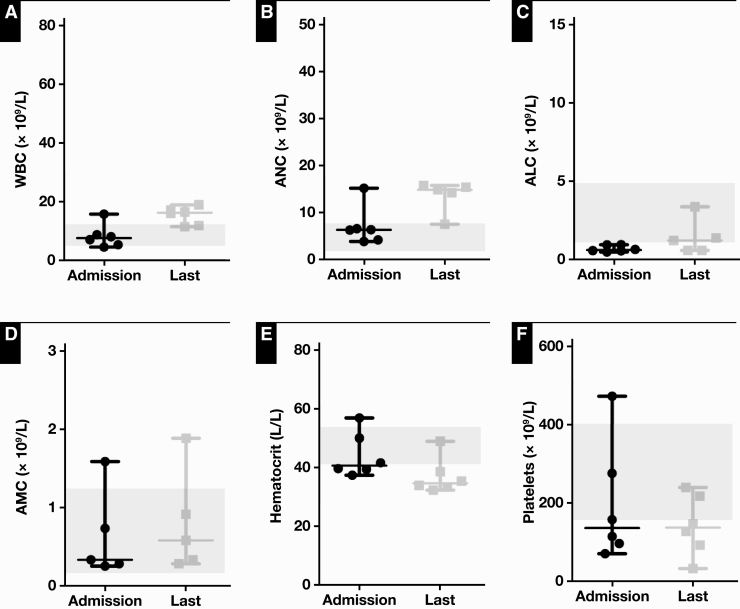
Six patients had bacterial or fungal coinfections during their hospitalization: Klebsiella pneumoniae pneumonia, Staphylococcus aureus pneumonia, Staphylococcus capitis bacteremia, Enterococcus faecalis bacteremia, Escherichia coli urinary tract infection, and cutaneous Candida albicans infection. In addition to positive bacterial or fungal cultures (respiratory and blood cultures for the bacterial infections and wound cultures for the fungal infection), all 6 patients were clinically diagnosed with either a bacterial or fungal coinfection. Among these 6 patients, hematologic abnormalities (summarized in Figure 2) included leukocytosis in 1 patient on admission (WBC count, 4.66-15.80 × 109/L; median, 7.67 × 109/L) and in all 6 patients on their last CBC (WBC count, 11.55-18.96 × 109/L; median, 16.31 × 109/L), elevated neutrophils in 1 patient on admission (ANC, 3.85-15.10 × 109/L; median, 6.32 × 109/L) and in 4 patients on their last CBC (ANC, 3.85-15.68 × 109/L; median, 14.47 × 109/L), lymphopenia in all 6 patients on admission (ALC, 0.48-0.93 × 109/L; median, 0.61 × 109/L) and in 2 patients on their last CBC (ALC, 0.58-3.34 × 109/L; median, 1.2 × 109/L), thrombocytopenia in 3 patients on admission (platelets, 71-472 × 109/L; median, 137 × 109/L) and in 4 patients on their last CBC (platelets, 33-240 × 109/L; median, 138 × 109/L). Of the 5 patients with leukocytosis on admission, 1 patient belonged to the cohort of coinfected patients, whereas the other 4 patients did not have a known coinfection. The 15 patients with leukocytosis on their last CBC included all 6 patients with coinfection and 9 patients without known coinfection. Of the 7 patients with elevated neutrophils on admission, 1 had a known coinfection and 6 did not. Of the 12 patients with elevated neutrophils on their last CBC, 4 had known coinfections and 8 did not. The patient with the highest ANC (34.1 × 109/L) did not have known coinfection. On admission, 11 patients had lymphopenia, which included all 6 patients with coinfection and 5 patients without. On their last CBC, the 5 patients with lymphopenia included 2 with coinfection and 3 without. Finally, the 6 patients with thrombocytopenia on admission included 3 with coinfection and 3 without, whereas the 5 patients with thrombocytopenia on their last CBC included 3 with coinfection and 2 without. Among the cohort with coinfections, between the first and last CBCs, there was a statistically significant increase in WBC count (7.04 × 109/L [95% CI, 2.48-11.61 × 109/L], P = .0107) and reduction in hematocrit (7.08 L/L [95% CI, 0.95-13.21 L/L], P = .0312).
Figure 2.
Hematologic data on admission and last CBC before death for the 6 patients with in-house autopsy and coinfections. Gray bar demonstrates normal range for WBC count (P = .0107) (A), absolute neutrophil count (ANC) (B), absolute lymphocyte count (ALC) (C), absolute monocyte count (AMC) (D), hematocrit (P = .0312) (E), and platelets (F).
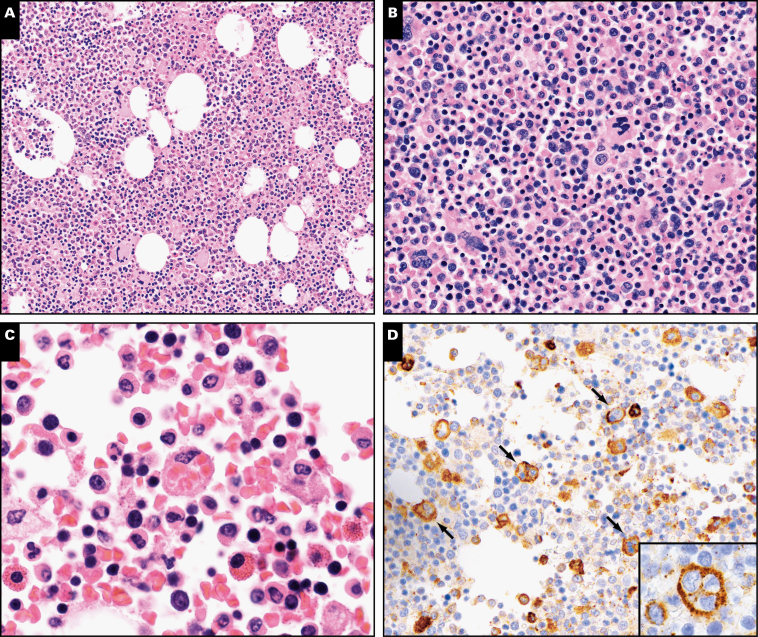
Postmortem histologic examination of the bone marrow revealed normocellular marrow in 8 patients and hypercellular marrow in 12 patients Figure 3. There was complete maturation of myeloid elements, often with a left shift in 13 patients, left-shifted myelopoiesis with a paucity of fully mature elements in 6 patients, and myeloid elements that appeared too sparse to evaluate for maturation in 1 patient. The myeloid-to-erythroid ratio was increased in 11 patients, decreased in 1 patient, and within normal limits in 8 patients. The marrow of 1 patient appeared necrotic, precluding further evaluation. Megakaryocytes were increased in 3 patients, decreased in 3 patients, and appeared to be present in adequate numbers in the remaining cases. The patient with erythrocytosis had a hypercellular marrow (60%) with an apparently normal myeloid-to-erythroid ratio. One patient had lymphoid aggregates with the immunophenotype of CLL (CD20+, CD5+, LEF1+, cyclin D1−) but no peripheral blood lymphocytosis, likely representing monoclonal B lymphocytosis. The patient with CLL had scattered clusters of lymphocytes composed of CD20+ B cells and fewer CD3+ T cells. In general, patients with higher WBC count and ANC in their last CBCs had higher marrow cellularity. Hemophagocytosis, ranging from rare to many scattered cells, was identified histologically on H&E and/or CD68 immunohistochemical stains for all 19 evaluable patients.
Figure 3.
A, Low power shows bone marrow that is hypercellular for age. B, Higher power shows trilineage hematopoiesis with maturing myeloid and erythroid elements, with a leftward shift in myeloid maturation. A large histiocyte with phagocytosis of multiple RBCs is seen at the center of the image (C, oil immersion). An immunostain for CD68 (D) shows scattered hemophagocytic histiocytes (arrows); the inset shows 1 hemophagocytic histiocyte with engulfed leukocytes (oil immersion).
In all cases, the hemophagocytic histiocytes were scattered in a background of hematopoietic elements. The hemophagocytic histiocytes did not form aggregates or replace zones of the marrow. The scattered histiocytes primarily demonstrated engulfed erythrocytes and occasional engulfed leukocytes (Figure 3).
Among the 20 patients, 17 had data for at least 4 of the 9 established criteria for HScore calculation. HScore ranged from 0 to 269 (median, 118). For patients with data for at least 7 of the 9 criteria, the median HScore was 125 (Table 3). Five patients had an HScore higher than 169.
Bone marrow of the 10 deceased patients who tested negative for COVID-19 was examined. The cohort consisted of 6 men and 4 women, with an age range of 48 to 84 years (median, 66 years). There were 7 White non-Hispanic patients and 3 Hispanic patients. The cohort showed the following comorbidities: 60% with hypertension, 40% with diabetes, 10% with asthma, and 10% with immunosuppression (renal transplant). The BMIs ranged from 19.0 to 31.6 (median, 26.3); 1 of the 10 patients was obese. The causes of death included infection in 40%, malignancy in 20%, cerebrovascular accident in 20%, cardiac arrythmia in 10%, and cardiogenic shock in 10%. Examination of the bone marrow revealed 3 instances of hemophagocytosis. Hemophagocytosis was identified in the bone marrow of a patient who died of cardiogenic shock following a protracted course in the intensive care unit (ICU) after open-heart surgery. In addition to hemophagocytosis, this patient’s bone marrow showed extensive hemorrhage. Rare hemophagocytosis was identified in a patient who died of multifocal cerebral infarction secondary to emboli following a recent coronary artery bypass grafting surgery. The third patient with identified hemophagocytosis died of a hemorrhagic cerebrovascular accident; however, review of the patient’s outpatient records revealed that there was a clinical suspicion of HLH, and the patient was undergoing further workup at time of death. This patient’s HScore was 195. There was a statistically significant difference in the finding of hemophagocytosis between the COVID-19–positive and COVID-19–negative cohorts (P < .0001).
Bone marrow of 2 living patients who tested positive for COVID-19 was examined. The first patient was a 48-year-old man with diabetes mellitus type 2 and hypertension who underwent below-the-knee amputation for osteomyelitis. CBC showed anemia. Marrow from the amputation specimen showed trilineage hematopoiesis with slightly left-shifted myelopoiesis but no apparent hemophagocytosis. The HScore was 19. The second patient was a 63-year-old man with a pericardial effusion who underwent excision of a portion of pericardium, evacuation of a clot from the pericardial cavity, and removal of a portion of the xiphoid process. His CBC was remarkable for a neutrophilic leukocytosis that resolved and for anemia. The marrow showed maturing trilineage hematopoiesis with a few hemophagocytic histiocytes highlighted by an immunohistochemical stain for CD68.
Discussion
In this study of the first 20 consecutive patients who died of COVID-19 and had a postmortem examination performed at our institution, there was a high prevalence of comorbidities that have been associated with poor outcome, including hypertension, diabetes mellitus, and obesity.5,13-15 Common hematologic abnormalities included neutrophilic leukocytosis, lymphopenia, anemia, and thrombocytopenia; the anemia and thrombocytopenia were mild in most cases. Lymphopenia is commonly associated with COVID-19,16-19 with more pronounced lymphopenia associated with more severe COVID-19 disease.14,15,19,20 The lymphopenia may be secondary to the cytokine storm induced by SARS-CoV-2. In addition, lymphocytes are reported to express ACE2 receptors on their surface and may become directly infected and killed by SARS-CoV-2.21
Neutrophilic leukocytosis became more prevalent over time so that nearly all (15 of 17) evaluable patients demonstrated an elevated ANC on their last CBC. In this cohort, the increases in both WBC count and ANC between the first and last CBCs were statistically significant. Neutrophilic leukocytosis has been documented previously in association with COVID-19 infection, although it was more common and with more striking elevation of neutrophils in some patients in this series compared with other studies.6,22 In some studies, leukopenia appeared to be more common than neutrophilia, and only a small minority of patients had leukocytosis.4,19,23 Median WBC count and ANC were higher among our deceased patients than in unselected hospitalized patients with COVID-19 at our institution, suggesting that a more pronounced neutrophilic leukocytosis may correlate with worse outcome in patients with COVID-19.6 In several studies from Wuhan and other areas in China, patients with severe COVID-19 disease had a higher WBC count14,16,18 and higher levels of neutrophils14-16,18,20,24 than patients without severe disease, although the WBC counts and ANCs in these studies were often still within the normal range, in contrast to the striking neutrophilia noted in a subset of our patients. In a study from Singapore, no patient had an elevated WBC count on admission, although patients in the ICU tended to develop neutrophilia during hospitalization4; however, their median ANC was lower than that seen in the last CBC of our patients. In 2 studies from Washington State in the United States,17,25 WBC count was higher on average than in most studies from China but still not as pronounced as in some of our patients.24
The cause of elevation of WBC count and ANC in patients with COVID-19 remains uncertain. Bacterial or fungal coinfection may play a role and has been described in a few patients from Wuhan.24 Additional studies have noted that patients with severe COVID-19 infection are more likely to have bacterial coinfections, likely secondary to lowered immune function.26 In our series, 6 patients had bacterial or fungal coinfection that may have contributed to their leukocytosis; nonetheless, the hematologic abnormalities were similar between the coinfected patients and patients without known coinfection in this cohort. Both the overall cohort and the patients with coinfections showed a statistically significant increase in WBC count and reduction in hematocrit, with a significant increase in ANC also noted in the overall cohort but not among the patients with coinfections. All patients without coinfection were monitored closely for signs of bacterial and/or fungal infection during their hospitalizations and received routine (often multiple) blood and urine cultures, all of which showed no growth. No clinical suspicion of coinfection was documented in their electronic medical records. Consequently, although a neutrophilic leukocytosis should prompt a search for superimposed bacterial and/or fungal infections, patients with COVID-19 and no known coinfections can nevertheless develop a pronounced neutrophilic leukocytosis.
As part of the cytokine storm induced by SARS-CoV-2, levels of granulocyte colony-stimulating factor (GCSF) and granulocyte-macrophage colony-stimulating factor are elevated, with more pronounced elevation of GCSF in severely ill patients compared with those with milder disease.18 Differences between our patients and those described in Wuhan, China, and other areas of Asia may be related to various factors, including differences in immune response related to ethnicities or other types of comorbidities. Additional larger and international studies are needed to investigate these factors.
Bone marrow taken at autopsy usually demonstrated trilineage hematopoiesis, sometimes with myeloid hyperplasia and/or a left shift. Similar findings have been reported previously in a few European series.5,13 We identified the presence of hemophagocytosis in all 19 (100%) evaluable autopsy bone marrows, excluding the necrotic bone marrow that was unevaluable. Hemophagocytic histiocytes were scattered throughout hematopoietic elements and did not form aggregates. A similarly high incidence of hemophagocytosis was noted in recent series of 17 and 35 patients with COVID-19 in Spain and the United Kingdom, respectively,5,27 although a series of 4 patients with COVID-19 in North America noted the presence of hemophagocytosis (specifically, lymphophagocytosis) in the lymph nodes and spleen but not in the bone marrow.28 Similar to the recent study from Spain, we identified primarily erythrophagocytosis in the bone marrow.5 Hemophagocytosis of leukocytes was also noted occasionally. The frequent presence of hemophagocytosis, as noted in several prior larger studies,5,27 suggests that COVID-19 can induce an HLH phenotype. Mechanistically, COVID-19 may predispose to HLH through activation of the IL-1/IL-6 pathway, including overproduction of IL-1β by macrophages.9,29 Hemophagocytosis, however, is not a specific finding for HLH.30 Erythrocytosis in particular appears to be more frequently noted in patients with underlying infections, many of whom do not ultimately receive a clinical diagnosis of HLH.30 In our cohort, erythrophagocytosis was the primary form of hemophagocytosis seen, regardless of the patient’s HScore.
Similar to the current findings of hemophagocytosis in patients with COVID-19, previous studies on severe acute respiratory syndrome (SARS) demonstrated variable bone marrow histologic changes.31 Trilineage hematopoiesis without evidence of hypoplastic marrow or HLH was reported in one study.28 Another study documented hemophagocytosis in the lungs of patients infected with SARS but did not examine the bone marrow of these patients,32 whereas hemophagocytosis was identified in the bone marrow of SARS-infected patients in 2 additional studies.33,34
Aberrant inflammatory response has been implicated in the pathogenesis of COVID-19 in several recent studies.9,29 The hyperinflammatory response may take the form of macrophage-activation syndrome, also known as secondary HLH. In one study, patients with clinical findings consistent with HLH were noted to show elevated HScores, which estimate the likelihood of HLH.9,12 Secondary HLH, in contrast to primary/hereditary hemophagocytic syndrome, is a reactive condition that may occur in response to infection, autoimmune diseases, or malignancies.12 Despite the potential importance of HLH as a driver of the proinflammatory cytokine response in some patients with COVID-19, to date there have been few reported analyses of the bone marrow in affected patients.35 A recent study documented the HScores of 8 patients who tested positive for COVID-19 but did not examine their bone marrow.29 Identification of underlying bone marrow alterations in patients with COVID-19 provides important data to support HLH as one of the manifestations of COVID-19 and furthers our understanding of its pathophysiology.
Secondary polycythemia, characterized by erythrocytosis with an elevated erythropoietin level, was noted in one autopsy patient who had a normal CBC documented 4 months previously. Secondary polycythemia can develop in people residing at high altitudes, those with pulmonary disease, and rarely as a paraneoplastic phenomenon. The striking elevation of the hemoglobin and the hematocrit in this patient was unusual and out of proportion to those in hypoxemic patients with lung disease and may represent an unusual manifestation of SARS-CoV-2 infection. Of note, rare patients positive for HIV with polycythemia that eventually resolves, sometimes in response to antiretroviral therapy, have been reported.36,37 To date, there has been only one prior report of (presumed secondary) polycythemia in patients with COVID-19.38
We identified hemophagocytosis in 3 of the 10 bone marrows of patients who tested negative for COVID-19. Two of the patients had had recent cardiac surgeries with protracted ICU courses. In one case, the bone marrow showed extensive hemorrhage. The hemophagocytosis seen may represent a normal response to the hemorrhage. In the third case, there was a clinical suspicion of HLH. The finding of hemophagocytosis in the patient’s bone marrow and an HScore of 195 raise a strong possibility of the diagnosis of HLH. Although the cohort was small, this finding further highlights the striking prevalence of hemophagocytosis in the bone marrow of patients with COVID-19 relative to the typical prevalence of hemophagocytosis in COVID-19–negative autopsies (P < .0001).
This study has several limitations. First, given the nature of a single-institution study with a limited sample size, our estimates of the incidence of peripheral blood abnormalities and hemophagocytosis may not be precise. Second, because this study primarily focused on patients with fatal COVID-19 disease, the incidence of hemophagocytosis in all patients with COVID-19, including those with asymptomatic or mild disease, remains unclear. Nevertheless, our findings are consistent with other reports of worse outcomes among patients with a clinical profile resembling HLH.27 Third, our autopsy cohort examined to date was predominantly White, limiting generalization of these findings to the overall racial and ethnic demographics of the United States or to the national infection and mortality trends.39 Finally, our analysis was based primarily on autopsy material with variable autolysis and degenerative change, which may render optimal evaluation of some histologic features difficult.
In conclusion, we identified a high incidence of neutrophilic leukocytosis, lymphopenia, and hemophagocytosis in patients with fatal COVID-19. We noted the frequent presence of hemophagocytosis in the bone marrow of deceased patients, present in 100% of evaluable bone marrow. Our findings support the burgeoning theory that COVID-19 induces HLH in a subset of patients. Finally, the absence or the presence of only mild hemophagocytosis in 2 bone marrows from living patients with COVID-19 may support the hypothesis that patients with an HLH phenotype experience worse clinical outcomes.
References
- 1. Fauci AS, Lane HC, Redfield RR. Covid-19—navigating the uncharted. N Engl J Med. 2020;382:1268-1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Barton LM, Duval EJ, Stroberg E, et al. COVID-19 autopsies, Oklahoma, USA. Am J Clin Pathol. 2020;153:725-733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fan BE, Chong VCL, Chan SSW, et al. Hematologic parameters in patients with COVID-19 infection. Am J Hematol. 2020;95:E131-E134. [DOI] [PubMed] [Google Scholar]
- 5. Prieto-Perez L, Fortes J, Soto C, et al. Histiocytic hyperplasia with hemophagocytosis and acute alveolar damage in COVID-19 infection. Mod Pathol. 2020:1-8. doi: 10.1038/s41379-020-0613-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sadigh S, Massoth LR, Christensen BB, et al. Peripheral blood morphologic findings in patients with COVID-19. Int J Lab Hematol. 2020;42:e248-e251. [DOI] [PubMed] [Google Scholar]
- 7. Tang N, Li D, Wang X, et al. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844-847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Felsenstein S, Herbert JA, McNamara PS, et al. COVID-19: immunology and treatment options. Clin Immunol. 2020;215:108448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Giamarellos-Bourboulis EJ, Netea MG, Rovina N, et al. Complex immune dysregulation in COVID-19 patients with severe respiratory failure. Cell Host Microbe. 2020;27:992.e3-1000.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hanley B, Lucas SB, Youd E, et al. Autopsy in suspected COVID-19 cases. J Clin Pathol. 2020;73:239-242. [DOI] [PubMed] [Google Scholar]
- 11. Tattoli L, Tsokos M, Sautter J, et al. Postmortem bone marrow analysis in forensic science: study of 73 cases and review of the literature. Forensic Sci Int. 2014;234:72-78. [DOI] [PubMed] [Google Scholar]
- 12. Fardet L, Galicier L, Lambotte O, et al. Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome. Arthritis Rheumatol. 2014;66:2613-2620. [DOI] [PubMed] [Google Scholar]
- 13. Menter T, Haslbauer JD, Nienhold R, et al. Postmortem examination of COVID-19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings in lungs and other organs suggesting vascular dysfunction. Histopathology. 2020;77:198-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934-943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mo P, Xing Y, Xiao Y, et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis. 2020:ciaa270. doi: 10.1093/cid/ciaa270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. JAMA. 2020;323:1612-1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708-1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Qian GQ, Yang NB, Ding F, et al. Epidemiologic and clinical characteristics of 91 hospitalized patients with COVID-19 in Zhejiang, China: a retrospective, multi-centre case series. QJM. 2020;113:474-481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Terpos E, Ntanasis-Stathopoulos I, Elalamy I, et al. Hematological findings and complications of COVID-19. Am J Hematol. 2020;95:834-847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zini G, Bellesi S, Ramundo F, et al. Morphological anomalies of circulating blood cells in COVID-19. Am J Hematol. 2020;95:870-872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wichmann D. Autopsy findings and venous thromboembolism in patients with COVID-19. Ann Intern Med. 2020;173:268-277. [DOI] [PubMed] [Google Scholar]
- 24. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bhatraju PK, Ghassemieh BJ, Nichols M, et al. Covid-19 in critically Ill patients in the Seattle Region—case series. N Engl J Med. 2020;382:2012-2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Liu Y, Du X, Chen J, et al. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J Infect. 2020. doi: 10.1016/j.jinf.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mehta P, McAuley DF, Brown M, et al. ; HLH Across Speciality Collaboration, UK . COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033-1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Prilutskiy A, Kritselis M, Shevtsov A, et al. SARS-CoV-2 infection-associated hemophagocytic lymphohistiocytosis. Am J Clin Pathol. 2020;154:466-474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dimopoulos G, de Mast Q, Markou N, et al. Favorable anakinra responses in severe Covid-19 patients with secondary hemophagocytic lymphohistiocytosis. Cell Host Microbe. 2020;28:117-123.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gars E, Purington N, Scott G, et al. Bone marrow histomorphological criteria can accurately diagnose hemophagocytic lymphohistiocytosis. Haematologica. 2018;103:1635-1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wong RSM, Wu A, To KF, et al. Haematological manifestations in patients with severe acute respiratory syndrome: retrospective analysis. BMJ. 2003:326:1358-1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nicholls JM, Poon LL, Lee KC, et al. Lung pathology of fatal severe acute respiratory syndrome. Lancet. 2003;361:1773-1778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hsueg PR, Chen PJ, Hsiao CH, et al. Patient data, early SARS epidemic, Taiwan. Emerg Infect Dis. 2004;10:489-493. [DOI] [PubMed] [Google Scholar]
- 34. Ng WF, To KF, Lam WW, et al. The comparative pathology of severe acute respiratory syndrome and avian influenza A subtype H5N1—a review. Hum Pathol. 2006;37:381-390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zulfiqar AA, Lorenzo-Villalba N, Hassler P, et al. Immune thrombocytopenic purpura in a patient with Covid-19. N Engl J Med. 2020;382:e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Edwards TB, Nelson RP, Ballester OF, et al. Polycythemia as a complication of human immunodeficiency virus infection. South Med J. 1993;86:686-688. [DOI] [PubMed] [Google Scholar]
- 37. Koduri PR, Sherer R, Teter C. Polycythemia in patients infected with human immunodeficiency virus-1. Am J Hematol. 2000;64:80-81. [DOI] [PubMed] [Google Scholar]
- 38. Khan TA. Polycythemia in SARS-CoV-2 positive patients: an early screening marker. J Coll Physicians Surg Pak. 2020;30:137. [DOI] [PubMed] [Google Scholar]
- 39. Richardson S, Hirsch JS, Narasimhan M, et al. ; Northwell COVID-19 Research Consortium . Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052-2059. [DOI] [PMC free article] [PubMed] [Google Scholar]