Abstract
Background
‘Wish to Die’ (WTD) involves thoughts of or wishes for one’s own death or that one would be better off dead.
Objective
To examine the prevalence, longitudinal course and mortality-risk of WTD in community-dwelling older people.
Design
Observational study with 6-year follow-up.
Setting
The Irish Longitudinal Study on Ageing, a nationally representative cohort of older adults.
Subjects
In total, 8,174 community-dwelling adults aged ≥50 years.
Methods
To define WTD, participants were asked: ‘In the last month, have you felt that you would rather be dead?’ Depressive symptoms were measured using the CES-D. Mortality data were compiled by linking administrative death records to individual-level survey data from the study.
Results
At Wave 1, 3.5% of participants (279/8,174) reported WTD. Both persistent loneliness (OR 5.73 (95% CI 3.41–9.64)) and depressive symptoms (OR 6.12 (95% CI 4.33–8.67)) were independently associated with WTD.
Of participants who first reported WTD at Wave 1 or 2, 72% did not report WTD when reassessed after 2 years, and the prevalence of depressive symptoms (−44%) and loneliness (−19%) was more likely to decline in this group at follow-up.
Fifteen per cent of participants expressing WTD at Wave 1 died during a 6-year follow-up.
Conclusions
WTD amongst community-dwelling older people is frequently transient and is strongly linked with the course of depressive symptoms and loneliness. An enhanced focus on improving access to mental health care and addressing social isolation in older people should therefore be a public health priority, particularly in the current context of the Covid-19 pandemic.
Keywords: Wish to Die, Depression, Loneliness, Death Ideation, Social Isolation, Older people
Key Points
One out of 29 community-dwelling older people reported that during the last month they have felt that they would rather be dead.
Sixty per cent of those with the wish to die also had co-existing depressive symptoms while almost 3/4 reported loneliness.
Seventy-two per cent of these participants no longer reported a wish to die when reassessed 2 years later, however.
Those who no longer reported a wish to die also demonstrated significantly lower levels of depression and loneliness.
One in seven participants who initially reported a wish to die died within the following 6 years.
Background
‘Wish to Die’ (WTD), also known as death ideation or a death wish, involves thoughts of one’s own death, that one would be better off dead, or wishing for one’s death [1].
While later life is generally characterised by emotional well-being and contentment [2], a minority of older people report WTD [3] with higher rates in selected groups, such as those receiving home care services [4] or with a higher burden of chronic disease [5].
WTD is a complex phenomenon. It is defined by international consensus as a reaction to suffering from which the patient can see no way out other than to accelerate his or her death [6]. WTD may mean different things to different individuals, however, and it appears that there are significant sociocultural factors underpinning this [7]. WTD can potentially be due to several factors, many of which are interlinked, including physical symptoms, psychological distress, existential suffering or social deprivation [6].
Assisted dying is the act of deliberately providing medical assistance to another person who wishes to end their own life [8]. Currently, in Ireland, it is illegal to provide such assistance to people with WTD or suicidal ideation. However, a new bill that would legalise assisted dying for those with terminal illnesses, the Dying with Dignity Bill 2020, is due to be considered by lawmakers in Ireland in the coming months.
In order to inform discussion around this complex issue, this report examines the prevalence of WTD in a large population-representative sample of people aged ≥50 years. We specifically examine factors associated with WTD; the longitudinal course of WTD and the relationship between WTD and death.
Methods
This is a longitudinal study examining the baseline prevalence and subsequent longitudinal course of WTD, as well as factors that may influence the persistence of WTD during follow-up. Our hypothesis is that WTD may be transient in a significant number of cases and that the trajectory of symptoms of depression or loneliness would influence whether WTD persists or resolves.
This study is based on data from the Irish Longitudinal Study on Ageing (TILDA), a large population-based study of a nationally representative sample of community-dwelling older adults aged ≥50 years.
TILDA was designed to investigate how the health, social and economic circumstances of the older Irish population interact in the determination of ‘healthy’ ageing. The TILDA study design has been outlined previously [9] but in short; the first wave of data collection (Wave 1, 2009–2011) was conducted using a stratified clustered procedure to randomly sample postal addresses from the Irish Geo-Directory (a listing of all residential addresses in the Republic of Ireland). All postal addresses in Ireland were assigned to one of 3,155 geographic clusters; using RANSAM (a random sampling design for Ireland), a sample of 640 of these clusters was selected stratified by socioeconomic group and geography, where all household residents aged ≥50 years were eligible to participate; Wave 2 was conducted in 2011–2012; Wave 3 was conducted in 2014–2015 and Wave 4 was conducted between 2015 and 2017.
Participants were included in this study if they were aged 50 years or older at Wave 1 and responded to the CAPI question on WTD. Participants were excluded from participation at Wave 1 if they had a pre-existing diagnosis of dementia.
Wish to die
At Wave 1, participants were asked: ‘In the last month, have you felt that you would rather be dead?’ Participants who answered affirmatively were defined as having WTD.
Loneliness
Participants were asked to rate their frequency of loneliness as rarely or never; some of the time; a moderate amount of time or all of the time.
Depressive symptoms
Depressive symptoms were assessed at Waves 1 and 2 using the 20-item Centre for Epidemiological Studies Depression Scale (CES-D), with a score ≥16 was used to define clinically significant depressive symptoms [10].
Mortality
In order to compile mortality data, death records were obtained for TILDA participants and linked to individual-level survey data from the study. Data linkage was performed for all individuals who died between April 2010 and December 2016. The data linkage procedures are reported fully elsewhere [11].
Other measures
Covariates were selected based on prior studies demonstrating a possible association with WTD [5,11,12]. Level of education was recorded as primary level or less, secondary level or tertiary level. Instrumental activities of daily living (IADL) impairment was elicited by asking about the ability to carry out the following tasks: Walking 100 m (100 yards); running or jogging about 1.5 km; Sitting for about 2 h; getting up from a chair after sitting for long periods; climbing several flights of stairs without resting; climbing one flight of stairs without resting; stooping, kneeling or crouching; reaching or extending your arms above shoulder level; pulling or pushing large objects like a living room chair; lifting or carrying weights over 10 pounds/5 kilos, like a heavy bag of groceries; picking up a small coin from a table. Participants were also asked about the presence of pain and to grade pain if present as mild, moderate or severe. Cardiovascular disease was defined as a self-report of angina, congestive cardiac failure or prior myocardial infarction. Self-report was also elicited for the following chronic diseases: eye disease (cataracts, glaucoma or age-related macular degeneration), lung disease, cancer, osteoporosis, liver disease, arthritis, urinary incontinence, Parkinson’s disease and diabetes. Participants were also asked specifically about a prior diagnosis of depression or other psychological/mental illness, as well as the treatment they received for this.
Statistical analysis
All analyses were conducted using Stata/MP 14 (StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015). Baseline characteristics of the study sample were presented descriptively by WTD.
A logistic regression model, reporting odds ratios with 95% confidence intervals (CIs), was used to delineate factors associated with WTD. Covariates were chosen a priori based on their likelihood of association with WTD. Pearson Goodness-of-fit tests were applied to this model.
Kaplan–Meier plots were used to compare survival in those with WTD compared to those who did not report WTD. Data were right-censored at the end of the follow-up period (December 2016). Cox regression was used to ascertain an unadjusted hazard ratio for WTD as a predictor of death during follow-up.
This longitudinal analysis was done in order to clarify the risk of death conferred by endorsing WTD, as well as the cause of death in this context.
Ethics
The TILDA study was approved by the Faculty of Health Sciences Research Ethics Committee at Trinity College Dublin and all participants gave informed written consent. All experimental procedures adhered to the Declaration of Helsinki.
Results
Baseline characteristics
At baseline assessment, almost 3.5% of participants (279/8,174) reported WTD within the last month. The baseline characteristics of this group are summarised in Table 1.
Table 1 .
Baseline characteristics of study sample by Wish to Die
| WTD (n = 279) | No WTD (n = 7,895) | ||
|---|---|---|---|
| Mean age (95% CI), years | 62.3 (61.1–63.5) | 63.9 (63.7–64.1) | t = 2.67; P = 0.0077 |
| Aged 50–64 years (%) | 62 | 57 | |
| Aged 65–74 years (%) | 26 | 27 | |
| Aged ≥75 years (%) | 12 | 17 | X 2 = 4.41; P = 0.110 |
| Female (%) | 59 | 54 | X 2 = 4.22; P = 0.040 |
| Location (%) | |||
| Dublin city or county | 32 | 23 | |
| Another town or city | 30 | 28 | |
| Rural area | 38 | 48 | X 2 = 15.21; P < 0.001 |
| Marital Status (%) | |||
| Married | 56 | 69 | |
| Never married | 9 | 10 | |
| Separated/divorced | 16 | 6 | |
| Widowed | 19 | 14 | X 2 = 52.01; P < 0.001 |
| Educational Attainment (%) | |||
| Primary | 43 | 30 | |
| Secondary | 34 | 40 | |
| Tertiary | 23 | 30 | X 2 = 21.41; P < 0.001 |
| Instrumental ADL impairmenta | |||
| No impairments | 73 | 94 | |
| 1 impairment | 10 | 3 | |
| ≥2 impairments | 17 | 3 | X 2 = 197.50;P < 0.001 |
| Frequency of loneliness (%) | |||
| Rarely or never | 36 | 82 | |
| Some of the time | 25 | 11 | |
| Moderate amount of time | 20 | 5 | |
| All of the time | 19 | 2 | X 2 = 628.08; P < 0.001 |
| Cardiac disease (%)b | 22 | 16 | X 2 = 6.08; P = 0.014 |
| Number of chronic diseases (%)c | |||
| 0 | 35 | 48 | |
| 1 | 23 | 29 | |
| 2–3 | 34 | 20 | |
| ≥4 | 9 | 3 | X 2 = 60.74; P < 0.001 |
| Chronic pain | |||
| No pain | 39 | 65 | |
| Mild pain | 12 | 10 | |
| Moderate pain | 18 | 16 | |
| Severe pain | 30 | 8 | X 2 = 186.30; P < 0.001 |
| Mean CES-D (95% CI) | 20.0 (18.4–21.6) | 5.4 (5.2–5.5) | t = −34.79; P < 0.001 |
| Depressive symptoms (%)d | 60 | 8 | X 2 = 785.08; P < 0.001 |
| Doctor’s diagnosis of depression (%) | 32 | 8 | X 2 = 198.02; P < 0.001 |
aDefined as self-reported number of deficits in the following instrumental activities of daily living: walking 100 m (100 yards); running or jogging about 1.5 km; sitting for about 2 h; getting up from a chair after sitting for long periods; climbing several flights of stairs without resting; climbing one flight of stairs without resting; stooping, kneeling or crouching; reaching or extending your arms above shoulder level; pulling or pushing large objects like a living room chair; lifting or carrying weights over 10 pounds/5 kilos, like a heavy bag of groceries; picking up a small coin from a table.
bDefined as self-report of angina, congestive cardiac failure or prior myocardial infarction.
cBased on the number of the following chronic diseases: eye disease (cataracts, glaucoma or age-related macular degeneration), lung disease, cancer, osteoporosis, liver disease, arthritis, urinary incontinence, Parkinson’s disease and diabetes.
dDefined a score of ≥ 16 on the 20-item CES-D.
There was no significant age difference by mean age or by age category between those who reported and those who did not report WTD. Participants endorsing WTD were more likely to be female, separated or divorced from a spouse and living in rural areas, with lower levels of educational attainment. There were higher rates of heart disease and other chronic diseases in those reporting WTD, as well as higher rates of functional disability and chronic pain. Participants with WTD were also seven times more likely to have current depressive symptoms, and four times more likely to have previously been diagnosed with depression by their doctor.
Table 2 demonstrates that, after adjusting for covariates, the factors independently associated with WTD are age ≥75 years (reduced likelihood), living in a rural area or a town or city other than Dublin, functional disability, chronic pain, higher burden of loneliness and depressive symptoms.
Table 2 .
Logistic regression model with wish to die as dependent variable
| Odds Ratio (95% CI) | z | P-value | |
|---|---|---|---|
| Age Range (Ref: 50–64 years) | |||
| Aged 65–74 years | 0.85 (0.60–1.20) | −0.91 | 0.362 |
| Aged ≥75 years | 0.52 (0.32–0.85) | −2.63 | 0.009 |
| Female sex | 0.78 (0.58–1.05) | −1.65 | 0.099 |
| Location (Ref: Dublin city or county) | |||
| Another town or city | 0.63 (0.44–0.90) | −2.57 | 0.010 |
| Rural area | 0.63 (0.46–0.87) | −2.78 | 0.005 |
| Marital status (Ref: married) | |||
| Never married | 0.79 (0.49–1.27) | −0.97 | 0.332 |
| Separated/Divorced | 1.31 (0.86–2.01) | 1.25 | 0.212 |
| Widowed | 1.01 (0.66–1.53) | 0.03 | 0.973 |
| Educational attainment (Ref: primary) | |||
| Secondary | 0.88 (0.64–1.22) | −0.76 | 0.448 |
| Tertiary | 0.78 (0.54–1.12) | −1.34 | 0.180 |
| Instrumental ADL impairment (Ref: none)a | |||
| 1 impairment | 1.83 (1.12–3.01) | 2.40 | 0.016 |
| ≥ impairments | 2.86 (1.80–4.53) | 4.47 | <0.001 |
| Frequency of loneliness (Ref: rarely/never) | |||
| Some of the time | 2.18 (1.49–3.20) | 4.00 | <0.001 |
| Moderate amount of time | 3.32 (2.15–5.12) | 5.43 | <0.001 |
| All of the time | 5.73 (3.41–9.64) | 6.58 | <0.001 |
| Cardiac diseaseb | 1.28 (0.90–1.83) | 1.37 | 0.170 |
| Number of chronic diseases (Ref: 0)c | |||
| 1 | 0.78 (0.54–1.13) | −1.32 | 0.188 |
| 2–3 | 1.19 (0.82–1.73) | 0.94 | 0.364 |
| ≥4 | 1.03 (0.56–1.88) | 0.09 | 0.932 |
| Chronic pain (Ref: no pain) | |||
| Mild pain | 1.56 (1.02–2.40) | 2.04 | 0.041 |
| Moderate pain | 0.89 (0.60–1.32) | −0.59 | 0.557 |
| Severe pain | 1.82 (1.24–2.69) | 3.03 | 0.002 |
| Depressive symptomsd | 6.12 (4.33–8.67) | 10.22 | <0.001 |
aDefined as self-reported number of deficits in the following instrumental activities of daily living: walking 100 m (100 yards); running or jogging about 1.5 km; sitting for about 2 h; getting up from a chair after sitting for long periods; climbing several flights of stairs without resting; climbing one flight of stairs without resting; stooping, kneeling or crouching; reaching or extending your arms above shoulder level; pulling or pushing large objects like a living room chair; lifting or carrying weights over 10 pounds/5 kilos, like a heavy bag of groceries; picking up a small coin from a table.
bDefined as self-report of angina, congestive cardiac failure or prior myocardial infarction.
cBased on the number of the following chronic diseases: eye disease (cataracts, glaucoma or age-related macular degeneration), lung disease, cancer, osteoporosis, liver disease, arthritis, urinary incontinence, Parkinson’s disease and diabetes.
dDefined a score of ≥ 16 on the 20-item CES-D.
Pearson goodness-of-fit test: Pearson χ2 = 3210.22; P = 0.7000. Ref = reference value.
Wish to die and loneliness
Figure 1 demonstrates the significantly higher burden of loneliness seen in participants with WTD. Almost three-quarters of participants reporting WTD also reported loneliness at least some of the time, while almost one fifth with WTD reported that they were lonely all the time. Almost one-third of participants who felt lonely all the time also endorsed WTD.
Figure 1 .
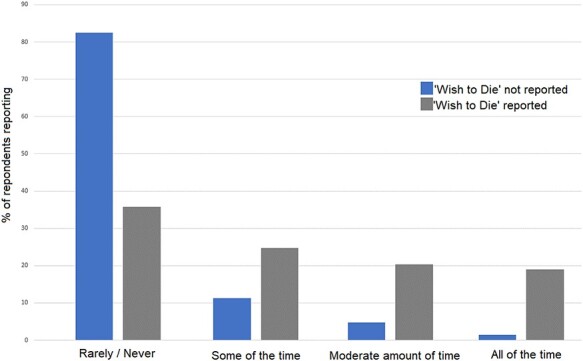
Frequency of loneliness by Wish to Die. Note: participants were asked to rate their frequency of loneliness as rarely or never; some of the time; moderate amount of time or all of the time.
Wish to die and depressive symptoms
Sixty per cent of participants with WTD also met the criteria for clinically significant depressive symptoms, with a CES-D score of ≥16. This was seven times higher than the prevalence of clinically significant depressive symptoms in those who did not report WTD.
Despite this, only 32% of participants with WTD had received a diagnosis of clinical depression by their doctor, indicating possible under-detection of depression within this group. Importantly, less than one-tenth of participants with WTD had received psychological counselling while one-fifth were prescribed antidepressant medication (see Figure 2).
Figure 2 .
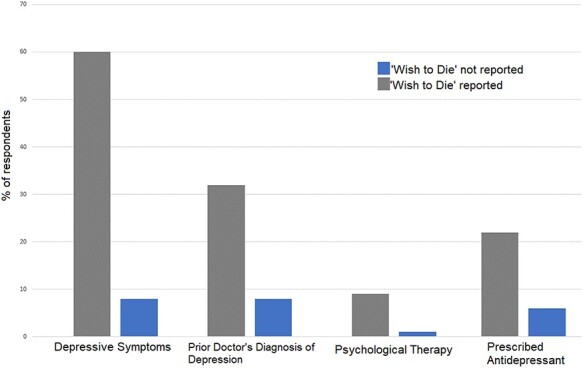
Depressive Symptoms by Wish to Die. Note: depressive symptoms were assessed using 20-item Centre for epidemiological studies depression scale.
Longitudinal course of wish to die
Participants reporting WTD at Wave 1 were reassessed at 2-year intervals up to and including Wave 4, i.e. every 2 years for 6 years.
Of those reporting WTD at Wave 1 (n = 279), 20% (n = 57) were lost to follow-up by Wave 2; 57% (n = 160) no longer reported WTD while 22% (n = 62) continued to report WTD. Of this cohort still reporting WTD (n = 62) at Wave 2, 18% (n = 11) were lost to follow-up by Wave 3; 53% (n = 33) no longer reported WTD at Wave 3, while 29% (n = 18) continued to report WTD. At Wave 4, 28% of those with persisting WTD (n = 5) were lost to follow-up, while one-third no longer reported WTD and 39% continued to report WTD, see Figure 3. One-quarter of those reporting WTD at Wave 1 but not at Wave 2 then re-reported WTD at Wave 3 or 4.
Figure 3 .
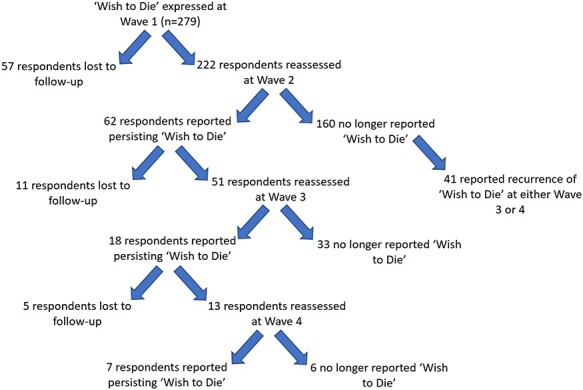
Does wish to die persist? Analysis of participants reporting wish to die at Wave 1. Notes: participants were followed at 2-yearly intervals, i.e. Wave 2 was 2 years after Wave 1 and so on. At each wave, participants were asked: ‘In the last month, have you felt that you would rather be dead?’ Those who answered affirmatively were defined as having wish to die.
A further 175 individuals first reported WTD at Wave 2 having denied WTD at Wave 1. Of these participants, 16% (n = 28) were lost to follow-up at Wave 3; 61% (n = 107) no longer reported WTD at Wave 3, while 23% (n = 40) continued to report WTD at Wave 3. At Wave 4, 20% of those with persisting WTD (n = 8) were lost to follow-up; 43% (n = 17) did not continue to report WTD at Wave 4, while a further 38% (n = 15) reported persisting WTD.
Overall, of the participants who first reported WTD at either Wave 1 or 2, 72% did not report WTD when reassessed after 2 years.
The prevalence of depressive symptoms in those where WTD did not persist from Waves 1 to 2 dropped by almost 44% from Wave 1 to 2, while the prevalence of depressive symptoms in those where WTD persisted dropped by 5%.
Similarly, in those whose WTD ‘resolved’ between Waves 1 and 2 prevalence of self-reported loneliness dropped from 59% to 40% compared to a drop from 81% to 79% in those with a persisting WTD, see Supplementary A1.
Wish to die and death
Fifteen per cent of participants expressing WTD at Wave 1 died during 6-year follow-up, compared to 9% of those who did not report WTD at Wave 1. Supplementary A2 demonstrates differences in survival for those reporting WTD at Wave 1 by censored age. The hazard ratio of WTD for death during follow-up was 1.75 (95% CI 1.27–2.40); likelihood ratio chi-square test = 10.3).
The commonest cause of death in participants reporting WTD was cardiovascular (41%), followed by cancer (17%) and respiratory illness (17%).
Discussion
This study examines the prevalence, predictors and course of WTD in a large population-representative sample of community-dwelling older adults aged ≥50 years.
We found that 3.5% of older adults reported a current WTD. People reporting a WTD were more likely to be female, to live in rural areas, to be separated or divorced from a spouse, to have lower levels of educational attainment, have a functional disability and chronic pain and a higher burden of chronic illness, heart disease, depressive symptoms and loneliness. When analyzed in adjusted models, however, the factors independently associated with WTD were living outside Dublin city or county, impairments in IADLs, chronic pain and current depressive symptoms and loneliness. Chronic disease burden was not associated with WTD in fully adjusted models. Older age (≥75 years) was independently associated with a lower likelihood of wish to die.
Rurup et al. [13] has previously reported that 3.4% of Dutch people aged 58–98 endorsed WTD, while 5% of a community-dwelling French sample of older adults aged 65–96 years [14] and 2% of an Australian sample of community-dwelling people aged ≥70 years [15] reported WTD. Higher rates have been shown in specific cohorts, such as older people attending general practise [5] or in hospital [16]. To our knowledge, this is the first study to ascertain a population-based prevalence of WTD in community-dwelling older adults, however.
WTD appears to be closely linked to loneliness and depressive symptoms. Almost three-quarters of participants with WTD also reported loneliness, while almost one fifth reported that they were lonely all the time. 60% of participants with WTD also had clinically significant depressive symptoms.
Importantly, only half of those with WTD and co-existing depressive symptoms report an established diagnosis of depression. Prior work has highlighted the potential burden of undiagnosed and therefore untreated population with depression within the TILDA cohort [17]. It is not surprising therefore that less than one-sixth of those with WTD and co-existing depressive symptoms have accessed psychological or counselling services given this apparently high rate of undetected depression.
Almost three-quarters of participants first reporting WTD at Wave 1 or 2 denied persisting WTD when questioned at Waves 2 and 3 respectively, indicating that in most cases WTD does not persist. Importantly, in cases where WTD did not persist, participants were significantly more likely to report lower levels of depressive symptoms and loneliness during follow-up also.
Almost 15% of participants reporting WTD at Wave 1 died within the 6-year follow-up period. The commonest cause of death was cardiovascular disease.
There are some limitations to this study that should be noted. WTD was assessed by asking only regarding the last month so excludes people who have had WTD outside this timeframe. Number reporting WTD at Wave 1 is also relatively low. Furthermore, while we discuss the role of mental health, loneliness, pain and functional disability in WTD, it must be emphasised that the WTD is clearly multifactorial and important factors that could not be examined in this study include spiritual factors, cultural aspects, the role of suffering or loss of meaning or the feeling of hopelessness. While the findings from this study suggest that ameliorating depressive symptoms or loneliness may help address death ideation in later life, it is likely that strategies aimed at addressing WTD would need to adopt a multifaceted approach. The strengths of the study include the well-described population-representative sample, with robust longitudinal measures of depressive symptoms, loneliness and mortality.
In conclusion, this study demonstrates that when questioned, 1 in 29 older people report that during the last month they have felt that they would rather be dead. Almost three-quarters of participants with WTD also reported loneliness, while 60% also had clinically significant depressive symptoms. Seventy-two per cent of participants who first report a WTD at either Wave 1 or 2 did not report a WTD when reassessed 2 years later, and in cases where WTD does not persist, loneliness and depressive symptoms improve longitudinally. Other factors that are closely linked with WTD are functional disability and chronic pain.
The timing of these findings greatly increases their importance for two reasons. Firstly, the prevalence data reported here should inform the decision of legislators and practitioners as they consider the Dying with Dignity Bill 2020. This aims to legislate around assisted dying in terminal illness only. This study, accepting cultural differences around this complex issue, is also relevant to other countries where assisted dying may be considered in individuals who report WTD and do not have a specific terminal illness.
It should also be noted, however, that the definition of ‘terminal illness’ in this newly proposed legislation is ‘an incurable and progressive illness which cannot be reversed by treatment, and the person is likely to die as a result of that illness or complications relating thereto’. Almost two-thirds of participants expressing WTD in his study have at least one chronic illness, many of which may be considered incurable but can be managed with appropriate medical therapy.
These data also have important implications for the framework relating to advance directives, as WTD amongst community-dwelling older people may be transient and is strongly linked with the course of depressive symptoms and feelings of loneliness. Depression and loneliness are both remediable, however, with robust international evidence demonstrating improvement with appropriate interventions [18,19,20].
Secondly, due to the COVID-19 pandemic, these decisions are being made at a time of greatly increased prevalence of depression and loneliness among older adults and given the strength of the associations shown here, it is reasonable to expect that the prevalence of WTD will have increased in line with increased depression and loneliness [21,22].
An enhanced focus on improving access to mental health care and addressing social isolation, chronic pain and disability in older people should therefore form an important part of any discussion around WTD and assisted dying in later life, particularly in the current context of Covid-19.
Supplementary Material
Contributor Information
Robert Briggs, Mercers Institute for Successful Ageing, St James’s Hospital, Dublin, Ireland; The Irish Longitudinal Study on Ageing, Trinity College Dublin, Dublin, Ireland; Department of Medical gerontology, Trinity College Dublin, Dublin, Ireland.
Mark Ward, The Irish Longitudinal Study on Ageing, Trinity College Dublin, Dublin, Ireland.
Rose Anne Kenny, Mercers Institute for Successful Ageing, St James’s Hospital, Dublin, Ireland; The Irish Longitudinal Study on Ageing, Trinity College Dublin, Dublin, Ireland; Department of Medical gerontology, Trinity College Dublin, Dublin, Ireland.
Declaration of Conflicts of Interest
None.
Declaration of Sources of Funding
Financial support was provided by Irish Government, the Atlantic Philanthropies and Irish Life plc. These funders were not involved in the study design, collection, analysis and interpretation of data, writing of the paper or submission for publication. Any views expressed in this report are not necessarily those of the Department of Health and Children or of the Minister for Health.
References
- 1. Raue PJ, Morales KH, Post EP, Bogner HR, Have TT, Bruce ML. The wish to die and 5-year mortality in elderly primary care patients. Am J Geriatr Psychiatry 2010; 18: 341–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mather M. The emotion paradox in the aging brain. Ann N Y Acad Sci 2012; 1251: 33–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stolz E, Fux B, Mayerl H, Rásky É, Freidl W. Passive suicide ideation among older adults in Europe: a multilevel regression analysis of individual and societal determinants in 12 countries (SHARE). J Gerontol B Psychol Sci Soc Sci 2016; 71: 947–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. O'Riley AA, Van Orden KA, He H, Richardson TM, Podgorski C, Conwell Y. Suicide and death ideation in older adults obtaining aging services. Am J Geriatr Psychiatry 2014; 22: 614–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kim YA, Bogner HR, Brown GK, Gallo JJ. Chronic medical conditions and wishes to die among older primary care patients. Int J Psychiatry Med 2006; 36: 183–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Balaguer A, Monforte-Royo C, Porta-Sales J et al. An international consensus definition of the wish to hasten death and its related factors. PLoS One 13: e0196754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rodríguez-Prat A, van Leeuwen E. Assumptions and moral understanding of the wish to hasten death: a philosophical review of qualitative studies. Med Health Care Philos 2018; 21: 63–75. [DOI] [PubMed] [Google Scholar]
- 8. NHS Choices . Euthanasia and Assisted Suicide [Internet]. UK; 2016. http://www.nhs.uk/Conditions/Euthanasiaandassistedsuicide/Pages/Introduction.aspx (2 February 2021, date last accessed). [Google Scholar]
- 9. Donoghue OA, McGarrigle CA, Foley M, Fagan A, Meaney J, Kenny RA. Cohort profile update: the Irish longitudinal study on ageing (TILDA). Int J Epidemiol 2018; 47: 1398–1398l. [DOI] [PubMed] [Google Scholar]
- 10. Roberts RE, Vernon SW. The center for epidemiologic studies depression scale: its use in a community sample. Am J Psychiatry 1983; 140: 41–6. [DOI] [PubMed] [Google Scholar]
- 11. Ward M, May P, Briggs R et al. Linking death registration and survey data: procedures and cohort profile for the Irish longitudinal study on ageing. HRB Open Res 2020; 3: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vanderhorst RK, McLaren S. Social relationships as predictors of depression and suicidal ideation in older adults. Aging Ment Health 2005; 9: 517–25. [DOI] [PubMed] [Google Scholar]
- 13. Rurup ML, Deeg DJH, Poppelaars JL, Kerkhof AJFM, Onwuteaka-Philipsen BD. Wishes to die in older people: a quantitative study of prevalence and associated factors. Crisis 2011; 32: 194–203. [DOI] [PubMed] [Google Scholar]
- 14. Bernier S, Lapierre S, Desjardins S. Social interactions among older adults who wish for death. Clin Gerontol 2020; 43: 4–16. [DOI] [PubMed] [Google Scholar]
- 15. Jorm AF, Henderson AS, Scott R, Korten AE, Christensen H, Mackinnon AJ. Factors associated with the wish to die in elderly people. Age Ageing 1995; 24: 389–92. [DOI] [PubMed] [Google Scholar]
- 16. Bornet M-A, Truchard ER, Waeber G et al. Life worth living: cross-sectional study on the prevalence and determinants of the wish to die in elderly patients hospitalized in an internal medicine ward. BMC Geriatr 2020; 20: 348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Briggs R, Tobin K, Kenny RA, Kennelly SP. What is the prevalence of untreated depression and death ideation in older people? Data from the Irish longitudinal study on aging. Int Psychogeriatr 2018; 30: 1393–401. [DOI] [PubMed] [Google Scholar]
- 18. Wilson K, Mottram PG, Sivananthan A, Nightingale A. Antidepressants versus placebo for the depressed elderly. Cochrane Database Syst Rev 2001; 2001: CD000561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jayasekara R, Procter N, Harrison J et al. Cognitive behavioural therapy for older adults with depression: a review. J Ment Health 2015; 24: 168–71. [DOI] [PubMed] [Google Scholar]
- 20. Hagan R, Manktelow R, Taylor BJ, Mallett J. Reducing loneliness amongst older people: a systematic search and narrative review. Aging Ment Health 2014; 18: 683–93. [DOI] [PubMed] [Google Scholar]
- 21. Hwang TJ, Rabheru K, Peisah C, Reichman W, Ikeda M. Loneliness and social isolation during the COVID-19 pandemic. Int Psychogeriatr 2020; 32: 1217–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wu B. Social isolation and loneliness among older adults in the context of COVID-19: a global challenge. Glob Heal Res Policy Global Health Research and Policy 2020; 5: 154–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


