Abstract
Background
Cross-sectional studies have found that the coronavirus disease 2019 (COVID-19) pandemic has negatively affected population-level mental health. Longitudinal studies are necessary to examine trajectories of change in mental health over time and identify sociodemographic groups at risk for persistent distress.
Purpose
To examine the trajectories of mental distress between March 10 and August 4, 2020, a key period during the COVID-19 pandemic.
Methods
Participants included 6,901 adults from the nationally representative Understanding America Study, surveyed at baseline between March 10 and 31, 2020, with nine follow-up assessments between April 1 and August 4, 2020. Mixed-effects logistic regression was used to examine the association between date and self-reported mental distress (measured with the four-item Patient Health Questionnaire) among U.S. adults overall and among sociodemographic subgroups defined by sex, age, race/ethnicity, household structure, federal poverty line, and census region.
Results
Compared to March 11, the odds of mental distress among U.S. adults overall were 1.84 (95% confidence interval [CI] = 1.65–2.07) times higher on April 1 and 1.92 (95% CI = 1.62–2.28) times higher on May 1; by August 1, the odds of mental distress had returned to levels comparable to March 11 (odds ratio [OR] = 0.80, 95% CI = 0.66–0.96). Females experienced a sharper increase in mental distress between March and May compared to males (females: OR = 2.29, 95% CI = 1.85–2.82; males: OR = 1.53, 95% CI = 1.15–2.02).
Conclusions
These findings highlight the trajectory of mental health symptoms during an unprecedented pandemic, including the identification of populations at risk for sustained mental distress.
Keywords: COVID-19, Mental health, Sociodemographic disparities, Psychiatric epidemiology
The prevalence of mental distress among U.S. adults fluctuated between March and August 2020, with a peak observed in mid-April; women experienced a proportionally larger increase in prevalence of mental distress compared to men.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic, declared a national emergency by President Trump on March 13, 2020 [1], has induced unprecedented changes to daily life in the USA. Starting with California on March 19, 2020, stay-at-home orders swept across the nation, eventually covering approximately 95% of the population [2]. Unemployment rates skyrocketed to historical highs of almost 15% in April and remained high throughout the summer [3]. On May 28, 2020, the death toll from COVID-19 surpassed 100,000 deaths and has continued to climb since, with projections of an increased caseload during the fall and winter months [4]. Collectively, these tragic events represent devastating losses to Americans—losses of social connectedness, stable employment, and the lives of family and friends—and are likely to have significant implications for population-level mental health [5–7].
Models of changes in mental distress after disasters, developed based on evidence from natural disasters and other public health crises, suggest that the prevalence of mental distress is likely to fluctuate in the population across the phases of the COVID-19 pandemic [8]. Mental distress refers to distress in response to an external stressor and can be characterized by anxiety, depression, and loneliness; this is different from a psychological disorder (e.g., major depression) that is a pattern of persistent behavioral or psychological symptoms that can influence multiple areas of life [9]. Initial response to an external stressor, such as a pandemic, is often uncertainty and fear followed by panic and shock. Other responses to external stressors can include a honeymoon phase, where an individual might engage in altruistic behaviors and confidence in a return to normal, and a disillusionment phase, where optimism wanes and prolonged stress results in exhaustion [8]. A number of commentaries and reviews have been written about the potential impact of the COVID-19 pandemic on mental distress [6, 7, 10–12]. One study compared the prevalence of symptoms of serious psychological distress between two nationally representative samples of adults and found a higher prevalence of symptoms of serious psychological distress in April 2020 compared to 2018 (13.6% vs. 3.9%) [13]. Similarly, a study comparing the prevalence of depressive symptoms between 2017–2018 and April 2020 in two population-based surveys showed an increase of more than threefold [14]. Another study observed increases in the prevalence of mental distress between March 10 and March 16, 2020, in states with early COVID-19 activity [5]. Finally, a study of three consecutive, nationally representative samples collected between March 18 andApril 18, 2020, observed significant increases in symptoms of acute stress and depression over time [15].
Together, these studies provide important preliminary evidence about how the COVID-19 pandemic may have influenced mental distress. However, longitudinal evidence remains scant; the existing literature is limited to the early months of the pandemic or focuses only on high-risk populations [16]. It is essential to current and future public health planning to understand how population-level mental distress has changed over time and if there are sociodemographic subgroups that may be at high risk of mental distress. Indeed, the negative ramifications of the COVID-19 pandemic, including caseload, mortality, and loss of employment, has disproportionately affected racial/ethnic minorities, low-income adults, young adults, and women, which may, in turn, translate to greater mental distress [17–19]. To address this need, we conducted a descriptive study of the epidemiology of mental distress over the course of the COVID-19 pandemic. Specifically, our objectives were to (a) examine changes in the prevalence of mental distress from March 10 to August 4, 2020, among U.S. adults and (b) determine if trajectories of mental distress differed between key sociodemographic subgroups. We hypothesized that sociodemographic groups made vulnerable to the negative implications of the COVID-19 pandemic would be more likely to experience adverse patterns of mental distress (i.e., greater relative increases over time and blunted recovery).
Methods
Participants
Participants were drawn from the Understanding America Study (UAS), a probability-based, nationally representative Internet panel of adults (18 years and older) representing the USA. Addresses used to sample participants come from the U.S. Postal Service Delivery Sequence file, prepared by the Marketing Systems Group to form a sampling frame of all household addresses in the USA. The recruitment involves several steps, including prepaid and conditional incentives and several reminders. Potential participants without prior internet access are provided with tablets and broadband internet connections. Once respondents have joined the panel, they are surveyed via computer, mobile device, or tablet. Respondents were compensated with $20 for 30 min of survey time. Informed consent was sought from all participants. UAS panel procedures have been approved by the University of Southern California Institutional Review Board. Additional details regarding the UAS methodology can be found on the UAS website (https://UASdata.usc.edu).
The baseline wave of data collection consisted of a tracking survey fielded on March 10; respondents had until March 31 to complete the survey. Starting on April 1, respondents were invited to participate in biweekly surveys according to a staggered schedule, whereby one fourteenth of the sample was invited every day. Participants who consented to further surveys completed follow-up surveys every 14 days between April 1 and August 4, during which there were nine follow-up surveys administered.
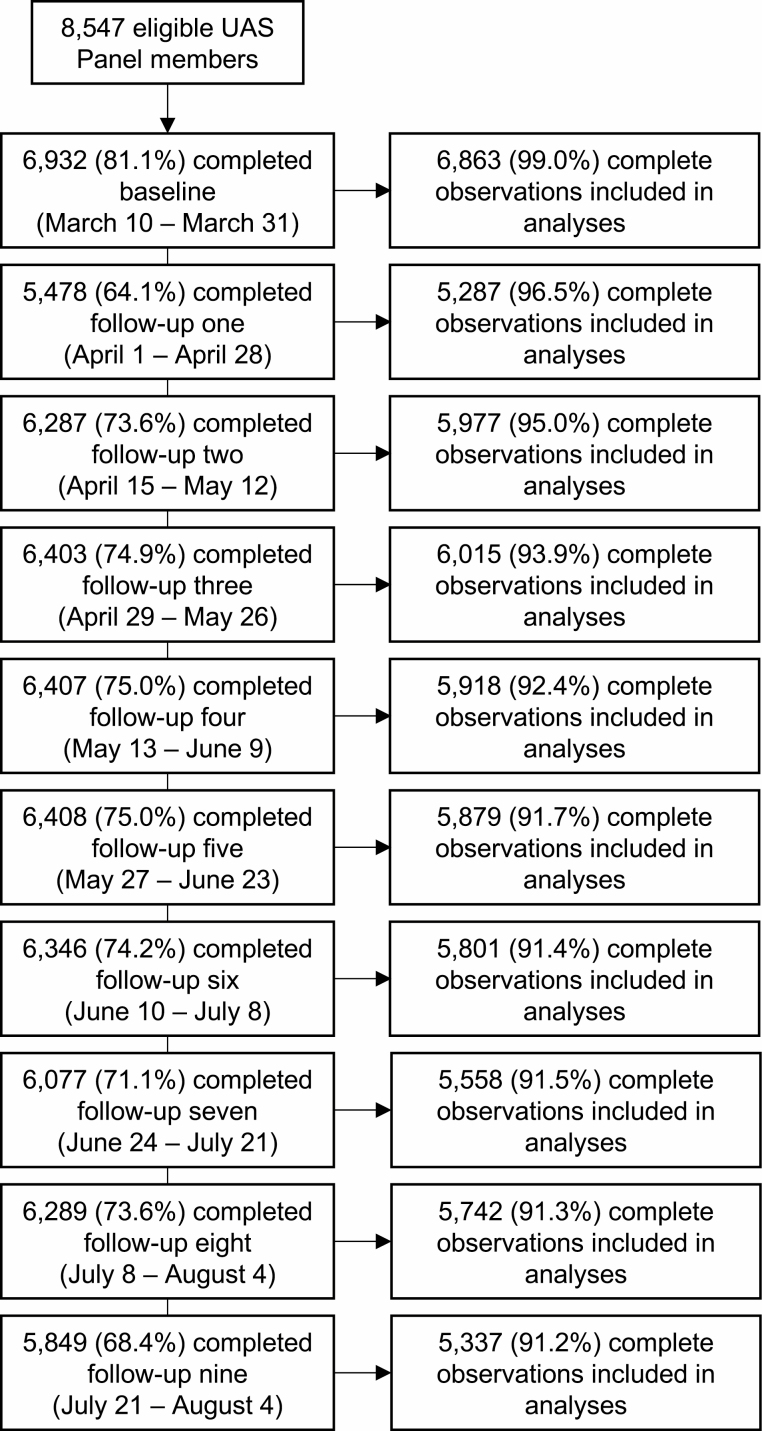
Overall, there were 8,547 eligible panel members. The response rate at baseline was 81.8%, and the average response rate across the nine follow-up surveys was 72.2%. Given the low proportion of missing data across the study period (6.4%), we included only complete cases at each time point in our analyses. Altogether, 6,901 participants were included in our analyses. These participants completed an average of 8.5 out of 10 possible surveys (baseline and nine follow-up surveys). Figure 1 presents the details of participant inclusion, response rates, and the proportion of missing data at each survey. Supplementary Table 1 presents the number of observations per day, and Supplementary Table 2 presents comparisons between participants completing all 10 surveys to those completing 9 or fewer surveys.
Fig. 1.
Participant flow diagram.
Measures
Mental Distress
The outcome of interest was mental distress, measured with the four-item Patient Health Questionnaire (PHQ-4) [20]. The PHQ-4 has been demonstrated to have adequate construct validity and is reliable in the general population [21]. Two items measuring depressive symptoms are drawn from the PHQ-9, and two items measuring anxiety symptoms are drawn from the seven-item Generalized Anxiety Disorder scale [20]. Participants were asked for the frequency over the past 2 weeks with which they had been bothered by “feeling nervous, anxious, or on edge,” “not being able to stop or control worrying,” “feeling down, depressed, or hopeless,” and “little interest or pleasure in doing things.” Scores were obtained by summing the four items (range 0–12), which were classified into categories indicating mental distress severity based on validated cut points (normal [0–2], mild [3–5], moderate [6–8], or severe [9–12]) [20]. We dichotomized these categories into a binary outcome (normal vs. mild/moderate/severe mental distress).
Survey Date
We used survey date as the time scale to assess changes over time. Survey date was entered into each model as a continuous variable representing the number of days since March 10, ending on August 4 (range, 0–147). Given the evidence of nonlinear changes in mental distress over time, we modeled survey date with restricted cubic splines, which generate smoothed curves for longitudinal continuous exposures. Cubic splines capture features that may be missed by traditional techniques, such as linear models or categorization into bins [22]. We generated splines with five knots using the percentiles recommended by Harrell (5, 27.5, 50, 72.5, and 95) [23]. The knots corresponded to the following dates: March 12 (Day 2), April 26 (Day 47), May 27 (Day 78), June 29 (Day 111), and July 29 (Day 141).
Sociodemographic Characteristics
Sociodemographic characteristics were measured at baseline as time-fixed variables. These included age (18–29, 30–49, 50–64, or 65+), sex (female or male), race/ethnicity (monoracial non-Hispanic White, monoracial Non-Hispanic Black, Hispanic/Latino, or other), and state of residence classified according to census regions (Midwest, South, West, and Northeast). We also included an indicator for whether an individual was living in a household above or below the Federal Poverty Line (FPL). Data for household income was recorded in categories; we calculated the median for each category and divided this by the number of individuals reported in the household to estimate the income per household member. This was used to classify individuals as living in a household above or below the poverty line according to the 2020 Federal Poverty Guidelines. We also included a variable reflecting the household structure in which an individual resided. Respondents reported their relationships to other household members and the ages of those members; we used this to classify individuals into five categories of household structure (living alone, living with a partner only, living with a partner and children, living with children only, and other).
Statistical Analysis
Association of date and sociodemographic characteristics with mental distress
We used mixed-effects logistic regression models with a random effect for participants to accommodate repeated measures. Analyses were conducted in three stages. First, we estimated a series of univariate models to examine the association of each sociodemographic characteristic with the prevalence of mental distress across the entire survey period. Second, we estimated a single model with the splines for days since March 10 as covariates to examine the trajectory of mental distress over time among all U.S. adults. Third, we estimated a series of models with interactions between the splines for days since March 10 and each sociodemographic characteristic to determine whether trajectories of mental distress over time differed between sociodemographic subgroups. Wald tests were used to determine whether interactions were significant. The margins and the xbrcspline commands in Stata were used to generate predicted probabilities of mental distress and to estimate odds ratios (ORs) for mental distress on given survey dates compared to March 11, respectively, in the overall sample and stratified by each sociodemographic subgroup [24]. March 11 was used as the reference date instead of March 10 due to a higher number of observations (2,252 vs. 415, respectively).
Sensitivity analyses
We conducted four sets of analyses to test the sensitivity of our results to multivariate adjustment for other sociodemographic characteristics, alternative dichotomizations of PHQ-4 scores, modeling with ordinal logistic regression, and use of survey weights (see Supplementary Material).
Inference
All analyses incorporated survey weights that account for probabilities of sample selection and survey nonresponse and are aligned with Current Population Survey benchmarks. Missing observations due to survey nonresponse were handled with full information maximum likelihood estimation. Statistical significance was assessed at the p < .05 level. Analyses were conducted using Stata version 16 (StataCorp Inc., College Station, TX) and R (R studio version 1.2.5042; R version 4.0.0).
Results
Associations of Sociodemographic Characteristics With the Prevalence of Mental Distress
The sample characteristics and ORs for prevalence of mental distress across the study period are reported in Table 1. The odds of mental distress were higher in female (OR = 4.00; 95% confidence interval [CI] = 3.47–4.61) compared to male respondents; Hispanic/Latino (OR = 1.78; 95% CI = 1.44–2.19) and other race/ethnicity (OR = 1.36; 95% CI = 1.44–2.19) compared to White respondents; adults living alone (OR = 2.81; 95% CI = 2.27–3.48), with a partner and children (OR = 1.82; 95% CI = 1.51–2.20), with children only (OR = 3.96; 95% CI = 2.79–5.61), and in other household structures (OR = 3.75; 95% CI = 3.10–4.55) compared to adults living with a partner only; adults living below the FPL (OR = 4.58; 95% CI = 3.67–5.73), compared to above the FPL; and adults living in the West (OR = 1.79; 95% CI = 1.50–2.13) census region compared to the South census region. The odds of mental distress were lower in older-age groups (30–49: OR = 0.38; 95% CI = 0.29–0.49; 50–64: OR = 0.19; 95% CI = 0.15–0.24; 65+: OR = 0.09; 95% CI = 0.07–0.11) compared to those aged 18–29 and in Black respondents compared to White respondents (OR = 0.56; 95% CI = 0.43–0.71).
Table 1.
Descriptive statistics of sample characteristics for U.S. adults at the first survey wave and associations with mental distress across the survey period (N = 6,901)
| Variable | n (%) | OR (95% CI) |
|---|---|---|
| Sex | ||
| Male | 2,860 (48.3) | ref. |
| Female | 4,041 (51.7) | 4.00 (3.47, 4.61) |
| Age | ||
| 18–29 | 822 (13.2) | ref. |
| 30–49 | 2,546 (40.5) | 0.38 (0.29, 0.49) |
| 50–64 | 2,042 (26.5) | 0.19 (0.15, 0.24) |
| 65+ | 1,491 (19.8) | 0.09 (0.07, 0.11) |
| Race | ||
| White | 4,515 (62.7) | ref. |
| Black | 538 (11.9) | 0.56 (0.43, 0.71) |
| Hispanic/Latino | 1,140 (16.7) | 1.78 (1.44, 2.19) |
| Other | 708 (8.7) | 1.36 (1.06, 1.73) |
| Household structure | ||
| With partner only | 2,030 (27.9) | ref. |
| Alone | 1,170 (16.2) | 2.81 (2.27, 3.48) |
| With partner and kids | 1,637 (24.7) | 1.82 (1.51, 2.20) |
| With kids only | 306 (4.5) | 3.96 (2.79, 5.61) |
| Other | 1,758 (26.6) | 3.75 (3.10, 4.55) |
| Federal poverty line | ||
| Above | 5,992 (83.8) | ref. |
| Below | 909 (16.2) | 4.58 (3.67, 5.73) |
| Census region | ||
| South | 1,778 (38.0) | ref. |
| Midwest | 1,593 (20.7) | 0.94 (0.78, 1.14) |
| Northeast | 725 (17.5) | 1.12 (0.88, 1.41) |
| West | 2,805 (23.8) | 1.79 (1.50, 2.13) |
All percentages are weighted. Bold font indicates statistical significance.
Trajectory of Mental Distress Over Time
ORs for mental distress on given days, compared to March 11, are reported in Table 2. Compared to March 11, the odds of mental distress among U.S. adults overall were 1.84 (95% CI = 1.65–2.07) times higher on April 1, 1.92 (95% CI = 1.62–2.28) times higher on May 1, 0.82 (95% CI = 0.69–0.96) times lower on June 1, 0.83 (95% CI = 0.70–1.00) times lower on July 1, and 0.80 (95% CI = 0.66–0.96) times lower on August 1.
Table 2.
Odds ratios (ORs) for mental distress on different dates in the survey period, compared to March 11, 2020, overall and stratified by sociodemographic characteristics
| Population | Prevalence of mental distress on March 11 (%) | OR for mental distressa, OR (95% CI) | p-value for interactionb | ||||
|---|---|---|---|---|---|---|---|
| April 1 | May 1 | June 1 | July 1 | August 1 | |||
| Overall | 26.1 | 1.84 (1.65, 2.07) | 1.92 (1.62, 2.28) | 0.82 (0.69, 0.96) | 0.83 (0.70, 1.00) | 0.80 (0.66, 0.96) | N/A |
| Sex | |||||||
| Male | 20.3 | 1.69 (1.41, 2.02) | 1.53 (1.15, 2.02) | 0.62 (0.48, 0.82) | 0.74 (0.55, 0.99) | 0.60 (0.44, 0.83) | .014 |
| Female | 30.2 | 1.98 (1.72, 2.28) | 2.29 (1.85, 2.82) | 0.99 (0.82, 1.21) | 0.91 (0.73, 1.14) | 0.97 (0.77, 1.23) | |
| Age | |||||||
| 18–29 | 41.8 | 1.39 (1.01, 1.91) | 1.27 (0.80, 2.03) | 0.58 (0.37, 0.90) | 0.47 (0.28, 0.80) | 0.63 (0.35, 1.13) | .674 |
| 30–49 | 29.2 | 2.09 (1.72, 2.53) | 2.32 (1.74, 3.11) | 0.94 (0.72, 1.23) | 0.99 (0.74, 1.33) | 0.83 (0.61, 1.13) | |
| 50–64 | 24.9 | 1.82 (1.49, 2.21) | 1.84 (1.37, 2.47) | 0.77 (0.57, 1.03) | 0.81 (0.59, 1.11) | 0.78 (0.56, 1.09) | |
| 65+ | 16.2 | 1.82 (1.42, 2.33) | 1.93 (1.33, 2.80) | 0.88 (0.62, 1.26) | 0.94 (0.64, 1.40) | 0.94 (0.62, 1.41) | |
| Race | |||||||
| White | 24.9 | 1.91 (1.67, 2.19) | 1.92 (1.58, 2.35) | 0.75 (0.62, 0.90) | 0.81 (0.66, 1.00) | 0.74 (0.60, 0.92) | .811 |
| Black | 20.1 | 1.39 (0.94, 2.06) | 1.50 (0.85, 2.65) | 0.93 (0.57, 1.53) | 0.73 (0.41, 1.32) | 0.74 (0.40, 1.36) | |
| Hispanic/Latino | 32.1 | 1.93 (1.41, 2.65) | 2.13 (1.31, 3.47) | 0.92 (0.58, 1.45) | 0.92 (0.55, 1.55) | 0.96 (0.54, 1.71) | |
| Other | 29.5 | 1.84 (1.27, 2.65) | 2.12 (1.17, 3.86) | 1.03 (0.52, 2.05) | 0.92 (0.47, 1.81) | 0.96 (0.46, 1.99) | |
| Household structure | |||||||
| With partner only | 21.1 | 1.76 (1.42, 2.17) | 1.83 (1.33, 2.51) | 0.84 (0.61, 1.14) | 0.88 (0.62, 1.23) | 0.93 (0.64, 1.33) | .589 |
| Alone | 26.4 | 1.59 (1.23, 2.07) | 1.58 (1.08, 2.32) | 0.80 (0.55, 1.16) | 0.86 (0.58, 1.26) | 0.78 (0.51, 1.19) | |
| With partner and kids | 25.4 | 2.04 (1.61, 2.59) | 2.02 (1.40, 2.91) | 0.69 (0.49, 0.97) | 0.76 (0.52, 1.10) | 0.72 (0.49, 1.06) | |
| With kids only | 24.1 | 1.92 (1.19, 3.09) | 2.04 (1.00, 4.18) | 0.89 (0.47, 1.67) | 1.03 (0.51, 2.11) | 1.13 (0.50, 2.56) | |
| Other | 33.1 | 1.92 (1.53, 2.42) | 2.17 (1.54, 3.05) | 0.94 (0.68, 1.29) | 0.81 (0.56, 1.18) | 0.70 (0.47, 1.05) | |
| Federal poverty line | |||||||
| Above | 24.1 | 1.93 (1.71, 2.19) | 2.06 (1.71, 2.47) | 0.85 (0.71, 1.01) | 0.87 (0.72, 1.06) | 0.83 (0.67, 1.02) | .496 |
| Below | 39.1 | 1.46 (1.08, 1.97) | 1.39 (0.89, 2.17) | 0.70 (0.46, 1.08) | 0.68 (0.42, 1.08) | 0.67 (0.41, 1.10) | |
| Census region | |||||||
| South | 23.4 | 1.77 (1.46, 2.14) | 1.75 (1.32, 2.32) | 0.72 (0.55, 0.94) | 0.73 (0.54, 1.00) | 0.79 (0.57, 1.11) | .930 |
| Midwest | 25.7 | 1.87 (1.51, 2.33) | 2.02 (1.44, 2.85) | 0.90 (0.64, 1.27) | 0.93 (0.63, 1.36) | 0.87 (0.58, 1.31) | |
| Northeast | 26.7 | 2.02 (1.43, 2.84) | 2.08 (1.25, 3.46) | 0.75 (0.48, 1.17) | 0.73 (0.46, 1.17) | 0.68 (0.40, 1.16) | |
| West | 27.8 | 1.82 (1.51, 2.19) | 1.98 (1.48, 2.65) | 0.95 (0.72, 1.26) | 0.98 (0.72, 1.34) | 0.83 (0.61, 1.14) |
Bold font indicates statistical significance.
aReference is odds of mental distress on March 11, 2020.
bInteraction terms are between the splines for days since March 10, 2020 and each sociodemographic characteristic.
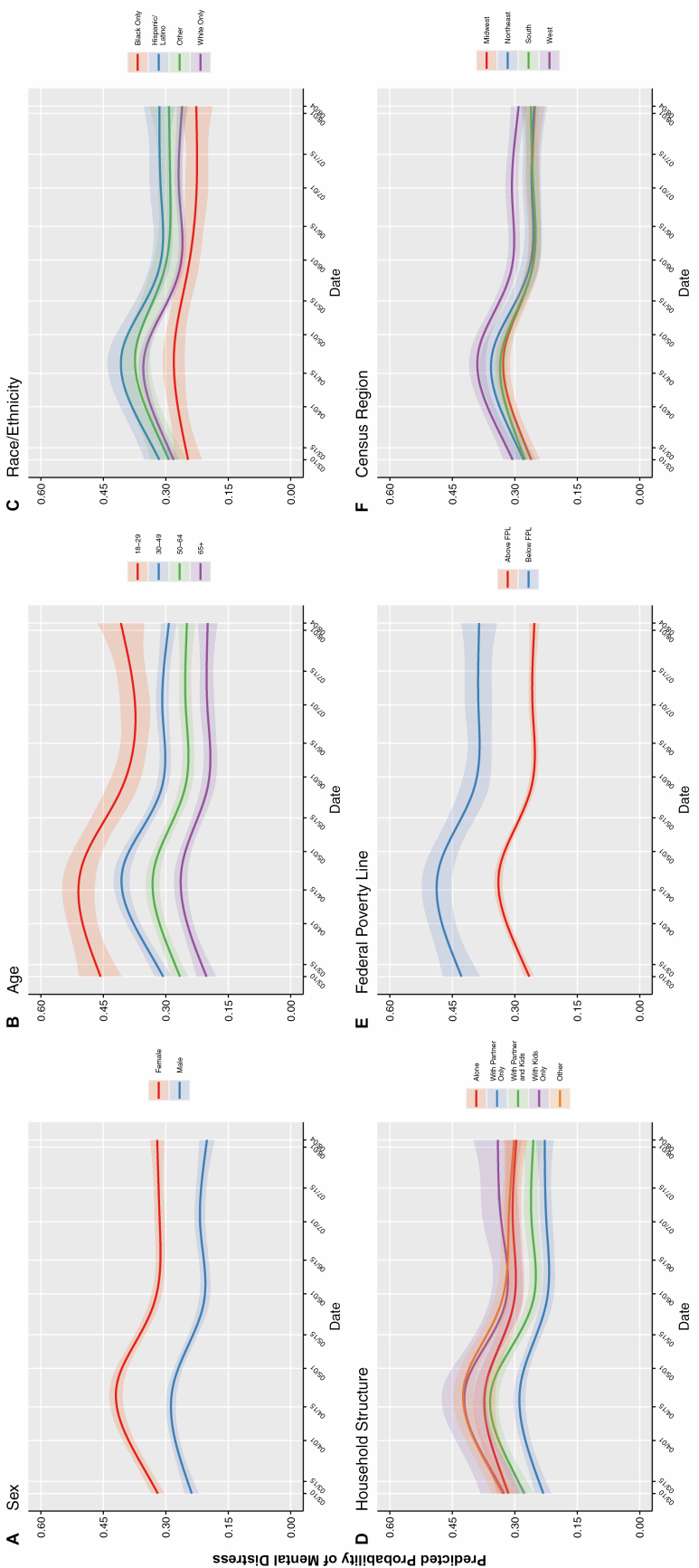
Trajectories of Mental Distress Over Time Among Sociodemographic Subgroups
Predicted probabilities of mental distress and 95% CIs on each day of the survey period, for each sociodemographic subgroup, are displayed in Fig. 2. Interactions between survey date and age, race/ethnicity, household structure, FPL, and census region were not statistically significant. The interaction between survey date and sex was statistically significant, indicating that trajectories of mental distress differed between males and females. Females experienced a sharper increase in mental distress between March and May than males (females: OR = 2.29, 95% CI = 1.85–2.82; males: OR = 1.53, 95% CI = 1.15–2.02), and mental distress declined more precipitously among males than females moving into June (females: OR = 0.99, 95% CI = 0.82–1.21; males: OR = 0.62, 95% CI = 0.48–0.82).
Fig. 2.
Predicted probabilities (bold lines) of self-reported mental distress with 95% confidence intervals (shaded areas) by date of survey completion, stratified by different sociodemographic characteristics, among U.S. adults in the UAS Panel, 2020 (n = 6,901).
Sensitivity Analyses
The results of the sensitivity analyses are described in the Supplementary Material. In analyses with an alternative dichotomization of PHQ-4 scores, the interaction term between the splines for survey date and sex was not statistically significant, suggesting that the movement between the normal and mild categories of mental distress primarily accounted for the differences in trajectories between male and female participants. Otherwise, the pattern of results was broadly consistent with the main analyses.
Discussion
In this study, we examined longitudinal changes in mental distress in a nationally representative sample of U.S. adults between March 10 and August 4, 2020. The prevalence of mental distress appeared to peak in mid-April to early May and declined thereafter. By June 1, the odds of mental distress were comparable to the odds observed on March 11, and this remained the case throughout the remainder of the study period ending on August 4. Across the study period, sociodemographic characteristics associated with a heightened prevalence of mental distress included female sex; younger age; Hispanic/Latino race/ethnicity; living alone, with a partner and children, with children only, or in another household structure; living below the FPL; and living in states in the West census region. Trajectories of mental distress over the four-and-a-half month study period were broadly similar between sociodemographic subgroups. However, differences at some points in the study period were observed between females and males; specifically, females experienced a greater relative increase in mental distress in April and May and a slower decrease thereafter compared to males. Collectively, these findings suggest that public health responses to the COVID-19 pandemic should implement universal and selective approaches to address the needs of both the population at large and specific sociodemographic subgroups.
Sex, age, and race/ethnicity are sociodemographic characteristics that are often associated with mental distress [25, 26]. In the context of the COVID-19 pandemic, another study found that low-income status, Hispanic/Latino ethnicity, and younger age (i.e., 18–29) were associated with serious psychological distress during April 2020 [13]. These sociodemographic differences in mental distress, as well as others observed in our study, are likely to stem from a variety of sources. These include regional differences in COVID-19 activity; a second pandemic of systemic racism [19]; prolonged social isolation [6]; and financial instability. Our study builds on existing findings by examining the trajectories of mental distress over time, extending until the beginning of August 2020. The overall trajectory of mental distress observed in our study population is in line with models of postdisaster mental distress, reflecting an initial increase in mental distress, followed by a honeymoon phase of decreased mental distress and return to normalcy [8]. As the pandemic worsens and extends into the winter, we hypothesize that the disillusionment phase, characterized by mental fatigue and exhaustion, may be imminent [8].
In contrast to the stark disparities observed in the prevalence of mental distress between subgroups, trajectories of change over time were broadly similar between sociodemographic subgroups. The absolute odds of mental distress were approximately four times higher across the study period in females compared to males; additionally, females experienced a greater relative increase in mental distress in April and May compared to males. A possible explanation is that some stressors created by the pandemic, including increased childcare and caregiving responsibilities, are traditionally gendered activities and may have resulted in greater stress among women [27]. Additionally, loss of employment due to the pandemic has disproportionately impacted women, who are more likely than men to be employed in sectors of the economy hit hardest during the pandemic, such as leisure and hospitality [18]. Finally, women make up approximately 78% of the health care workforce in the USA [3]; increased mental distress among health care workers during the pandemic has been widely documented [28] and may have been more prominent among women. Future research should examine whether these sex-related disparities in mental distress have persisted into more recent phases of the pandemic, and how sex relates to transitions between the honeymoon and disillusionment phases of postdisaster mental distress [8].
Based on our findings, we recommend that both universal and selective interventions to support mental health be deployed. Universal interventions are valuable since prior work has shown residual mental distress after the actual pandemic [29] and could prevent the development of longer-term adverse outcomes. Opportunities include equitable access to psychotherapy through state and federally funded mechanisms, evidenced-based public health campaigns to reduce stigma around seeking care, and mental health screening and treatment, particularly in the primary care settings that serve as the locus of care for most U.S. adults. Given high levels of mental distress over time among adults in low-income households, screening and treatment should be priorities in the settings that disproportionately serve low-income adults, such as federally qualified health centers and rural health clinics. Health care financing policy changes may facilitate the integration of mental health treatment into these settings, including enhanced reimbursement for clinicians practicing in primary care medical homes, which has been shown to improve mental illness identification and treatment [30, 31], through the 2015 Medicare Access and CHIP Reauthorization Act and the behavioral health integration billing codes introduced by the Center for Medicare and Medicaid services in 2017 [32–34].
Some limitations related to the content of this study should be noted. We were unable to study all sociodemographic characteristics that may have influenced mental distress during the study period, including time-varying covariates, such as employment status; intersectional identities, such as racial/ethnic minorities living in poverty; and aspects of identity not measured in the UAS, such as sexual or gender identity. In addition, our study results are largely descriptive, and we did not examine prepandemic predictors of trajectories of mental distress, such as lifetime trauma or prior mental disorders. We also did not examine the effect of other historical events that occurred during this period on mental distress, such as the death of George Floyd and the wildfires on the West coast. These will be important objectives for subsequent studies to address.
Other limitations relate to our study design. First, we used measures of mental distress from March 11 as the baseline for comparisons; measures of mental distress were not available in this sample prior to March 10. If increases in mental distress in response to the pandemic had already occurred by this date, our comparisons over time may have been underestimated. Second, although survey dates were randomly assigned at each follow-up wave, they were not randomly assigned for the baseline wave. There may be systematic differences between participants who responded on earlier compared to later dates. Third, there were some sociodemographic differences observed between participants who responded to all surveys compared to those who missed at least one survey, as well as between participants missing data at baseline and those with no missing values. To the extent that participants who missed at least one survey, or were missing data at baseline, differed in their trajectory of mental distress, this may have biased our findings. Fourth, although our survey weights were adjusted for nonresponse at baseline, they were not poststratified to account for nonresponse at each follow-up wave, which may have affected the representativeness of our sample. Fifth, to yield more readily interpretable parameters, we chose to model mental distress as a dichotomous outcome instead of continuously; this may have resulted in some loss of information and variability.
Between March and August 2020, the prevalence of mental distress among U.S. adults increased, peaked in approximately mid-April, and then returned to prepandemic levels. High levels of mental distress were observed in some sociodemographic subgroups, including young adults and those living below the FPL. Interventions and resources to support mental health during the COVID-19 pandemic should be targeted both toward the adult population broadly as well as selectively toward certain sociodemographic subgroups at higher risk. The data presented herein reflect only the first 5 months of the pandemic; it is possible that more recent changes in mental distress have occurred in the meantime, such as exhaustion and fatigue, reflecting the disillusionment phase of models of postdisaster mental distress [8]. It will, therefore, be important to track long-term mental distress and related outcomes as the pandemic continues in the USA and worldwide.
Supplementary Material
Acknowledgments
The authors would like to thank Dr. Elizabeth Colantuoni for her assistance with methodological aspects of the study design. The Understanding America Study is funded from several sources, including the Social Security Administration and the National Institute on Aging under grant 5U01AG054580. The survey that collected the mental health- and COVID-19-related data used in this paper was funded by the Center for Economic and Social Research at the University of Southern California and received substantial support from the Bill and Melinda Gates Foundation. Work on the current manuscript was in part supported by the National Institute of Child Health and Human Development (U54 HD079123). This work was also supported by a RAPID grant from the National Science Foundation (grant number 2028683) and by a Capital Group COVID-19 Response Fund Grant. C.B.V.’s participation in this research was made possible through an National Institute of Health/National Institute on Alcohol Abuse and Alcoholism Ruth Kirschstein Postdoctoral Research Fellowship (F32AA025816). K.E.R. was supported by the National Institute of Mental Health Mental Health Services and Systems Training Program (5T32MH109436-03) and by a Doctoral Foreign Study Award from the Canadian Institutes of Health Research.
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards The authors report no financial relationships with commercial interests. The project described in this paper relies on data from survey(s) administered by the Understanding America Study (UAS), which is maintained by the Center for Economic and Social Research at the University of Southern California (USC). The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of USC or UAS. For any questions or more information about the UAS, contact Tania Gutsche, Project and Panel Manager, Center for Economic and Social Research, University of Southern California, at tgutsche@usc.edu.
Authors’ Contributions Ms. K.E. Riehm, conceptualized and designed the study, carried out data analyses, drafted the initial manuscript, and revised the manuscript. Dr. C. Holingue and Dr. E.A. Stuart conceptualized and designed the study and revised the manuscript. Ms. E. J. Smail assisted with data analyses and reviewing the manuscript. Drs. E. A. Stuart, J. Thrul, F. Kreuter, D. Bennett, and A. Kapteyn designed the survey. Drs. D. Bennett and A. Kapteyn designed and implemented the survey. Drs. D. Bennett, A. Kapteyn, R.M. Johnson, L.G. Kalb, C.B. Veldhuis, M.D. Fallin, F. Kreuter, E.E. McGinty, and J. Thrul assisted with interpreting results and reviewing the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Ethical Approval UAS panel procedures have been approved by the University of Southern California Institutional Review Board.
Informed Consent Informed consent was sought from all participants.
References
- 1. Taylor DB. How the coronavirus pandemic unfolded: A timeline. NY Times. 2020. Available at https://www.nytimes.com/article/coronavirus-timeline.html. Accessibility verified June 30, 2020. [Google Scholar]
- 2. Mervosh S, Lu D, Swales V. See which states and cities have told residents to stay at home. NY Times. 2020. Available at https://www.nytimes.com/interactive/2020/us/coronavirus-stay-at-home-order.html. Accessibility verified June 30, 2020. [Google Scholar]
- 3. Bureau of Labor Statistics, U.S. Department of Labor. The Employment Situation—May 2020. Available at https://www.bls.gov/news.release/pdf/empsit.pdf. Accessibility verified June 30, 2020.
- 4. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Holingue C, Kalb LG, Riehm KE, et al. Mental distress in the United States at the beginning of the 2019 coronavirus disease (COVID-19) pandemic. Am J Public Health. In press. doi: 10.2105/AJPH.2020.305857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Intern Med. Online ahead of print, April 10, 2020. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- 7. Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. Online ahead of print, April 13 2020. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 8. DeWolfe DJ. Training Manual for Mental Health and Human Service Workers in Major Disasters. 2nd ed. HHS Publication No. ADM 90–538. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services. [Google Scholar]
- 9. Horwitz AV. Distinguishing distress from disorder as psychological outcomes of stressful social arrangements. Health. 2007;11(3):273–289. [DOI] [PubMed] [Google Scholar]
- 10. Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. Online ahead of print, May 11, 2020. doi: 10.1001/jama.2020.8598. [DOI] [Google Scholar]
- 11. Otu A, Charles CH, Yaya S. Mental health and psychosocial well-being during the COVID-19 pandemic: The invisible elephant in the room. Int J Ment Health Syst. 2020;14(1):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Holmes EA, O’Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McGinty EE, Presskreischer R, Han H, et al. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. Online ahead of print, June 3, 2020. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ettman CK, Abdalla SM, Cohen GH, et al. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020;3(9):e2019686-e2019686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Holman EA, Thompson RR, Garfin DR, Silver RC. The unfolding COVID-19 pandemic: A probability-based, nationally representative study of mental health in the United States. Sci Adv. 2020;6(42):eabd5390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Karpman M, Zuckerman S, Gonzalez D, et al. The COVID-19 pandemic is straining families’ abilities to afford basic needs. Available at https://www.urban.org/sites/default/files/publication/102124/the-covid-19-pandemic-is-straining-families-abilities-to-afford-basic-needs_2.pdf. Accessibility verified June 30, 2020. [Google Scholar]
- 18. Kochhar R. Hispanic women, immigrants, young adults, those with less education hit hardest by COVID-19 job losses. Available at https://www.pewresearch.org/fact-tank/2020/06/09/hispanic-women-immigrants-young-adults-those-with-less-education-hit-hardest-by-covid-19-job-losses. Accessibility verified June 30, 2020. [Google Scholar]
- 19. Egede LE, Walker RJ. Structural racism, social risk factors, and Covid-19—A dangerous convergence for Black Americans. N Engl J Med. 2020;383(12):e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kroenke K, Spitzer RL, Williams JBW, et al. An ultra-brief screening scale for anxiety and depression: The PHQ–4. Psychosomatics. 2009;50(6):613–621. [DOI] [PubMed] [Google Scholar]
- 21. Löwe B, Wahl I, Rose M, et al. A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122(1):86–95. [DOI] [PubMed] [Google Scholar]
- 22. Gauthier J, Wu QV, Gooley TA. Cubic splines to model relationships between continuous variables and outcomes: a guide for clinicians. Bone Marrow Transplant. 2020;55(4):675–680. [DOI] [PubMed] [Google Scholar]
- 23. Harrell FE, Jr. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. Switzerland: Springer International Publishing; 2015. [Google Scholar]
- 24. Orsini N. XBRCSPLINE: Stata Module to Tabulate Differences in Predicted Responses After Restricted Cubic Spline Models. Statistical Software Components S457092. Boston College Department of Economics; 2019. Available at https://econpapers.repec.org/software/bocbocode/s457092.htm. [Google Scholar]
- 25. Eaton WW, Kalaydjian A, Scharfstein DO, et al. Prevalence and incidence of depressive disorder: The Baltimore ECA follow-up, 1981–2004. Acta Psychiatr Scand. 2007;116(3):182–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Breslau J, Kendler KS, Su M, et al. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychol Med. 2005;35(3):317–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Collins C, Landivar LC, Ruppanner L, et al. COVID-19 and the gender gap in work hours. Gend Work Organ. Online ahead of print, July 2, 2020. doi: 10.1111/gwao.12506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Charney AW, Katz C, Southwick SM, et al. A call to protect the health care workers fighting COVID-19 in the United States. Am J Psychiatry. 2020; doi: 10.1176/appi.ajp.2020.20040535. [DOI] [PubMed] [Google Scholar]
- 29. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395(10227):912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sklar M, Aarons GA, O’Connell M, et al. Mental health recovery in the patient-centered medical home. Am J Public Health. 2015;105(9):1926–1934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Domino ME, Wells R, Morrissey JP. Serving persons with severe mental illness in primary care–based medical homes. Psychiatr Serv. 2015;66(5):477–483. [DOI] [PubMed] [Google Scholar]
- 32. McGinty EE, Daumit GL. Integrating mental health and addiction treatment into general medical care: The role of policy. Psychiatr Serv. Online ahead of print, June 3, 2020. doi: 10.1176/appi.ps.202000183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cross DA, Qin X, Huckfeldt P, et al. Use of Medicare’s behavioral health integration service codes in the first two years: An observational study. J Gen Intern Med. Online ahead of print, December 16, 2019. doi: 10.1007/s11606-019-05579-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Carlo AD, Baden AC, McCarty RL, et al. Early health system experiences with collaborative care (CoCM) billing codes: A qualitative study of leadership and support staff. J Gen Intern Med. 2019;34(10):2150–2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.