Abstract
Importance: Driving is one of the most important instrumental activities of daily living. As adults age, many face challenges with maintaining independent driving, leading to risk for decreased occupational engagement and quality of life. The extent to which occupational therapy services meet the driver rehabilitation needs of older adults is unknown.
Objective: To characterize driver rehabilitation service utilization among a nationally representative sample of community-dwelling older adults.
Design: Exploratory, descriptive cross-sectional study using the National Health and Aging Trends Study 2016 wave.
Participants: Community-dwelling adults age 65 and older who received rehabilitation services in the past year (N = 1,173).
Outcomes and Measures: Sociodemographic information, comorbidities, rehabilitation use, community mobility, and participation restrictions were collected using self-report and performance-based measures.
Results: Of this sample of older adults, 63.0% reported driving as their primary mode of transportation, 25.8% reported limitations in community participation related to transportation, and 9.2% reported having received rehabilitation focused on driving or other transportation goals in the past year. Findings from this study suggest a discrepancy between utilization of driver rehabilitation and self-reported need.
Conclusions and Relevance: Many older adults reported limitations in community participation for transportation-related reasons, yet driver rehabilitation represented only a small proportion of services used. As experts in driver rehabilitation, occupational therapy practitioners should lead the way in advocating for increased utilization of driver rehabilitation and development of innovative, accessible transportation options to promote community mobility and participation among older adults.
What This Article Adds: The results of this study illustrate an important discrepancy between self-reported need for and utilization of driver rehabilitation services. Occupational therapy practitioners can play an important role in meeting older adults’ driving and transportation needs to enable them to fully participate in their community and daily routines.
Driving is the most common means by which older adults carry out their daily routines, social activities, and community participation (Luiu et al., 2017). Limitations in driving ability can have significant implications for older adults’ engagement in social life, daily activities, and overall quality of life (Chihuri et al., 2016). Reasons for driving cessation among older adults have been well documented (Ratnapradipa et al., 2019). Such reasons include not only medical events such as stroke, transient ischemic attack (TIA), or acute injury but also age-related decline in cognitive, physical, visual, and overall function (Bond et al., 2017; Choi et al., 2014; Ryvicker et al., 2020).
Access to reliable transportation is important in enabling independent living and community participation among older adults (Jones et al., 2018). In the event of driving limitation or cessation, many older adults have limited access to alternative formal or informal transportation services that would allow them to successfully complete their daily activities and routines (Choi et al., 2014). The impact of limited community mobility is complex and varies on the basis of individual sociodemographic and environmental factors, but for many older adults transportation-related participation restrictions can lead to significant risk of health and functional decline (Strogatz et al., 2020).
Occupational therapy practitioners are recognized as leading experts in the field of driver rehabilitation (Mielenz et al., 2017). The complex nature of this important instrumental activity of daily living, paired with the growth of the older adult population, offer opportunities for occupational therapy practitioners to play a role in optimizing safe, accessible community mobility and participation for older adults (American Occupational Therapy Association, 2015; Gibbs et al., 2018). Although acknowledgment of the need for increased attention to the community-based needs of the aging population is well documented, a significant gap remains between the extent of this need and the availability of programs and services to support older drivers’ safety and independence goals (Ng et al., 2020; Parisi et al., 2019). The goal of this study was to determine the characteristics of a sample of community-dwelling older adults who received driver rehabilitation services to identify opportunities for occupational therapy practice and development of policy recommendations related to older adults’ community mobility and participation.
Method
Study Design and Participants
To better understand driving-related rehabilitation utilization and need, we conducted a descriptive, cross-sectional study using data from the 2016 wave of the National Health and Aging Trends Study (NHATS). The NHATS is a longitudinal cohort study that tracks late-life function among a national sample of older adults in the United States. The NHATS is run by a multidisciplinary team of investigators at the Johns Hopkins Bloomberg School of Public Health in collaboration with the University of Michigan with data collection by Westat and support from the National Institute on Aging. The NHATS uses the Medicare enrollment database as its sampling frame and a complex survey sampling design to yield a nationally representative cohort of U.S. Medicare beneficiaries age 65 and older in the United States (Kasper & Freedman, 2017).
Data Collection
NHATS data are collected during annual in-person structured interviews using a wide array of validated self-report and performance measures of function (Montaquila et al., 2012). Full information about the NHATS, including survey sample design and validation of measures, can be found at http://www.nhatsdata.org. In 2015, specific rehabilitation items were added to the survey. The current study focuses on community-dwelling older adults because they are the population most likely to use services focused on driver rehabilitation. NHATS respondents were included in this study if they reported being community dwelling (N = 5,930) and receiving any rehabilitation services in the past year. Respondents who reported living in nursing homes or noncommunity settings were excluded from the study. Because the current study involved secondary data analysis of publicly available, deidentified data, study procedures were exempt from the university’s human participants review board.
Variables
Sociodemographics
Participants’ sociodemographic characteristics included self-reported sex, age category (65–69, 70–84, ≥85), race and ethnicity, health, marital status, geographic density (metropolitan or nonmetropolitan area), and living arrangement (alone vs. with others).
Rehabilitation Use
Rehabilitation use was identified using the following item: “Have you received rehabilitation services in the past year?” Those who responded yes answered follow-up questions regarding the underlying medical condition that was the reason for obtaining rehabilitation services, the place services were last received, and the goals of the services. For this study, driving-related rehabilitation use was indicated by a positive response of either “driving” or “using other forms of transportation” to the question “Sometimes rehab focuses on improving ways of moving or getting around. . . . Which of these were you trying to improve?”
Rehabilitation goal attainment was measured by evaluating participants’ responses to two items: “When your rehab services ended, had you met all or most of your goals?” and “Since your rehab services ended, have your functioning and ability to do activities improved, got worse, or stayed about the same?” The complete case approach was used to handle missing data for 11 participants related to the goals of rehabilitation services.
Community Mobility
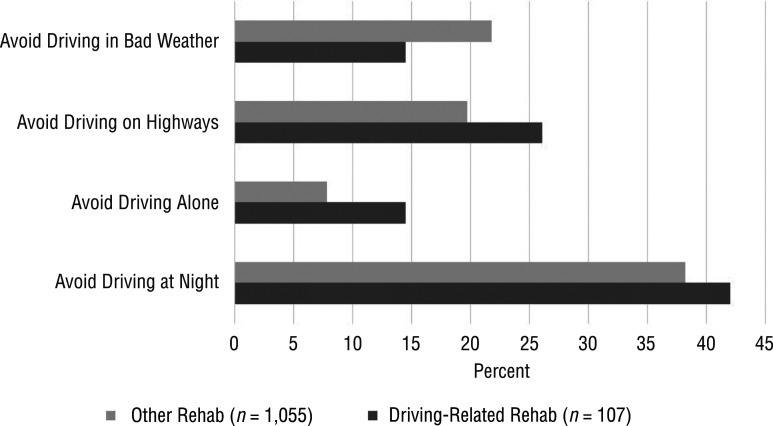
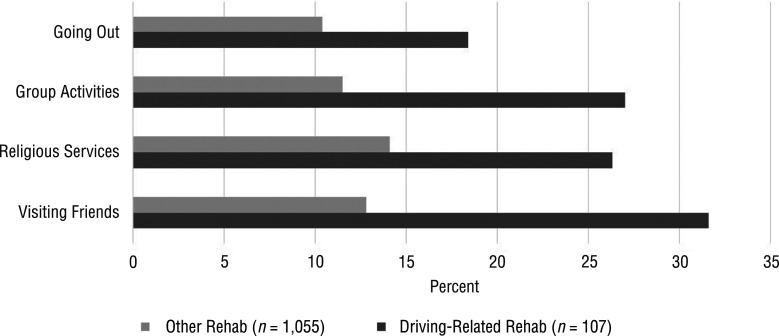
Driving status was measured by self-report of driving in the past year. Community mobility participation restrictions were measured using the participation module of the NHATS survey, which asks respondents whether driving or transportation problems prevented them from participating in activities such as visiting friends or family; attending religious services; participating in clubs, classes, or other organized activities; and going out for enjoyment. Responses to these items were dichotomized (0 = no restriction, 1 = restriction). Driving avoidance behavior was measured similarly by asking respondents whether they avoided driving in bad weather, on highways, alone, or at night, which were recoded as individual dichotomous variables (Huseth-Zosel & Hammer, 2018).
Comorbidities
Underlying medical conditions were self-reported physician diagnoses such as cardiovascular disease, hypertension, diabetes, dementia, or cancer. Any endorsement of a medical condition was coded yes. Likewise, previous hospitalization in the past year was measured as dichotomous yes–no response. General physical function was measured with the Short Physical Performance Battery (Guralnik et al., 1995), a performance-based measure of lower body function, balance, and gait. Self-reported physical activity was assessed with an item asking about engagement in “vigorous activity” in the past year. Mental health was assessed using the Patient Health Questionnaire–4 (Kroenke et al., 2009), a generic screen for depression and anxiety. Perceived health was measured using a single-item rating of overall health on a Likert scale from poor to excellent.
Data Analysis
Given the exploratory design of this study, no formal hypotheses were tested, and data analysis was limited to primarily descriptive techniques (Liamputtong, 2010). Frequency distributions, percentages, cross-tabulations, and graphic displays were used to characterize participants’ need for and use of driver rehabilitation services. Frequency distributions were calculated for sample characteristics, and χ2 and t tests were used to test differences in rehabilitation utilization, demographics, and health variables of interest at the α = .05 significance level. All analyses were performed using SAS Version 9.3 (SAS Institute, Cary, NC).
Results
Among the sample of community-dwelling older adults who had received any rehabilitation services in the past year (N = 1,173), 63.0% reported driving as their primary mode of community mobility, 25.8% reported limitations in community participation for transportation-related reasons, and 9.2% reported having received rehabilitation services focused on driving or transportation-related goals in the past year. Sociodemographic and health characteristics differed little between participants who reported using driver rehabilitation (n = 107) and those who received other transportation-related rehabilitation services (n = 1,055), except for age distribution and history of hospitalization in the past year (data were missing for 11 participants; Table 1).
Table 1.
Sample Characteristics, by Type of Rehabilitation Services Received in the Past Year
| Characteristic | Driving-Related Rehabilitation (N = 107), n (%) | Other Rehabilitation (N = 1,055), n (%) | p |
| Sex | .907 | ||
| Male | 42 (39.3) | 408 (38.7) | |
| Female | 65 (60.7) | 647 (61.3) | |
| Age, yr | .012 | ||
| 65–69 | 18 (16.8) | 105 (10.0) | |
| 70–84 | 72 (67.3) | 671 (63.6) | |
| ≥85 | 17 (15.9) | 279 (26.4) | |
| Race or ethnicity | .129 | ||
| White, non-Hispanic | 69 (66.3) | 785 (75.8) | |
| Black, non-Hispanic | 27 (26.0) | 174 (16.8) | |
| Hispanic | 5 (4.8) | 45 (4.3) | |
| Other, non-Hispanic | 3 (2.9) | 31 (3.0) | |
| Missing | 3 | 20 | |
| Self-rated health | .291 | ||
| Excellent or very good | 25 (23.4) | 323 (30.7) | |
| Fair or good | 71 (66.4) | 633 (60.1) | |
| Poor | 11 (10.3) | 97 (9.2) | |
| Missing | 0 | 2 | |
| Marital status | .522 | ||
| Married or partnered | 56 (52.3) | 535 (50.7) | |
| Divorced, separated, or single | 21 (19.6) | 174 (16.5) | |
| Widowed | 30 (28.0) | 346 (32.8) | |
| Geographic density | .872 | ||
| Metropolitan area | 89 (83.2) | 871 (82.6) | |
| Nonmetro area | 18 (16.8) | 184 (17.4) | |
| Lives alone | 30 (28.0) | 317 (30.0) | .665 |
| Has a chronic condition | 42 (39.3) | 322 (30.5) | .064 |
| Was hospitalized in the past year | 76 (71.0) | 517 (49.0) | <.0001 |
| Engages in routine physical activity | 37 (34.6) | 381 (36.1) | .747 |
| SPPB score,a M ± SD | 7.0 ± 4.2 | 6.9 ± 4.1 | .686 |
| PHQ–4 score,b M ± SD | 2.4 ± 2.7 | 2.3 ± 2.7 | .944 |
Note. PHQ–4 = Patient Health Questionnaire–4; SPPB = Short Physical Performance Battery.
Higher SPPB scores indicate better physical function. Total score ranges from 0 to 12 and is the sum of 3 individual scores: Total Balance, Chair Stand, and Gait Speed.
Higher PHQ–4 scores indicate increased depression and anxiety risk. Total score is the sum of scores on the 4 items; scores are rated as normal (0–2), mild (3–5), moderate (6–8), or severe (9–12).
Of the 107 participants who had used driver rehabilitation services in the past year, most were female (60.8%), White (66.4%), ages 70–84 (67.3%), and living in a metropolitan area (83.2%). Musculoskeletal conditions, including fractures, were the most commonly reported underlying medical conditions (53.0%), with stroke or TIA being the second most common (16.3%). Therapeutic goals focused on driving only for 72.9%, other transportation modes only for 15.9%, and both driving and other transportation modes for 11.2%. Of the 107 participants who had received driving-related rehabilitation services, 39.3% reported that their function had improved when rehab ended, with 28.0% reporting their function improving “a lot”; and 57.0% reported having met their goals when rehab ended.
Figure 1 displays the self-reported driving avoidance behaviors of the older adults who used rehabilitation services in the past year. Given limitations in the sample size and missing data, these findings should be interpreted with caution. However, the figure shows that a significantly higher proportion of driver rehabilitation participants avoided driving alone compared with participants in other rehabilitation programs (p < .05). Differences in the other avoidance behaviors did not meet statistical significance but do indicate patterns of variation in driving avoidance behaviors between these two groups of community-dwelling older adults.
Figure 1.
Driving avoidance behavior, by rehabilitation type.
Figure 2 displays restrictions on participation in activities because of transportation limitations across several domains of activities. In general, participants in driver rehabilitation reported such restrictions more than those in other rehabilitation programs, with significant differences observed for participation in group activities, religious services, and visiting friends.
Figure 2.
Community participation restrictions resulting from transportation limitations, by rehabilitation type.
Discussion
Overall, our findings support the importance of driving and transportation as factors in older adults’ community participation. A substantial proportion of this sample of older adults reported driving as their primary mode of transportation enabling daily activity engagement and independence. Likewise, a notable proportion reported limitations in driving-related function and in participation in various daily activities. This study suggests a potential unmet need for driver rehabilitation services among community-dwelling older adults in that only a small proportion of those who had received rehabilitation services had therapeutic goals directed at community mobility (i.e., driving or other modes of transportation). Among those who engaged in driver rehab, the majority reported improved function and goal attainment at the end of services.
These results indicate a possible underutilization of driving-related rehabilitation services. Previous research has identified barriers to driver rehabilitation services that include cost and lack of reimbursement, lack of program awareness, and lack of access to trained driver rehabilitation specialists (Betz et al., 2014). Challenges related to driver rehabilitation use and accessibility are multifaceted and exist at the individual, community, and societal levels (Jones et al., 2016; Stav, 2012). Addressing such barriers requires collaboration among multiple stakeholders, including occupational therapy educators, policy makers, and local communities, to increase accessibility, knowledge, and sustainability of innovative community mobility rehabilitation programs targeting both driving and alternative modes of transportation.
A salient feature of this study is the two-dimensional conceptualization of community mobility and rehabilitation services as driving, on one hand, and use of other forms of transportation, on the other. This approach is consistent with the literature documenting the importance of not only driving ability but also access to other means of transportation by older adults in their daily activities and routines (Jones et al., 2018; Pristavec, 2018). Future research should focus on ways in which occupational therapy practitioners can offer innovative solutions and increase access to both direct practice interventions and advocacy to improve driving ability and use of other modes of transportation among community-dwelling older adults.
Limitations
Although this study provides insight into an important aspect of driver rehabilitation utilization among older adults, some limitations should be noted. The sample of older adults who had participated in driver rehabilitation in the past year was substantially smaller than the sample who had participated in other rehabilitation programs, making specific analyses of relationships and differences not feasible. Because of missing data for many of the driving-related outcomes, including domains of activity restriction and driving avoidance behavior, the findings should be interpreted as general trends that should be further validated to allow a deeper understanding of the impact of driving limitations on older adults’ driving behaviors and community participation. This study provides valuable insights that aid in understanding and characterizing trends across a national sample of older adults, but this sample may not be fully representative of older adults participating in driver rehabilitation programs. Because this study is cross-sectional and descriptive, the focus was on characterizing the use of driver rehabilitation services.
In terms of variable specificity, the NHATS does not allow for specific exploration of possible differences in driving-related rehabilitation services provided by physical, occupational, and speech therapy professionals because participants were not asked to distinguish the types of rehabilitation services they used. However, given the expertise occupational therapy practitioners have in driver rehabilitation, the findings can be used as evidence with practice and policy implications for the field of occupational therapy. Future work examining longitudinal trends in use are needed to better identify and improve the overall accessibility of driver rehabilitation services. Despite these limitations, this study identified a potential unmet need for driver rehabilitation services among a national sample of community-dwelling older adults.
Implications for Occupational Therapy Practice
The results of this study have the following implications for occupational therapy practice:
Increased awareness is needed by health professionals and key community and policy stakeholders of older adults’ driving- and transportation-related participation restrictions.
Facilitating community-dwelling older adults’ access to driving and other modes of transportation is crucial to support their independence in community mobility and participation.
Occupational therapy practitioners need to actively promote the use of driver rehabilitation services among other health professionals and stakeholders to increase awareness and utilization of these services.
Conclusion
The results of this study illustrate an important discrepancy between utilization of driver rehabilitation services and self-reported need. A large proportion of older adults depend on driving and other modes of transportation to enable them to fully participate in their community and daily routine. Many older adults report limitations in community participation for transportation-related reasons, yet driver rehabilitation represents only a small proportion of rehabilitation services used by this population. As experts in driver rehabilitation and accommodation strategies, occupational therapy practitioners should lead the way in advocating for increased utilization of driver rehabilitation services and development of innovative, accessible community transportation options to improve participation and late-life function among community-dwelling older adults.
Acknowledgments
All contributing authors worked collaboratively on this article. Elizabeth Marfeo was the lead in study design and analysis. Meredith Grinnell contributed to developing conceptual clarity and implications of this work for occupational therapy. Amelia Coffey and Nathan Ward contributed to manuscript preparation, revisions, and final editorial review. There are no conflicts of interest to report.
Contributor Information
Elizabeth Marfeo, Elizabeth Marfeo, PhD, MPH, OT, is Assistant Professor, Department of Occupational Therapy, School of Arts and Sciences, Tufts University, Medford, MA; elizabeth.marfeo@tufts.edu.
Meredith Grinnell, Meredith Grinnell, OTD, CBIS, is Lecturer and Level I Fieldwork Coordinator, Department of Occupational Therapy, School of Arts and Sciences, Tufts University, Medford, MA..
Amelia Coffey, Amelia Coffey, is Student, Department of Mechanical Engineering, Tufts University, Medford, MA..
Nathan Ward, Nathan Ward, PhD, is Assistant Professor, Department of Psychology, School of Arts and Sciences, Tufts University, Medford, MA..
References
- American Occupational Therapy Association. (2015). Evidence-based consensus statements for driving and community mobility. https://www.aota.org/∼/media/Corporate/Files/Practice/Aging/Driving/evidence-based-consensus-statements-driving-community-mobility.pdf
- Betz, M. E., Dickerson, A., Coolman, T., Schold Davis, E., Jones, J., & Schwartz, R. (2014). Driving rehabilitation programs for older drivers in the United States. Occupational Therapy in Health Care , 28, 306–317. 10.3109/07380577.2014.908336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond, E. G., Durbin, L. L., Cisewski, J. A., Qian, M., Guralnik, J. M., Kasper, J. D., & Mielenz, T. J. (2017). Association between baseline frailty and driving status over time: A secondary analysis of the National Health and Aging Trends Study. Injury Epidemiology , 4, 9. 10.1186/s40621-017-0106-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chihuri, S., Mielenz, T. J., DiMaggio, C. J., Betz, M. E., DiGuiseppi, C., Jones, V. C., & Li, G. (2016). Driving cessation and health outcomes in older adults. Journal of the American Geriatrics Society , 64, 332–341. 10.1111/jgs.13931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi, M., Lohman, M. C., & Mezuk, B. (2014). Trajectories of cognitive decline by driving mobility: Evidence from the Health and Retirement Study. International Journal of Geriatric Psychiatry , 29, 447–453. 10.1002/gps.4024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbs, V., Cook, T., & Matteo, M. (2018). Development of a community-based older driver rehabilitation program: What role does occupational therapy play? American Journal of Occupational Therapy , 72, 7211515266. 10.5014/ajot.2018.72S1-PO6021 [DOI] [Google Scholar]
- Guralnik, J. M., Ferrucci, L., Simonsick, E. M., Salive, M. E., & Wallace, R. B. (1995). Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. New England Journal of Medicine , 332, 556–562. 10.1056/NEJM199503023320902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huseth-Zosel, A. L., & Hammer, K. D. (2018). Risky driving behaviors for older adults: Differences by veteran’s status. Journal of Community Health , 43, 827–832. 10.1007/s10900-018-0489-x [DOI] [PubMed] [Google Scholar]
- Jones, J., Dickerson, A., Flaten, H. K., Belmashkan, S., & Betz, M. E. (2016). Driving rehabilitation specialists’ perspectives on older driver evaluations. American Journal of Occupational Therapy , 70, 7002270010. 10.5014/ajot.2016.016915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, V. C., Johnson, R. M., Rebok, G. W., Roth, K. B., Gielen, A., Molnar, L. J., . . . Mielenz, T. (2018). Use of alternative sources of transportation among older adult drivers. Journal of Transport and Health , 10, 284–289. 10.1016/j.jth.2018.07.001 [DOI] [Google Scholar]
- Kasper, J. D., & Freedman, V. A. (2017). National Health and Aging Trends Study (NHATS) user guide: Rounds 1–6 final release. Johns Hopkins University School of Public Health. [Google Scholar]
- Kroenke, K., Spitzer, R. L., Williams, J. B., & Löwe, B. (2009). An ultra-brief screening scale for anxiety and depression: The PHQ–4. Psychosomatics , 50, 613–621. 10.1176/appi.psy.50.6.613 [DOI] [PubMed] [Google Scholar]
- Liamputtong, P. (2010). Research methods in health: Foundations of evidence-based practice. Oxford University Press. [Google Scholar]
- Luiu, C., Tight, M., & Burrow, M. (2017). The unmet travel needs of the older population: A review of the literature. Transport Reviews , 37, 488–506. 10.1080/01441647.2016.1252447 [DOI] [Google Scholar]
- Mielenz, T. J., Durbin, L. L., Cisewski, J. A., Guralnik, J. M., & Li, G. (2017). Select physical performance measures and driving outcomes in older adults. Injury Epidemiology , 4, 14. 10.1186/s40621-017-0110-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montaquila, J., Freedman, V. A., Edwards, B., & Kasper, J. D. (2012). National Health and Aging Trends Study: Round 1 sample design and selection (NHATS Technical Paper No. 1). Johns Hopkins University School of Public Health. [Google Scholar]
- Ng, L. S., Guralnik, J. M., Man, C., DiGuiseppi, C., Strogatz, D., Eby, D. W., . . . Mielenz, T. J. (2020). Association of physical function with driving space and crashes among older adults. Gerontologist , 60, 69–79. 10.1093/geront/gny178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parisi, J. M., Roberts, L., Szanton, S. L., Hodgson, N. A., & Gitlin, L. N. (2019). Valued activities among individuals with and without cognitive impairments: Findings from the National Health and Aging Trends Study. Gerontologist , 57, 309–318. 10.1080/01924788.2018.1521254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pristavec, T. (2018). Social participation in later years: The role of driving mobility. Journals of Gerontology, Series B : Psychological Sciences and Social Sciences, 73, 1457–1469. 10.1093/geronb/gbw057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratnapradipa, K. L., Wang, J., Berg-Weger, M., & Schootman, M. (2019). Effects of older adult driving resumption on all-cause mortality. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75, 2263–2267. 10.1093/geronb/gbz058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryvicker, M., Bollens-Lund, E., & Ornstein, K. A. (2020). Driving status and transportation disadvantage among Medicare beneficiaries. Journal of Applied Gerontology , 39, 935–943. 10.1177/0733464818806834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stav, W. B. (2012). Developing and implementing driving rehabilitation programs: A phenomenological approach. American Journal of Occupational Therapy , 66, e11–e19. 10.5014/ajot.2012.000950 [DOI] [Google Scholar]
- Strogatz, D., Mielenz, T. J., Johnson, A. K., Baker, I. R., Robinson, M., Mebust, S. P., . . . Li, G. (2020). Importance of driving and potential impact of driving cessation for rural and urban older adults. Journal of Rural Health , 36, 88–93. 10.1111/jrh.12369 [DOI] [PubMed] [Google Scholar]