Abstract
Background and Objective
During the COVID-19 pandemic, resources in intensive care units (ICUs) have the potential to be inadequate to treat all those who might benefit. Therefore, it is paramount to identify the views of the community regarding how to allocate such resources. This study aims to quantify Australian community preferences for ventilation allocation.
Methods
A discrete choice experiment was designed and administrated to an adult Australian online panel. Each survey respondent answered 12 choice sets from a total design of 120. Each choice set placed the respondent in the role of hypothetical decision maker, prioritising care between two patients. Conditional logit, mixed logit regression and latent class analysis were used to analyse the data. Additionally, we asked a series of attitudinal questions about different methods of making such decisions in practice, focusing on who should be responsible.
Results
A total of 1050 community members completed the survey and responded to each choice. Dimensions considered most important were age, likely effectiveness, smoking status, whether the person has dependents, whether they are a healthcare worker, and whether they have a disability or not. Estimating marginal rates of substitution between patient characteristics and chance of survival if ventilated yielded values of up to 30 percentage points if the patient was 70 years old relative to being 30. However, respondents typically said they would prefer such decisions to be made by medical professionals.
Conclusion
This study demonstrated the preferences of the community to allocation of ventilators during the COVID-19 pandemic. The use of such information should be treated with some caution as the underlying reason for such preferences are unclear, and respondents themselves preferred the decision to be made by others.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40271-021-00498-z.
Key Points for Decision Makers
| When considering allocation of ventilators during COVID-19, the Australian general public are willing to prioritise groups based on age, likelihood of treatment success, disability, whether the patient has dependents, smoking status, and whether they work in healthcare. |
| However, when asked who should make such decisions, they tend to prefer clinicians to be the final decision makers. |
| There are considerable differences in opinion across the population. So, while the general population may prefer decision making to be made by others, this process has to be informed through a broad set of stakeholders. |
Introduction
Allocation of scarce resources is an ongoing challenge in the healthcare sector. Studies have explored societal values, which may or may not move away from the principle of health maximisation that is typically pursued in Health Technology Assessment [28, 29]. The COVID-19 pandemic has brought questions of resource allocation into particular focus, as demand (or potential demand) for certain kinds of healthcare and health expenditure has increased significantly in a short period of time. One example of this is availability of ventilators in those regions most severely affected by COVID-19, particularly in the intensive care unit (ICU) context. As cases increase in a region, demand can spike beyond what is available, leading to difficult decisions being made around allocation of such resources, often with very real consequences.
While the availability of a ventilator does not guarantee survival for patients with severe COVID-19 (mortality rates for patients requiring mechanical ventilation have been reported to be up to 86%), governments worldwide have scrambled to create pandemic plans to ensure large-scale availability of ICU beds and ventilators [6, 26]. Further, it is unclear where that decision-making burden should fall; it is likely that the default position is for this to fall on individual clinicians, and at a time when they are likely to be facing considerable physical and emotional strain. Of the many recently published reviews and guidelines on frameworks for allocating intensive care resources in COVID-19, very few have included public participation in their creation [7, 10, 20, 34]. More generally, previous work has suggested that the public wanted to be involved in high-level priority setting, but not decisions at the individual level [18].
When making such resource allocation decisions, there have been concerns that some groups might be de-prioritised in terms of access to healthcare resources. One such group is people with disability. It is well established that people with disability experience significant challenges in accessing health services due to discriminatory attitudes and practices [11]. In some countries (e.g. England), initial clinical guidance on ‘triaging’ and rationing access to critical care for all people with COVID-19 recommended use of a frailty index designed to predict outcomes for elderly patients. This meant COVID-19 patients with disability were less likely to get access to critical care such as respiratory support [23, 24]. A high-profile campaign and legal action overturned aspects of these guidelines [5]. However, reports suggest that people requiring assistance with daily living are less likely to receive advanced respiratory support and more likely to die than other groups [14]. There have also been cases where primary care services have issued blanket Do Not Resuscitate (DNR) notices to groups of people with disability without consultation, and where DNRs have been found on the notes of people with disability without consultation [17]. Given that these attitudes had been identified in other settings, we sought to understand whether similar perspectives were held in the Australian context.
Against this background, this paper explores how the general public would choose to allocate ventilators in ICUs if faced with such a decision, and whether they want a say in this process, or prefer for such decisions to be made by other parties (i.e. senior clinicians or health department officials). As context, this research was conducted in mid-2020 in Australia, which at the time was experiencing low infection and mortality rates relative to highly affected countries (including Italy, the United States and China). In those countries, more hard rationing decisions concerning ventilators were being made and there was significant discussion in the medical community and the general public about the potential for the same difficult decisions to be required if the pandemic worsened in Australia. We sought to explore perspectives concerning the question of how to choose who should receive a ventilator, and who should make that choice.
In this paper, we first describe the general method used to elicit preferences, namely the discrete choice experiment (DCE). Second, we outline how this specific choice situation was framed, through definition of appropriate dimensions and levels. Third, we describe survey elements and implementation. Fourth, we describe our analysis techniques. Fifth, we provide results from the survey, and finally, we draw some possible implications for policy and practice in this fraught area of health provision. The intended contribution of the paper is therefore to quantify community preferences for ventilator allocation, and to explore who should be making such decisions in practice.
Methods
Preferences were elicited using a DCE. This is a stated-preference approach that asks respondents to make hypothetical choices between options defined by a series of dimensions, each of which can take one of a finite list of possible levels. Relative to revealed preference approaches, DCEs have both strengths and weaknesses. A key strength is they can be used to ask questions that have not yet been posed, or to gain preferences regarding options that do not yet exist, but may at some point. A key weakness is their hypothetical nature may mean respondents do not reply as they would if actually faced with the task. Despite this, their use in health research has increased considerably over time [31].
In this study, the DCE was presented as a series of forced choice pairwise choices posed to the respondent acting as a hypothetical public decision maker. We chose a forced choice as an opt-out option would be hard to frame, and would not be chosen by the vast majority of respondents. We chose pairwise comparisons to minimise cognitive burden for respondents in what is a challenging and unfamiliar choice context. The task was framed as a prioritisation exercise between two people who both have high medical needs and capacity to benefit from receiving ventilation. To build a DCE it is important to design the dimensions and levels used to describe these hypothetical people in a way that captures key parameters that might drive choice, but also not present options that are implausible, or extremely hard to imagine. We defined our parameters through an iterative process involving the authors and a consumer representative. In this process we first explored the existing literature in a non-systematic way to identify a pool of dimensions that might be relevant to this exercise [21, 24, 30]. Using a set of dimensions that were intended to not overlap (and therefore cause implausible combinations), we then presented the task to a consumer representative, who made suggestions about how we described the task, dimensions and levels. This consumer representative is a male adult embedded in the University (Curtin University, Western Australia), whose role is to help research be better informed by community attitudes. The approach of using a single consumer representative was chosen as it was necessary to generate results quickly to help inform the response to rising demand during the pandemic; therefore, the approach potentially did not provide the optimal set of dimensions and levels that might be developed using gold-standard development methods. In our case, the consumer representative provided guidance about the dimension related to disability status, and we consequently added more information to the level descriptor if the respondent hovered over it. The final dimensions and levels are presented in Table 1; each hypothetical respondent in the choice tasks was one of the 5×5×2×2×3×3×5 (= 4500) combinations of these levels. The number of dimensions reflected a choice, balancing the desire for a range of potential drivers of societal preferences with respondent cognitive burden. The use of seven dimensions is slightly higher than the median in a recent review of DCEs in health, but not considerably higher, and as documented below, our analysis plan allows for identification of relatively more random data [31].
Table 1.
Dimensions and levels
| Dimension | Level 1 | Level 2 | Level 3 | Level 4 | Level 5 |
|---|---|---|---|---|---|
| Age | 30 years | 40 years | 50 years | 60 years | 70 years |
| Chance of survival if ventilated | 30% | 40% | 50% | 60% | 70% |
| Gender | Female | Male | |||
| Smoking status | No | Yes | |||
| Dependents (e.g. children, adults with care needs) | Two or more dependents | One dependent | No dependents | ||
| Healthcare worker | No | Yes, not involved in COVID-19 care | Yes, involved in COVID-19 care | ||
| Disability status | No disability | Mild intellectual disability | Moderate intellectual disability | Mild physical disability | Moderate physical disability |
Under a quality-adjusted life-year (QALY)-type approach, it is interesting to consider which of these are relevant for determining value of treating individuals. Age, chance of survival if ventilated, gender, smoking status and disability status might be considered as impacting on the QALYs that might result from treating a particular individual. However, the spillover dimensions (dependents and whether the person is a healthcare worker) are not typically factored into estimation of QALYs, and hence preferences where these dimensions matter are in contrast with standard cost-utility analysis.
The experimental design was developed in Ngene 1.2.1. The design consisted of 120 choice pairs split into 10 blocks of 12 choice pairs each; the choice of 12 was based on balancing respondent burden with information, and a recent review suggested 12 was typically manageable [31]. Efficiency was based on D-efficiency using the multinomial logit. Small non-zero priors were employed on chance of success, dependents and healthcare workers to reflect our expectation around the signs of coefficients. Simulated random data were used to ensure that the design was able to retrieve zero coefficients. The survey was implemented in Survey Engine, a software designed to house DCEs. Respondents were members of an online panel who had agreed to participate in research projects for a small reimbursement, quota sampled for age and gender. Ethics approval was received from the Curtin University Human Research Ethics Committee (HRE2020-0368).
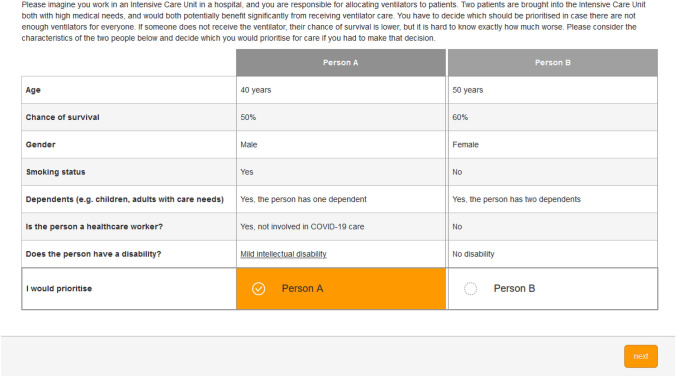
An example choice set is presented in Fig. 1.
Fig 1.
An example choice set
Survey Elements
The survey consisted of the following elements, and is reproduced in full in the electronic supplementary material [ESM]. First, potential respondents were introduced to the general task, flagging that allocation of ventilators might be a major issue if COVID-19 became widespread in the community. Respondents were then given a description of the survey structure and asked if they were willing to participate. If they were, they were asked to provide their age [< 18 (who would be excluded), 18–29, 30–39, 40–49, 50–59, 60–69 and ≥ 70 years] and gender (female, male, would rather not say, and other). Sampling quota on these two variables was used, with the representative number of each combination established based on Australian Bureau of Statistics data, and respondents were excluded if their quota was full. We did not exclude anyone who declined to provide gender, or defined themselves as other. Following this, we provided a walk-through task where sections of a hypothetical choice task were highlighted sequentially with some descriptive text provided. Respondents then completed 12 choice tasks such as the one presented in Fig. 1. They then conducted a prioritisation task, which presented a series of ways of allocating healthcare, and were asked to provide a Likert scale response to each, ranging from ‘strongly support’ to ‘strongly oppose’. These methods for allocating healthcare were adapted from a recent cross-sectional study of public attitudes regarding triage of intensive care patients during an influenza pandemic [4]. These options were (1) using a first come, first served approach to decide; (2) let a senior doctor decide; (3) use a set of criteria or rules that have been determined by the Health Department to decide; (4) use random selection to decide; (5) use a patient’s ability to pay to decide; and (6) use the importance of the patient to decide. Again, each of these had additional explanatory text to help respondents understand their implications, which is provided in the ESM. Respondents then provided the following demographic data: country of birth (Australia, other English-speaking country, other non-English-speaking country); primary language; highest educational achievement; number of children less than 5 years old, between 5 and 18, and older than 18; hours of paid employment pre-COVID-19, and current hours of paid employment; general health; previous admission to an ICU (either personally or in someone close to the respondent); smoking status; whether the respondent considers themselves to have either a physical or intellectual disability; whether they work (or have worked) in the healthcare system; and whether they believe the Australian government has handled the COVID-19 pandemic well or not. Finally, respondents were asked to describe how they answered the DCE tasks, and whether they have any further comments about the survey. On completion, respondents were redirected to the panel, and received a small reimbursement for their time (approximately $5).
We first used a soft launch (in this case, 101 respondents) conducted in July 2020. After these individuals completed the survey, we ran basic conditional logit analysis on the data (described below), and examined the free-text responses to identify any recurrent problematic elements. The analyses suggested respondents were engaged with the task, based on logical ordering of coefficients in the regression model, a reasonable time to complete the survey, and no over-riding concerns in the free-text field. We therefore progressed to full data collection, aiming for a sample of 1000 respondents (although as documented below the final sample exceeded that slightly as the survey host oversampled). This sample size allowed 100 observations per choice pair, which exceeds the rule of thumb described by Lancsar and Louviere [15], and the median number of respondents identified in a recent review by Soekhai et al. [31]. This occurred in August 2020.
Analysis
The DCE data were analysed using three methods. First, we used the conditional logit model. This is the most common approach to analysing DCE data in health [22, 31]. The significant drawback of this approach is that it assumes responses come from a common utility function, which is highly unlikely to be the case here. Thus, we extended the conditional logit in two ways. First, we ran a mixed logit model with all parameters random and uncorrelated. The mixed logit assumes that preferences are represented by a distribution, typically a normal distribution, which can therefore be characterised with a mean and standard deviation. The mixed logit model is used to identify unobserved heterogeneity. This was fitted in STATA 16 using the mixlogit command [13]. In our analyses we used 5000 Halton draws, reflecting recent evidence that the default 50 Halton draws is problematic, and a significantly higher number are needed to achieve robust coefficients [9]. The second extension of the conditional logit was to conduct a latent class analysis. Latent class analysis assumes that there is a distinct number of classes and predicts the probability of respondents belonging to a particular class. Preferences vary across classes but not within each class [12]. Latent class analysis was used to examine the heterogeneity. The latent class model was fitted using the lclogitml2 command in STATA 16 [36]. The optimal number of classes was determined by comparing the Bayesian Information Criterion (BIC) [8]. The characteristics of respondents likely to have preferences aligned with each latent class were explored by estimating multinominal regression models using the ‘mlogit’ command in STATA 16 (StataCorp, College Station, TX, USA [32]). Respondent characteristics were used as the independent variables. The dependent variable was the respondent’s class assignment based on the highest posterior probability from the choice responses. From these multinomial regression models, we report the odds ratio where results are positive and statistically significant at the 5% level.
As the survey was conducted online, there is a risk that respondents rush through the task in a more random way than if an interviewer was collecting responses. To explore this, the data were divided into deciles, and the conditional logit was repeated for each group. The pseudo R2 was collected for each and presented graphically.
Although the design was focused on main effects only, we conducted exploratory analyses on interactions between dimensions. We considered each dimension pair separately, including the two-factor interactions between each.
To assist policy makers, we also estimated marginal rates of substitution (MRS) using chance of survival as the numeraire [16]. In the base-case analysis, we dummy coded each level of this numeraire to allow for non-linearity. For the purpose of estimating MRS, we assumed the relationship across levels was linear, re-estimated the conditional logit model, and divided each other coefficient in the regression by the coefficient on this new linear chance of survival dimension. These results can then be interpreted as the willingness to trade-off survival probability based on the other characteristics of the hypothetical individual.
Results
The analysis included data from 1050 respondents. The characteristics of respondents are provided in Table 2.
Table 2.
Sample characteristics
| Sample characteristic | Sample N = 1050 n (%) |
Population where available, % |
|---|---|---|
| Age | ||
| 18–29 years | 213 (20.3) | 21.7 |
| 30–39 years | 189 (18.0) | 18.6 |
| 40–49 years | 186 (17.7) | 16.6 |
| 50–59 years | 170 (16.2) | 15.6 |
| 60–69 years | 146 (13.9) | 13.3 |
| 70 years and older | 146 (13.9) | 14.2 |
| Gender | ||
| Female | 547 (52.1) | 50.9 |
| Male | 498 (47.4) | 49.1 |
| Would rather not say | 3 (0.3) | |
| Other | 2 (0.2) | |
| Country of birth | ||
| Australia | 780 (74.3) | 64.3 |
| Other, English-speaking | 109 (10.4) | 35.7 |
| Other, non-English speaking | 132 (12.6) | |
| Highest level of education | ||
| Year 11 or below | 112 (10.7) | 24.2 |
| Year 12 (i.e. school completion) | 152 (14.5) | 15.2 |
| Trade certificate | 141 (13.4) | 5.9 |
| Diploma | 151 (14.4) | 15.5 |
| Bachelor’s degree | 305 (29.0) | 15.3 |
| Advanced degree | 154 (14.7) | 6.3 |
| Children aged < 5 years | ||
| None | 886 (84.4) | |
| 1 | 100 (9.5) | |
| 2 | 23 (2.2) | |
| 3 or more | 4 (0.4) | |
| Children aged 5–18 years | ||
| None | 728 (69.3) | |
| 1 | 137 (13.0) | |
| 2 | 129 (12.3) | |
| 3 or more | 20 (1.9) | |
| Children aged 18 years and older | ||
| None | 654 (62.3) | |
| 1 | 105 (10.0) | |
| 2 | 149 (14.2) | |
| 3 or more | 106 (10.1) | |
| General health | ||
| Excellent | 162 (15.4) | 10.4 |
| Very good | 318 (30.3) | 34.6 |
| Good | 362 (34.5) | 36.5 |
| Fair | 148 (14.1) | 14.9 |
| Poor | 22 (2.1) | 3.6 |
| Ever admitted to ICU | ||
| Yes | 199 (19.0) | |
| Someone close admitted to ICU | ||
| Yes | 466 (44.4) | |
| Smoking status | ||
| Current | 188 (17.9) | |
| Former | 223 (21.2) | |
| No | 600 (57.1) | |
| Physical/intellectual disability? | ||
| Yes | 158 (15.0) | |
| Ever worked in healthcare? | ||
| Yes, current | 94 (9.0) | |
| Yes, past | 105 (10.0) | |
| No | 812 (77.3) |
Age and gender data sourced from the Australian Bureau of Statistics. These data only report males and females (i.e. not other). The country of birth data allows estimation from 20 and older rather than 18 and over. Highest level of education and general health both drawn from Household Income and Labour Dynamics in Australia (HILDA) survey Wave 19.
The sample is representative of the general population by age and gender. The sample reports a higher proportion of Australia-born respondents, higher educational levels, and slightly better health than the general population.
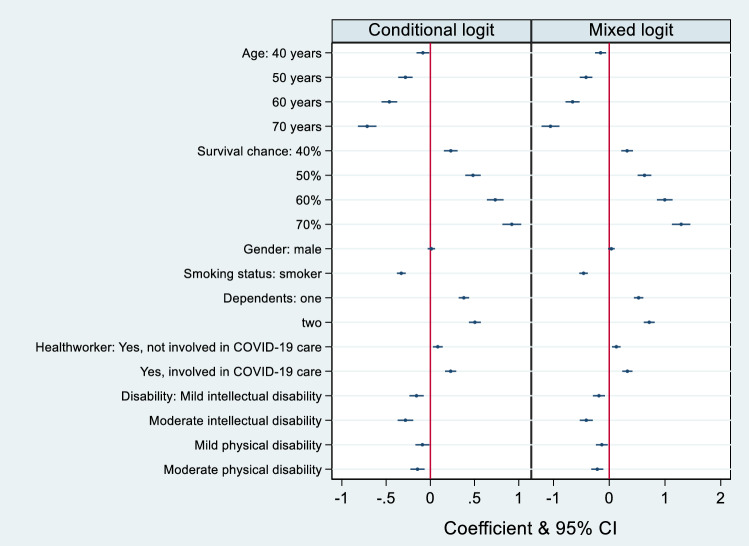
The conditional logit and mixed logit results are presented in the ESM and Table 3, respectively. Both sets of results are reported in Fig. 2.
Table 3.
Conditional and mixed logit results
| Dimension | Level | Model 2: mixed logit Coefficient (SE) |
Standard deviation (SE) |
|---|---|---|---|
| Age (30 years is omitted) | 40 years | − 0.154 (0.050)*** | 0.264 (− 0.149)* |
| 50 years | − 0.415 (0.057)*** | 0.009 (0.014) | |
| 60 years | − 0.657 (0.064)*** | 0.311 (0.133)** | |
| 70 years | − 1.054 (0.082)*** | 1.182 (0.090)*** | |
| Chance of survival if ventilated (30% is omitted) | 40% | 0.321 (0.054)*** | 0.245 (0.163) |
| 50% | 0.633 (0.062)*** | 0.164 (0.177) | |
| 60% | 0.996 (0.071)*** | 0.669 (0.081)*** | |
| 70% | 1.290 (0.084)*** | 1.082 (0.086)*** | |
| Gender (female is omitted) | Male | 0.038 (0.030) | 0.396 (0.071)*** |
| Smoking status (non-smoker is omitted) | Smoker | − 0.461 (0.039)*** | 0.704 (0.055)*** |
| Dependents (none is omitted) | One dependent | 0.527 (0.043)*** | 0.102 (0.099) |
| Two dependents | 0.718 (0.050)*** | 0.539 (0.063)*** | |
| Healthcare worker (non-healthcare worker is omitted) | Healthcare worker, not COVID-19 related | 0.128 (0.039)*** | 0.220 (0.108)** |
| Healthcare worker, COVID-19 related | 0.326 (0.046)*** | 0.728 (0.059)*** | |
| Intellectual disability (no disability is omitted) | Mild intellectual disability | − 0.184 (0.055)*** | 0.135 (0.190) |
| Moderate intellectual disability | − 0.411 (0.060)*** | 0.561 (0.088)*** | |
| Physical disability (no disability is omitted) | Mild physical disability | − 0.133 (0.054)** | 0.028 (0.045) |
| Moderate physical disability | − 0.214 (0.054)*** | 0.081 (0.260) | |
| Log-likelihood | − 7431 | ||
| AIC | 14934 | ||
| BIC | 15227 |
Statistical significance is denoted at the 1% level (***), the 5% level (**) and the 10% level (*)
Fig. 2.
Conditional and mixed logit results
For the conditional logit (reported in Table S1, see ESM), relative to the omitted level of age (30 years), each of the other ages (40, 50, 60, and 70 years) have negative coefficients meaning that the average respondent preferred to allocate the ventilator to the youngest group. Furthermore, the absolute size of the coefficient increased in progressively older age groups, reflecting a clear and monotonic age effect. Independent of age, effectiveness is the strongest predictor of choice in this experiment. Moving from relatively low to high effectiveness also monotonically increased the likelihood of an individual being preferred for ventilator care. Gender was, on average, not considered to be an important parameter in allocating resources (p = 0.56 in the conditional logit). Respondents were willing to prioritise non-smokers over smokers; this may be due to an efficiency or an equity motive, but it is important to note that this is controlling for the effectiveness of the ventilation itself (suggesting that an efficiency argument would likely focus on the life expectancy of the individual, which was not controlled for in the DCE). The typical respondent was willing to distinguish between those who have dependents and those who do not (favouring the former), and also between those who work in the healthcare system (particularly in COVID-19 care) and those who do not. Regarding disability, there was a small but statistically significant preference towards giving ventilation to people without intellectual and physical disabilities. Relative to an individual without these disabilities, all p values were < 0.05, and three of the four were < 0.01. As a robustness check, the analysis was repeated with an alternative specific constant (available on request from the authors); the coefficient on this was small (albeit statistically significant) and had a negligible effect on the other coefficients, so was excluded from the final analysis.
The coefficients on the survival chance dimension are estimated based on dummy-coded levels, but appear to be largely linear (0.231, 0.482, 0.734, 0.921). When the model was re-estimated using a linear term of survival chance, the model fit and other coefficients were, as expected, largely unchanged. The MRS are linear transformations of the coefficients from the regression, and are reported in Table S1 (see ESM).
The exploratory interaction analysis estimated 133 interaction coefficients. Of these, 12 (9%) were statistically significant at the 5% level (results available on request from the authors). The coefficients were difficult to explain and may reflect that the design was not constructed to allow their precise and unbiased estimation; hence these results have to be treated with some caution.
The relationship between completion time decile and pseudo R2 is shown in Fig. 3. The pattern suggested that those who finished quickest were not engaged with the task, and the predictive value of the model in that sub-group was almost zero. In progressively slower deciles, the R2 increases up to the sixth quartile, and then declines beyond the eighth.
Fig. 3.
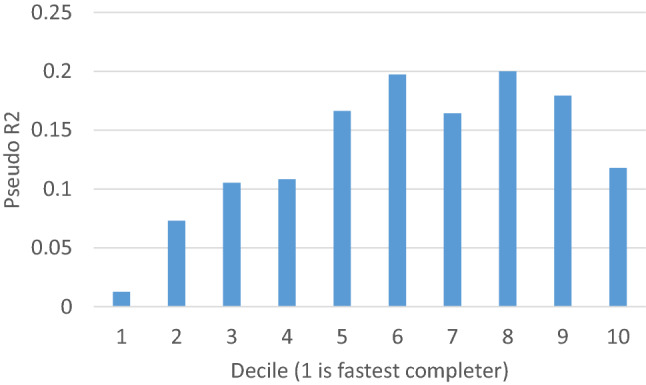
The relationship between completion time and pseudo R2
The mixed logit demonstrated similar patterns in terms of mean response; age and probability of success were considered to be most important, and gender was not statistically significant. It is apparent that there was considerable heterogeneity in preferences among respondents. Of the eighteen standard deviations estimated, seven were statistically significant at the 5% level. The largest standard deviations were seen around the coefficients for the higher age ranges, the highest success probability, smoking status, whether the hypothetical person has no dependents, and whether the hypothetical person is involved in delivering care for COVID-19 patients. This improvement in model fit is reflected in a 273-point improvement in log-likelihood and in both AIC and BIC, suggesting the mixed logit outperforms the conditional logit.
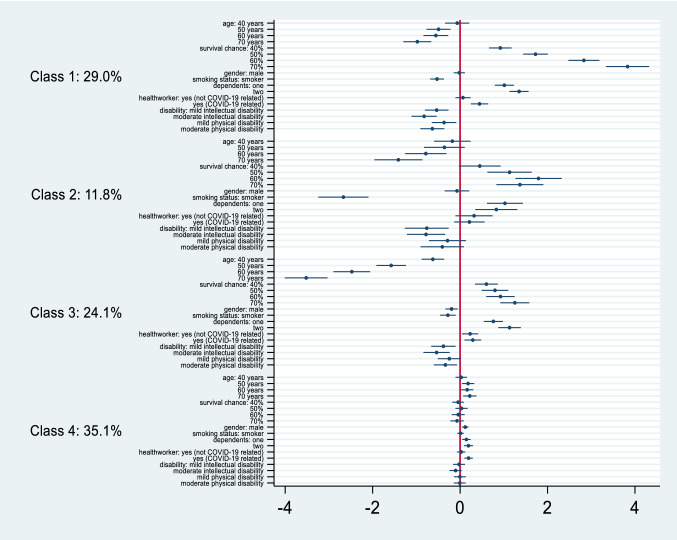
The latent class analysis findings are in Fig. 4, with the coefficients, and accompanying characteristics of people who provided data in each class, reported in the ESM.
Fig. 4.
Latent class analysis
The latent class analysis confirms the heterogeneity observed in the mixed logit. Based on the information criteria for different numbers of latent classes, the optimal number of classes appears to be four. These demonstrate four distinct response approaches. Class 1 (29%) likely included respondents that have the strongest preferences for allocating ventilators to those with a higher chance of survival. Class 2 (12%) likely included respondents with a strong preference against a smoker being allocated a ventilator. Class 3 (24%) have strong preferences against allocating a ventilator as the patient’s age increases. Class 4 (35%) included respondents who did not have strong preferences for the attributes presented. The results from the prioritisation task are reported in Table 4. There is strong support to have the decision around allocation of ventilators be made by either a senior doctor or the Department of Health. Conversely, ability to pay and random selection were not supported in our cohort.
Table 4.
Prioritisation task findings
| Statement | Strong support | Support | Neither support nor oppose | Oppose | Strongly oppose |
|---|---|---|---|---|---|
| Use a first come, first served approach to decide | 112 (10.8) | 302 (29.2) | 374 (36.1) | 175 (16.9) | 72 (7.0) |
| Let a senior doctor decide | 249 (24.1) | 506 (48.9) | 200 (19.3) | 57 (5.5) | 23 (2.2) |
| Use a set of criteria or rules that have been determined by the Health Department to decide | 192 (18.6) | 424 (41.0) | 280 (27.1) | 109 (10.5) | 30 (2.9) |
| Use random selection to decide | 51 (4.9) | 113 (10.9) | 191 (18.5) | 352 (34.0) | 328 (31.7) |
| Use a patient’s ability to pay to decide | 72 (7.0) | 113 (10.9) | 188 (18.2) | 221 (21.4) | 441 (42.6) |
| Use the importance of the patient to decide | 86 (8.3) | 221 (21.4) | 265 (25.6) | 211 (20.4) | 252 (24.4) |
Discussion
This study explored characteristics of patients that make the general population more or less willing to allocate access to ventilators. On average, prioritised patients were younger, more likely to benefit from care, non-smokers, with dependents, healthcare workers, and those with no physical or intellectual disability. In circumstances where COVID-19 rates in Australia increase significantly, this result might be used to help inform policy around allocation of ventilators in an ICU setting. Australian COVID-19 rates have remained relatively under control through 2020, although with variability across states (with Victoria the most severely affected to date). Interestingly, the results contrast with the likely prioritisation of the COVID-19 vaccines. The focus there is on those at greatest risk, both of suffering the more serious consequences of COVID-19, and of transmitting the virus to others. Our view is that this contrast is not necessarily of significant concern. Our DCE focuses on resource allocation contingent on having COVID-19 and needing ventilation. Thus, issues around risk are less relevant and the focus is on both efficiency (particularly likelihood of successful treatment and capacity to benefit) and equity.
This is not the first paper to address the dilemmas and challenges posed by limited resources for intensive care (including ventilators) during the COVID-19 pandemic, and our results do not offer simple solutions for making these contentious and often tragic decisions. We are conscious of the burden of responsibility that currently falls on clinicians working at the front line of the COVID-19 pandemic, and therefore of the need to generate information that might help inform such decision making. The specific contribution of this study is to provide an empirical insight into public preferences, albeit in a partial and limited way. We hope these insights add value to the current literature, which is dominated by normative appeals based on, for example, ‘bio-ethical reasoning’ [33], ‘medical ethics’ [19] and ‘trust’ [27]. We further hope that evidence such as that presented in our study will help to promote ethical and defensible decision making in which responsibility for the resulting inevitable harms to patients can be shared.
It is noteworthy that results from the mixed logit and latent class analysis demonstrate considerable heterogeneity in preferences. This is important as it shows that, if these decisions are vested in a single person, it is possible the conclusions a person reaches would diverge considerably from the mean societal preference. This is likely to be an unattractive conclusion and hence an indication that decision making should be conducted using a set of rules built through achieving consensus among a wide group of stakeholders.
The results from the prioritisation task provide an interesting contrast to those from the DCE. While the DCE presents public attitudes to allocation if they were forced into making such a choice, the prioritisation task suggests that members of the general population are typically more willing to have such decisions made by others, be they senior doctors or medical administrators. This finding is important, both for this work and for the DCE field in health more generally. For this work, it suggests that the DCE findings should be treated with some caution. It may be that respondents did not feel qualified to make such difficult decisions, and hence answered with uncertainty. More generally, it suggests that, while we can get plausible DCE results in a wide range of settings, we need to consider carefully how such findings are used in practice. The views of members of society are always valuable, but may well better be considered as supportive evidence for an alternative decision maker.
There are a number of limitations to the work that require consideration, both in the DCE itself, and in how policy makers might seek to utilise findings. First, the use of a single consumer representative in the qualitative work to identify appropriate dimensions and levels for the DCE is a limitation and having balance between multiple consumer representatives would have been a better approach. Having additional consumer input may have changed either the structure of the task or the way it was presented; if we had captured a broader number of dimensions of importance to the community, we might have reduced the latent class who demonstrated weak preferences across the dimensions that were presented. Without repeating the task with a fuller developmental process, it is difficult to determine the degree to which this matters. Indeed, it may not be possible to do so since public preferences might change as the COVID-19 situation develops over time. Regarding the DCE, the use of an online panel might be considered a weakness; if the involvement in the panel is associated with different preferences to the rest of the population, then external generalisability is problematic. On this point, it should be noted that our sample was age- and gender-representative by design, and did not appear to be extremely different from the general population in other collected characteristics. However, repeating such work using a different recruitment approach would augment the robustness of the findings. Secondly, the DCE was conducted online without an interviewer. This means respondents did not have the opportunity to ask clarifying questions, and may have been more inclined to use short cuts to completion. There is a strong relationship between completion time and predictive ability; the fastest 10% appear to be answering almost at random, while the best quality data (defined by Pseudo R2) came from those between the fifth and ninth decile of completion time. Based on these findings, we explored whether the main results were robust to the exclusion of the fastest decile, and they were (results available on request from the authors). Having stated that using online panels can be considered a weakness for this kind of study, there is a counter-argument that respondents are more willing to express their true opinion if there is no interviewer present [25]; again, before judging whether one mode of administration is superior to another, it is important to identify if the decision makes a substantive difference to the findings. Another possible limitation is that the design is focused on main effects only. This is a potential limitation as, under a QALY approach, you might expect interactions to matter (particularly between age and chance of survival if ventilated).
Our findings add to wider debates regarding the social values that should inform resource allocation in healthcare and the ethical quandaries inherent in prioritisation based on the characteristics of patient populations. For example, assertions of personal responsibility for health may inform the preference to treat non-smokers ahead of smokers, and the desire to reduce rates of premature death may inform the de-prioritisation of older patients that have achieved their ‘fair innings’. However, both of these positions are problematic and subject to challenge. For example, the extent of autonomy, and therefore responsibility, for personal health has been questioned [3], and age-based rationing has been the subject of longstanding critique [2, 35]. Perhaps most controversial is the apparent preference for prioritisation of able-bodied patients. This would seem to support concerns expressed about the risks of disability-based discrimination in responses to the COVID-19 pandemic [1]. In their present form, these findings run counter to claims regarding the importance of equal treatment and respect of human rights to healthcare. Clearly, more exploration is required of the underlying logic of such preferences and future research might include deliberative methods to explore, and possibly, refine views. Overall, these preferences should be considered in combination with our finding that citizens wish to defer to clinical authorities and professionals over decisions for individual patients. In other words, whilst public preference can help inform the weighing of competing moral claims when planning services for whole populations, they are not supported as a means for rationing of services ‘at the bedside’.
Supplementary Information
Below is the link to the electronic supplementary material.
Declarations
Funding
Fieldwork was funded using internal University resources.
Conflict of interest
None
Availability of data and material
The full survey is available in the Electronic Supplementary Material. Data are available on request from the authors.
Code availability
Code is available on request from the authors.
Authors contributions
RN and MA initiated the study. RN, SR, HD, IW and MA helped develop the experiment. RN, EM and KM analysed the data. All authors approved the final manuscript.
Ethics approval (include appropriate approvals or waivers)
Ethics approval was granted through the Curtin University Human Research Ethics Committee ((HRE2020-0368)
Consent for publication
All authors consented to the submission of this work for publication.
References
- 1.Andrews EE, Ayers KB, Brown KS, Dunn DS, Pilarski CR. No body is expendable: medical rationing and disability justice during the COVID-19 pandemic. Am Psychol. 2020 doi: 10.1037/amp0000709. [DOI] [PubMed] [Google Scholar]
- 2.Bognar G. Fair innings. Bioethics. 2015;29(4):251–261. doi: 10.1111/bioe.12101. [DOI] [PubMed] [Google Scholar]
- 3.Brown RC. Moral responsibility for (un)healthy behaviour. J Med Ethics. 2013;39(11):695–698. doi: 10.1136/medethics-2012-100774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheung W, Myburgh J, McGuinness S, Chalmers D, Parke R, Blyth F, New Zealand Intensive Care Society Clinical Trials, G A cross-sectional survey of Australian and New Zealand public opinion on methods totriage intensive care patients in an influenza pandemic. Crit Care Resusc. 2017;19(3):254–265. [PubMed] [Google Scholar]
- 5.Disability Rights UK. Covid 19 and the rights of disabled people. 2020. https://www.disabilityrightsuk.org/news/2020/april/covid-19-and-rights-disabled-people. Accessed 23 Feb 2021.
- 6.Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, Investigators, I. C. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985. doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dos Santos MJ, Martins MS, Santana FLP, Furtado M, Miname F, Pimentel R, da Silva LH. COVID-19: instruments for the allocation of mechanical ventilators-a narrative review. Crit Care. 2020;24(1):582. doi: 10.1186/s13054-020-03298-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dziak JJ, Coffman DL, Lanza ST, Li R, Jermiin LS. Sensitivity and specificity of information criteria. Brief Bioinform. 2020;21(2):553–565. doi: 10.1093/bib/bbz016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ellis AR, Howard K, Thomas KC, De Bekker-Grob EW, Ryan M, Lancsar E, Rose JM (2019) Number of Halton draws required for valid random parameter estimation with discrete choice data. Paper presented at the 10th Meeting of the International Academy of Health Preference Research, Basel, Switzerland.
- 10.Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, Phillips JP. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382(21):2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 11.Green C, Dickinson H, Carey G, Joyce A (2020) Barriers to policy action on social determinants of health for people with disability in Australia. Disability and Society
- 12.Greene WH, Hensher DA. A latent class model for discrete choice analysis: contrasts with mixed logit. Transport Res Part B Methodol. 2003;37(8):681–698. doi: 10.1016/S0191-2615(02)00046-2. [DOI] [Google Scholar]
- 13.Hole A. Fitting mixed logit models by using maximum simulated likelihood. STATA J. 2007;7:388–401. doi: 10.1177/1536867X0700700306. [DOI] [Google Scholar]
- 14.Intensive Care National Audit & Research Centre (2020) Report on COVID-19 in critical care Retrieved from https://www.icnarc.org/About/Latest-News/2020/03/22/Report-On-196-Patients-Critically-Ill-With-Covid-19.
- 15.Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user's guide. Pharmacoeconomics. 2008;26(8):661–677. doi: 10.2165/00019053-200826080-00004. [DOI] [PubMed] [Google Scholar]
- 16.Lancsar E, Louviere J, Flynn T. Several methods to investigate relative attribute impact in stated preference experiments. SocSci Med. 2007;64(8):1738–1753. doi: 10.1016/j.socscimed.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 17.Learning Disability England (2020) DNAR decisions—What the members survey told us. https://www.learningdisabilityengland.org.uk/news/dnar-decisions-what-the-members-survey-told-as/. Accessed 23 Feb 2021.
- 18.Litva A, Coast J, Donovan J, Eyles J, Shepherd M, Tacchi J, Morgan K. 'The public is too subjective': public involvement at different levels of health-care decision making. SocSci Med. 2002;54(12):1825–1837. doi: 10.1016/s0277-9536(01)00151-4. [DOI] [PubMed] [Google Scholar]
- 19.Mannelli C. Whose life to save? Scarce resources allocation in the COVID-19 outbreak. J Med Ethics. 2020;46(6):364–366. doi: 10.1136/medethics-2020-106227. [DOI] [PubMed] [Google Scholar]
- 20.Maves RC, Downar J, Dichter JR, Hick JL, Devereaux A, Geiling JA, Care ATFMC Triage of Scarce Critical Care Resources in COVID-19 an implementation guide for regional allocation: an expert panel report of the task force for mass critical care and the American College of Chest Physicians. Chest. 2020;158(1):212–225. doi: 10.1016/j.chest.2020.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McKie J, Richardson J. Social preferences for prioritising the treatment of disabled and chronically ill patients: beyond the order effect. Health Econ Policy Law. 2019;14(4):443–467. doi: 10.1017/S1744133118000154. [DOI] [PubMed] [Google Scholar]
- 22.Mulhern B, Norman R, Street DJ, Viney R. One method, many methodological choices: a structured review of discrete-choice experiments for health state valuation. Pharmacoeconomics. 2019;37(1):29–43. doi: 10.1007/s40273-018-0714-6. [DOI] [PubMed] [Google Scholar]
- 23.National Institute for Health and Care Excellence. COVID-19 rapid guideline: critical care in adults. 2020. https://www.nice.org.uk/guidance/ng159. Accessed 12 Feb 2021. [PubMed]
- 24.Norman R, Hall J, Street DJ, Viney R. Efficiency and equity: a stated preference approach. Health Econ. 2012;22(5):568–581. doi: 10.1002/hec.2827. [DOI] [PubMed] [Google Scholar]
- 25.Poder TG, He J. Willingness to pay and the sensitivity of willingness to pay for interdisciplinary musculoskeletal clinics: a contingent valuation study in Quebec, Canada. Int J Health Econ Manag. 2016;16(4):337–361. doi: 10.1007/s10754-016-9193-5. [DOI] [PubMed] [Google Scholar]
- 26.Potere N, Valeriani E, Candeloro M, Tana M, Porreca E, Abbate A, Di Nisio M. Acute complications and mortality in hospitalized patients with coronavirus disease 2019: a systematic review and meta-analysis. Crit Care. 2020;24(1):389. doi: 10.1186/s13054-020-03022-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ramachandran P, Swamy L, Kaul V, Agrawal A. A National strategy for ventilator and ICU resource allocation during the coronavirus disease 2019 pandemic. Chest. 2020;158(3):887–889. doi: 10.1016/j.chest.2020.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reckers-Droog V, van Exel J, Brouwer W. Equity weights for priority setting in healthcare: severity, age, or both? Value Health. 2019;22(12):1441–1449. doi: 10.1016/j.jval.2019.07.012. [DOI] [PubMed] [Google Scholar]
- 29.Shah KK. Severity of illness and priority setting in healthcare: a review of the literature. Health Policy. 2009;93(2–3):77–84. doi: 10.1016/j.healthpol.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 30.Skedgel CD, Wailoo AJ, Akehurst RL. Choosing vs allocating: discrete choice experiments and constant-sum paired comparisons for the elicitation of societal preferences. Health Expect. 2015;18(5):1227–1240. doi: 10.1111/hex.12098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Soekhai V, de Bekker-Grob EW, Ellis AR, Vass CM. Discrete choice experiments in health economics: past present and future. Pharmacoeconomics. 2019;37(2):201–226. doi: 10.1007/s40273-018-0734-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.StataCorp . Stata version 16. College Station: Stata Press; 2019. [Google Scholar]
- 33.Vergano M, Bertolini G, Giannini A, Gristina GR, Livigni S, Mistraletti G, Petrini F. Clinical ethics recommendations for the allocation of intensive care treatments in exceptional, resource-limited circumstances: the Italian perspective during the COVID-19 epidemic. Crit Care. 2020;24(1):165. doi: 10.1186/s13054-020-02891-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.White DB, Lo B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. JAMA. 2020;323(18):1773–1774. doi: 10.1001/jama.2020.5046. [DOI] [PubMed] [Google Scholar]
- 35.Williams A, Evans JG. The rationing debate. Rationing health care by age. BMJ. 1997;314(7083):820–825. doi: 10.1136/bmj.314.7083.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yoo HI. lclogit2: an enhanced module to estimate latent class conditional logit models. 2019. https://ssrn.com/abstract=3484429. Accessed 23 Feb 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.