Abstract
Adults with congenital heart disease often have complex medical issues requiring individualised multidisciplinary care for optimising outcomes and quality of life. Chronic pain is an example. We report a rare case of intercostal neuralgia seemingly caused by irritation from a prosthetic valve in a right ventricle to pulmonary artery conduit in a patient with tetralogy of Fallot. Intercostal neuralgia is a painful disorder linked to nerve irritation or injury from trauma, infection or pressure. Although chronic postsurgical pain after cardiac surgery is prevalent, rarely the aetiology relates to valve irritation on a single intercostal nerve. After failing pharmacological therapy for 8 months, the neuralgia completely resolved after an ultrasound-guided neurolytic block with long-term effectiveness and improvement in patient satisfaction.
Keywords: pain, pain (neurology), cardiovascular medicine, medical management, cardiothoracic surgery
Background
Patients undergoing cardiothoracic surgery are at risk of developing chronic postsurgical pain, with a reported prevalence of 20% after 3 years.1 The pathophysiology of chronic postsurgical pain is poorly understood and includes direct or indirect trauma to intercostal nerves and surrounding myofascial components, presence of chronic inflammatory changes and altered neural regeneration pathways.2 Intercostal neuralgia after cardiothoracic surgery can manifest as intense dysesthetic pain.3 The pain has neuropathic characteristics and is often described as burning or tearing in nature, can involve any of the intercostal nerves including the subcostal nerve of the 12th rib, and is minimally affected by deep inspiration or expiration.4 While most commonly reported after cardiothoracic surgery, intercostal neuralgia has been reported to occur from trauma, lung neoplasia, bone tumour proximity and infection.5–8
Adults with congenital heart disease are at high risk of developing chronic postsurgical pain due to the multiple procedures for treatment of their cardiac condition. We present an unusual case which suggests intercostal neuralgia can be caused by irritation of an intercostal nerve by a prosthetic valve in an intrathoracic right ventricle to pulmonary artery conduit.
Case presentation
Ten years after cardiac surgery, a 40-year-old man presented with the chief problem of a sporadic focal chest pain to the left of his sternum lasting for 1 month. He described his pain as ‘tearing’, but not dull, aching or tingling. The pain, was more noticeable at rest, could appear suddenly and wake him from sleep, and was unrelated to exercise or body position. His pain intensity ranged from 0 to 6/10 on the Numeric Pain Rating Scale (scale of 0 to 10, 0 being ‘no pain’ and 10 being ‘the worst pain imaginable’) and only mild relief resulted with oral ibuprofen. His wife reported him to be ‘stoic’. The patient identified a horizontal oval area of approximately 4×3 cm in size extending from the left sternocostal border to 5 cm laterally over the anterior fourth and fifth ribs. He was born with tetralogy of Fallot and pulmonary atresia with multiple aortopulmonary collateral arteries. He had undergone staged surgical repair with numerous surgeries, including placement of a right ventricle to pulmonary artery conduit with a 26 mm Hancock valve 10 years previously. He also had a defibrillator placed for atrial flutter and ventricular tachycardia 2 years earlier. While this patient had four sternotomies, he had never undergone a thoracotomy. He was compliant with visits and treatment plans and was followed closely by a multidisciplinary team. A review of other organ systems was negative. His medications included aspirin, furosemide, spironolactone, losartan, metoprolol, mexiletine and a multivitamin. The patient was concerned that the pain could be cardiac in origin and represented a worsening dilation of his ascending aorta.
On exam, the patient was 86.4 kg and had a body mass index of 25. The right arm blood pressure was 111/55, pulse 80, respirations 24 and pulse oximetry 97% on room air. His pain score was 0/10 on the Numeric Pain Rating Scale. Pertinent physical findings included clear and equal breath sounds, regular cardiac rate and rhythm with a widely split S2, and a left upper sternal II/VI systolic ejection murmur. The chest wall was normal in shape, and there were no skin changes other than a healed midline sternotomy scar and associated lateral upper abdomen chest tube scars.
Investigations
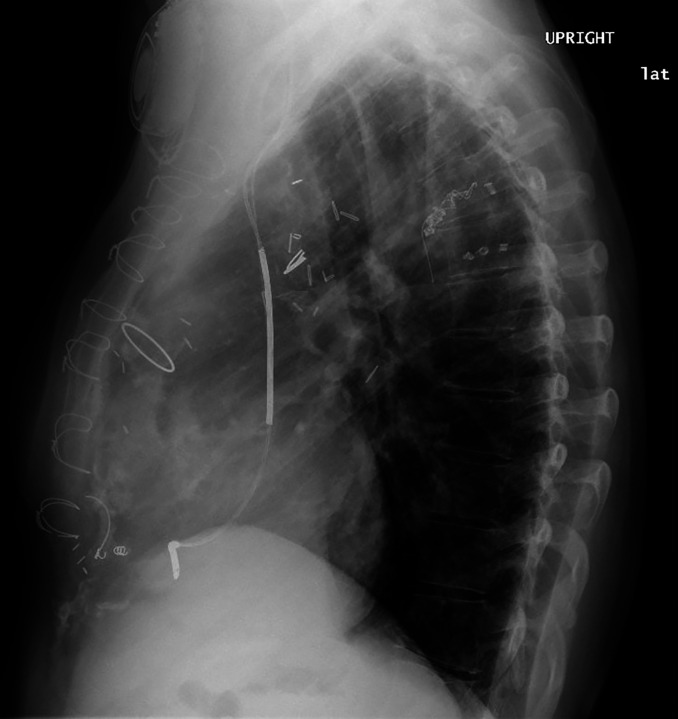
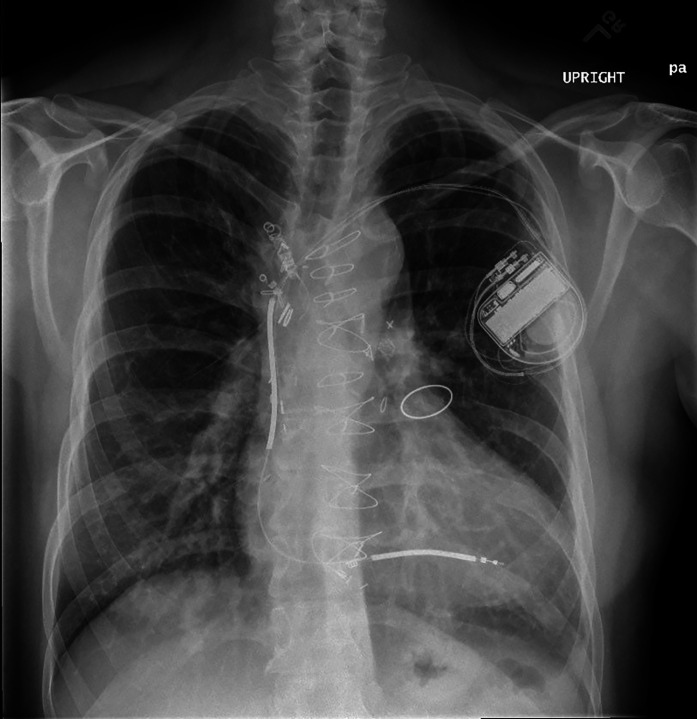
A chest roentgenogram showed stable cardiomegaly and a prosthetic pulmonary valve ring oriented in the sagittal plane adjacent to the anterior rib cage (figures 1 and 2). A cardiac CT scan was also performed which showed stable ascending aortic dimensions.
Figure 1.
Lateral chest X-ray showing the pulmonary valve ring adjacent to anterior chest wall.
Figure 2.
Posterior anterior chest X-ray. Note location of pulmonary valve ring in left chest next to the sternum.
Differential diagnosis
The history and presentation was highly suggestive of intercostal neuralgia. Other broad differential diagnoses were considered and included spinal radiculopathies, intercostal nerves and lung neoplasms, localised mass effect from other aetiologies, history of trauma, and infectious causes such as herpes zoster. Intercostal neuralgia is most commonly caused by trauma resulting from a thoracotomy, chest tube placement or penetrating chest wound. Despite this patient’s past multiple surgical interventions, the painful site had no evidence of scars or trauma. The skin was intact by inspection. Operative reports did not indicate chest tubes or surgical incisions at the site. The chest roentgenogram was revealing as it showed a prosthetic pulmonary valve ring adjacent and oriented to the anterior rib cage, coincident to the area of pain.
Treatment
After reassurance that the pain pattern was not related to worsening cardiac function, the patient initially agreed to take an oral course of gabapentin at 100 mg three times a day. The pain became more tolerable, but was not decreased in frequency or intensity. He was not interested in increasing his gabapentin dose or trying a different medication. After 8 months, the pain still persisted with little improvement in pain scores. The patient was intolerant of gabapentin’s sedative effects and decided to undergo a neurolytic block. Since the pain was sporadic, the patient was asked to make notes of where the pain occurred. Under 2-D ultrasound, a test left fourth rib anaesthetic block with 2% buffered lidocaine was placed at the mid-axillary line. After confirmation of anaesthesia in the marked area, a left fourth rib neurolytic block with 1.5 mL 50% ethanol/0.2% ropivacaine was placed distal to the previous block in the mid-clavicular line. The pain did not return after this intervention. The patient continued to have periodic multidisciplinary care follow ups confirming the resolution of the painful neuralgia.
Outcome and follow-up
Three years after the neurolytic block, the patient received a transcatheter pulmonary valve replacement for pulmonary artery conduit stenosis. Follow-up 7 years after the block showed continued pain resolution.
Discussion
The number of adults with congenital heart disease are growing due to advances in modern medicine. Generally, these patients have complex medical and surgical histories. Chronic postsurgical pain in this patient population is commonly reported and can be challenging to treat. Despite many sternotomies, this patient had no significant complaints of chest wall-related pain until the initial presentation as described, 10 years after the last open cardiac surgery.
Intercostal neuralgia is most commonly caused by thoracotomy, chest tube placement, or penetrating chest wound trauma.3 Other causes of intercostal neuralgia may include spinal radiculopathies, sarcoidosis, neoplasms of the intercostal nerve and lung, and infectious aetiologies, primarily herpes zoster.3 This case is unique among traumatic causes in that a prosthetic pulmonary valve ring became a mechanical irritant of a single intercostal nerve by cardiogenic movement adjacent to the anterior fourth intercostal nerve. The evidence for this aetiology is suggested by the response to treatment and the spatial association of the valve ring with the anterior fourth rib on chest roentgenogram.
The pain of intercostal neuralgia is the result of nerve damage or inflammation and can be localised to one or more of the intercostal spaces. The pathophysiology of chronic intercostal neuralgia pain is multivariable and involves a combination of peripheral, central, and psychological mechanisms. The inciting event is variable and can include skin and muscle injury, rib dislocation, costovertebral ligament damage, post-herpetic neuralgia, or post-thoracotomy pain.4 The pathophysiology involves activated peripheral nociceptors that are triggered by cytokines released from damaged tissue and resultant cellular inflammation. This in turn leads to generation of action potentials that are conducted from the peripheral nociceptors to the thoracic spinal cord via the intercostal nerves.4 A structural or inflammatory source can be identified in some; however, most patients have a primary pain disorder with uncertain aetiology.9 Intercostal neuralgia is typically difficult to treat as no treatment modality has been shown to be curative.4 However, several treatment options are available including systemic medications, topical or invasive nerve blocks, surgery, and cryoablation.3 10–12
There is no definitive treatment protocol for intercostal neuralgia as small sample sizes, difficulty in determining control groups, and nebulous outcome measures have limited studies of scale.4 Treatment is usually divided into pharmacological (tricyclic antidepressants or TCAs, anticonvulsants, and topical agents), non-somatic (psychological/cognitive behavioural treatment), interventional pain treatment (intercostal nerve blocks/dorsal root ganglion pulsed radiofrequency treatment), and surgery (dorsal root entry zone ablation).4 For initial treatment, TCAs were avoided after consideration of the adverse side effect profile and instead the patient was placed on gabapentin 100 mg three times a day. After a trial of several months, the patient experienced minimal pain relief and was unhappy with drowsiness and ataxia, both common side effects of gabapentin. On investigating further treatment options, an intercostal neurolytic block seemed to have the best risk/benefit profile as it was non-surgical and could be performed without the need for a general anaesthetic or monitored anaesthesia care.
In summary, this is an unusual case of intercostal neuralgia involving a single dermatome presumably caused by trauma from a prosthetic pulmonary valve ring in an intrathoracic right ventricle to pulmonary artery conduit. Pain medicine providers should consider intercostal neuralgia in the differential diagnoses when evaluating patients complaining of non-cardiogenic chest pain after thoracic surgery, especially when the thoracic pain is focal and not associated with chest or mediastinal tube placements.
Patient’s perspective.
I must admit when we were talking about doing the procedure, I wasn’t sure it would be the answer to my problem. Dr. Schmitz and I have been through a lot together so I always listen to his advice. I am glad I did because it was a huge success. Still not having any problems.
Learning points.
Adults survivors of congenital heart disease are increasing due to modern medical advances.
Chronic postsurgical pain in adult patients with congenital heart disease is prevalent.
Although rare, intercostal neuralgia involving a single dermatome could be associated with the presence of a prosthetic pulmonary valve in an intrathoracic right ventricle to pulmonary artery conduit.
Pain medicine clinicians should include intercostal neuralgia in the differential diagnoses when evaluating patients with non-cardiogenic chest pain after thoracic surgery, especially when the pain is focal and not associated with chest or mediastinal tube placements.
Acknowledgments
The authors would like to thank Ms. Patti E. Griffey for her editing assistance for this manuscript.
Footnotes
Twitter: @mls131219
Contributors: All authors made substantial contributions to the creation of this report, the acquisition of the details, the analysis and discussion of the case; also, to the drafting and revision of important intellectual content. All authors gave final approval of the version published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Marcassa C, Faggiano P, Greco C, et al. Italian association of cardiovascular prevention, rehabilitation (GICR-IACPR). A retrospective multicenter study on long-term prevalence of chronic pain after cardiac surgery. J Cardiovasc Med 2015;16:768–74. [DOI] [PubMed] [Google Scholar]
- 2.Mazzeffi M, Khelemsky Y. Poststernotomy pain: a clinical review. J Cardiothorac Vasc Anesth 2011;25:1163–78. 10.1053/j.jvca.2011.08.001 [DOI] [PubMed] [Google Scholar]
- 3.Waldman SD. Chest wall pain syndromes. : Waldman SD, . Pain management. 2nd edn. Philadelphia: Elsevier Saunders, 2011: 632–45. [Google Scholar]
- 4.Dureja GP. Intercostal neuralgia: a review. J Neurol Transl Neurosci 2017;5:1–8. [Google Scholar]
- 5.Dajczman E, Gordon A, Kreisman H, et al. Long-Term postthoracotomy pain. Chest 1991;99:270–4. 10.1378/chest.99.2.270 [DOI] [PubMed] [Google Scholar]
- 6.Wong L. Intercostal neuromas: a treatable cause of postoperative breast surgery pain. Ann Plast Surg 2001;46:481–4. 10.1097/00000637-200105000-00004 [DOI] [PubMed] [Google Scholar]
- 7.Santos PSSdos, Resende LAL, Fonseca RG, et al. Intercostal nerve mononeuropathy: study of 14 cases. Arq Neuropsiquiatr 2005;63:776–8. 10.1590/S0004-282X2005000500011 [DOI] [PubMed] [Google Scholar]
- 8.Kobayashi H, Shinoda Y, Ohki T, et al. Intercostal neuralgia as a symptom of an osteoblastoma in thoracic spine. BMJ Case Rep 2015;2015. 10.1136/bcr-2015-210720. [Epub ahead of print: 02 Jul 2015]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang L, Singla AK. Intercostal nerve block. : Lennard TA, Vivian DG, WalkowskiSD SAK, . Pain procedures in clinical practice. 3rd edn. Philadelphia: Saunders, 2011: 289–92. [Google Scholar]
- 10.Devers A, Galer BS. Topical lidocaine patch relieves a variety of neuropathic pain conditions: an open-label study. Clin J Pain 2000;16:205–8. 10.1097/00002508-200009000-00005 [DOI] [PubMed] [Google Scholar]
- 11.Byas-Smith MG, Gulati A. Ultrasound-Guided intercostal nerve cryoablation. Anesth Analg 2006;103:1033–5. 10.1213/01.ane.0000237290.68166.c2 [DOI] [PubMed] [Google Scholar]
- 12.Williams EH, Williams CG, Rosson GD, et al. Neurectomy for treatment of intercostal neuralgia. Ann Thorac Surg 2008;85:1766–70. 10.1016/j.athoracsur.2007.11.058 [DOI] [PubMed] [Google Scholar]