Abstract
Purpose
Depression, one of the most common mental disorders, is up-surging worldwide amid the ongoing coronavirus disease 2019 (COVID-19) pandemic, especially among the older population. This study aims to measure prevalent depressive symptoms and its associates among older adults amid the COVID-19 pandemic in Bangladesh.
Methods
This cross-sectional study was carried out among 1032 older Bangladeshi adults, aged 60 years and above, through telephone interviews in October 2020. We used a semi-structured questionnaire to collect data on participants’ socio-demographic and lifestyle characteristics, pre-existing medical conditions, and COVID-19-related information. Meanwhile, depressive symptoms were measured using the 15-item Geriatric Depression Scale (GDS-15). The binary logistic regression model was used to identify the factors associated with depressive symptoms.
Results
Two-in-five participants showed depressive symptoms on the GDS-15 scale. Poor socioeconomic characteristic such as low family income, dependency on the family for living, recipient of financial support during the pandemic was associated with higher odds of depressive symptoms. Participants with pre-existing medical conditions had 91% higher odds of depressive symptoms. Social isolation, captured in terms of living alone (aOR = 2.11, 95% CI 1.11–4.01), less frequent communication during pandemic (aOR = 1.55, 95% CI 1.07–2.26), perceived loneliness (aOR = 2.25, 95% CI 1.47–3.45), and isolation from others (aOR = 2.45, 95% CI 1.62–3.70) were associated with higher odds of depressive symptoms.
Conclusions
Our study found a sizeable proportion of study participants with depressive symptoms amidst the ongoing pandemic. The findings of the present study call for the urgent need for mental health support package targeting this vulnerable group of population.
Keywords: COVID-19, Mental disorders, Depressive symptoms, Older adults, Bangladesh
Background
Globally, an estimated 703 million people were aged 65 years or above in 2019 [1]. Population is aging rapidly in many parts of the world, including Bangladesh, a South Asian country, where the current legal provision identifies individuals 60 and over as older adults [2]. According to the estimates for 2019, the population of 60 + in Bangladesh was over 13 million (8% of the total population), which is projected to increase nearly three-fold to 36 million in 2050 (21.9% of the total estimated population) [3].
Along with several chronic conditions, mental disorders, including depression, are prevalent in older ages [4]. Data from the Global Burden of Diseases and the World Health Organization indicate about 264 million people aged 60 years and above have depressive symptoms [5, 6]. Despite the outrageously high prevalence of depression among older adults in low-and middle-income countries (LMICs), compared to high-income countries, it has received fairly low attention in many LMICs, including Bangladesh [7]. The emergence of Coronavirus disease 2019 (COVID-19) pandemic, which has already taken 1,393,227 lives and added more than 58 million to the global burden of disease [8], has aggravated the psychological toll on the general population, particularly among the older population who are at an increased vulnerability to severe illness and mortality. Historically, the mental well-being of the population has been disrupted in large-scale outbreaks and pandemics. For example, during the H1N1 influenza virus outbreak in 2009, anxiety among the UK's general population increased by 10–30% [9]. Similarly, during the severe acute respiratory syndrome (SARS) epidemic, psychiatric morbidities, depression, and stress disorder increased [10]. Furthermore, during the Ebola outbreak, in 2013–2016 in Guinea, Liberia, and Sierra Leone, the psychosocial well-being of the people was seriously hampered [11]. Likewise, stress, anxiety, depressive symptoms, insomnia, denial, anger, and fear are associated with the COVID-19 [12].
In Bangladesh, even prior to the onset of the COVID-19 pandemic, mental health issues have not received attention in policy discourse. Recognizing the high burden of mental health disorders, recently, the Government of Bangladesh passed the Mental Health ACT 2018, but the implementation of this act seems challenging because of the fragile health system and inadequate mental health professionals [13]. There is a lack of adequate mental health services in the first place, but even those limited services are underutilized because the social stigma and stereotypes regarding mental illness discourage people from acknowledging their symptoms or seeking healthcare. Having said that, the ongoing COVID-19 pandemic may have seriously aggravated the mental health conditions among Bangladeshi older adults for several reasons to be noted here. First, with over 447,000 COVID-19 confirmed cases and 6388 COVID-19-related deaths as of 23rd November 2020, Bangladesh is ranked 24th country in terms of the highest number of COVID-19 confirmed cases [8]. Second, older adults are at increased risk of severe illness and mortality due to COVID-19 than younger age groups [14]. Third, the high prevalence of non-communicable chronic conditions, such as hypertension, obesity, diabetes, cardiovascular disease, and chronic lung disease, and comorbidities, among Bangladeshi older adults [15] increases their risk of severe health outcomes like poor self-management of conditions, poor quality of life and increased hospitalizations [16]. Moreover, the unplanned lockdown and subsequent difficulty in accessing food, health care, medication, and psychological support as well as social distancing and isolation could have exacerbated anxiety and depression in this particular group of population[17, 18]. All these factors can interplay to worsen the mental health conditions among older adults in Bangladesh amid this pandemic.
Amidst the COVID-19 pandemic, some studies from Bangladesh have shed light on depressive symptoms and mental health among university students [19] and the general population [20], but to our best knowledge, no studies have been undertaken to study depressive symptoms among older adults in Bangladesh who are most vulnerable to the pandemic. While such evidence is lacking in the Bangladeshi context, evidence from LMICs shows that the prevalence of depressive symptoms and anxiety was overwhelmingly high among older adults during the COVID-19 pandemic [21–23]. A 2019 study (conducted before the onset of the COVID-19 pandemic) reported a 36.9% prevalence of depressive symptoms among Bangladeshi older adults [24]. The current study on the same topic amid the COVID-19 pandemic may complement our understanding. In terms of correlates of depressive symptoms among the older population, previous research from LMICs, including Bangladesh, noted several associated factors such as age, low socioeconomic status (SES), presence of single or comorbid non-communicable disease, sleep disturbances, and so forth [25–28]. However, our understanding of correlates specific to COVID-19 is lacking. Therefore, it is of utmost importance to study depressive symptoms among the most at-risk population during the ongoing pandemic. In this light, the present study aimed to determine the prevalence of depressive symptoms and its associates among older adults of Bangladesh. The findings from this study might help relevant stakeholders in designing and implementing multisectoral approaches to address the mental health needs of this vulnerable and neglected group of people.
Methods
Study design and participants
Given the virus's highly contagious nature and the subsequent risk of spreading through face-to-face contact, this cross-sectional study was conducted remotely through telephone interviews.
The study was conducted by the Aureolin Research, Consultancy and Expertise Development (ARCED) Foundation in October 2020. The primary challenge for this study was to develop a sampling frame to select participants, and thus, we utilized our pre-established registry, which included households from all eight administrative divisions of Bangladesh as a sampling frame. Considering 50% prevalence with a 5% margin of error, at the 95% level of confidence, 90% power of the test, and 95% response rate, a sample size of 1096 was calculated. However, 1032 approached eligible participants responded to the study with an overall response rate of approximately 94%. Based on the population distribution of older adults by geography in Bangladesh, we adopted probability proportionate to size (of the eight division) approach to select older adults in each division [2]. Stratified random sampling technique was followed to select the targeted number of households from each administrative division. One eligible respondent was interviewed from the sampled households. In case of more than one eligible participant in a selected household, the oldest one was interviewed. The inclusion criterion was the minimum age of 60 years, and the exclusion criteria included adverse mental conditions (clinically proved schizophrenia, bipolar mood disorder, dementia/cognitive impairment), a hearing disability, or inability to communicate.
Measures
Outcome measure
The primary outcome of the study was depressive symptoms, measured using the 15-item Geriatric Depression Scale (GDS-15), a widely used scale for measuring depressive symptoms among older adults in both clinical and community setting [29]. Briefly, each item in the scale is measured as yes/no questions. After reverse coding of some negatively worded items, a cumulative score of the 15 items, with ranges 0–15, is calculated. The total score was dichotomized into probable absence (score ≤ 5) or presence of depressive symptoms (> 5) [27]. The GDS-15 scale has previously been validated and used among the Bangladeshi older population [24]. We also found it to be a reliable scale, indicated by the high internal consistency (Cronbach’s alpha 0.77) among our study participants.
Explanatory variables
Explanatory variables considered in this study were age, sex, marital status, literacy, family size, family monthly income (BDT), residence, occupation, living arrangements, financial dependence on family for a living, walking time to the nearest health center, problem in memory or concentration, presence of pre-existing medical conditions, feeling concerned about COVID-19, feeling overwhelmed by COVID-19, difficulty in getting food, medicine, and routine medical care during COVID-19, difficulty in earning during COVID-19, feeling of loneliness and isolation, frequency of communication during COVID-19, receiving any financial support (government or non-government) during COVID-19, and source of COVID-19-related information. The definition and description of the explanatory variables are presented in Table 1.
Table 1.
Definition and description of explanatory variables
| Study variables | Description and categories |
|---|---|
| Administrative division | Administrative divisions of Bangladesh (1 = Barishal, 2 = Chattogram, 3 = Dhaka, 4 = Mymensingh, 5 = Khulna, 6 = Rajshahi, 7 = Rangpur, 8 = Sylhet) |
| Age | Age of the respondent (1 = 60–69 years, 2 = 80–79 years and 3 = 80 years or more) |
| Sex | Sex of the respondent (1 = male, 2 = female) |
| Marital status | Marital status of the respondent (1 = married, 2 = widowed) |
| Literacy | Respondent can read and write (1 = illiterate, 2 = literate) |
| Family size | Number of household member (1 = 0–4, 2 = more than 4) |
| Family monthly income (BDT1) | Monthly family income in Bangladeshi taka (1 = less than 5000, 2 = 5000–10,000, 3 = more than 10,000) |
| Residence | Current residence of the respondent (1 = Urban, 2 = Rural) |
| Current occupation | Current employment status of the respondent (1 = Currently employed, 2 = Unemployed or retired) |
| Living arrangement | Current living arrangement of the respondent (1 = living with other family members, 2 = living alone) |
| Financial dependency on family for living | Respondent financially dependent on the family for a living (1 = no, 2 = yes) |
| Walking time to the nearest health centre | Walking time to the nearest health centre from respondent’s residence (1 = < 30 min, 2 = ≥ 30 min) |
| Problem in memory or concentration | Respondent has a memory or concentration problem (1 = no problem, 2 = low memory or concentration) |
| Pre-existing medical conditions | Self-reported information on pre-existing medical conditions, such as arthritis, hypertension, heart diseases, stroke, hypercholesterolemia, diabetes, chronic respiratory diseases, chronic kidney disease, and cancer (1 = no condition, 2 = has pre-existing condition) |
| Feeling concerned about COVID-19 | Respondent feeling concerned about COVID-19 (1 = hardly, 2 = sometimes/often) |
| Overwhelmed by COVID-19 | Respondent overwhelmed by COVID-19 (1 = hardly, 2 = sometimes/often) |
| Difficulty in getting food during COVID-19 | Respondent faced difficulty in getting food during COVID-19 (1 = no, 2 = yes) |
| Difficulty in getting medicine during COVID-19 | Respondent faced difficulty in getting medicine during COVID-19 (1 = no, 2 = yes) |
| Difficulty in earning during COVID-19 | Respondent faced difficulty in earning during COVID-19 (1 = no, 2 = yes) |
| Difficulty receiving routine medical care during COVID-19 | Respondent faced difficulty in receiving routine medical care during COVID-19 (1 = no, 2 = yes) |
| Feeling of loneliness | Perceived feeing of loneliness by respondent (1 = hardly, 2 = sometimes/often) |
| Feeling isolated from others | Perceived feeling of isolation from others by respondent (1 = hardly, 2 = sometimes/often) |
| Frequency of communication during COVID-19 | Frequency of communication with friends and family during COVID-19 (1 = same as previous, 2 = less than previous) |
| Received any financial support (Government or non-government) during COVID-19 | Received any financial support (Government or non-government) during COVID-19 (1 = no, 2 = yes) |
| Source of COVID-19-related information | Source of receiving COVID-19-related information (1 = radio/television, 2 = health workers, 3 = friends/family/neighbours) |
1BDT stands for Bangladesh taka and 1 BDT ~ 84.7 US dollars
Data collection tools and techniques
A pre-tested semi-structured questionnaire was used to collect the information through a telephone interview. Data collection was accomplished electronically using SurveyCTO mobile app (https://www.surveycto.com/) by trained research assistants, recruited based on previous experience of administering health surveys in the electronic platform. The research assistants were trained extensively before the data collection through Zoom meetings.
The English version of the questionnaire was first translated to Bengali language and then back translated to English by two researchers to ensure the contents' consistency. The questionnaire was then piloted among a small sample (n = 10) of older adults to refine the language in the final version. The tool used in the pilot study did not receive any corrections/suggestions from the participants in relation to the contents developed in the Bengali language.
Statistical analysis
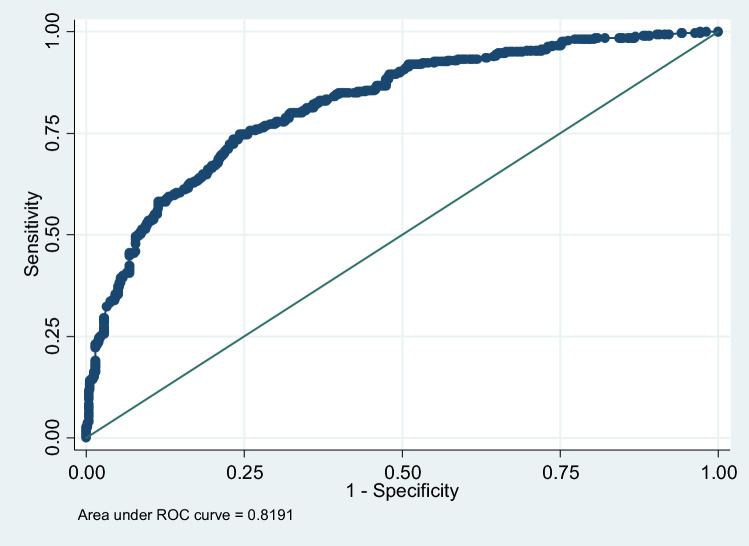
The distribution of the variables was assessed through descriptive analysis. Given our variables' categorical nature, Chi-square tests were performed to compare differences in the prevalence of depressive symptoms by explanatory variables, with a 5% level of significance. We used binary logistic regression models to explore the factors associated with dichotomized depressive symptoms. The initial model was run with all potential covariates (Table 1) and then using the backward elimination criteria with the Akaike information criterion (AIC) final model was selected. Adjusted odds ratio (aOR) and associated 95% confidence interval (95% CI) are reported. The area under the curve (AUC) (Annex 1) and Hosmer–Lemeshow test (p value = 0.17) indicate that our model fits the data well. All analyses were performed using the statistical software package Stata (Version 14.0).
Results
Characteristics of the participants
Table 2 shows the summary statistics of the study participants. Among the 1032 study participants, 20.4% were from Dhaka division, 77.8% aged 60–69 years, 65.5% male, 73.9%% from the rural areas, 58.3% illiterate, and 81.4% were currently married. Over half of the participants (53.8%) had a family income of > 10,000 BDT, 40.6% were currently employed, 92.3% resided with their family members, 68.1% depended on their family for living, and 58.9% had pre-existing medical conditions. Approximately 83.0% of the participants reported radio/television as the source of COVID-19-related information. Moreover, 71.0%% of the participants were concerned about the pandemic, 62.7% had difficulty earning, and 24.7% had difficulty getting medicine during the pandemic.
Table 2.
Characteristics of the participants (N = 1032)
| Characteristics | n | % |
|---|---|---|
| Socioeconomic characteristics | ||
| Administrative division | ||
| Barishal | 149 | 14.4 |
| Chattogram | 137 | 13.3 |
| Dhaka | 210 | 20.4 |
| Mymensingh | 63 | 42.0 |
| Khulna | 158 | 15.3 |
| Rajshahi | 103 | 10.0 |
| Rangpur | 144 | 14.0 |
| Sylhet | 68 | 6.5 |
| Age (year) | ||
| 60—69 | 803 | 77.8 |
| 70–79 | 174 | 16.9 |
| ≥ 80 | 55 | 5.3 |
| Sex | ||
| Male | 676 | 65.5 |
| Female | 356 | 34.5 |
| Marital status | ||
| Married | 840 | 81.4 |
| Widowed | 192 | 18.6 |
| Literacy | ||
| Illiterate | 602 | 58.3 |
| Literate | 430 | 41.7 |
| Family size | ||
| ≤ 4 | 318 | 30.8 |
| > 4 | 714 | 69.2 |
| Family monthly income (BDT1) | ||
| < 5000 | 145 | 14.1 |
| 5000–10,000 | 331 | 32.1 |
| > 10,000 | 556 | 53.8 |
| Residence | ||
| Urban | 269 | 26.1 |
| Rural | 763 | 73.9 |
| Current occupation | ||
| Currently employed | 419 | 40.6 |
| Unemployed/retired | 613 | 59.4 |
| Living arrangement | ||
| Living with other family members | 953 | 92.3 |
| Living alone | 79 | 7.7 |
| Financial dependency on family for living | ||
| No | 329 | 31.9 |
| Yes | 703 | 68.1 |
| Walking time to the nearest health centre | ||
| < 30 min | 508 | 49.2 |
| ≥ 30 min | 524 | 50.8 |
| Physical and mental health | ||
| Problem in memory or concentration | ||
| No problem | 782 | 75.8 |
| Low memory or concentration | 250 | 24.2 |
| Pre-existing medical conditions | ||
| No | 424 | 41.1 |
| Yes | 608 | 58.9 |
| Feeling of loneliness | ||
| Hardly | 590 | 57.2 |
| Sometimes/often | 442 | 42.8 |
| Feeling isolated from others | ||
| Hardly | 636 | 61.6 |
| Sometimes/often | 396 | 38.4 |
| COVID-19-related information | ||
| Feeling concerned about COVID-19 | ||
| Hardly | 299 | 29.0 |
| Sometimes/often | 733 | 71.0 |
| Overwhelmed by COVID-19 | ||
| Hardly | 370 | 36.4 |
| Sometimes/often | 647 | 63.6 |
| Difficulty in getting food during COVID-19 | ||
| No | 553 | 55.3 |
| Yes | 447 | 44.7 |
| Difficulty in getting medicine during COVID-19 | ||
| No | 733 | 75.3 |
| Yes | 240 | 24.7 |
| Difficulty in earning during COVID-19 | ||
| No | 340 | 37.4 |
| Yes | 570 | 62.6 |
| Difficulty receiving routine medical care during COVID-19 | ||
| No | 644 | 69.6 |
| Yes | 281 | 30.4 |
| Frequency of communication during COVID-19 | ||
| Same as previous | 598 | 58.0 |
| Less than previous | 434 | 42.1 |
| *Source of COVID-19-related information | ||
| Radio/Television | 857 | 83.0 |
| Health workers | 96 | 9.3 |
| Friends/family/neighbours | 735 | 71.2 |
| Received any financial support (Government or non-government) during COVID-19 | ||
| No | 764 | 74.0 |
| Yes | 268 | 26.0 |
1BDT stands for Bangladesh taka and 1 BDT ~ 84.7 US dollars
*Multiple responses
Prevalence of depressive symptoms
Overall, 40.1% of the participants had depressive symptoms (Table 3). The bivariate association between depressive symptoms and different explanatory variables are shown in Table 3. The prevalence of depressive symptoms was significantly higher among the oldest age group (52.7%), females (48.9%), widowed (51.6%), illiterate (43.9%), at the lowest bracket of family income (62.1%), those living alone (68.4%), and receiving COVID-19-related information from health workers (62.5%). The prevalence of depressive symptoms was also higher among the participants who had memory or concentration problems (58.4%), concerns about the pandemic (46.1%), overwhelmed by the pandemic (47.3%), and those facing difficulty earning (49.3%) and getting medicines during the pandemic (59.6%).
Table 3.
Depressive symptoms and bivariate analysis (n = 1032)
| Characteristics | n | %depressed | P |
|---|---|---|---|
| Overall | 1032 | 40.1 | |
| Age (year) | |||
| 60—69 | 803 | 37.1 | 0.001 |
| 70–79 | 174 | 50.0 | |
| ≥ 80 | 55 | 52.7 | |
| Sex | |||
| Male | 676 | 35.5 | < 0.001 |
| Female | 356 | 48.9 | |
| Marital status | |||
| Married | 840 | 37.5 | < 0.001 |
| Widowed | 192 | 51.6 | |
| Literacy | |||
| Illiterate | 602 | 43.9 | 0.004 |
| Literate | 430 | 34.9 | |
| Family size | |||
| ≤ 4 | 318 | 41.2 | 0.637 |
| > 4 | 714 | 39.6 | |
| Family monthly income (BDT1) | |||
| < 5000 | 145 | 62.1 | < 0.001 |
| 5000–10,000 | 331 | 37.8 | |
| > 10,000 | 556 | 35.8 | |
| Residence | |||
| Urban | 269 | 36.4 | 0.152 |
| Rural | 763 | 41.4 | |
| Current occupation | |||
| Currently employed | 419 | 37.0 | 0.091 |
| Unemployed/retired | 613 | 42.3 | |
| Living arrangement | |||
| Living with other family members | 953 | 37.8 | < 0.001 |
| Living alone | 79 | 68.4 | |
| Financial dependency on family for living | |||
| No | 329 | 32.5 | 0.001 |
| Yes | 703 | 43.7 | |
| Walking time to the nearest health centre | |||
| < 30 min | 508 | 35.6 | 0.004 |
| ≥ 30 min | 524 | 44.5 | |
| Problem in memory or concentration | |||
| No problem | 782 | 34.3 | < 0.001 |
| Low memory or concentration | 250 | 58.4 | |
| Pre-existing medical conditions | |||
| No | 424 | 27.6 | < 0.001 |
| Yes | 608 | 48.9 | |
| Feeling of loneliness | |||
| Hardly | 590 | 22.4 | < 0.001 |
| Sometimes/often | 442 | 63.8 | |
| Feeling isolated from others | |||
| Hardly | 636 | 23.6 | < 0.001 |
| Sometimes/often | 396 | 66.7 | |
| Feeling concerned about COVID-19 | |||
| Hardly | 299 | 25.4 | < 0.001 |
| Sometimes/often | 733 | 46.1 | |
| Overwhelmed by COVID-19 | |||
| Hardly | 370 | 26.5 | < 0.001 |
| Sometimes/often | 647 | 47.3 | |
| Difficulty in getting food during COVID-19 | |||
| No | 553 | 29.5 | < 0.001 |
| Yes | 447 | 51.2 | |
| Difficulty in getting medicine during COVID-19 | |||
| No | 733 | 32.2 | < 0.001 |
| Yes | 240 | 59.6 | |
| Difficulty in earning during COVID-19 | |||
| No | 340 | 22.7 | < 0.001 |
| Yes | 570 | 49.3 | |
| Difficulty receiving routine medical care during COVID-19 | |||
| No | 644 | 30.6 | < 0.001 |
| Yes | 281 | 59.8 | |
| Frequency of communication during COVID-19 | |||
| Same as previous | 598 | 37.8 | 0.074 |
| Less than previous | 434 | 43.3 | |
| *Source of COVID-19-related information | |||
| Radio/television | 857 | 37.5 | < 0.001 |
| Health workers | 96 | 62.5 | < 0.001 |
| Friends/family/neighbours | 735 | 36.6 | < 0.001 |
| Received any financial support (Government or non-government) during COVID-19 | |||
| No | 764 | 36.3 | < 0.001 |
| Yes | 268 | 51.1 | |
1BDT stands for Bangladesh taka and 1 BDT ~ 84.7 US dollars
*Multiple responses
Factors associated with depressive symptoms
Table 4 shows the factors associated with depressive symptoms in the final adjusted model, and Annex 1 shows the model diagnostics. Depressive symptoms were associated with monthly family income, living arrangements, dependency on the family for living, proximity to the health facility, pre-existing medical conditions, communication frequency with friends/family during the pandemic, feeling lonely and isolated, and recipient of financial support during COVID-19.
Table 4.
Factors associated with depressive symptoms among the participants (N = 1032)
| Characteristics | aOR | 95% CI | P |
|---|---|---|---|
| Monthly family income (BDT1) | |||
| < 5,000 | Ref | ||
| 5000–10,000 | 0.57 | 0.31–1.04 | 0.066 |
| > 10,000 | 0.42 | 0.23–0.76 | 0.004 |
| Living arrangements | |||
| Living with other family members | Ref | ||
| Living alone | 2.11 | 1.11–4.01 | 0.022 |
| Financial dependency on family for living | |||
| No | Ref | ||
| Yes | 1.64 | 1.12–2.40 | 0.011 |
| Walking time to the nearest health centre | |||
| < 30 min | Ref | ||
| ≥ 30 min | 1.53 | 1.08–2.17 | 0.016 |
| Memory or concentration problem | |||
| No problem | Ref | ||
| Low memory or concentration | 1.47 | 0.98–2.20 | 0.060 |
| Pre-existing medical conditions | |||
| No | Ref | ||
| Yes | 1.91 | 1.31–2.80 | 0.001 |
| Difficulty in earning during COVID-19 | |||
| No | Ref | ||
| Yes | 1.48 | 0.97–2.26 | 0.067 |
| Difficulty in getting medicine during COVID-19 | |||
| No | Ref | ||
| Yes | 1.47 | 0.94–2.30 | 0.093 |
| Difficulty receiving routine medical care during COVID-19 | |||
| No | Ref | ||
| Yes | 1.43 | 0.90–2.27 | 0.129 |
| Frequency of communication during COVID-19 | |||
| Same as previous | Ref | ||
| Less than previous | 1.55 | 1.07–2.26 | 0.022 |
| Feeling of loneliness | |||
| Hardly | Ref | ||
| Sometimes/often | 2.25 | 1.47–3.45 | < 0.001 |
| Feeling isolated from others | |||
| Hardly | Ref | ||
| Sometimes/often | 2.45 | 1.62–3.70 | < 0.001 |
| *Radio/television as the source of COVID-19 information | |||
| No | Ref | ||
| Yes | 0.63 | 0.37–1.06 | 0.079 |
| Received financial support during COVID-19 | |||
| No | Ref | ||
| Yes | 1.46 | 1.01–2.13 | 0.047 |
aOR adjusted odds ratio, CI confidence interval, Ref reference
1BDT stands for Bangladesh taka and 1 BDT ~ 84.7 US dollars
*Multiple responses
We found that the participants in the highest income category (> 10,000 BDT) had nearly 60% lower odds of depressive symptoms than those in the lowest income bracket (aOR = 0.42, 95% CI 0.23–0.76). Financial dependency, as indicated by dependency on family members (aOR = 1.64, 95% CI 1.12–2.40) and receiving financial support during the pandemic (aOR: 1.46, 95% CI 1.01–2.13), was associated with higher odds of depressive symptoms. Participants with pre-existing medical conditions had 91% higher odds of depressive symptoms (aOR = 1.91, 95% CI 1.31–2.80) and those living at distant (≥ 30 min walking) from health facility had 53% higher odds (aOR = 1.53, 95% CI 1.44–3.06) than their counterparts.
Social isolation, captured in terms of living alone (aOR = 2.11, 95% CI 1.11–4.01), less frequent communication during pandemic (aOR = 1.55, 95% CI 1.07–2.26), perceived loneliness (aOR = 2.25, 95% CI 1.47–3.45), and isolation from others (aOR = 2.45, 95% CI 1.62–3.70), was associated with higher odds of depressive symptoms.
Discussion
To the best of our knowledge, this is the first nationwide study assessing depressive symptoms among the older adults in Bangladesh during this COVID-19 pandemic. Compared to the 2019 pre-pandemic prevalence estimates of 36.9% among Bangladeshi older adults [24], our study reports a 3.2% point increase in depressive symptoms, which could be a proxy measure to suggest the troll of the ongoing pandemic on older adult’s mental health.
The prevalence of depressive symptoms reported in this study is relatively higher compared to pre-pandemic estimates from Bangladesh [25, 30], India [31] and Pakistan [32]. However, a recent online survey among Bangladeshis aged 18 and above, conducted during the COVID-19 pandemic, reported a 47.2% prevalence of depressive symptoms, quantified using Depression Anxiety Stress Scale 21 (DASS 21) [20]. Notably, in that study, almost three in five participants were students and one of the eligibility criteria was Bangladeshi citizens and not explicitly those residing in Bangladesh. Hence, it could be biased by Bangladeshi nationals abroad who are likely to experience greater emotional stress due to changing immigration policies amidst the pandemic, international travel restrictions, and family members' well-being back home. Additionally, we also believe that our prevalence estimates are underreported due to the phone interview technique as participants might have felt it difficult to elaborate and record their responses by phone [33, 34].
The statistically significant correlates in our study could be broadly categorized into three themes: economic status, health status, and social connectedness. Poor socioeconomic factors such as lower family income, financial dependence on family, and receiving financial assistance during the pandemic were associated with higher odds of depressive symptoms. Notably, there is consensus in the literature regarding the protective role of higher SES against depression [25, 26]. The underlying mechanism linking depression with SES is multitude and complex. Higher SES reduces everyday living stress by ensuring better access to daily needs, including food, housing, and transportation. It also means affordability and access to healthcare, including mental health services [35, 36]. SES is also a way to establish social prestige, social network, and self-esteem [37, 38]. Financially self-dependent individuals are endowed with such resources that help to buffer the impact of stress on depression. Relatedly and consistent with previous studies among older populations [25, 26, 28], we found that being distant from a health facility increased the likelihood of depressive symptoms. With the background information that owning a private motor vehicle is within the privileges of the rich in Bangladesh, being distant was an indication of difficulty in accessing health services. During the COVID-19 time, residing far away from health facility also means easily and timely inaccessible diagnostics, preventive, and curative services for COVID-19 and for other conditions which could have further aggravated the stress among our study population given that they are aware of their vulnerability since the news is widespread that both case fatality and severity is more in older people.
Like the cultures of many other South Asian countries, in Bangladesh, older family members are revered and cared for by family members. Nevertheless, abuse and abandonment cases are also increasing, especially when children view their older parents as financial burdens [39, 40]. The lockdown imposed by the Bangladeshi Government to curb COVID-19 spread in the country caused economic turmoil among many Bangladeshi families, which could have also impacted the caregiving and providing for older family members. Thus, our participants financially dependent on family may have experienced changes in family caregiving and increased conflict, which may have impacted their mental well-being [26].
Lack of or inadequate social connectedness, indicated by living alone, less frequent communication with friends and family during the pandemic, and perceived loneliness and isolation, meant increased vulnerability for depressive symptoms, which is in line with previous studies in China, Pakistan, and Bangladesh [25, 41, 42]. There is widespread consensus in the literature that social connectedness causally protects and promotes mental health [43]. Social connectedness impacts mental health through mechanisms involving promoting healthy behaviors, access to health and buffering stress [44, 45]. The unplanned lockdown and social restriction amid the pandemic contributed to the lack of social interactions and family visits, increasing the emotional and psychological stress.
Pre-existing medical conditions were positively associated with depressive symptoms among our participants, which is in line with previous studies that noted higher stress, anxiety, and depression among older adults with non-communicable chronic conditions [46]. Physical and mental health are overlapping domains; poor mental health is a risk factor for chronic physical conditions and vice versa [47, 48]. Both poor physical and mental health have many common risk factors, such as those related to lifestyle, that explain the overlap [49]. Furthermore, in a resource-constrained setting, such as Bangladesh, people with pre-existing medical conditions, who need routine medical check-up and medications, may frequently worry about being unable to access those essential needs [50] and that worry could have been worsened during the pandemic due to prolonged shutdown and transport restriction and subsequent critical shortages of drugs supply and shutdown of health centers [51]. In the light that people with pre-existing medical conditions are vulnerable to COVID-19-related deaths [16], it is logical to assume that our participants with an underlying condition are at more risk of adverse health outcomes.
Policy implications
The findings of the current study, also supported by previous studies documenting highly prevalent depression among older Bangladeshis, have significant policy implications for combating and preventing depressive symptoms among older adults in Bangladesh, both during and after the COVID-19 pandemic. Our findings also suggest the need of psychosocial support for older adults from low-income families and living alone was at risk. Additionally, existing mobile telehealth facilities may be expanded to include targeted psychological counseling to the older adults who are poor, having pre-existing non-communicable chronic conditions, who depend on family caregiving and lives at distant from public health care facility. Increasing awareness of mental health issues among family members may be important to identify symptoms and encourage treatment-seeking and medical adherence, and open dialogues on depression to reduce stigma. Finally, to sum up, the government of Bangladesh should call on the findings of this study to achieve the Sustainable Development Goals (2015–2030) aimed to reduce mental health problems through promotion and prevention, and providing comprehensive and social care in community-based settings [52].
Strengths and limitations of the study
This is the first nationwide study covering all the eight administrative divisions of the country and providing an insight into prevalent depressive symptoms among Bangladeshi older adults amid this COVID-19 pandemic. However, our study has some limitations, as well. First, we prepared our sampling frame based on the available household-level information in our data repository; thus, selection bias is possible. Second, in the absence of pre-pandemic estimates, we cannot assert that the increased prevalence of depressive symptoms noted in our study could be attributed to the COVID-19 pandemic.
Conclusion
The present study found a high prevalence of depressive symptoms, amidst this pandemic, among older adults in Bangladesh, which needs urgent attention from stakeholders. Various associated factors could be intervened, managed, and solved by taking appropriate measures; otherwise, the burden of depression may lead to a high cause of cognitive dysfunction among Bangladeshi older adults. We also suggest the need for screening of depressive symptoms among the most vulnerable group, such as people with pre-existing medical conditions where health care providers can intervene to avert the worsening of health condition.
Acknowledgements
We acknowledge the role of Md. Zahirul Islam, Project Associate, ARCED Foundation; Sadia Sumaia Chowdhury, Program Manager, ARCED Foundation and Shakil Al Mamun, Senior Officer, Data Management, ARCED Foundation for their all-out support in data collection and data management for the study.
Appendix 1
See Fig. 1
Fig. 1.
The area under the curve (AUC) plot
Author contributions
SKM, AMI and UNY conceived and designed of the study. SKM, MBH and AMI carried out the data analysis. SKM, AMI, MBH, UNY, SG, MAR, and NMI contributed in writing the first draft of the manuscript. SG, UNY and RH commented extensively on the draft of the manuscript to finalize it. All authors read and approved the final version of the manuscript.
Funding
This research was not funded.
Compliance with ethical standards
Conflict of interest
The authors have no conflict of interest to disclose.
Ethics approval
The institutional review board of the Institute of Health Economics, University of Dhaka, Bangladesh, approved the study protocol (Ref: IHE/2020/1037), and the guidelines of the Declaration of Helsinki were followed in every stage of the study.
Consent to participate
All participants enrolled in the study provided voluntary verbal informed consents.
Availability of data and material
The data are available on reasonable request from the corresponding author.
References
- 1.Dhama K, Patel SK, Kumar R, Rana J, Yatoo MI, Kumar A, Tiwari R, Dhama J, Natesan S, Singh RJ. Geriatric population during COVID-19 pandemic: problems, considerations, exigencies and beyond Head Title: Geriatrics during COVID-19 pandemic. Front Public Health. 2020;8:562. doi: 10.3389/fpubh.2020.574198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.BBS . Elderly population in Bangladesh: current features and future perspectives. Dhaka: Banglaedsh Bureau of Statistics Ministry of Bangladesh, Government of Bangladesh; 2015. [Google Scholar]
- 3.United Nations (2019) World population prospects 2019. Accessed 19/11/2020
- 4.World Health Organization (2017) Mental health of older adults. https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults. Accessed 19 Nov 2020
- 5.World Health Organization (2020) The World Health Report 2001: mental disorders affect one in four people. https://www.who.int/news/item/28-09-2001-the-world-health-report-2001-mental-disorders-affect-one-in-four-people. Accessed 03 Nov 2020
- 6.James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, Abbastabar H, Abd-Allah F, Abdela J, Abdelalim A. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet. 2018;392(10159):1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patel V. Mental health in low-and middle-income countries. Br Med Bull. 2007;81(1):81–96. doi: 10.1093/bmb/ldm010. [DOI] [PubMed] [Google Scholar]
- 8.Worldometer (2020) COVID-19 coronavirus pandemic. https://www.worldometers.info/coronavirus/. Accessed 18 Aug 2020
- 9.Rubin GJ, Potts HWW, Michie S. The impact of communications about swine flu (influenza A H1N1v) on public responses to the outbreak: results from 36 national telephone surveys in the UK. Health Technol Assess. 2010;14(34):183–266. doi: 10.3310/hta14340-03. [DOI] [PubMed] [Google Scholar]
- 10.Sim K, Chan YH, Chong PN, Chua HC, Soon SW. Psychosocial and coping responses within the community health care setting towards a national outbreak of an infectious disease. J Psychosom Res. 2010;68(2):195–202. doi: 10.1016/j.jpsychores.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Bortel T, Basnayake A, Wurie F, Jambai M, Koroma AS, Muana AT, Hann K, Eaton J, Martin S, Nellums LB. Psychosocial effects of an Ebola outbreak at individual, community and international levels. Bull World Health Organ. 2016;94(3):210. doi: 10.2471/BLT.15.158543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66:317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- 13.Hossain MM, Hasan MT, Sultana A, Faizah F. New mental health act in Bangladesh: unfinished agendas. The Lancet Psychiatry. 2019;6(1):e1. doi: 10.1016/S2215-0366(18)30472-3. [DOI] [PubMed] [Google Scholar]
- 14.Xiang Y-T, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, Ng CH. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Biswas T, Townsend N, Islam MS, Islam MR, Gupta RD, Das SK, Al Mamun A. Association between socioeconomic status and prevalence of non-communicable diseases risk factors and comorbidities in Bangladesh: findings from a nationwide cross-sectional survey. BMJ open. 2019;9(3):e025538. doi: 10.1136/bmjopen-2018-025538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yadav UN, Rayamajhee B, Mistry SK, Parsekar SS, Mishra SK. A syndemic perspective on the management of non-communicable diseases amid the COVID-19 pandemic in low-and middle-income countries. Front Public Health. 2020;8:508. doi: 10.3389/fpubh.2020.00508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu B. Social isolation and loneliness among older adults in the context of COVID-19: a global challenge. Global Health Res Policy. 2020;5(1):1–3. doi: 10.1186/s41256-020-00154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheruvu VK, Chiyaka ET. Prevalence of depressive symptoms among older adults who reported medical cost as a barrier to seeking health care: findings from a nationally representative sample. BMC Geriatr. 2019;19(1):192. doi: 10.1186/s12877-019-1203-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Islam MA, Barna SD, Raihan H, Khan MNA, Hossain MT. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: a web-based cross-sectional survey. PLoS ONE. 2020;15(8):e0238162. doi: 10.1371/journal.pone.0238162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al Zubayer A, Rahman ME, Islam MB, Babu SZD, Rahman QM, Bhuiyan MRAM, Khan MKA, Chowdhury MAU, Hossain L, Habib RB. Psychological states of Bangladeshi people four months after the COVID-19 pandemic: an online survey. Heliyon. 2020;6(9):e05057. doi: 10.1016/j.heliyon.2020.e05057. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 21.Peyman N, Olyani S. Iranian older adult's mental wellbeing during the COVID-19 epidemic. Asian J Psychiatry. 2020;54:102331. doi: 10.1016/j.ajp.2020.102331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vahia VN, Shah AB (2020) COVID-19 pandemic and mental health care of older adults in India. Int Psychogeriatr 1–3 [DOI] [PMC free article] [PubMed]
- 23.Gyasi RM (2020) COVID-19 and mental health of older Africans: an urgency for public health policy and response strategy. Int Psychogeriatr 1–6 [DOI] [PMC free article] [PubMed]
- 24.Disu TR, Anne NJ, Griffiths MD, Mamun MA. Risk factors of geriatric depression among elderly Bangladeshi people: a pilot interview study. Asian J Psychiatry. 2019;44:163–169. doi: 10.1016/j.ajp.2019.07.050. [DOI] [PubMed] [Google Scholar]
- 25.Rahman MS, Rahman MA, Ali M, Rahman MS, Maniruzzaman M, Yeasmin MA, Ahmed NAMF, Abedin MM, Islam SMS. Determinants of depressive symptoms among older people in Bangladesh. J Affect Disord. 2020;264:157–162. doi: 10.1016/j.jad.2019.12.025. [DOI] [PubMed] [Google Scholar]
- 26.Yadav UN, Thapa TB, Mistry SK, Pokhrel R, Harris MF. Socio-demographic characteristics, lifestyle factors, multi-morbid conditions and depressive symptoms among Nepalese older adults. BMC Psychiatry. 2020;20(1):1–9. doi: 10.1186/s12888-020-02680-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.El-Gilany A-H, Elkhawaga GO, Sarraf BB. Depression and its associated factors among elderly: a community-based study in Egypt. Arch Gerontol Geriatr. 2018;77:103–107. doi: 10.1016/j.archger.2018.04.011. [DOI] [PubMed] [Google Scholar]
- 28.Liu Q, Cai H, Yang LH, Xiang Y-B, Yang G, Li H, Gao Y-T, Zheng W, Susser E, Shu X-O. Depressive symptoms and their association with social determinants and chronic diseases in middle-aged and elderly Chinese people. Sci Rep. 2018;8(1):1–11. doi: 10.1038/s41598-018-22175-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17(1):37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 30.Wahlin Å, Palmer K, Sternäng O, Hamadani JD, Kabir ZN. Prevalence of depressive symptoms and suicidal thoughts among elderly persons in rural Bangladesh. Int Psychogeriatr. 2015;27(12):199. doi: 10.1017/S104161021500109X. [DOI] [PubMed] [Google Scholar]
- 31.Pilania M, Yadav V, Bairwa M, Behera P, Gupta SD, Khurana H, Mohan V, Baniya G, Poongothai SJBPH. Prevalence of depression among the elderly (60 years and above) population in India, 1997–2016: a systematic review and meta-analysis. BMC Public Health. 2019;19(1):832. doi: 10.1186/s12889-019-7136-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mubeen SM, Henry D, Qureshi SN. Prevalence of depression among community dwelling elderly in Karachi, Pakistan. Iran J Psychiatry Behav Sci. 2012;6(2):84. [PMC free article] [PubMed] [Google Scholar]
- 33.Turner CF, Villarroel MA, Rogers SM, Eggleston E, Ganapathi L, Roman AM, Al-Tayyib A. Reducing bias in telephone survey estimates of the prevalence of drug use: a randomized trial of telephone audio-CASI. Addiction. 2005;100(10):1432–1444. doi: 10.1111/j.1360-0443.2005.01196.x. [DOI] [PubMed] [Google Scholar]
- 34.Herath HMM, Weerasinghe NP, Weerarathna TP, Hemantha A, Amarathunga A. Potential use of telephone-based survey for non-communicable disease surveillance in Sri Lanka. BMC Public Health. 2017;17(1):984. doi: 10.1186/s12889-017-4993-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Surachman A, Wardecker B, Chow S-M, Almeida D. Life course socioeconomic status, daily stressors, and daily well-being: examining chain of risk models. J Gerontol Ser B. 2019;74(1):126–135. doi: 10.1093/geronb/gby014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baum A, Garofalo JP, Yali AM. Socioeconomic status and chronic stress: does stress account for SES effects on health? Ann N Y Acad Sci. 1999;896(1):131–144. doi: 10.1111/j.1749-6632.1999.tb08111.x. [DOI] [PubMed] [Google Scholar]
- 37.Twenge JM, Campbell WK. Self-esteem and socioeconomic status: a meta-analytic review. Personal Soc Psychol Rev. 2002;6(1):59–71. doi: 10.1207/S15327957PSPR0601_3. [DOI] [Google Scholar]
- 38.Manstead ASR. The psychology of social class: how socioeconomic status impacts thought, feelings, and behaviour. Br J Soc Psychol. 2018;57(2):267–291. doi: 10.1111/bjso.12251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Farid S. Elder abuse and neglect in Bangladesh: understanding issues, associated factors and consequences. Family Med Primary Care Rev. 2017;2:123–127. doi: 10.5114/fmpcr.2017.67865. [DOI] [Google Scholar]
- 40.Barikdar A, Ahmed T, Lasker SP. The situation of the elderly in Bangladesh. Banglandesh J Bioeth. 2016;7(1):27–36. doi: 10.3329/bioethics.v7i1.29303. [DOI] [Google Scholar]
- 41.Manandhar K, Risal A, Shrestha O, Manandhar N, Kunwar D, Koju R, Holen A. Prevalence of geriatric depression in the Kavre district, Nepal: findings from a cross sectional community survey. BMC Psychiatry. 2019;19(1):271. doi: 10.1186/s12888-019-2258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang J, Zhao X. Family functioning and social support for older patients with depression in an urban area of Shanghai China. Arch Gerontol Geriatr. 2012;55(3):574–579. doi: 10.1016/j.archger.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 43.Perkins JM, Subramanian SV, Christakis NA. Social networks and health: a systematic review of sociocentric network studies in low-and middle-income countries. Soc Sci Med. 2015;125:60–78. doi: 10.1016/j.socscimed.2014.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Newman MG, Zainal NH. The value of maintaining social connections for mental health in older people. The Lancet Public Health. 2020;5(1):e12–e13. doi: 10.1016/S2468-2667(19)30253-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Saeri AK, Cruwys T, Barlow FK, Stronge S, Sibley CG. Social connectedness improves public mental health: Investigating bidirectional relationships in the New Zealand attitudes and values survey. Aust N Z J Psychiatry. 2018;52(4):365–374. doi: 10.1177/0004867417723990. [DOI] [PubMed] [Google Scholar]
- 46.Gorrochategi MP, Munitis AE, Santamaria MD, Etxebarria NO (2020) Stress, anxiety, and depression in people aged over 60 in the COVID-19 outbreak in a sample collected in Northern Spain. Am J Geriatr Psychiatry [DOI] [PMC free article] [PubMed]
- 47.Clarke DM, Currie KC. Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence. Med J Aust. 2009;190:S54–S60. doi: 10.5694/j.1326-5377.2009.tb02471.x. [DOI] [PubMed] [Google Scholar]
- 48.De Hert M, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen DAN, Asai I, Detraux J, Gautam S, Möller H-J, Ndetei DM. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10(1):52. doi: 10.1002/j.2051-5545.2011.tb00014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yadav UN, Tamang MK, Thapa TB, Hosseinzadeh H, Harris MF, Yadav KK. Prevalence and determinants of frailty in the absence of disability among older population: a cross sectional study from rural communities in Nepal. BMC Geriatr. 2019;19(1):283. doi: 10.1186/s12877-019-1290-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mazumder H, Murshid M-E, Faizah F, Hossain MM. Geriatric mental health in Bangladesh: a call for action. Int Psychogeriatr. 2020;32(5):667–668. doi: 10.1017/S1041610220000423. [DOI] [PubMed] [Google Scholar]
- 51.Anwar S, Nasrullah M, Hosen MJ (2020) COVID-19 and Bangladesh: challenges and how to address them. Front Public Health 8 [DOI] [PMC free article] [PubMed]
- 52.United Nations take action for the sustainable development goals. https://www.un.org/sustainabledevelopment/sustainable-development-goals/. Accessed 23 Nov 2020