Abstract
Purpose of Review
The last decade has seen a boom in hip arthroscopy with refined indications. Improved understanding of pathoanatomy and disease progression has allowed for the development of advanced techniques. Labral reconstruction has been developed to substitute a non-functional or absent labrum. It has become an important technique in the armamentarium of high-volume arthroscopic hip surgeons.
Recent Findings
Basic science studies have improved understanding of hip biomechanics in the presence and absence of a labrum with a labral reconstruction allowing for reconstitution of normalcy. Current techniques have shown success with autograft and allograft tissue options. While autograft tissue allows for easy access intra-operatively and maintains patient biology, donor site morbidity is possible. Allografts negate donor site morbidity and allow for an abundance of tissue but can be resource-intensive and face availability concerns. Recent studies support outcomes of labral reconstructions using both autograft and allograft. Promising results have also allowed for performing labral reconstruction in a primary setting.
Summary
Labral reconstruction can be successfully performed using both autograft and allograft. Patient biology should be respected, and native hip biomechanics restored. The literature is plentiful for appropriate surgical decision-making allowing the surgeon with multiple graft choices depending on training, experience, and resources.
Keywords: Hip labrum, Hip arthroscopy, Labral reconstruction, Graft options, Technique
Introduction
Almost a century after its first description [1], hip arthroscopy has surged in popularity worldwide seeing increases of 600% in the USA [2] and 727% in England in the last two decades [3]. With this tremendous momentum, it is projected to increase by 1388% by 2023 based on some estimates [3]. This rapid growth has been a result of better understanding and recognition of pathology, improved investigations and arthroscopic instrumentation, and surgical innovation.
The acetabular labrum has been the cornerstone of the understanding of hip joint biomechanics and progression of disease [4–11]. Labral tears have been one of the leading pathologies identified in patients with hip pain and during hip arthroscopy [12]. Although, the prevalence of labral pathology is not well understood, the crucial role of the labrum in hip biomechanics is well established [8, 9, 13]. Furthermore, there has been an evolution since the turn of the century in its management during hip arthroscopy. While initial studies are reported on labral debridement [14], the focus has shifted towards labral repair/refixation in an effort to preserve and restore anatomy [15–17]. However, in recent years, there has been a paradigm shift towards labral augmentation and reconstruction to address deficient and irreparable labra, respectively [13, 18–20]. The initial favorable results have been convincing insomuch that labral reconstruction is being considered the treatment of choice in revision hip arthroscopy [21] particularly as surgeons look for a solution in patients doing poorly following labral debridement. Some authors have also advocated for its use in primary hip arthroscopy [22, 23].
Sierra and Trousdale first described labral reconstruction as part of a surgical hip dislocation using a ligamentum teres (LT) autograft [24]. Philippon et al. [25] thereafter described the first arthroscopic labral reconstruction using iliotibial band (ITB) autograft. This has since been adopted by open and arthroscopic surgeons alike and spawned myriad different techniques with various graft options [19, 25–30, 31••]. The scientific community has decisively taken notice with four systematic reviews on the topic in the last 6 years [32–35]. As more is known about this procedure, it has established itself as the new frontier in hip preservation and thus should be part of the arsenal of the experienced hip preservation surgeons. The purpose of the current review is to elucidate the different graft options available for acetabular labral reconstruction, their results in the literature, and the authors’ preferred technique of labral reconstruction.
Acetabular Labrum—Anatomy, Role, and Biomechanics
The acetabular labrum is a horseshoe-shaped soft tissue structure of the hip attached to the acetabular rim circumferentially with inferior attachments to the transverse acetabular ligament (TAL) [5, 36]. It is triangular in cross section with the articular surface made of fibrocartilage and the non-articular surface comprising of dense connective tissue [5]. The vascular contribution is from a vascular anastomotic ring surrounding the capsular attachment; however, it attenuates towards the articular surface [36]. Its innervation consists of multiple sensory nerves and receptors [7, 37] differentiating it from the knee meniscus and supporting the theory of a labral tear potentiating hip pain [36, 38].
The labrum plays a key role in improving hip stability and cartilage consolidation with its suction seal effect resisting distractive forces and forming a pressurized layer of synovial fluid that can evenly distribute compressive loads, thereby reducing cartilage stress and strain [5]. Philippon et al. [8] showed in a cadaveric study that partial labral resection decreased intra-articular fluid pressures and restored them with labral repair and reconstruction. In a follow-up study, Nepple et al. [9] showed the same effects on distractive forces with labral resection decreasing distractive strength and labral reconstruction vastly improving hip distractibility.
Indications for Labral Reconstruction
The management options of labral pathology have been described in a treatment algorithm by Domb et al. [38]. The indications for labral reconstruction have evolved. In a recent consensus study, Maldonado et al. [39] surveyed 12 high-volume hip surgeons performing labral reconstructions and reported 100% of them would reconstruct in revision cases with irreparable labral tears and the majority would reconstruct in primary cases with poor-quality labral tissue and calcified labrum. Other studies have broadened indications to increased age, non-functional labrum, dense capsulolabral adhesions, and hips with 0–1 Tonnis grade on radiographs [34, 40].
Graft Options
There are various techniques of labral reconstruction broadly divided into segmental and circumferential reconstruction. The original technique was devised to address a segment of labrum either absent or pathological. Recent literature has moved towards circumferential reconstruction, which is a misnomer as the labrum does not envelope the acetabulum circumferentially but instead covers it from one end of the TAL to the other. The authors’ preference is to refer to circumferential reconstruction as a large segmental or total labral reconstruction. The graft options can be divided into autografts and allografts. The various options, their advantages and disadvantages, and results in the literature have been documented in Tables 1 and 2, respectively. A significant difference in patient-reported outcome scores between autograft and allograft labral reconstructions has not been identified; however, one study reported better patient satisfaction with allograft use compared to autograft [41]. Furthermore, multiple grafts have similar cyclic elongation behavior as the native labrum, and hence, there are multiple viable options for this procedure [42].
Table 1.
Autograft options for labral reconstruction
| Graft type | Advantages | Disadvantages | Outcomes |
|---|---|---|---|
| Ligamentum teres [24, 26] | 1. Harvest is part of the approach in open procedure |
1. Unknown implications to hip biomechanics 2. No arthroscopic equivalent described 3. May require augmentation by another graft |
• UCLA score 8.5 |
| Hip capsule [44, 48] |
1. Local tissue 2. No donor site morbidity (pain, scarring, and blood loss) in patients where a separate capsular procedure (closure/plication) is not desired/indicated |
1. Limited to small labral defects (typically for 10 to 20 mm) 2. Precludes any capsular procedure (closure/plication) if indicated 3. Less robust graft source |
• MHHS 91, HOS-ADL 86, HOS-SS = 75 |
| Indirect head of rectus femoris [30, 45–48] |
1. Local tissue 2. No graft preparation necessary 3. No donor site morbidity 4. Preserved vascularity |
1. Not ideal for large segments of labral deficiencies 2. Lacks basic science support for recreation of suction seal and distractibility of the femoral head |
• MHHS 84 [45] • MHHS 98 [30] • MHHS 75, HOS-ADL 91, HOS-SS 83 [48] • MHHS 93 [47] |
| Iliotibial band [25, 49–52] |
1. Proximity to anterolateral portal 2. Large series of patients and midterm outcomes reported on using this graft making its results more scientifically familiar |
1. Soft tissue complications at harvest site 2. Extra incision and its effects on cosmesis |
• MHHS 85, HOS-ADL 90, HOS-SS 75, WOMAC 9, SF-12 P 53 [51] • Conversion to THA 13.2% at minimum 2-year follow-up [51] |
| Gracilis [19, 28, 53] |
1. Ease of harvest for most surgeons 2. Spare tissue to allow for reuse in the case of a technical problem |
1. Patient positioning and draping intra-operatively 2. Additional pain generator distant from site of original surgery 3. Soft tissue complications at harvest site 4. Extra incision and its effects on cosmesis |
• NAHS 92 [28] • MHHS 75, HOS-ADL 81, HOS-SS 65, NAHS = 78 [19] |
| Quadriceps [29] | 1. Potential biomechanical properties (this is unsubstantiated for the acetabular labrum in the literature) |
1. Patient positioning and draping intra-operatively 2. Additional pain generator distant from site of original surgery 3. Soft tissue complications at harvest site 4. Extra incision and its effects on cosmesis 5. Need to rehabilitate the knee after a quadriceps harvest 6. Possibility of a graft-to-recipient length mismatch if a total reconstruction is desired |
Case report with 3-month follow-up • MHHS, 83, WOMAC 15 |
MHHS, Modified Harris Hip Score; HOS-ADL, Hip Outcome Score–Activities of Daily Living subscale; HOS-SS, Hip Outcome Score–Sports Specific subscale; NAHS, Non-arthritic Hip Score; WOMAC, Western Ontario and McMaster Universities Osteoarthritis index; SF-12 P, Short Form 12-Item Health Survey physical component; THA, total hip arthroplasty
Table 2.
Allograft options for labral reconstruction
| Graft type | Outcomes |
|---|---|
| Semitendinosus [66] | • OHS 36, HOS 79 |
| Tibialis anterior [31••] |
• MHHS 87, NAHS 86, HOS-SS 78, iHOT-12 7, SF-12 P, 50, SF-12 M 55, VR-12 P 50, VR-12 M 60, VAS 2 • Conversion to THA = 5.4% at mean 16 months postoperatively |
| Iliotibial band [27] |
• MHHS, 88, LEFS 68, VAS 2 • Conversion to THA = 9.9% at mean 15 months postoperatively |
| Tensor fascia lata [63, 64] |
• MHHS 95 [63] • MHHS 85, SF-12 P 49, SF-12 M 56, iHOT-12 68, HOS-ADL 82, HOS-SS 66 [64] |
| Peroneus brevis [65] | • No outcomes reported |
OHS, Oxford Hip Score; MHHS, Modified Harris Hip Score; NAHS, Non-arthritic Hip Score; iHOT, International Hip Outcome Tool; SF-12 P, Short Form 12-Item Health Survey physical component; SF-12 M, Short Form 12-Item Health Survey mental component; LEFS, Lower Extremity Function Score; VR-12 P, Veterans RAND 12-Item Health Survey physical component; VR-12 M, Veterans RAND 12-Item Health Survey mental component; VAS, visual analogue scale; HOS-ADL, Hip Outcome Score–Activities of Daily Living subscale; HOS-SS, Hip Outcome Score–Sports Specific subscale; THA, total hip arthroplasty
Autografts
The major advantages of autografts are maintaining patient biology, no risk of disease transmission, availability, and lower cost. Additionally, Shi et al. [43] showed that autologous tendon tissue has the ability to convert to fibrocartilage in a porcine model. Meanwhile, the donor site morbidity and increased surgical time are concerns depending on the graft. Generally, autografts can be either regional or distant depending on their proximity to the hip. Regional autografts include LT [24, 26], hip capsule [44], indirect head of rectus femoris [30, 45–48], and ITB [25, 49–52]. Distant autografts include gracilis [19, 53] and quadriceps [29] tendons.
A clear function of the LT remains elusive [54]. Its transection is necessary during a surgical dislocation of the hip as described by Ganz [55]. Hence, it served as an obvious choice for a graft for labral reconstruction [24]. The authors reported improved UCLA scores from 5 to 8.2 in five patients in the original study and up to 8.5 in a subsequent study (although pre-operative scores were not presented). The major advantage of this graft is that its harvest is part of the approach to the hip. However, its disadvantages include the need for an open procedure and occasionally requiring further augmentation with a tensor fascia lata (TFL) graft to supplement cases where the LT is not long enough to reconstruct the labral deficiency [26].
Recently, literature has made great strides in the understanding of the hip capsule. Its proximity to the labrum makes it a naturally appealing contender as an autograft. Domb et al. [44] described a technique of using capsular autograft to reconstruct small labral defects. Unfortunately, its use limits the ability to close or plicate the capsule. Locks et al. [48] reported on the results of capsular autografts used in labral reconstruction. In eight patients with a mean age of 36.4 years and a mean follow-up of 71.6 months (minimum follow-up of 12 months), the authors showed a mean improvement in the Modified Harris Hip Score (MHHS) from 68 to 91, in the Hip Outcome Score–Activities of Daily Living (HOS-ADL) subset from 71 to 86, and in Hip Outcome Score–Sports Subscale (HOS-SS) from 54 to 75.
The indirect head of rectus femoris tendon can also offer a local source of autograft. Sampson [45] described this technique in 2015 which involved splitting the indirect head of rectus femoris tendon longitudinally to its fibers depending on the desired width of the neo-labrum followed by securing the graft to the acetabular rim. Improvements in MHHS from 65 pre-operatively to 84 postoperatively were reported in 31 patients. A modification of this technique was later reported by Sharfman et al. [46]. Amar et al. reported on the results of this technique in 22 patients (median age of 43 years) with improved MHHS scores from 67 pre-operatively to 98 postoperatively at a median follow up of 36.2 months (minimum 24-month follow-up). Rathi et al. [47] have reported early results showing improvement in MHHS scores from 56 pre-operatively to 93 postoperatively at average 15-month follow-up. Locks et al. [48] also reported improvement in three patients in their study that underwent reconstruction using this autograft. Advantages include the local presence of this tissue during hip arthroscopy making it easy to harvest without donor site morbidity, no need for graft preparation, and a vascularized graft with an intact distal blood supply. However, with a finite length of tendon available, it may not be suitable for large segment labral reconstructions. It is difficult to line the rectus graft up with the remaining labrum. Additionally, it lacks basic science support of reconstituting the suction seal and distractibility of the femoral head.
The ITB was the graft of choice for the first described arthroscopic labral reconstruction by Philippon et al. [25]. Its proximity to the arthroscopic portals allows harvest of a rectangular portion of the ITB through an incision distal to the anterolateral portal after which the graft is tubularized for placement in the joint. However, soft tissue complications at the harvest site are possible [52]. The outcomes of this graft have been the most reported in the literature with midterm results. In the initial article, Philippon et al. [25] reported on their results in 47 patients at mean follow-up of 18 months (minimum 12 months), showing significant improvements in MHHS from 62 pre-operatively to 85 postoperatively. Four patients (9%) underwent conversion to total hip arthroplasty (THA). Geyer et al. [50] published a follow-up study on the same population in 2013 and illustrated a more realistic snapshot of midterm outcomes (between 3 and 6 years postoperatively). Of the 76 patients analyzed, 19 (25%) had progressed to THA at mean 28 months postoperatively. The MHHS showed similar significant improvements as the original study from 59 pre-operatively to 83 postoperatively. A caveat to this patient population is that it was from 2005 to 2008, a time before general guidelines for exclusion of hip arthroscopy were established in arthritic patients [56, 57]. The same institution reported their findings on the same patient population again in 2018 and found older age, two or more previous surgeries, joint space 2 mm or less, and lateral center edge angle less than 25° as factors associated with conversion to THA. [51]. Furthermore, higher pre-operative outcome scores predicted improvement after labral reconstruction. Deshmane et al. [49] described an all-arthroscopic ITB autograft harvesting technique for labral reconstruction in two cases. However, there is paucity in the literature regarding the outcomes of this approach.
Distant autograft usage was popularized by Matsuda [53] who used gracilis autograft in labral reconstruction by harvesting it from the ipsilateral knee in a figure-of-4 position and reported his results in eight patients with an average of 30-month follow-up (minimum 24 months). The Non-arthritic Hip Score (NAHS) improved from 42 pre-operatively to 92 postoperatively. Chandrasekaran et al. [19] reported their results using a mixed cohort of labral reconstructions using gracilis autograft and semitendinosus allografts in 22 patients and found improvements in MHHS from 64 pre-operatively to 75 postoperatively, in HOS-ADL from 64 pre-operatively to 81 postoperatively, in HOS-SS from 42 pre-operatively to 65 postoperatively, and in NAHS from 59 pre-operatively to 78 postoperatively. A substantial advantage of the gracilis autograft harvest is the familiarity of most surgeons with the harvesting technique as it is a commonly used graft for other arthroscopic procedures like an anterior cruciate ligament (ACL) reconstruction. Secondly, there is spare tissue in the case of a technical problem to repeat the process. The disadvantages include the distant nature to the site of surgery (as a challenge from patient positioning and draping intra-operatively, and as an added pain generator postoperatively for patients), soft tissue complications at the harvest site, and cosmesis.
Park and Ko have described the use of quadriceps autograft for labral reconstruction in a case report [29]. The authors noted the advantage of this graft choice akin to that of cruciate ligament reconstructions [58] using quadriceps, primarily being biomechanical compatibility. However, in the opinion of the authors of this review, the biomechanical properties of cruciate ligaments are different from the acetabular labrum. This graft has the same disadvantages as the gracilis autograft and, in addition, includes the burden of rehabilitating the knee due to an operated extensor mechanism. Moreover, Karns et al. [59] reported the mean circumferential (total) length from one arm of the TAL to the other) of the acetabular rim as 15.82 cm and 13.67 cm in male and female cadavers, respectively. Lippe et al. [60] investigated the anatomy of the quadriceps tendon for harvesting and found the maximal possible tendon length to be 9.97 cm. Hence, if a total labral reconstruction is desired, there is a graft-to-recipient length mismatch.
Authors’ Preferred Technique for ITB Autograft Labral Reconstruction
One of the senior authors (MJB) uses this technique for all labral reconstruction. Hip arthroscopy is performed in the lateral position using anterolateral, mid-anterior, and distal anterolateral accessory (DALA) portals. Diagnostic arthroscopy is performed to identify labral insufficiency, a destroyed labrum, labral ossification, or extensive capsulolabral adhesions. The segment to be reconstructed is removed with a radiofrequency wand (Arthrocare supermultivac) and shaver (5.5-mm bone cutter, Smith and Nephew). The narrow bone of the iliopsoas recess is a difficult location to anchor the most anterior portion of the graft. It is the author’s preference to begin the graft at the predictable wider area of bone adjacent the TAL at the 5 o’clock position using the acetabular clock-face system standardized to the right hip.
The DALA portal is used to drill holes to accommodate the knotless anchors (Stryker CinchLock) at 10-mm intervals via a flexible cannula. The most anterior hole is immediately behind the iliopsoas recess. Care must be taken to sound this hole with the nitinol wire to ensure the inner table of the pelvis has not been breached. The most posterior hole is immediately adjacent to the remaining labrum. The number of holes allows for graft sizing by using 10 mm for each hole and adding 30 mm for a larger male hip and 25 mm for a smaller patient. Thus, five holes will require an 80-mm graft in a large male.
The major advantages of this technique are that the ITB is accessible, biologically compatible, and always available. It makes for the ideal choice when allograft is not readily available, too costly, or a labral reconstruction has been decided upon intra-operatively. It also arms the surgeon with a technique in a situation when a need for labral reconstruction is encountered in an unexpected scenario. The sheath of the arthroscope is carefully parked on the acetabular rim and traction is released. The cannula is removed, and the DALA portal is enlarged distally by 35 to 40 mm. Dissection to the ITB is performed taking care not to perforate. A large Cobb elevator is used to expose a 40-mm wide strip of the ITB from 20 mm above the incision to 120 mm below the incision. A 15 blade is used to incise the ITB 5–10 mm posterior to the TFL muscle. The incision is extended both superiorly and inferiorly using a Smillie knife or Metzenbaum scissors. An assessment of the thickness of the ITB can then be made. If thin, a graft width of 25–30 mm is chosen. If thicker, 20 mm will suffice. The second longitudinal incision is made in the ITB. Pott’s angled scissors are used to perform the proximal transverse cut. A graft length of 120 mm is harvested. The quadriceps tendon harvesting transverse cutter (Karl Storz) has 1-cm gradations on the shaft and works well for dividing the graft distally without enlarging the skin incision.
The distal end of the graft is folded back to provide the correct length of graft. It is then tubularized and sewn with a 3–0 Vicryl baseball stitch (Fig. 1). A loop of no. 1 magnum wire (Stryker) is fixed to the double thickness end of the graft with a Kessler suture. The graft is wrapped in a vancomycin-soaked gauze while traction is reapplied.
Fig. 1.
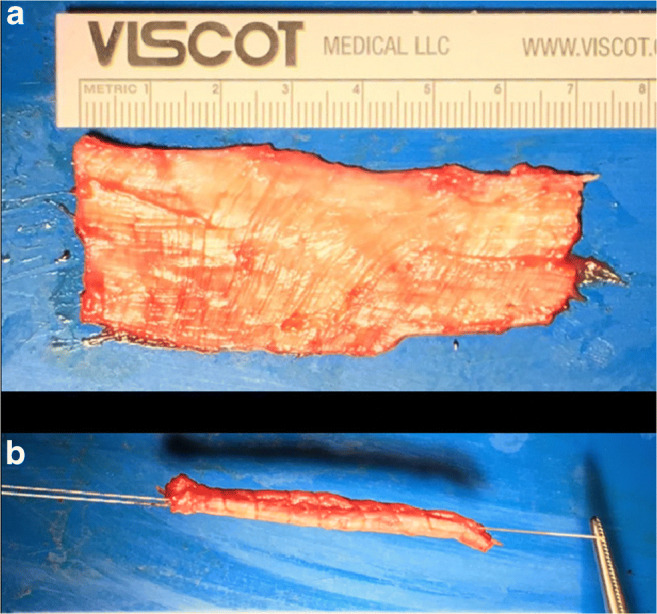
Iliotibial band (ITB) autograft. a Harvested strip of ITB prior to graft preparation. b Tubularized strip of ITB with no. 1 magnum wire (Stryker) suture on the left and 3–0 Vicryl suture from the whip-stitch on the right
The anterolateral portal is checked to ensure it is free of constrictions from the skin to the joint to avoid graft snagging. A 1.4-mm all-suture anchor (Stryker Iconix) is inserted at the 5 o’clock position via the anterolateral portal. One limb of the Iconix suture is passed through the single thickness end of the graft. The graft is introduced via the same portal using a half-hitch which is then completed to a revo knot to dock the graft anteriorly (Fig. 2a). The graft is pushed deep into the joint and held with a grasper. The magnum wire is retrieved via the flexible cannula which has been reintroduced into the DALA portal. The CinchLock Anchor is then used to fix the graft adjacent the native labrum posteriorly (Fig. 2b). The remainder of the repair resembles a standard labral repair employing knotless anchors and labrum base sutures. This ensures a predictable inverted repair that sits firmly against the femoral head when traction is removed (Fig. 2c). Being an autograft, a predictable seamless healing of the graft to the labrum occurs, and hence, further fixation to the native labrum is not required.
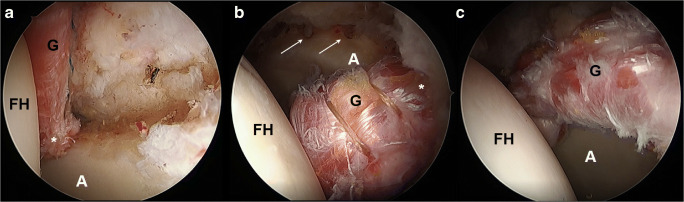
Fig. 2.
Left hip arthroscopy showing the iliotibial band autograft being anchored a anteriorly with the asterisk showing the 5 o’clock position and b posteriorly with the asterisk showing the 11 o’clock position for a segmental labral reconstruction and the arrows showing the pre-drilled holes for anchors to be used to secure the body of the graft to the acetabular rim. c Completed segmental labral reconstruction with the body of the graft anchored to the acetabular rim (A, acetabulum; FH, femoral head; G, graft)
Allografts
Allografts have the luxury of no donor site morbidity, plethora of sizing options, and potential reduction in surgical time. Disadvantages include risk of disease transmission, the economic burden, and possibly longer time to graft incorporation compared to an autograft. Common allografts that have been reported in the literature include semitendinosus [61, 62••], tibialis anterior [31••], ITB [13, 21–23, 27], TFL [63, 64], and peroneus brevis [65]. In general, there has not been any superiority in allograft choice reported in the literature and the authors of this review presume the choice was predominantly made based on reporting authors’ preferences and availability in the studies discussed.
One of the senior authors (BGD) has published on two different arthroscopic techniques using a double-stranded semitendinosus allograft. The first technique was primarily for segmental labral reconstructions [61]. The authors thereafter published their results in combination with some gracilis autografts that have been reported above [19]. The second, more novel, technique was developed for total labral reconstructions [62••]. Using the same technique, but primarily using tibialis anterior allograft, Domb et al. [31••] demonstrated high patient satisfaction in 37 patients with statistically significant multiple patient-reported outcome scores. Majority of patients reached the minimal clinically important difference (MCID) and patient acceptable symptomatic state (PASS) for MHHS and iHOT-12 scores.
Costa Rocha et al. [66] reported on their technique of a total labral reconstruction using fresh frozen semitendinosus allograft at the time of a surgical hip dislocation. In their four-patient case series, at mean 19 months postoperatively, the authors found an improvement in the Oxford Hip Score (OHS) from 30 pre-operatively to 36 postoperatively and in the HOS from 60 pre-operatively to 79 postoperatively.
ITB and TFL allografts have also been used extensively in the literature. White et al. [13, 21–23, 27] have published extensively on the ITB allograft labral reconstruction. In one of their studies, the authors reported on 131 patients undergoing ITB allograft labral reconstruction at minimum 2-year follow-up. Ninety-nine of these patients were primary procedures. A combination of frozen and freeze-dried allografts were used. Thirteen patients required conversion to THA at mean 15 months postoperatively. The MHHS scores improved from 54 pre-operatively to 88 postoperatively. Lower Extremity Function Score (LEFS) improved from 41 pre-operatively to 68 postoperatively [22]. In another study by White et al. [22], the authors undertook a comparison of hips in patients who underwent bilateral hip arthroscopies, one treated with primary labral repair and the other with primary labral reconstruction. They concluded that hips undergoing labral repair were more likely to fail (31%) compared to those undergoing primary reconstruction (0%). These findings have been met with criticism from other authors with the general consensus in most high-volume arthroscopic hip surgeons being that primary labral repair remains the treatment of choice when the labrum is repairable [67]. In a recent study, White et al. [23] published their results in patients undergoing hip arthroscopy over the age of 40 years and found that labral reconstruction led to lower failure rate compared to labral repair and similar outcomes compared to labral repair in patients 30–39 years of age.
TFL allograft has also been used in recent studies. Rathi and Mazek [63] reported their technique in 2017 in ten patients with minimum follow-up of 12 months. There was improvement in MHHS from 58 pre-operatively to 95 postoperatively. Carreira et al. [64] followed with their results on this allograft using a shuttle technique at minimum 2-year follow-up. In their series of 31 patients, the authors reported improvements in from 64 pre-operatively to 85 postoperatively, in SF-12 Physical score from 40 pre-operatively to 49 postoperatively, in SF-12 Mental score from 50 pre-operatively to 56 postoperatively, in iHOT-12 from 36 pre-operatively to 68 postoperatively, in HOS-ADL from 63 pre-operatively to 82 postoperatively, and in HOS-SS from 33 pre-operatively to 66 postoperatively.
Moya et al. [65] described their technique of using the peroneus brevis allograft in an arthroscopic mini-open posterior labral reconstruction. There have not been any outcomes reported on this graft or technique.
Authors’ Preferred Technique for Allograft Labral Reconstruction
This technique has been published by one of the senior authors (BGD) and is briefly described here [31••, 32–61, 62••]. Figure 3 demonstrates an illustration of a total reconstruction using the knotless pull-through technique. Hip arthroscopy is performed in the modified supine position using the anterolateral, mid-anterior, DALA, and posterolateral portals. A previously published algorithm for labral treatment [38] is followed, and when deemed appropriate, a total labral reconstruction from the anterior to posterior points of the TAL is undertaken using a 6.5- to 7.5-mm single-strand tibialis anterior or tibialis posterior allograft. The allograft is whip-stitched on both ends using a no. 2 FiberLoop (Arthrex) suture.
Fig. 3.
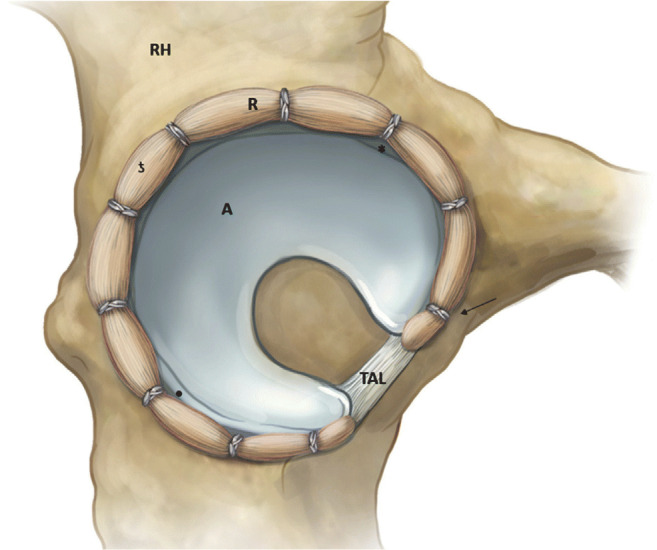
Schematic showing a total labral reconstruction (R) in a right hip (RH) using the pull-through technique with a total of 10 knotless suture anchors (arrow). The asterisk indicates the 3 o’clock position; letter “ƾ” 12 o’clock position; and dot, 9 o’clock position (A, acetabulum; TAL, transverse acetabular ligament) [31••]
Figure 4 shows an irreparable labral tear at diagnostic arthroscopy. The labrum is removed in its entirety. From the mid-anterior portal, the drill for the 2.9-mm PEEK PushLock (Arthrex) is used to create a hole adjacent to the anterior attachment of the TAL. This point of fixation will be used after all of the following Knotless FiberTak (Arthrex) anchors are placed throughout the rest of the acetabular rim until the posterior attachment of the TAL spaced out by 6 to 8 mm. One should be mindful of suture management, which can be done by “parking” the sutures from the anchors using hemostat clamps to the surgical drape in sequential order from the DALA portal.
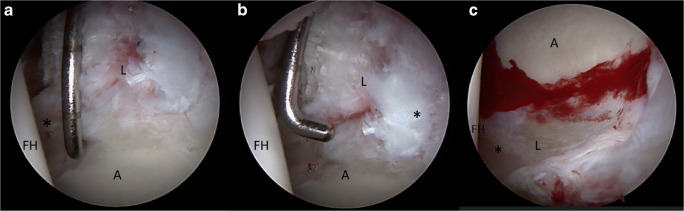
Fig. 4.
Left hip arthroscopy showing an irreparable labral tear (L) with the asterisk marking the a 4 o’clock position, b 12 o’clock position, and c 7 o’clock position (A, acetabulum; FH, femoral head)
The allograft is introduced into the joint through the mid-anterior portal and anchored to the anterior 2.9-mm pilot hole with a PushLock anchor (Arthrex). The rest of the graft is delivered into the joint and pulled through the posterolateral portal using the FiberLoop (Arthrex) suture attached to the posterior end of the graft. While maintaining mild tension to the graft using this posterior FiberLoop (Arthrex) suture, each Knotless FiberTak (Arthrex) anchor is sequentially passed around the graft and tightened to the desired tension to attach the graft to the acetabular rim. Once all anchors have been deployed and the graft securely repaired to the rim, the remainder of the graft is amputated to the desired length using radiofrequency device (Fig. 5). Traction is released and the suction seal is evaluated (Fig. 6).
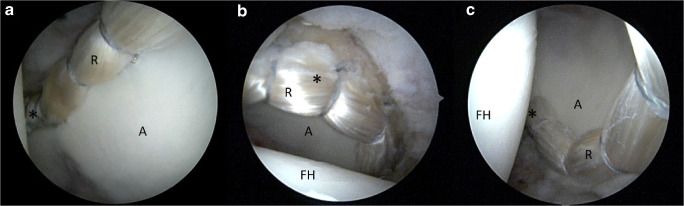
Fig. 5.
Total labral reconstruction (R) in the same hip using tibialis anterior allograft and the knotless pull-through technique. The asterisk marks a the most medial point of fixation at the 4 o’clock position, b the 12 o’clock position, and c the most posterior point of fixation at the 7 o’clock position (A, acetabulum; FH, femoral head)
Fig. 6.
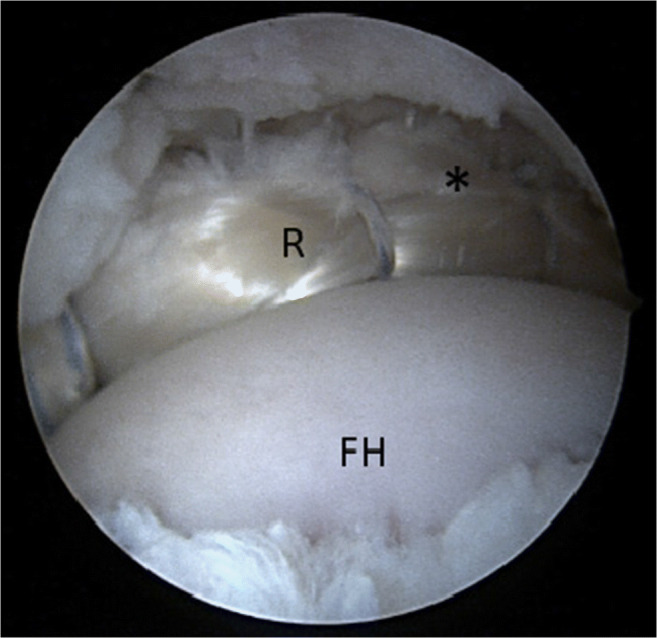
Traction is released, and restoration of labral seal is noted. The asterisk marks the 12 o’clock position (R, reconstructed labrum; FH, femoral head)
This technique has many advantages. Firstly, it eliminates the graft “mismatch” error. As the length of graft can be perfectly matched to the defect every time, measurement of defect size is not required. Secondly, the use of knotless technology makes this technique more reproducible and efficient. Thirdly, the use of allograft would potentially increase patient satisfaction as donor site morbidity [41]. Fourthly, the inherent tubular shape of the tibialis anterior/posterior eliminates the necessity of graft tubularization.
Conclusion
Labral reconstruction is the new frontier in hip arthroscopy. The past decade has seen a rise in advanced arthroscopic techniques and validation in outcomes with longitudinal studies. This continues to be an area of substantial research. The authors have presented various graft options, their advantages and disadvantages, and preferred techniques. However, regardless of which graft or technique is employed, one must be mindful to respect anatomy with a normal suction seal and distractibility with a labral repair where possible, and if not, restore it with a reconstruction. The choice of a graft rests in the hands of the surgeon, his/her training, familiarity, circumstances, and resources.
Compliance with Ethical Standards
Conflict of Interest
Parth Lodhia has nothing to disclose.
Mark O. McConkey has nothing to disclose.
Jordan M. Leith has nothing to disclose.
David R. Maldonado has nothing to disclose.
Matthew J. Brick reports personal fees from Stryker, other from Arthrex, outside the submitted work.
Benjamin G. Domb is the Medical Director of Hip Preservation at St. Alexius Medical Center, the Clinical Instructor at the University of Illinois College of Medicine; is a board member for the American Hip Institute Research Foundation, AANA Learning Center Committee, the Journal of Hip Preservation Surgery, the Journal of Arthroscopy; and has had ownership interests in the American Hip Institute, Hinsdale Orthopedic Associates, Hinsdale Orthopedic Imaging, SCD#3, North Shore Surgical Suites, and Munster Specialty Surgery Center.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Outcomes Research in Orthopedics
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Parth Lodhia, Email: parth.lodhia@ubc.ca.
Mark O. McConkey, Email: mark_mcconkey@hotmail.com
Jordan M. Leith, Email: jleith@shaw.ca
David R. Maldonado, Email: davidricardoms@gmail.com
Matthew J. Brick, Email: mat@orthosports.co.nz
Benjamin G. Domb, Email: drdomb@americanhipinstitute.org
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Burman MS. Arthroscopy or the direct visualization of joints: an experimental cadaver study. Clin Orthop Relat Res. 1931;2001(390):5–9. doi: 10.1097/00003086-200109000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Bozic KJ, Chan V, Valone FH, 3rd, Feeley BT, Vail TP. Trends in hip arthroscopy utilization in the United States. J Arthroplast. 2013;28(8 Suppl):140–143. doi: 10.1016/j.arth.2013.02.039. [DOI] [PubMed] [Google Scholar]
- 3.Palmer AJ, Malak TT, Broomfield J, Holton J, Majkowski L, Thomas GE, et al. Past and projected temporal trends in arthroscopic hip surgery in England between 2002 and 2013. BMJ Open Sport Exerc Med. 2016;2(1):e000082. doi: 10.1136/bmjsem-2015-000082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee AJ, Armour P, Thind D, Coates MH, Kang AC. The prevalence of acetabular labral tears and associated pathology in a young asymptomatic population. Bone Joint J. 2015;97-B(5):623–627. doi: 10.1302/0301-620X.97B5.35166. [DOI] [PubMed] [Google Scholar]
- 5.Bsat S, Frei H, Beaule PE. The acetabular labrum: a review of its function. Bone Joint J. 2016;98-B(6):730–735. doi: 10.1302/0301-620X.98B6.37099. [DOI] [PubMed] [Google Scholar]
- 6.Heerey JJ, Kemp JL, Mosler AB, Jones DM, Pizzari T, Souza RB, et al. What is the prevalence of imaging-defined intra-articular hip pathologies in people with and without pain? A systematic review and meta-analysis. Br J Sports Med. 2018;52(9):581–93. 10.1136/bjsports-2017-098264. [DOI] [PubMed]
- 7.Alzaharani A, Bali K, Gudena R, Railton P, Ponjevic D, Matyas JR, et al. The innervation of the human acetabular labrum and hip joint: an anatomic study. BMC Musculoskelet Disord. 2014;15:41. 10.1186/1471-2474-15-41. [DOI] [PMC free article] [PubMed]
- 8.Philippon MJ, Nepple JJ, Campbell KJ, Dornan GJ, Jansson KS, LaPrade RF, et al. The hip fluid seal--part I: the effect of an acetabular labral tear, repair, resection, and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):722–729. doi: 10.1007/s00167-014-2874-z. [DOI] [PubMed] [Google Scholar]
- 9.Nepple JJ, Philippon MJ, Campbell KJ, Dornan GJ, Jansson KS, LaPrade RF, et al. The hip fluid seal--part II: the effect of an acetabular labral tear, repair, resection, and reconstruction on hip stability to distraction. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):730–736. doi: 10.1007/s00167-014-2875-y. [DOI] [PubMed] [Google Scholar]
- 10.Hawellek T, Hubert J, Hischke S, Krause M, Bertrand J, Schmidt BC, et al. Calcification of the acetabular labrum of the hip: prevalence in the general population and relation to hip articular cartilage and fibrocartilage degeneration. Arthritis Res Ther. 2018;20(1):104. 10.1186/s13075-018-1595-y. [DOI] [PMC free article] [PubMed]
- 11.McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. The Otto E. Aufranc Award: The role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res 2001(393):25–37. 10.1097/00003086-200112000-00004. [DOI] [PubMed]
- 12.O’Connor M, Steinl GK, Padaki AS, Duchman KR, Westermann RW, Lynch TS. Outcomes of revision hip arthroscopic surgery: a systematic review and meta-analysis. Am J Sports Med. 2020;48(5):1254–1262. doi: 10.1177/0363546519869671. [DOI] [PubMed] [Google Scholar]
- 13.White BJ, Herzog MM. Labral reconstruction: when to perform and how. Front Surg. 2015;2:27. doi: 10.3389/fsurg.2015.00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Byrd JW, Jones KS. Hip arthroscopy for labral pathology: prospective analysis with 10-year follow-up. Arthroscopy. 2009;25(4):365–368. doi: 10.1016/j.arthro.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 15.Krych AJ, Thompson M, Knutson Z, Scoon J, Coleman SH. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy. 2013;29(1):46–53. doi: 10.1016/j.arthro.2012.07.011. [DOI] [PubMed] [Google Scholar]
- 16.Haddad B, Konan S, Haddad FS. Debridement versus re-attachment of acetabular labral tears: a review of the literature and quantitative analysis. Bone Joint J. 2014;96-B(1):24–30. doi: 10.1302/0301-620X.96B1.32425. [DOI] [PubMed] [Google Scholar]
- 17.Wu ZX, Ren WX, Ren YM, Tian MQ. Arthroscopic labral debridement versus labral repair for patients with femoroacetabular impingement: a meta-analysis. Medicine (Baltimore) 2020;99(19):e20141. doi: 10.1097/MD.0000000000020141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Philippon MJ, Bolia IK, Locks R, Briggs KK. Labral preservation: outcomes following labrum augmentation versus labrum reconstruction. Arthroscopy. 2018;34(9):2604–2611. doi: 10.1016/j.arthro.2018.04.021. [DOI] [PubMed] [Google Scholar]
- 19.Chandrasekaran S, Darwish N, Close MR, Lodhia P, Suarez-Ahedo C, Domb BG. Arthroscopic reconstruction of segmental defects of the hip labrum: results in 22 patients with mean 2-year follow-up. Arthroscopy. 2017;33(9):1685–1693. doi: 10.1016/j.arthro.2017.03.015. [DOI] [PubMed] [Google Scholar]
- 20.Domb BG, Battaglia MR, Perets I, Lall AC, Chen AW, Ortiz-Declet V, et al. Minimum 5-year outcomes of arthroscopic hip labral reconstruction with nested matched-pair benchmarking against a labral repair control group. Am J Sports Med. 2019;47(9):2045–55. 10.1177/0363546518825259. [DOI] [PubMed]
- 21.White BJ, Patterson J, Herzog MM. Revision arthroscopic acetabular labral treatment: repair or reconstruct? Arthroscopy. 2016;32(12):2513–2520. doi: 10.1016/j.arthro.2016.07.024. [DOI] [PubMed] [Google Scholar]
- 22.White BJ, Patterson J, Herzog MM. Bilateral hip arthroscopy: direct comparison of primary acetabular labral repair and primary acetabular labral reconstruction. Arthroscopy. 2018;34(2):433–440. doi: 10.1016/j.arthro.2017.08.240. [DOI] [PubMed] [Google Scholar]
- 23.White BJ, Patterson J, Scoles AM, Lilo AT, Herzog MM. Hip arthroscopy in patients over 40: greater success with labral reconstruction compared to labral repair. Arthroscopy. 2020;36:2137–2144. doi: 10.1016/j.arthro.2020.04.031. [DOI] [PubMed] [Google Scholar]
- 24.Sierra RJ, Trousdale RT. Labral reconstruction using the ligamentum teres capitis: report of a new technique. Clin Orthop Relat Res. 2009;467(3):753–759. doi: 10.1007/s11999-008-0633-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Philippon MJ, Briggs KK, Hay CJ, Kuppersmith DA, Dewing CB, Huang MJ. Arthroscopic labral reconstruction in the hip using iliotibial band autograft: technique and early outcomes. Arthroscopy. 2010;26(6):750–756. doi: 10.1016/j.arthro.2009.10.016. [DOI] [PubMed] [Google Scholar]
- 26.Walker JA, Pagnotto M, Trousdale RT, Sierra RJ. Preliminary pain and function after labral reconstruction during femoroacetabular impingement surgery. Clin Orthop Relat Res. 2012;470(12):3414–3420. doi: 10.1007/s11999-012-2506-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.White BJ, Stapleford AB, Hawkes TK, Finger MJ, Herzog MM. Allograft use in arthroscopic labral reconstruction of the hip with front-to-back fixation technique: minimum 2-year follow-up. Arthroscopy. 2016;32(1):26–32. doi: 10.1016/j.arthro.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 28.Matsuda DK, Burchette RJ. Arthroscopic hip labral reconstruction with a gracilis autograft versus labral refixation: 2-year minimum outcomes. Am J Sports Med. 2013;41(5):980–987. doi: 10.1177/0363546513482884. [DOI] [PubMed] [Google Scholar]
- 29.Park SE, Ko Y. Use of the quadriceps tendon in arthroscopic acetabular labral reconstruction: potential and benefits as an autograft option. Arthrosc Tech. 2013;2(3):e217–e219. doi: 10.1016/j.eats.2013.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Amar E, Sampson TG, Sharfman ZT, Caplan A, Rippel N, Atzmon R, et al. Acetabular labral reconstruction using the indirect head of the rectus femoris tendon significantly improves patient reported outcomes. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2512–8. 10.1007/s00167-017-4641-4. [DOI] [PubMed]
- 31.••. Domb BG, Kyin C, Rosinsky PJ, Shapira J, Yelton MJ, Meghpara MB, et al. Circumferential labral reconstruction for irreparable labral tears in the primary setting: minimum 2-year outcomes with a nested matched-pair labral repair control group. Arthroscopy. 2020. 10.1016/j.arthro.2020.02.014Two-year results of this novel technique of total labral reconstruction showcased in this review show promising results in patients with femoroacetabular impingement along with irreparable labral tears with high patient-reported outcome scores, satisfaction, and comparable functional outcomes.
- 32.Trivedi NN, Sivasundaram L, Su CA, Knapik D, Nho SJ, Mather RC, 3rd, et al. Indications and outcomes of arthroscopic labral reconstruction of the hip: a systematic review. Arthroscopy. 2019;35(7):2175–2186. doi: 10.1016/j.arthro.2019.02.031. [DOI] [PubMed] [Google Scholar]
- 33.••.Rahl MD, LaPorte C, Steinl GK, O’Connor M, Lynch TS, Menge TJ. Outcomes after arthroscopic hip labral reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2019;363546519878147:1748–55. 10.1177/0363546519878147. This review looks at the literature with an eye to compare results between autograft and allograft labral reconstructions in the hip. [DOI] [PubMed]
- 34.••.Al Mana L, Coughlin RP, Desai V, Simunovic N, Duong A, Ayeni OR. The hip labrum reconstruction: indications and outcomes-an updated systematic review. Curr Rev Musculoskelet Med. 2019;12(2):156–65. 10.1007/s12178-019-09546-6. Builds on a similar study performed in 2014 showcasing recent findings in labral reconstruction of the hip. It alludes to the fast pace of research in this field and the rising popularity of this procedure. Short and mid term follow up results are presented. [DOI] [PMC free article] [PubMed]
- 35.Ayeni OR, Alradwan H, de Sa D, Philippon MJ. The hip labrum reconstruction: indications and outcomes--a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):737–743. doi: 10.1007/s00167-013-2804-5. [DOI] [PubMed] [Google Scholar]
- 36.Safran MR. The acetabular labrum: anatomic and functional characteristics and rationale for surgical intervention. J Am Acad Orthop Surg. 2010;18(6):338–345. doi: 10.5435/00124635-201006000-00006. [DOI] [PubMed] [Google Scholar]
- 37.Kim YT, Azuma H. The nerve endings of the acetabular labrum. Clin Orthop Relat Res. 1995;320:176–181. [PubMed] [Google Scholar]
- 38.Domb BG, Hartigan DE, Perets I. Decision making for labral treatment in the hip: repair versus debridement versus reconstruction. J Am Acad Orthop Surg. 2017;25(3):e53–e62. doi: 10.5435/JAAOS-D-16-00144. [DOI] [PubMed] [Google Scholar]
- 39.Maldonado DR, Lall AC, Walker-Santiago R, Rosinsky P, Shapira J, Chen JW, et al. Hip labral reconstruction: consensus study on indications, graft type and technique among high-volume surgeons. J Hip Preserv Surg. 2019;6(1):41–9. 10.1093/jhps/hnz008. [DOI] [PMC free article] [PubMed]
- 40.Woyski D, Mather RC., 3rd Surgical treatment of labral tears: debridement, repair, reconstruction. Curr Rev Musculoskelet Med. 2019;12(3):291–299. doi: 10.1007/s12178-019-09575-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Maldonado DR, Lall AC, Laseter JR, Kyin C, Chen JW, Go CC, et al. Primary hip arthroscopic surgery with labral reconstruction: is there a difference between an autograft and allograft? Orthop J Sports Med. 2019;7(3):2325967119833715. 10.1177/2325967119833715. [DOI] [PMC free article] [PubMed]
- 42.Ferro FP, Philippon MJ, Rasmussen MT, Smith SD, LaPrade RF, Wijdicks CA. Tensile properties of the human acetabular labrum and hip labral reconstruction grafts. Am J Sports Med. 2015;43(5):1222–1227. doi: 10.1177/0363546514568086. [DOI] [PubMed] [Google Scholar]
- 43.Shi YY, Chen LX, Xu Y, Hu XQ, Ao YF, Wang JQ. Acetabular labral reconstruction with autologous tendon tissue in a porcine model: in vivo histological assessment and gene expression analysis of the healing tissue. Am J Sports Med. 2016;44(4):1031–1039. doi: 10.1177/0363546515623784. [DOI] [PubMed] [Google Scholar]
- 44.Domb BG, Gupta A, Stake CE, Hammarstedt JE, Redmond JM. Arthroscopic labral reconstruction of the hip using local capsular autograft. Arthrosc Tech. 2014;3(3):e355–e359. doi: 10.1016/j.eats.2014.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sampson TG. Surgical technique: arthroscopic rectus autograft. In: Nho S. LM, Larson C., Bedi A., Kelly B., editor. Hip arthroscopy and hip joint preservation surgery. New York: Springer; 2015. p. 6.
- 46.Sharfman ZT, Amar E, Sampson T, Rath E. Arthroscopic labrum reconstruction in the hip using the indirect head of rectus femoris as a local graft: surgical technique. Arthrosc Tech. 2016;5(2):e361–e364. doi: 10.1016/j.eats.2016.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rathi R, Mazek J. Arthroscopic acetabular labral reconstruction with rectus femoris tendon autograft: our experiences and early results. J Orthop. 2018;15(3):783–786. doi: 10.1016/j.jor.2018.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Locks R, Chahla J, Bolia IK, Briggs KK, Philippon MJ. Outcomes following arthroscopic hip segmental labral reconstruction using autologous capsule tissue or indirect head of the rectus tendon. J Hip Preserv Surg. 2018;5(1):73–77. doi: 10.1093/jhps/hnx033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Deshmane PP, Kahlenberg CA, Patel RM, Han B, Terry MA. All-arthroscopic iliotibial band autograft harvesting and labral reconstruction technique. Arthrosc Tech. 2013;2(1):e15–e19. doi: 10.1016/j.eats.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Geyer MR, Philippon MJ, Fagrelius TS, Briggs KK. Acetabular labral reconstruction with an iliotibial band autograft: outcome and survivorship analysis at minimum 3-year follow-up. Am J Sports Med. 2013;41(8):1750–1756. doi: 10.1177/0363546513487311. [DOI] [PubMed] [Google Scholar]
- 51.Lebus GF, Briggs KK, Dornan GJ, McNamara S, Philippon MJ. Acetabular labral reconstruction: development of a tool to predict outcomes. Am J Sports Med. 2018;46(13):3119–3126. doi: 10.1177/0363546518796838. [DOI] [PubMed] [Google Scholar]
- 52.Chahla J, Soares E, Bhatia S, Mitchell JJ, Philippon MJ. Arthroscopic technique for acetabular labral reconstruction using Iliotibial band autograft. Arthrosc Tech. 2016;5(3):e671–e677. doi: 10.1016/j.eats.2016.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Matsuda DK. Arthroscopic labral reconstruction with gracilis autograft. Arthrosc Tech. 2012;1(1):e15–e21. doi: 10.1016/j.eats.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rosinsky PJ, Shapira J, Lall AC, Domb BG. All about the ligamentum teres: from biomechanical role to surgical reconstruction. J Am Acad Orthop Surg. 2020;28(8):e328–ee39. doi: 10.5435/JAAOS-D-19-00352. [DOI] [PubMed] [Google Scholar]
- 55.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83(8):1119–1124. doi: 10.1302/0301-620x.83b8.11964. [DOI] [PubMed] [Google Scholar]
- 56.Domb BG, Gui C, Lodhia P. How much arthritis is too much for hip arthroscopy: a systematic review. Arthroscopy. 2015;31(3):520–529. doi: 10.1016/j.arthro.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 57.Skendzel JG, Philippon MJ, Briggs KK, Goljan P. The effect of joint space on midterm outcomes after arthroscopic hip surgery for femoroacetabular impingement. Am J Sports Med. 2014;42(5):1127–1133. doi: 10.1177/0363546514526357. [DOI] [PubMed] [Google Scholar]
- 58.Sheean AJ, Musahl V, Slone HS, Xerogeanes JW, Milinkovic D, Fink C, et al. Quadriceps tendon autograft for arthroscopic knee ligament reconstruction: use it now, use it often. Br J Sports Med. 2018;52(11):698–701. 10.1136/bjsports-2017-098769. [DOI] [PubMed]
- 59.Karns MR, Patel SH, Kolaczko J, Liu RW, Mather RCR, White BJ, et al. Acetabular rim length: an anatomical study to determine reasonable graft sizes for labral reconstruction. J Hip Preserv Surg. 2017;4(1):106–112. doi: 10.1093/jhps/hnw038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lippe J, Armstrong A, Fulkerson JP. Anatomic guidelines for harvesting a quadriceps free tendon autograft for anterior cruciate ligament reconstruction. Arthroscopy. 2012;28(7):980–984. doi: 10.1016/j.arthro.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 61.Redmond JM, Cregar WM, Martin TJ, Vemula SP, Gupta A, Domb BG. Arthroscopic labral reconstruction of the hip using semitendinosus allograft. Arthrosc Tech. 2015;4(4):e323–e329. doi: 10.1016/j.eats.2015.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.••.Perets I, Hartigan DE, Chaharbakhshi EO, Walsh JP, Close MR, Domb BG. Circumferential labral reconstruction using the knotless pull-through technique-surgical technique. Arthrosc Tech. 2017;6(3):e695–e6e8. doi: 10.1016/j.eats.2017.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rathi R, Mazek J. Arthroscopic acetabular labral reconstruction with fascia lata allograft: clinical outcomes at minimum one-year follow-up. Open Orthop J. 2017;11:554–561. doi: 10.2174/1874325001611010554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Carreira DS, Kruchten MC, Emmons BR, Martin RL. Arthroscopic labral reconstruction using fascia lata allograft: shuttle technique and minimum two-year results. J Hip Preserv Surg. 2018;5(3):247–258. doi: 10.1093/jhps/hny028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Moya E, Natera LG, Cardenas C, Astarita E, Bellotti V, Ribas M. Reconstruction of massive posterior nonrepairable acetabular labral tears with peroneus brevis tendon allograft: arthroscopy-assisted mini-open approach. Arthrosc Tech. 2016;5(5):e1015–e1e22. doi: 10.1016/j.eats.2016.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Costa Rocha P, Klingenstein G, Ganz R, Kelly BT, Leunig M. Circumferential reconstruction of severe acetabular labral damage using hamstring allograft: surgical technique and case series. Hip Int. 2013;23(Suppl 9):S42–S53. doi: 10.5301/HIP.2013.11662. [DOI] [PubMed] [Google Scholar]
- 67.Bhatia S, Ellman MB, Nho S, Mather RC, 3rd, Bedi A, Aoki SK, et al. Bilateral hip arthroscopy: direct comparison of primary acetabular labral repair and primary acetabular labral reconstruction. Arthroscopy. 2018;34(6):1748–1751. doi: 10.1016/j.arthro.2018.03.027. [DOI] [PubMed] [Google Scholar]