Abstract
Purpose of Review
To describe the (1) indications, (2) preoperative precautions, and (3) stepwise technical details of modern femoral stem cemented fixation.
Recent Findings
Femoral stem cementation provides excellent implant longevity with a low periprosthetic fracture rate among patients with compromised bone quality or aberrant anatomy. Unfamiliarity with the details of modern cementation techniques among trainees who may lack frequent exposure to cementing femoral stems may preclude them from offering this viable option to suitable patients in later stages of their careers. As such, maximizing benefit from cemented femoral stem fixation among suitable candidates is contingent upon the meticulous use of modern cementation techniques.
Summary
In addition to proper patient selection, modern cementation techniques emphasize the use of (1) pulsatile lavage of the femoral canal, (2) utilization of epinephrine-soaked swabs, (3) vacuum cement mixing, (4) retrograde cement introduction, (5) cement pressurization, and (6) the use of stem centralizers. Furthermore, identifying and optimizing the preoperative status of at-risk patients with pre-existing cardiopulmonary compromise, in addition to intraoperative vigilance, are essential for mitigating the risk of developing bone cement implantation syndrome. Further research is required to assess the utility of cemented femoral stem fixation among younger patients.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12178-020-09681-5.
Keywords: Total hip arthroplasty (THA), Hemiarthroplasty, Cemented femoral stem fixation, Operative steps, Femoral stem design, Modern cementation technique
Introduction
Over 370,000 total hip arthroplasties (THAs) are performed annually in the USA [1], although only 1–2 out of 10 (14%) utilize cemented femoral stem fixation [2]. Conversely, such regional pattern is upended in Europe, where 73.1% [3] and 56.7% [4] rates of cemented femoral stem fixation were described in Sweden and the UK, respectively. Overall, cemented and cementless arthroplasties have robust and predictable outcomes, with reported overall 15-year survival rates estimated at 77–82% [5, 6] and 78–80%, respectively [7, 8]. However, multiple studies have outlined that cementless femoral stem fixation is associated with higher early revision rates compared to its cemented counterpart owing to an increased risk of 3-month postoperative fracture and/or loosening [9••, 10–12]. Similarly, superior midterm outcomes of cemented femoral stems among patients with poor bone quality have been described [13, 14].
Despite the reported good to excellent track record of cemented fixation of femoral stems, the proportion of cementless hip arthroplasty has continued to grow, especially in the USA [2]. Such disparity between literature and practice has been attributed to the ease of using cementless implants and strong marketing for cementless solutions, in addition to an unfamiliarity with the details of modern cementation technique among US trainees who may lack frequent exposure to cementing femoral stems [15–17]. Several limitations attributed to cementing femoral stems are based on outdated cementation techniques which engender high cement porosity, poor cement penetration at the cement–bone interface as well as frequent contamination with impurities as residual blood, bone marrow contents, and air bubbles that compromise the cemented construct’s integrity and mitigate survivorship [16, 18, 19••]. Nevertheless, many of these limitations have been addressed by advancements in current fourth-generation cementation techniques required to perform a high-quality cemented femoral stem fixation.
Of note, while cemented femoral stems have demonstrated advantageous clinical outcomes relative to their cementless counterparts, the same has not held for acetabular components. Cementless acetabular fiber-mesh components have been reported to have lower rates of radiographic loosening (p = 0.012) at 10 years postoperatively [20]. Furthermore, 3D highly porous titanium acetabular cups achieve reliable osteointegration and have reported short-term survivorships up to 99.3% [21, 22]. Hybrid THA describes the isolated cemented fixation of the femoral component and has evolved to encompass the advantages of cemented femoral stem fixation while mitigating the risk of aseptic loosening associated with the cemented fixation of acetabular components [23–25]. Therefore, adequate working knowledge of the techniques of femoral stem cementation is of crucial significance.
To this end, the aim of the current review is to provide a stepwise technical guide to performing appropriate femoral stem cementation using modern fourth-generation cementation techniques.
Choosing the Correct Patient
Potentially, most patients could be treated with either a cemented or cementless femoral component. While cemented femoral stems provide added value among certain populations, there is no clear delineation of subgroup characteristics beyond which cementation would be contraindicated [26]. Current evidence emphasizes favorable outcomes of cemented femoral components in the elderly with particular emphasis on females and those with overall poor bone quality [19••, 27] (Table 1). Conferred advantages within this population include lower intraoperative complications [28, 29•], aseptic loosening [30], and all-cause revision rates [31••, 32, 33], in addition to enhanced 10-year implant survivorship [34–36]. However, designating an age cutoff for improved outcomes is controversial [36]. Analyses of multiple national registries report a lower risk of revision conferred by femoral component cementation in patients older than 75 years undergoing primary THA [19••, 26, 37]. Abdel et al. broadened these findings through an analysis of 32,644 patients undergoing cemented and cementless THA, reporting a 14-fold increase in intraoperative periprosthetic fractures within patients undergoing THA with cementless femoral components [28]. Particular at-risk subgroups were female patients and patients ≥ 65 years. Of note, several cementless designs demonstrated overall survival exceeding 90% at 20 years, particularly among younger populations (< 50 years) [38, 39]. As such, it may be more appropriate for younger patients to receive cementless implants in the absence of a compelling reason for cementation [40].
Table 1.
Patient subgroups with potential to benefit from femoral stem cementation
| Candidates for femoral stem cementation | |
| Elderly patients (≥ 65 years) especially females | |
| Femur type C Dorr classification (inner canal diameter at the midportion of lesser trochanter divided by diameter 10 cm distal > 0.75) | |
| Severe osteoporosis | |
| Femoral neck fracture | |
| Narrow femoral canal or aberrant proximal femoral anatomy |
Additional patient subgroups who could benefit from femoral stem cementation include patients with femoral neck fractures [31••], those exhibiting narrow proximal femoral canals [27] as in developmental dysplasia of the hip, patients with periprosthetic fractures, or significant proximal femoral bone loss (Dorr type C) [27, 28, 30, 41–44]. Indeed, a recent analysis from the Norwegian Hip Fracture Register highlighted a 1.5-fold increase in all-cause reoperation among patients receiving cementless hemiarthroplasty compared to cemented stem fixation [31••]. These findings emphasize the value of femoral component cementation in attenuating the risk of intraoperative and postoperative periprosthetic fractures among predisposed populations with compromised bone quality or aberrant anatomy.
Perioperative Precautions
The preoperative identification of high-risk patients for developing bone cement implantation syndrome (BCIS) is critical to prevent intra- and perioperative morbidity and mortality [45]. BCIS is an intraoperative systemic complication defined as a constellation of hypoxia, hypotension, and/or cardiopulmonary collapse occurring around the time of cementation, prosthesis insertion, reduction of the joint, or, occasionally, limb tourniquet deflation in a patient undergoing cemented bone surgery [45]. Established risk factors for BCIS include ≥ 65 years of age, male gender, diuretic or warfarin use, COPD, cardiopulmonary disease, pre-existing pulmonary hypertension, and metastatic bony disease [45–47]. Additional local factors include the presence of a hip fracture, a wide femoral canal (≥ 21 mm), and revision surgery [47, 48]. While the definitive cause of BCIS remains controversial, several reports have implicated embolic phenomena, methyl methacrylate (MMA) particle or histamine-induced vasodilation, complement activation, or a combination of the aforementioned pathogeneses [47, 49].
Preoperative considerations for at-risk patients include maximizing cardiopulmonary stability, volume repletion, and optimizing comorbidities [19••, 45, 47]. Furthermore, choice of anesthesia should account for the exaggerated hemodynamic manifestations of BCIS when coupled with inhalation agents [47, 50]. In addition to intraoperative high oxygen concentration, systolic BP within 20% of baseline should be targeted. Capnography and pulse oximetry are essential, potentially coupled with an arterial line as well as invasive hemodynamic monitoring for early detection of hemodynamic instability, and the possible need for frequent arterial blood gases [19••, 47].
Femoral Stem Considerations
Femoral stem design typically conforms to one of two established biomechanical philosophies: taper-slip (force closed) or composite-beam (shape closed) stems [19••, 51]. Taper-slip femoral stems become wedged into the surrounding cement mantle [52, 53]. Postoperative controlled stem subsidence of 1–2 mm is expected over the initial year and is considered conducive to biomechanical stability [54–56]. Controlled subsidence ensures transmission of the axial forces acting on the femoral stem into radial compressive forces transmitted to the proximal femoral cortex in the form of hoop stress [19••, 57]. This philosophy allows for both improved proximal loading of the cement and significant reduction of the peak pressures at the proximal and distal cement mantles [51]. With the goal of subsidence-dependent fixation, taper-slip stems are characterized by a smooth polished surface with bi- or tri-planar tapers, thereby ensuring a robust cement–bone bond through cement–bone interdigitation. In addition, the weaker stem–cement interface allows for controlled subsidence and micromotion tolerance with minimal debris generation [58]. Of note, there have been reports of proximal bone remodeling in response to the indirect load transmission through the cement mantle; however, the implications of such findings remain unclear [59].
The rotational stability of taper fit stems is influenced by its cross-sectional geometry. Whereas rectangular cross-section stems offer higher rotational stability against torsional forces [60], the resultant stress risers generated at the corners predispose to the development of microfractures within the cement mantle, which can adversely affect the durability of the construct [19••, 61]. A similar mechanism is not evident among oval cross-section stems where stress riser points are not readily created [51, 61]. Notably, the permissiveness of taper-slip stems to micromotion makes mitigating stress riser generation a crucial consideration to avert compromise in the construct’s longevity.
Unlike taper-slip femoral stems, composite-beam designs are intended to attain postoperative stability with minimal to no early subsidence [57, 62]. Composite-beam designs exhibit strong adhesive forces between the textured stem surface and the cement mantle. This construct leads to the conversion of the axial forces acting on the femoral stem into tensile shear forces that are transmitted to the cement–bone interface [19••, 51]. Such shear forces at the cement–bone interface coupled with cyclic loading cause progressive debris generation, a major driver of osteolysis and implant loosening. Indeed, a 4% increase in revision rate has been associated with each 0.1 mm of subsidence beyond the acceptable 0.15 mm threshold at 2 years postoperatively [62].
The impact of femoral stem size relative to the diameter of the femoral canal (canal fit) on construct integrity varies according to the femoral stem type. While a greater femoral stem size might be counterproductive in taper-slip designs owing to impedance of early migration and wedging [19••, 61], composite-beam stems might benefit from the added stability of stem–cortex points of contact [19••, 63]. Conversely, points of direct contact between cortical bone and the femoral stem are considered weak points through which the previously isolated debris generated at the stem–cement interface could migrate, reaching the cement–bone interface and aggravating osteolysis [61].
Composite-beam femoral stem precoating with polymethyl methacrylate (PMMA) evolved to enhance adhesion at the stem–cement interface, in an attempt to counter loosening and promote construct longevity [64]. However, early results using second-generation cementation techniques outlined high 10-year failure rates of 9.5% compared to 3.9% for their uncoated polished counterparts [65]. Paradoxical failure occurred at the stem–cement interface and was mainly attributed to the thin cement mantle associated with precoated cement use. Recent 15-year follow-up reports describe a combination of poor cementation second-generation cementation techniques to be a major driver of the failure of such designs, in addition to potential inherent design flaws [64, 66].
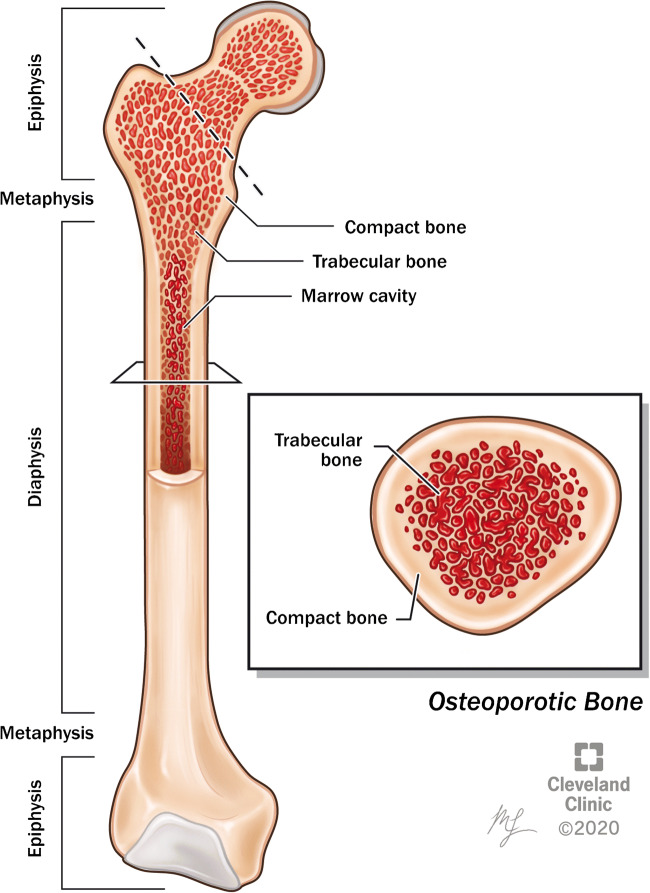
Overall acceptable survivorship has been established for both taper-slip and composite-beam femoral stem designs [56, 67]. However, a recent analysis of 292,987 cemented hip arthroplasties between 2003 and 2013 from the National Joint Registry of England and Wales highlighted higher revision rates among composite-beam stems (1.7%) compared to taper-slip designs (1.3%; p < 0.001) [56]. The less forgiving nature of composite-beam designs to suboptimal cementation technique should be factored in the decision-making process. The abrasive capacity and surface roughness of the cemented femoral stem is likewise an important consideration (Fig. 1). Similarly, the wide array of the extent of taper-slip stem surface roughness influences its biomechanical behavior. Indeed, taper-slip stems could be subclassified into polished (Ra < 1.0 μm causing minimal cement abrasion), matte (Ra < 2.0 μm causing no excessive cement abrasion assuming no significant stem micromotion), and rough (Ra > 2.0 μm causing excessive cement abrasion, can only be applied to locations with minimal micromotion) [68–71].
Fig. 1.
Rough (left) and polished (right) taper-slip stem designs fixed using fourth-generation cementation techniques
Choice of Approach
Traditionally, the implantation of cemented femoral components may be conducted through any approach including posterior, anterolateral, direct lateral, or anterior approach highlighting the need to obtain satisfactory exposure of the femoral canal, which is critical for reliable orientation of the femoral components intraoperatively [19••]. Furthermore, candidates for cemented femoral components typically demonstrate poor bone quality, an established risk factor for perioperative proximal femoral fractures, especially when coupled with broaching under poor visualization/blind broaching [72].
Nevertheless, implanting cemented femoral components through a direct anterior approach remains a viable option in the absence of anatomical constraints and general anterior approach contraindications [72]. Further emphasis should be made to ensure adequate exposure of the proximal femur. While exposure and osteotomy can be achieved through minimal incision length, sufficient control over the femoral stem insertion and final orientation within the cemented canal dictates the presence of a generous exposure [73]. Therefore, a proximal extension of the anterior surgical incision may be required [72]. Anterior approaches require prudence to establish a posterolateral entry point into the femoral canal and secure a neutral position of the femoral stem within the canal.
Proximal Femoral Osteotomy and Canal Preparation
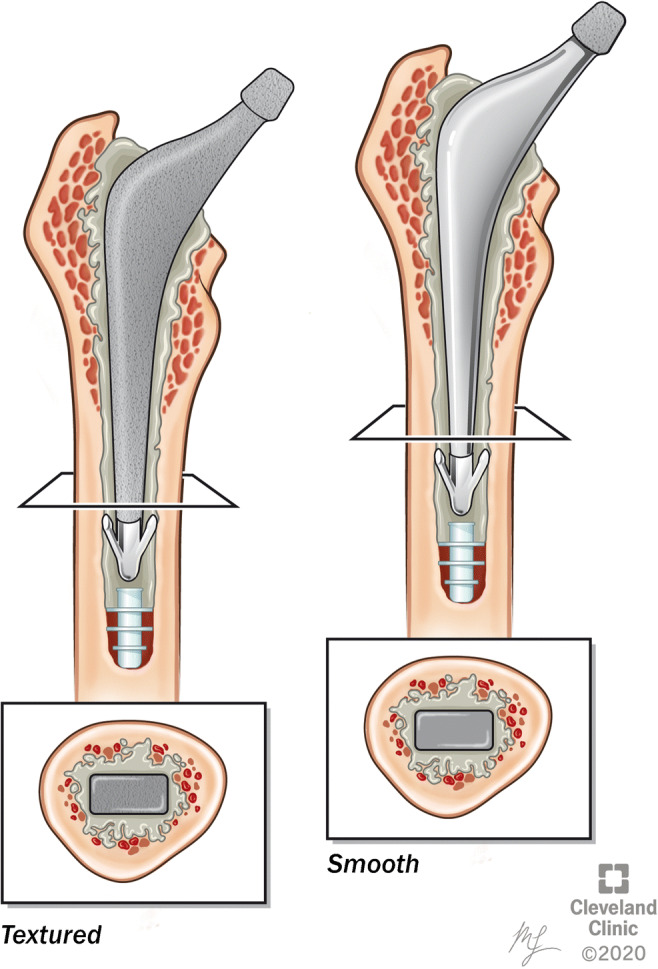
The femoral neck osteotomy is started in accordance with the preoperative templating; generally, one fingerbreadth above the lesser trochanter medially to provide sufficient metaphyseal calcar support and subsequently extended laterally to exit at the level of the saddle (Fig. 2) [19••]. The use of a neck resection guide, combined with electrocautery to outline resection borders, can alternatively guide a more accurate resection [74]. Erring on the side of conservative resection rather than over-resection is preferred since the former can be rectified via calcar planning or re-cutting the femoral neck. Collarless femoral stems are more tolerant of minor deviations from planned femoral neck cuts, allowing for minor corrections to increase the insertion depth of the stem after cementation. Conversely, a collared stem impinges on the calcar, making a precise neck cut critical to achieving the desired vertical offset [19••, 61, 63]. Notably, over-resecting the femoral neck can be partially rectified by utilizing a collared stem cemented at a greater vertical offset with an intervening cement mantle between the collar and the deficient calcar (proud stem).
Fig. 2.
Sagittal and coronal section of the proximal femur with an outlined plane of the femoral neck cut (dashed line)
The remaining cortex at the femoral neck–greater trochanteric junction is breached using a box osteotome to enter the femoral canal in an identical trajectory to that of the straight reamer (Fig. 3). A straight reamer can then be inserted at a posterolateral initiation point of the resection plane near the piriformis fossa to ensure appropriate alignment within the femoral canal [19••, 75]. Femoral canal preparation is undertaken according to the implant-specific surgical technique guide, through a serial reaming if indicated followed by sequential broaching with repetitive irrigation and suctioning between broach size increments to mitigate the risk of embolization (Fig. 4) [19••, 76]. Broaching should be performed while maintaining a trajectory conducive to proper implant alignment (avoiding varus) and continued until all but the outer 3–4 mm of cancellous metaphyseal bone is removed, and the desired axial and rotational stability within the femoral canal is attained to permit a trial reduction [19••]. At this point, further alterations of calcar height could be performed.
Fig. 3.
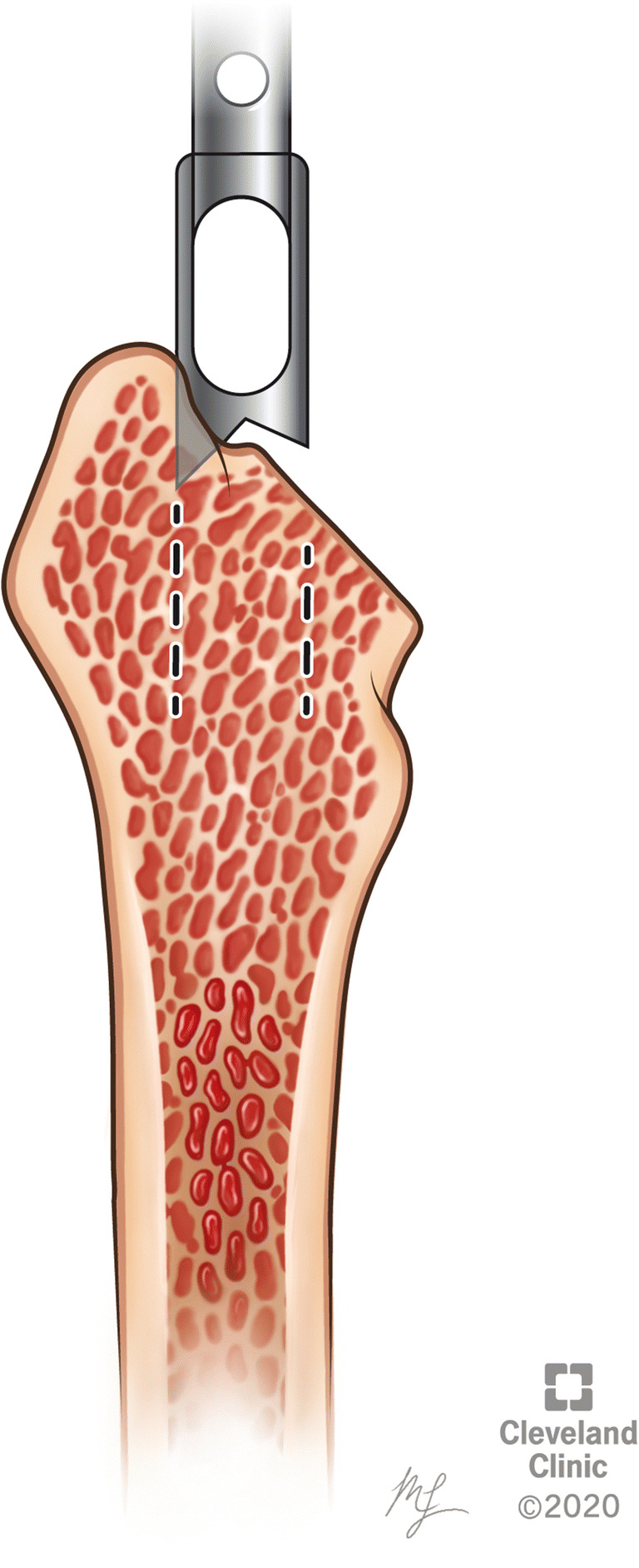
Box osteotome removing the proximal cortex in alignment with the medullary canal’s trajectory
Fig. 4.
Sequential broaching of the medullary canal followed by irrigation and clearance of debris. Care should be taken to pull the broach laterally after introduction to avoid varus positioning of the implant
After successful trial reduction, marking the broach shoulder height and the desired stem anteversion, on the greater trochanter and the cut surface of the femoral neck, respectively, aids in the accurate insertion of the permanent implant at the desired depth, alignment, and orientation [19••]. A cement restrictor is inserted to a level 1–1.5 cm distal to the planned level of the femoral stem tip to allow for an adequate distal cement mantle (Fig. 5) [19••, 48]. Upsizing femoral restrictors is encouraged to prevent distal migration and provide sufficient counter-force during cement pressurization.
Fig. 5.
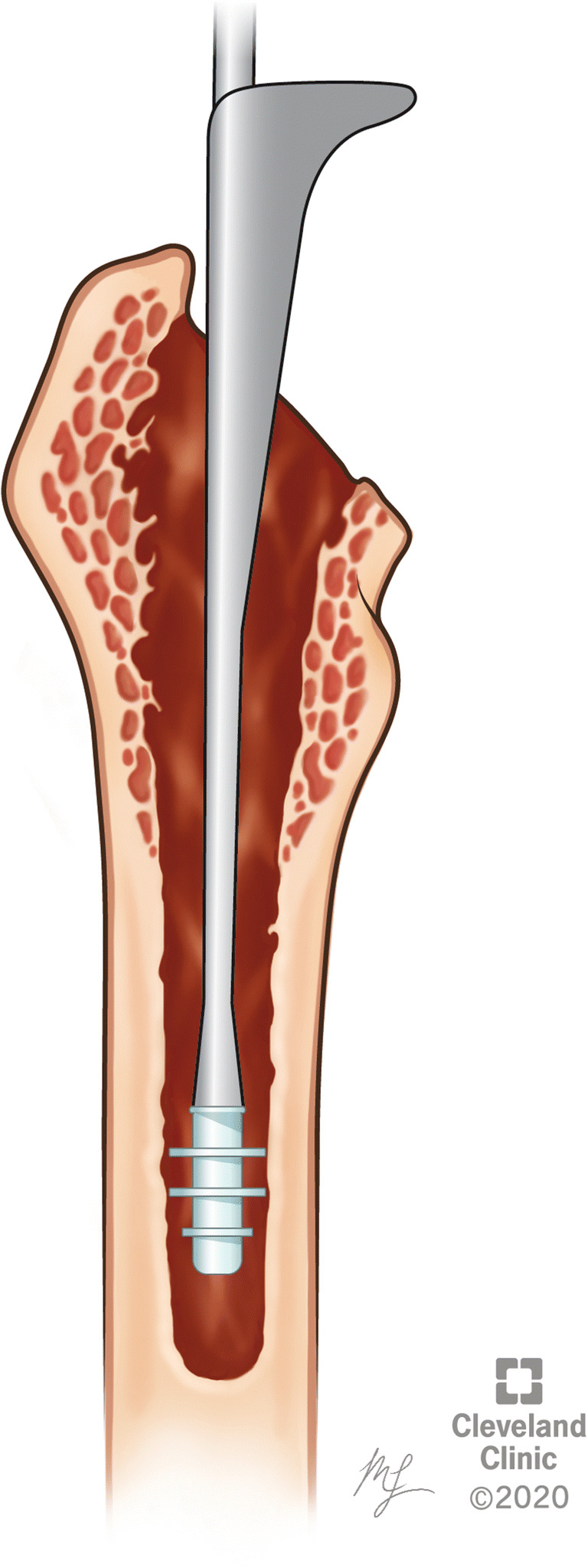
Insertion of cement restrictor distally
Thorough pulse lavage of the femoral canal in addition to possible canal brushing and adequate suctioning promote interdigitation at the cement–bone interface that would otherwise be compromised by intervening blood, fat, and marrow cells, and also mitigates the risk of embolization and BCIS during cement insertion and pressurization [19••, 47, 50, 77, 78]. A dry sponge can be used to ensure canal dryness, followed by scrubbing with an epinephrine-soaked sponge (1:100,000 epinephrine: normal saline) [79] to attain a bloodless canal (if no systemic contraindications). Hypotensive anesthesia could be used in conjunction with the aforementioned methods to diminish blood extravasation, which involves a 40% reduction of mean arterial BP (MAP of ≤50 mm Hg) [80, 81]. However, surgeons should be cautioned that decrement in MAP may be detrimental if complicated by a sudden drop of BP secondary to BCIS.
Cement Insertion and Pressurization
Surgeons are encouraged to notify the anesthesia team prior to cement insertion. Necessary precautions to counter the potential development of BCIS include increasing inhaled oxygen concentration as well as establishing invasive monitoring modalities in high-risk patients if not already implemented [19••, 47, 50]. In addition, vasopressors should be readily available to reverse potential sudden drops in BP, in addition to aggressive volume resuscitative measures [19••, 47].
Cement preparation can be initiated simultaneously with the final steps of femoral canal preparation. Proper cementation technique using modern (fourth-generation) cementation principles are the cornerstone for improved construct longevity [19••, 82] (Table 2). The powdered PMMA/co-polymer and benzoyl peroxide accelerator are vacuum mixed with the liquid combination of MMA monomer, N,N-dimethyl para-toluidine/dimethyl para-toluidine accelerator and the hydroquinone stabilizer [48]. Vacuum mixing decreases cement porosity, mitigates cement lamination, and diminishes the formation of air microbubbles that compromise cement integrity [19••, 82–84]. Furthermore, fume byproducts generated on contact between the liquid MMA monomer and the powdered MMA–styrene co-polymer are considered an occupational hazard and should not exceed 125 ppm in room air [47]. Mixing typically lasts for 1–1.5 min, followed by loading the cement mixture into a long-nozzle cement gun [19••, 85].
Table 2.
Principles of fourth-generation cementation techniques
| Fourth-generation cementation techniques | |
| Femoral canal preparation followed by pulsatile lavage | |
| Canal packing with epinephrine-soaked swabs | |
| Vacuum cement mixing | |
| Retrograde cement introduction using a long-nozzle cement gun | |
| Cement pressurization | |
| Stem insertion with distal and proximal centralizers |
Several factors may accelerate cement setting, including higher temperatures, prolonged mixing, manual handling, and excessive humidity [48]. Extrusion of a small amount of cement from the nozzle to assess for adequate consistency is recommended prior to administration [19••, 48]. A combination of reduced cement luster and a manually moldable non-sticky cement sample are indicators of appropriate cement consistency for canal filling. Cement injection at excessively low consistency causes mixing with residual blood and fat marrow components. On the other hand, delayed application with a subsequently high cement consistency increases the risk of cement lamination, compromises pressurization, and mitigates interdigitation at the cement–bone interface, in addition to potentially impeding complete stem insertion [19••, 86].
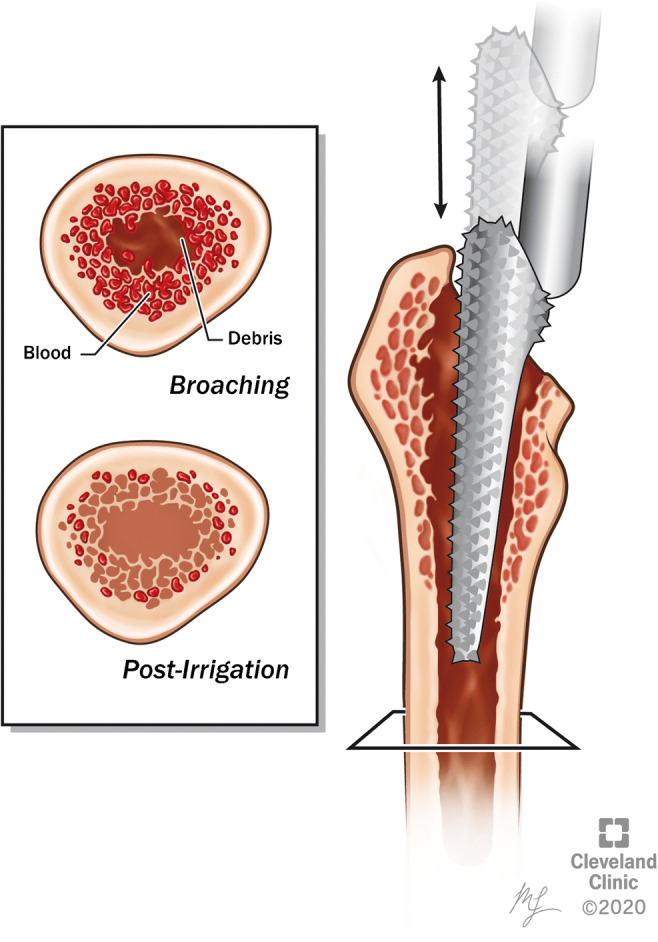
The introduction of cement into the femoral canal is started between 2 and 4 min from the start of mixing [86]. Cement insertion is performed in a retrograde fashion from distal to proximal, coupled with continuous suction proximally using a small catheter, thereby obviating the risk of air or fluid trapping within the cement substance as well as compartmentalizing marrow content residue which reduces BCIS risk [19••, 45, 47, 50]. Further cement interdigitation within the surrounding remnants of the cancellous bone layer is achieved through cement pressurization [19••]. In addition, pressurized cement exerts counter-pressure against bleeding into the cement–bone interface (Fig. 6) [87]. The cement pressurizer is applied after full canal cementation, combined, and continuous pressure is applied for 30 to 60 s. The use of a cement pressurizer necessitates vigilance of the stage of cement hardening. Alternatively, finger pressurization can be performed, which provides useful tactile feedback regarding cement consistency, yet at the expense of the attained peak pressures [19••]. Regardless of the pressurization method, extruded cement should not be reintroduced into the canal because of the potential for its contamination with integrity-compromising fluid particles and air voids. Of note, new cement can be added to replace the extruded volume if needed. Excessive pressurization should be averted among patients with severely osteoporotic bone, geriatric femoral neck fractures, or cardiopulmonary compromise due to the associated risk of developing BCIS [19••, 47].
Fig. 6.
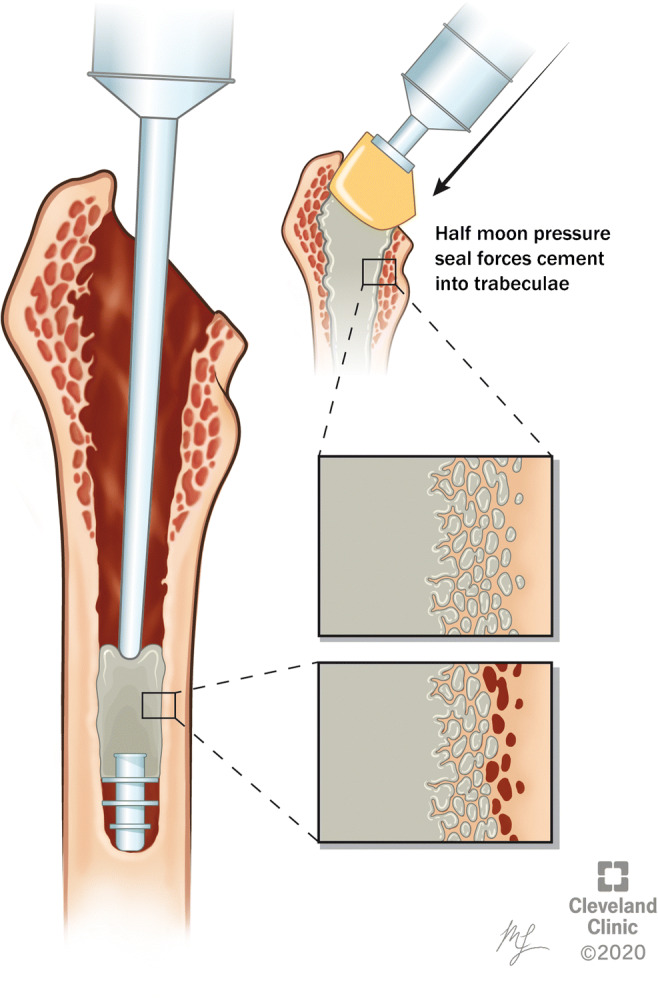
Retrograde insertion of bone cement into the medullary canal with suboptimal penetration (left), followed by pressurization of the inserted cement with improved cement penetration (right)
Femoral canal preparation and cement insertion have been associated with the highest circulating levels of prothrombin F1.2, thrombin–antithrombin complexes, fibrinopeptide A, and D-dimer among the steps of hip arthroplasty [88]. The prothrombotic action of these factors prompted several authors to advocate for heparin administration either continuously or via a single 1000–1500 U dose prior to canal preparation [88–91]. Indeed, several reports have established the safety of intraoperative heparin with blood loss increments as low as 25 ml compared to non-heparinized patients [91–93]. Furthermore, early studies [90, 94] outlined a significant reduction in the rates of proximal femoral deep venous thrombosis with astounding decrements in incidence from 9.1 to 1.7% (p < 0.02), as reported by Huo et al. [90]. Later randomized controlled double-blinded trial by Westrich et al. [89] outlined the similar rates of proximal DVT development among heparinized and non-heparinized patients (p = 0.79) and concluded that single dose of intraoperative heparin does not prevent their formation, but may be effective at preventing ipsilateral femoral thrombi. Overall, they advocated for combined approach of prophylaxis against thromboembolic phenomena encompassing the use of postoperative aspirin or anti-coagulants, pneumatic compression devices, and early mobilization [89].
Femoral Stem Insertion
The use of a distal stem centralizer in conjunction with collarless taper-slip stems provides a more uniform cement mantle around the femoral stem by ensuring a central position of the distal tip within the femoral canal (Fig. 1) [19••, 48, 95]. In addition, stem centralizers protect against distal cement mantle fractures through attenuating the formation of stress risers around the stem tip [96]. Notably, while hollow stem centralizers were found to be associated with greater stem subsidence compared to their solid counterpart, a recent randomized controlled trial by Weber et al. found no difference in revision or radiographic loosening between both centralizer subtypes over a 10-year follow-up period [96].
Much controversy surrounds the timing of femoral stem insertion into the cement-filled canal. Advocates for stem insertion into early-cure cement describe the risks associated with delayed insertion, including bleeding into the cement–bone interface and excessive cement hardening that hinders full-depth insertion with a subsequently arduous reduction and limb length discrepancy [19••]. Conversely, in vitro studies outline the advantages of the additional pressurization exerted through stem insertion into late-cure cement with subsequently improved interdigitation at the bone–cement interface [48, 97]. Furthermore, Hunt et al. compared in vivo femoral stem pull-out force and radiographic cement interdigitation between polished femoral stem insertion into early- versus late-cure cement mantles [98]. Pullout forces were significantly higher within the late-cure cement group (908 N) compared to the early-cure cement group (503 N; p = 0.049). However, both groups demonstrated similar degrees of radiographic cement–bone interdigitation. Furthermore, the choice of insertion timing is influenced by the type of utilized femoral stem. Taper-slip stems are more amenable to insertion into late-cure cement owing to their polished surfaces with minimal shear forces at the stem–cement interface [98, 99]. On the other hand, composite-beam designs exhibit significant shear forces at the stem–cement interface owing to their textured nature and are therefore more acquiescent to early-cure insertion with lower cement resistance [98, 99].
Preheating femoral stems has been described as a method of mitigating cement porosity and increasing cement strength at the stem–cement interface [100–102]. Baleani et al. [100] compared the biomechanical properties of femoral stems cemented into pseudo-femurs at variable temperatures (heated to 45 °C vs. 23 °C) with air- versus vacuum-mixed cement. The authors noted a significantly higher bending strength (p = 0.003) and bending modulus (p < 0.001) as well as lower cement porosity (p < 0.001) within the preheated vacuum-mixed constructs. Several studies have described similar outcomes with preheating to a range of temperatures from 37 to 50 °C [100–105]. Although there are currently no studies comparing clinical outcomes of preheated versus non-preheated implants, reports describing the adverse impact high stem–cement interface porosity on the debonding energy as well as the interface resistance to torsion, cracks, and fatigue failure may favor implant preheating [48, 106–108].
Femoral stem insertion is performed manually with emphasis on preventing varus malalignment through ensuring appropriate trajectory, orienting one of the centralizer prongs parallel to the lateral border of the stem, and exerting manual counter-pressure on the medial calcar using the surgeon’s thumb during stem advancement [19]. The latter aids in maintaining pressure within the cement mantle as well [97]. Modification of stem alignment or rotation is absolutely prohibited after full insertion to prevent compromising the cement mantle integrity with introduced air and fluid voids. Therefore, checking the stem orientation and trajectory should be performed when two thirds of the stem has been inserted and prior to full insertion of the component.
Joint Reduction
Ensuring full cement hardening prior to attempted reduction should be guided by the duration from the initiation of cement mixing (12–15 min) as well as examining a cement sample from the same batch. However, surgeons should be cautioned that manual handling of the cement sample in addition to heat and humidity could introduce discordance between the curing times of the intramedullary cement and the extracorporeal cement sample [48]. Extruded cement should be cleared from the surgical field prior to joint reduction. Despite being extremely rare, surgeons should be cautious of stem dislodgement during reduction, especially in polished taper-slip stems [109].
Assessment of Postoperative Radiographs
While the value of routine postoperative radiographs during the index surgical admission remains controversial, the majority of providers obtain anteroposterior and frog-leg lateral radiographs at least within 14 to 90 days postoperatively [110–112]. Such radiographs serve to detect possible component malpositioning or fixation compromise in an attempt to prevent mid- to long-term complications. Acceptable radiographic parameters include a LLD < 1 cm, vertical and horizontal centers of rotation equivalent to those of the contralateral hip, acetabular inclination between 30 and 50°, acetabular anteversion between 5 and 25°, femoral stem longitudinally aligned with axis of the femoral shaft, and a cement mantle thickness of 2–3 mm [111]. Early postoperative radiographic parameters should be recorded for comparison purposes to those obtained in upcoming follow-up [111, 113]. A minimum of 1- and 2-year follow-up visits are recommended with routine radiographs [114••]. In addition to the aforementioned parameters, evaluation of femoral stem subsidence should be emphasized. Acceptable subsidence for taper-slip models should not exceed 5 mm nor progress beyond 2 years [114••]. Evidence of either, especially in symptomatic patients, should be considered evidence of loosening. Furthermore, cement mantle status could be assessed using the Barrack classification [24] (Table 3). Of note, the Barrack classification may be influenced by the extent of cancellous bone removal at reaming and broaching, which may provide a false sense of cement integrity in cases with little to no cancellous bone remnants.
Table 3.
Outline of the Barrack classification [24]
| Grade | Radiographic finding |
|---|---|
| A |
• Cement fills the medullary canal AND • No evidence of radiolucent lines at the cement–bone interface |
| B | • Evidence of radiolucent lines extending ≤ 50% of the cement–bone interface |
| C |
• Evidence of radiolucent lines extending 5–99% of the cement–bone interface OR • Cement mantle defects |
| D |
• Complete radiolucent line (100%) at the cement–bone interface OR • Loss of the cement mantle distal to the femoral stem |
Summary/Conclusion
Femoral stem cementation is a safe and viable alternative to cementless femoral stems and confers superior longevity among certain populations with diminished bone quality. Such process involves sufficient femoral broaching with an appropriate trajectory, canal preparation with the aid of pulse lavage and epinephrine-soaked sponges, vacuum cement mixing, use of cement restrictor, retrograde cement insertion to achieve a ≥ 2-mm cement mantle, cement pressurization, and careful femoral stem insertion with the aid of a stem centralizer. Intricate knowledge of implant properties, cement setting time, and the utilization of the aforementioned fourth-generation cementation techniques are essential for attaining favorable results and mitigating revision rates. Furthermore, adequate communication with the anesthesia team, use of proper cementation techniques, and vigilance of BCIS aid in mitigating intraoperative systemic complications and mortality.
Supplementary Information
(DOCX 16 kb)
Funding
No funding was required for the current investigation.
Compliance with Ethical Standards
V.E.K. reports the following disclosures, none of which are relevant to the topic of the current investigation:
Stryker: royalties; paid speaker; paid consultant.
Journal of Arthroplasty: editorial/governing board.
M.R.B. reports the following disclosures, none of which are relevant to the topic of the current investigation:
AAOS: board or committee member.
R.M.M. reports the following disclosures, none of which are relevant to the topic of the current investigation:
American Association of Hip and Knee Surgeons: board or committee member.
Stryker: paid consultant; paid presenter or speaker; research support.
Zimmer: research support.
N.S.P. reports the following disclosures, none of which are relevant to the topic of the current investigation:
ISCT: board or committee member.
Journal of Hip Surgery: editorial or governing board.
Journal of Knee Surgery: editorial or governing board.
Orthopedic Research Society: board or committee member.
RegenLab: research support.
Zimmer: research support.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Sloan M, Premkumar A, Sheth NP. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J bone joint Surg am United States. 2018;100:1455–1460. doi: 10.2106/JBJS.17.01617. [DOI] [PubMed] [Google Scholar]
- 2.Huo MH, Parvizi J, Bal BS, Mont MA. What’s new in total hip arthroplasty. J Bone Jt Surgery-American. 2009;91:2522–2534. doi: 10.2106/JBJS.I.00801. [DOI] [PubMed] [Google Scholar]
- 3.Paxton EW, Cafri G, Nemes S, Lorimer M, Kärrholm J, Malchau H, Graves SE, Namba RS, Rolfson O. An international comparison of THA patients, implants, techniques, and survivorship in Sweden, Australia, and the United States. Acta Orthop. 2019;90:148–152. doi: 10.1080/17453674.2019.1574395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Joint Registry for England, Wales NI and the I of M. 15th Annual Report 2018. 15th Annu Rep [Internet]. 2018;1821:218. Available from: http://www.njrcentre.org.uk/njrcentre/default.aspx
- 5.Jaffe WL, Hawkins CA. Normalized and proportionalized cemented femoral stem survivorship at 15 years. J Arthroplasty. 1999;14:708–713. doi: 10.1016/s0883-5403(99)90226-7. [DOI] [PubMed] [Google Scholar]
- 6.Bedard NA, Callaghan JJ, Stefl MD, Liu SS. Systematic review of literature of cemented femoral components: what is the durability at minimum 20 years followup? Clin Orthop Relat Res. 2015;473:563–571. doi: 10.1007/s11999-014-3876-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ritter MA, Meneghini RM. Twenty-year survivorship of cementless anatomic graduated component total knee arthroplasty. J Arthroplasty. 2010;25:507–513. doi: 10.1016/j.arth.2009.04.018. [DOI] [PubMed] [Google Scholar]
- 8.Khanuja HS, Vakil JJ, Goddard MS, Mont MA. Cementless femoral fixation in total hip arthroplasty. J Bone Jt Surg. 2011;93:500–509. doi: 10.2106/JBJS.J.00774. [DOI] [PubMed] [Google Scholar]
- 9.Tanzer M, Graves SE, Peng A, Shimmin AJ. Is cemented or cementless femoral stem fixation more durable in patients older than 75 years of age? A comparison of the best-performing stems. Clin Orthop Relat Res. 2018;476:1428–1437. doi: 10.1097/01.blo.0000533621.57561.a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morshed S, Bozic KJ, Ries MD, Malchau H, Colford JM. Comparison of cemented and uncemented fixation in total hip replacement: a meta-analysis. Acta Orthop. 2007;78:315–326. doi: 10.1080/17453670710013861. [DOI] [PubMed] [Google Scholar]
- 11.McMinn DJW, Snell KIE, Daniel J, Treacy RBC, Pynsent PB, Riley RD. Mortality and implant revision rates of hip arthroplasty in patients with osteoarthritis: registry based cohort study. BMJ. BMJ Publishing Group. 2012;345:e3319. doi: 10.1136/bmj.e3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Corbett KL, Losina E, Nti AA, Prokopetz JJZ, Katz JN. Population-based rates of revision of primary total hip arthroplasty: a systematic review. PLoS One. 2010;5:e13520. doi: 10.1371/journal.pone.0013520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang C, Han X, Wang J, Yuan Z, Wang T, Zhao M. Cemented versus uncemented femoral component total hip arthroplasty in elderly patients with primary osteoporosis : retrospective analysis with 5-year follow-up. 2019; [DOI] [PMC free article] [PubMed]
- 14.Valle A, Comba F, Zoppi A, Salvati E. Favourable mid-term results of the VerSys CT polished cemented femoral stem for total hip arthroplasty. Int Orthop. 2006;30:381–386. doi: 10.1007/s00264-006-0077-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Troelsen A, Malchau E, Sillesen N, Malchau H. A review of current fixation use and registry outcomes in total hip arthroplasty: the uncemented paradox. Clin Orthop Relat Res. 2013;471:2052–2059. doi: 10.1007/s11999-013-2941-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones LC, Hungerford DS. Cement disease. Clin Orthop Relat Res. 1987:192–206. [PubMed]
- 17.Emara AK, Klika AK, Piuzzi NS. Evidence-based orthopedic surgery—from synthesis to practice. JAMA Surg. 2020. 10.1001/jamasurg.2020.1521. [DOI] [PubMed]
- 18.Learmonth ID. The evolution of contemporary cementation techniques. Orthopedics SLACK Incorporated. 2005;28:S831–S832. doi: 10.3928/0147-7447-20050802-06. [DOI] [PubMed] [Google Scholar]
- 19.Scanelli JA, Reiser GR, Sloboda JF, Moskal JT. Cemented femoral component use in hip arthroplasty. J Am Acad Orthop Surg. 2019;27:119–127. doi: 10.5435/JAAOS-D-17-00245. [DOI] [PubMed] [Google Scholar]
- 20.Takenaga RK, Callaghan JJ, Bedard NA, Liu SS, Klaassen AL, Pedersen DR. Cementless total hip arthroplasty in patients fifty years of age or younger: a minimum ten-year follow-up. J Bone Jt Surg - Ser A. Journal of Bone and Joint Surgery Inc. 2012;94:2153–2159. doi: 10.2106/JBJS.L.00011. [DOI] [PubMed] [Google Scholar]
- 21.Perticarini L, Zanon G, Rossi SMP, Benazzo FM. Clinical and radiographic outcomes of a trabecular titanium acetabular component in hip arthroplasty: results at minimum 5 years follow-up. BMC Musculoskelet Disord. 2015;16:375. doi: 10.1186/s12891-015-0822-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Malahias M-A, Kostretzis L, Greenberg A, Nikolaou VS, Atrey A, Sculco PK. Highly porous titanium acetabular components in primary and revision total hip arthroplasty: a systematic review. J Arthroplasty. 2020. [DOI] [PubMed]
- 23.Harris WH, Maloney WJ. Hybrid total hip arthroplasty. Clin Orthop Relat Res. 1989:21–9. [PubMed]
- 24.Barrack RL, Mulroy RD, Harris WH. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review. J Bone Joint Surg Br. 1992;74:385–389. doi: 10.1302/0301-620X.74B3.1587883. [DOI] [PubMed] [Google Scholar]
- 25.Firestone DE, Callaghan JJ, Liu SS, Goetz DD, Sullivan PM, Vittetoe DA, et al. Total hip arthroplasty with a cemented, polished, collared femoral stem and a cementless acetabular component. J Bone Jt Surg. 2007;89:126–132. doi: 10.2106/JBJS.E.01214. [DOI] [PubMed] [Google Scholar]
- 26.Moskal JT, Capps SG, Scanelli JA. Still no single gold standard for using cementless femoral stems routinely in total hip arthroplasty. Arthroplast Today. 2016;2:211–218. doi: 10.1016/j.artd.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sierra RJ. Cemented femoral fixation: when is it the right choice? Orthop Proc [Internet]. The British Editorial Society of Bone & Joint Surgery. 2019;101-B:74. doi: 10.1302/1358-992X.2019.8.074. [DOI] [Google Scholar]
- 28.Abdel MP, Watts CD, Houdek MT, Lewallen DG, Berry DJ. Epidemiology of periprosthetic fracture of the femur in 32 644 primary total hip arthroplasties: a 40-year experience. Bone Joint J England. 2016;98-B:461–467. doi: 10.1302/0301-620X.98B4.37201. [DOI] [PubMed] [Google Scholar]
- 29.Chammout G, Muren O, Laurencikas E, Bodén H, Kelly-Pettersson P, Sjöö H, et al. More complications with uncemented than cemented femoral stems in total hip replacement for displaced femoral neck fractures in the elderly: a single-blinded, randomized controlled trial with 69 patients. Acta Orthop. 2017;88:145–151. doi: 10.1080/17453674.2016.1262687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lamb JN, King SW, van Duren BH, West RM, Pandit HG. Comparison of cementless versus cemented stem survival: an analysis of 2934 patients with bilateral hip arthroplasties in the National Joint Registry of England and Wales. Orthop Proc [Internet]. The British Editorial Society of Bone & Joint Surgery; 2019;101-B:20. Available from: 10.1302/1358-992X.2019.6.020
- 31.Kristensen TB, Dybvik E, Kristoffersen M, Dale H, Engesaeter LB, Furnes O, et al. Cemented or uncemented hemiarthroplasty for femoral neck fracture? Data from the Norwegian Hip Fracture Register. Clin Orthop Relat Res. 2020;478:90–100. doi: 10.1097/CORR.0000000000000826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hailer NP, Garellick G, Karrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish hip arthroplasty register. Acta Orthop England. 2010;81:34–41. doi: 10.3109/17453671003685400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Malviya A, Abdul N, Khanduja V. Outcomes following total hip arthroplasty: a review of the registry data. Indian J Orthop. 2017;51:405–413. doi: 10.4103/ortho.IJOrtho_177_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Evans JT, Evans JP, Walker RW, Blom AW, Whitehouse MR, Sayers A. How long does a hip replacement last ? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet [Internet]. The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY 4.0 license; 2016;393:647–54. Available from: 10.1016/S0140-6736(18)31665-9 [DOI] [PMC free article] [PubMed]
- 35.Maggs J, Wilson M. The relative merits of cemented and uncemented prostheses in total hip arthroplasty. Indian J Orthop [internet]. Medknow Publications & Media Pvt ltd; 2017;51:377–85. Available from: https://www.ncbi.nlm.nih.gov/pubmed/28790466. [DOI] [PMC free article] [PubMed]
- 36.Kiran M, Johnston LR, Sripada S, Mcleod GG, Jariwala AC. Cemented total hip replacement in patients under 55 years. Acta Orthop [Internet]. 2018/01/18. Taylor & Francis; 2018;89:152–5. Available from: https://pubmed.ncbi.nlm.nih.gov/29345170 [DOI] [PMC free article] [PubMed]
- 37.NJR. 14th Annual Report National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. Natl. Jt. Regist. 2017.
- 38.Vidalain JP. Twenty-year results of the cementless Corail stem. Int Orthop Springer. 2011;35:189–194. doi: 10.1007/s00264-010-1117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McLaughlin JR, Lee KR. Total hip arthroplasty with an uncemented tapered femoral component in patients younger than 50 years of age: a minimum 20-year follow-up study. J Arthroplasty. Churchill Livingstone Inc.; 2016;31:1275–8. [DOI] [PubMed]
- 40.Cherian JJ, Jauregui JJ, Banerjee S, Pierce T, Mont MA. What host factors affect aseptic loosening after THA and TKA? Clin. Orthop. Relat. Res. Springer New York LLC. 2015:2700–9. [DOI] [PMC free article] [PubMed]
- 41.Chareancholvanich K, Bourgeault CA, Schmidt AH, Gustilo RB, Lew WD. In vitro stability of cemented and cementless femoral stems with compaction. Clin Orthop Relat Res. United States. 2002;394:290–302. doi: 10.1097/00003086-200201000-00034. [DOI] [PubMed] [Google Scholar]
- 42.Kobayashi S, Takaoka K, Saito N, Hisa K. Factors affecting aseptic failure of fixation after primary Charnley total hip arthroplasty. Multivariate survival analysis. J Bone Joint Surg Am United States. 1997;79:1618–1627. doi: 10.2106/00004623-199711000-00002. [DOI] [PubMed] [Google Scholar]
- 43.Wroblewski BM, Siney PD, Fleming PA. Triple taper polished cemented stem in total hip arthroplasty: rationale for the design, surgical technique, and 7 years of clinical experience. J Arthroplasty United States. 2001;16:37–41. doi: 10.1054/arth.2001.28374. [DOI] [PubMed] [Google Scholar]
- 44.Spitzer AI. The cemented femoral stem: selecting the ideal patient. Orthopedics United States. 2005;28:s841–s848. doi: 10.3928/0147-7447-20050802-08. [DOI] [PubMed] [Google Scholar]
- 45.Donaldson AJ, Thomson HE, Harper NJ, Kenny NW. Bone cement implantation syndrome. Br J Anaesth England. 2009;102:12–22. doi: 10.1093/bja/aen328. [DOI] [PubMed] [Google Scholar]
- 46.Olsen F, Kotyra M, Houltz E, Ricksten S-E. Bone cement implantation syndrome in cemented hemiarthroplasty for femoral neck fracture: incidence, risk factors, and effect on outcome. BJA Br J Anaesth [internet]. 2014;113:800–6. Available from: 10.1093/bja/aeu226, 2014. [DOI] [PubMed]
- 47.Hines CB. Understanding bone cement implantation syndrome. AANA J United States. 2018;86:433–441. [PubMed] [Google Scholar]
- 48.Vaishya R, Chauhan M, Vaish A. Bone cement. J Clin Orthop Trauma. 2013/12/15 Elsevier. 2013;4:157–163. doi: 10.1016/j.jcot.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Piuzzi NS, Zanotti G, Comba FM, Buttaro MA, Piccaluga F. Paradoxical cerebral fat embolism in revision hip surgery. Case Rep Orthop. 2014;2014:140757. doi: 10.1155/2014/140757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Khanna G, Cernovsky J. Bone cement and the implications for anaesthesia. Contin Educ Anaesth Crit care pain [internet]. 2012;12:213–6. Available from: 10.1093/bjaceaccp/mks011, 2012.
- 51.Maggs J, Wilson M. The relative merits of cemented and uncemented prostheses in total hip arthroplasty. Indian J Orthop. Medknow Publications & Media Pvt Ltd. 2017;51:377–385. doi: 10.4103/ortho.IJOrtho_405_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shen G. Femoral stem fixation. An engineering interpretation of the long-term outcome of Charnley and Exeter stems. J bone joint Surg Br England. 1998;80:754–756. doi: 10.1302/0301-620x.80b5.8621. [DOI] [PubMed] [Google Scholar]
- 53.Fowler JL, Gie GA, Lee AJ, Ling RS. Experience with the Exeter total hip replacement since 1970. Orthop Clin North Am United States. 1988;19:477–489. [PubMed] [Google Scholar]
- 54.Kaneuji A, Yamada K, Hirosaki K, Takano M, Matsumoto T. Stem subsidence of polished and rough double-taper stems: in vitro mechanical effects on the cement–bone interface. Acta Orthop [internet] Informa Healthcare. 2009;80:270–276. doi: 10.3109/17453670902967265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Verdonschot N, Huiskes R. Surface roughness of debonded straight-tapered stems in cemented THA reduces subsidence but not cement damage. Biomaterials Netherlands. 1998;19:1773–1779. doi: 10.1016/s0142-9612(98)00088-x. [DOI] [PubMed] [Google Scholar]
- 56.Kazi HA, Whitehouse SL, Howell JR, Timperley AJ. Not all cemented hips are the same: a register-based (NJR) comparison of taper-slip and composite beam femoral stems. Acta Orthop. 2019;90:214–219. doi: 10.1080/17453674.2019.1582680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Huiskes R, Verdonschot N, Nivbrant B. Migration, stem shape, and surface finish in cemented total hip arthroplasty. Clin Orthop Relat Res. United States. 1998;355:103–112. doi: 10.1097/00003086-199810000-00011. [DOI] [PubMed] [Google Scholar]
- 58.Hutt J, Hazlerigg A, Aneel A, Epie G, Dabis H, Twyman R, et al. The effect of a collar and surface finish on cemented femoral stems: a prospective randomised trial of four stem designs. Int Orthop [internet]. 2014/01/29. Springer Berlin Heidelberg. 2014;38:1131–1137. doi: 10.1007/s00264-013-2256-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jayasuriya RL, Buckley SC, Hamer AJ, Kerry RM, Stockley I, Tomouk MW, et al. Effect of sliding-taper compared with composite-beam cemented femoral prosthesis loading regime on proximal femoral bone remodeling: a randomized clinical trial. J Bone Joint Surg Am United States. 2013;95:19–27. doi: 10.2106/JBJS.K.00657. [DOI] [PubMed] [Google Scholar]
- 60.Kedgley AE, Takaki SE, Lang P, Dunning CE. The effect of cross-sectional stem shape on the torsional stability of cemented implant components. J Biomech Eng United States. 2007;129:310–314. doi: 10.1115/1.2720907. [DOI] [PubMed] [Google Scholar]
- 61.Scheerlinck T, Casteleyn P-P. The design features of cemented femoral hip implants. J bone joint Surg Br [internet]. The British editorial Society of Bone & joint surgery; 2006;88-B:1409–18. Available from: 10.1302/0301-620X.88B11.17836, 2006. [DOI] [PubMed]
- 62.van der Voort P, Pijls BG, Nieuwenhuijse MJ, Jasper J, Fiocco M, Plevier JWM, et al. Early subsidence of shape-closed hip arthroplasty stems is associated with late revision. A systematic review and meta-analysis of 24 RSA studies and 56 survival studies. Acta Orthop [internet]. Informa Healthcare. 2015;86:575–585. doi: 10.3109/17453674.2015.1043832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Verdonschot N. Philosophies of stem designs in cemented total hip replacement. Orthopedics. United States. 2005;28:s833–s840. doi: 10.3928/0147-7447-20050802-07. [DOI] [PubMed] [Google Scholar]
- 64.Suh DH, Yun HH, Chun SK, Shon WY. Fifteen-year results of precoated femoral stem in primary hybrid total hip arthroplasty. Clin Orthop Surg [internet]. 2013/05/15. The Korean Orthopaedic Association. 2013;5:110–117. doi: 10.4055/cios.2013.5.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ong A, Wong KL, Lai M, Garino JP, Steinberg ME. Early failure of precoated femoral components in primary total hip arthroplasty. J Bone Joint Surg Am. United States. 2002;84:786–792. doi: 10.2106/00004623-200205000-00014. [DOI] [PubMed] [Google Scholar]
- 66.Shon WY, Chotai P, Siddaraju VK. Fifteen year results of hybrid THA using a precoated femoral stem: a single center experience. Orthop Proc [Internet]. The British Editorial Society of Bone & Joint Surgery; 2012;94-B:217. Available from: 10.1302/1358-992X.94BSUPP_XXV.ISTA2010-217
- 67.Makela K, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. Cemented total hip replacement for primary osteoarthritis in patients aged 55 years or older: results of the 12 most common cemented implants followed for 25 years in the Finnish arthroplasty register. J Bone Joint Surg Br England. 2008;90:1562–1569. doi: 10.1302/0301-620X.90B12.21151. [DOI] [PubMed] [Google Scholar]
- 68.Sanchez-Sotelo J, Berry DJ, Harmsen S. Long-term results of use of a collared matte-finished femoral component fixed with second-generation cementing techniques: a fifteen-year-median follow-up study. J Bone Jt Surg - Ser A. Journal of Bone and Joint Surgery Inc.; 2002;84:1636–41. [DOI] [PubMed]
- 69.Collis DK, Mohler CG. Comparison of clinical outcomes in total hip arthroplasty using rough and polished cemented stems with essentially the same geometry. J Bone Jt Surg - Ser A. Journal of Bone and Joint Surgery Inc.; 2002;84:586–92. [DOI] [PubMed]
- 70.Howie DW, Middleton RG, Costi K. Loosening of matt and polished cemented femoral stems. J Bone Joint Surg Br. 1998;80:573–576. doi: 10.1302/0301-620x.80b4.8629. [DOI] [PubMed] [Google Scholar]
- 71.Verdonschot N. Stem design philosophies. Well-Cemented Total Hip Arthroplast Theory Pract. Springer Berlin Heidelberg; 2005. p. 168–79.
- 72.Menken LG, Berliner ZP, Mercer N, Rodriguez JA. Cemented primary total hip arthroplasty using a direct anterior approach. Semin Arthroplasty [Internet]. 2018;29:147–52. Available from: http://www.sciencedirect.com/science/article/pii/S1045452719300227
- 73.Noordin S, Lakdawala R, Masri BA. Primary total hip arthroplasty: staying out of trouble intraoperatively. Ann Med Surg. 2018;29:30–33. doi: 10.1016/j.amsu.2018.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yang L, Zheng Z, Chen W, Wang J, Zhang Y. Femoral neck osteotomy guide for total hip arthroplasty. BMC Surg [Internet]. BioMed Central; 2015;15:29. Available from: https://pubmed.ncbi.nlm.nih.gov/25887586 [DOI] [PMC free article] [PubMed]
- 75.Morley JR, Barker R, Howell JR. Cemented total hip replacement. BT - European Surgical Orthopaedics and Traumatology: The EFORT Textbook. In: Bentley G, editor. Berlin, Heidelberg: Springer Berlin Heidelberg; 2014. p. 2397–422. Available from: 10.1007/978-3-642-34746-7_226.
- 76.DiGiovanni CW, Garvin KL, Pellicci PM. Femoral preparation in cemented total hip arthroplasty: reaming or broaching? J Am Acad Orthop Surg United States. 1999;7:349–357. doi: 10.5435/00124635-199911000-00001. [DOI] [PubMed] [Google Scholar]
- 77.Kapoor B, Datir SP, Davis B, Wynn-Jones CH, Maffulli N. Femoral cement pressurization in hip arthroplasty: a laboratory comparison of three techniques. Acta Orthop Scand. 2004;75:708–712. doi: 10.1080/00016470410004076. [DOI] [PubMed] [Google Scholar]
- 78.Korhonen RK, Koistinen A, Konttinen YT, Santavirta SS, Lappalainen R. The effect of geometry and abduction angle on the stresses in cemented UHMWPE acetabular cups—finite element simulations and experimental tests. Biomed Eng Online. 2005;4:1–14. doi: 10.1186/1475-925X-4-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Daniel J. Berry; Mark W Pagano. Illustrated Tips and Tricks in Hip and Knee Reconstructive and Replacement. Lippincott Williams & Wilkins. 2019.
- 80.Bombardieri AM, Sharrock NE, Ma Y, Go G, Drummond JC. An observational study of cerebral blood flow velocity during hypotensive epidural anesthesia. Anesth Analg United States. 2016;122:226–233. doi: 10.1213/ANE.0000000000000985. [DOI] [PubMed] [Google Scholar]
- 81.Badiola IJ, Liu J, Neuman MD. Deliberate hypotension for hip arthroplasty: still more questions than answers. Anesth Analg [Internet] 2016;122:15–16. doi: 10.1213/ANE.0000000000001000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Maloney WJ. Femoral cementing techniques: lest we forget. Orthop Proc [Internet]. The British Editorial Society of Bone & Joint Surgery; 2017;99-B:113. Available from: 10.1302/1358-992X.99BSUPP_15.CCJR2017-113
- 83.Pitto RP, Koessler M, Kuehle JW. Comparison of fixation of the femoral component without cement and fixation with use of a bone-vacuum cementing technique for the prevention of fat embolism during total hip arthroplasty. A prospective, randomized clinical trial. J Bone Joint Surg Am. United States. 1999;81:831–843. doi: 10.2106/00004623-199906000-00010. [DOI] [PubMed] [Google Scholar]
- 84.Geiger MH, Keating EM, Ritter MA, Ginther JA, Faris PM, Meding JB. The clinical significance of vacuum mixing bone cement. Clin Orthop Relat Res United States. 2001;382:258–266. doi: 10.1097/00003086-200101000-00034. [DOI] [PubMed] [Google Scholar]
- 85.Lidgren L, Bodelind B, Möller J. Bone cement improved by vacuum mixing and chilling 2009;6470. [DOI] [PubMed]
- 86.Gheduzzi S. Femoral cementing techniques: current trends in the UK. 2017; [DOI] [PMC free article] [PubMed]
- 87.Waanders D, Janssen D, Mann KA, Verdonschot N. The mechanical effects of different levels of cement penetration at the cement–bone interface. J Biomech. 2010;43:1167–1175. doi: 10.1016/j.jbiomech.2009.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sharrock NE, Go G, Harpel PC, Ranawat CS, Sculco TP, Salvati EA. The John Charnley Award. Thrombogenesis during total hip arthroplasty. Clin Orthop Relat Res. United States. 1995:16–27. [PubMed]
- 89.Westrich GH, Salvati EA, Sharrock N, Potter HG, Sánchez PM, Sculco TP. The effect of intraoperative heparin administered during total hip arthroplasty on the incidence of proximal deep vein thrombosis assessed by magnetic resonance venography. J Arthroplast. 2005;20:42–50. doi: 10.1016/j.arth.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 90.Huo MH, Salvati EA, Sharrock NE, Brien WW, Sculco TP, Pellicci PM, et al. Intraoperative heparin thromboembolic prophylaxis in primary total hip arthroplasty. A prospective, randomized, controlled, clinical trial. Clin Orthop Relat Res. United States; 1992;35–46. [PubMed]
- 91.Sharrock MB, ChB NE, Go BSG, Sculco MDTP, Salvati MDEA, Westrich MDGH, Harpel MDPC. Dose response of intravenous heparin on markers of thrombosis during primary total hip replacement. Anesthesiol J Am Soc Anesthesiol. 1999;90:981–987. doi: 10.1097/00000542-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 92.Chen CM, Ashjian P, Disa JJ, Cordeiro PG, Pusic AL, Mehrara BJ. Is the use of intraoperative heparin safe? Plast Reconstr Surg. United States. 2008;121:49e–53e. doi: 10.1097/01.prs.0000299267.84139.2a. [DOI] [PubMed] [Google Scholar]
- 93.McDougall CJ, Gray HS, Simpson PM, Whitehouse SL, Crawford RW, Donnelly WJ. Complications related to therapeutic anticoagulation in total hip arthroplasty. J Arthroplasty [internet]. Elsevier Inc.; 2013;28:187–92. Available from: 10.1016/j.arth.2012.06.001, 2013. [DOI] [PubMed]
- 94.Nassif JM, Ritter MA, Meding JB, Keating EM, Faris PM. The effect of intraoperative intravenous fixed-dose heparin during total joint arthroplasty on the incidence of fatal pulmonary emboli. J Arthroplasty [internet]. Elsevier; 2000;15:16–21. Available from: 10.1016/S0883-5403(00)91025-8, 2000. [DOI] [PubMed]
- 95.Kusserow A, Ficklscherer A, Kreuz PC, Finze S, Mittelmeier W, Jansson V, et al. Importance of a distal centralizer in experimental malpositioning of cemented stems. A biomechanical study on human femora. Arch Med Sci [internet]. 2015/12/11. Termedia Publishing House. 2015;11:1324–1329. doi: 10.5114/aoms.2015.56361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Weber E, Olsson C, Kesteris U, Flivik G. Is a hollow centralizer necessary when using a polished, tapered, cemented femoral stem? Acta Orthop. 2017;88:377–382. doi: 10.1080/17453674.2017.1315553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Churchill DL, Incavo SJ, Uroskie JA, Beynnon BD. Femoral stem insertion generates high bone cement pressurization. Clin Orthop Relat Res. United States. 2001;393:335–344. doi: 10.1097/00003086-200112000-00039. [DOI] [PubMed] [Google Scholar]
- 98.Hunt S, Stone C, Seal S. Timing of femoral prosthesis insertion during cemented arthroplasty: cement curing and static mechanical strength in an in vivo model. Can J Surg. 2011;54:33–38. doi: 10.1503/cjs.001110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Shepard MF, Kabo JM, Lieberman JR. The Frank Stinchfield Award. Influence of cement technique on the interface strength of femoral components. Clin Orthop Relat Res. United States. 2000:26–35. [DOI] [PubMed]
- 100.Baleani M, Bialoblocka-Juszczyk E, Engels GE, Viceconti M. The effect of vacuum mixing and pre-heating the femoral component on the mechanical properties of the cement mantle. J Bone Jt Surg - Ser B. 2010;92:454–460. doi: 10.1302/0301-620X.92B3.22579. [DOI] [PubMed] [Google Scholar]
- 101.Hsieh P-H, Tai C-L, Chang Y-H, Lee MS, Shih H-N, Shih C-H. Precooling of the femoral canal enhances shear strength at the cement–prosthesis interface and reduces the polymerization temperature. J Orthop Res United States. 2006;24:1809–1814. doi: 10.1002/jor.20242. [DOI] [PubMed] [Google Scholar]
- 102.Iesaka K, Jaffe WL, Kummer FJ. Effects of preheating of hip prostheses on the stem–cement interface. J Bone Joint Surg Am. United States. 2003;85:421–427. doi: 10.2106/00004623-200303000-00003. [DOI] [PubMed] [Google Scholar]
- 103.Jafri AA, Green SM, Partington PF, McCaskie AW, Muller SD. Pre-heating of components in cemented total hip arthroplasty. J Bone Jt Surg - Ser B. 2004;86:1214–1219. doi: 10.1302/0301-620x.86b8.14660. [DOI] [PubMed] [Google Scholar]
- 104.Wilairatana V, Pirot C, Limpaphayom N. Effects of cemented hip stem pre-heating on stem push-out strength. Orthop Surg [Internet]. John Wiley and Sons Inc.; 2015;7:261–5. Available from: https://pubmed.ncbi.nlm.nih.gov/26311102 [DOI] [PMC free article] [PubMed]
- 105.Bishop NE, Ferguson S, Tepic S. Porosity reduction in bone cement at the cement–stem interface. J Bone Jt Surg - Ser B. 1996;78:349–356. [PubMed] [Google Scholar]
- 106.Saleh KJ, El Othmani MM, Tzeng TH, Mihalko WM, Chambers MC, Grupp TM. Acrylic bone cement in total joint arthroplasty: a review. J Orthop Res. 2016;34:737–744. doi: 10.1002/jor.23184. [DOI] [PubMed] [Google Scholar]
- 107.Katzer A, Ince A, Hahn M, Morlock MM, Steens W. Cement mantle defects in total hip arthroplasty: influence of stem size and cementing technique. J Orthop Traumatol. 2007;8:167–172. [Google Scholar]
- 108.Digas G, Kärrholm J. The implant–cement Interface in total hip arthroplasty. BT - bone–implant interface in orthopedic surgery: basic science to clinical applications. In: Karachalios T, editor. London: Springer; 2014. p. 35–54. Available from: 10.1007/978-1-4471-5409-9_4, 2014.
- 109.Rajeev A, Mohamed A, Shaikh M, Banaszkiewicz P. Dislodgement of a cemented Exeter femoral stem during closed manipulative reduction of a dislocated total hip replacement. Int J Surg Case Rep [Internet]. 2016/03/18. Elsevier; 2016;22:66–9. Available from: https://pubmed.ncbi.nlm.nih.gov/27060643 [DOI] [PMC free article] [PubMed]
- 110.Mulhall KJ, Masterson E, Burke TE. Routine recovery room radiographs after total hip arthroplasty: ineffective for screening and unsuitable as baseline for longitudinal follow-up evaluation. J Arthroplasty. United States. 2004;19:313–317. doi: 10.1016/j.arth.2003.08.021. [DOI] [PubMed] [Google Scholar]
- 111.Vanrusselt J, Vansevenant M, Vanderschueren G, Vanhoenacker F. Postoperative radiograph of the hip arthroplasty: what the radiologist should know. Insights Imaging. 2015;6:591–600. doi: 10.1007/s13244-015-0438-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ndu A, Jegede K, Bohl DD, Keggi K, Grauer JN. Recovery room radiographs after total hip arthroplasty: tradition vs utility? J Arthroplasty. 2012;27:1051–1056. doi: 10.1016/j.arth.2011.12.020. [DOI] [PubMed] [Google Scholar]
- 113.Teo TL, Schaeffer EK, Mulpuri K. Need for higher quality evidence to determine the utility of postoperative radiography. JAAOS Glob Res Rev [Internet]. 2018;2. Available from: https://journals.lww.com/jaaosglobal/Fulltext/2018/08000/Need_for_Higher_Quality_Evidence_to_Determine_the.2.aspx [DOI] [PMC free article] [PubMed]
- 114.Cassar-Gheiti AJ, McColgan R, Kelly M, Cassar-Gheiti TM, Kenny P, Murphy CG. Current concepts and outcomes in cemented femoral stem design and cementation techniques: the argument for a new classification system. EFORT open Rev. 2020;5:241–252. doi: 10.1302/2058-5241.5.190034. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 16 kb)