Abstract
Previous studies have suggested an increased risk of ischemic heart disease related to air pollution. This study aimed to explore both the short-term and long-term effects of air pollutants on the risk of ischemic heart disease after adjusting for meteorological factors. The Korean National Health Insurance Service-Health Screening Cohort from 2002 to 2013 was used. Overall, 2155 participants with ischemic heart disease and 8620 control participants were analyzed. The meteorological data and air pollution data, including SO2 (ppm), NO2 (ppm), O3 (ppm), CO (ppm), and particulate matter (PM)10 (μg/m3), were analyzed using conditional logistic regression. Subgroup analyses were performed according to age, sex, income, and region of residence. One-month exposure to SO2 was related to 1.36-fold higher odds for ischemic heart disease (95% confidence interval [95% CI] 1.06–1.75). One-year exposure to SO2, O3, and PM10 was associated with 1.58- (95% CI 1.01–2.47), 1.53- (95% CI 1.27–1.84), and 1.14 (95% CI 1.02–1.26)-fold higher odds for ischemic heart disease. In subgroup analyses, the ≥ 60-year-old group, men, individuals with low income, and urban groups demonstrated higher odds associated with 1-month exposure to SO2. Short-term exposure to SO2 and long-term exposure to SO2, O3, and PM10 were related to ischemic heart disease.
Subject terms: Cardiology, Medical research
Introduction
Ischemic heart disease is a fatal disease with high morbidity and mortality. The prevalence increased from the early twentieth century to the 1960s, likely due to the increase in smoking and high fat intake, which promote the development of coronary atherosclerosis1. Although the prevalence and mortality of ischemic heart disease have decreased, it is still one of the leading causes of mortality worldwide2,3. Atherosclerotic and calcified plaques in coronary arteries have been described as the main pathologies of ischemic heart disease4. Inflammation in the cardiovascular system has been suggested to cause these changes in coronary vessels and to be linked with systemic inflammatory diseases5.
Although early diagnosis and intervention increase the survival rate of ischemic heart disease, the primary prevention of ischemic heart disease might be most effective at reducing disease burden. Several modifiable risk factors have been reported, including the lifestyle factors of obesity, alcohol consumption, and tobacco smoking6–8. In addition to these lifestyle factors, which are largely dependent on individuals, an accumulating number of studies has documented that environmental factors, including toxic compounds, could be modifiable factors to prevent the risk of ischemic heart disease at the social level9.
Many previous epidemiologic studies have described an increased risk of ischemic heart disease related to air pollution10–16, particularly long-term exposure to air pollution11,17. On the other hand, the effect of short-term exposure to air pollution has also been suggested, with some conflicting findings10,18. A case-crossover study reported that a 10 µg/m3 increase in exposure to fine particulate pollution (particulate matter with an aerodynamic diameter ≤ 2.5 µm; PM2.5) was associated with a 4.5% increased risk of ischemic heart disease (95% CI 1.1–8.0)10. However, a time-series study demonstrated that increased exposure to sulfur dioxide (SO2), but not PM2.5 or nitrogen dioxide (NO2), for 3 days was related to an increased risk of ischemic heart disease mortality18. The heterogeneous study design, regional and ethnic differences and types of measured pollutants might have contributed to these controversial results.
Few studies have reported a wide range of air pollution exposure periods from short-term to long-term exposure. Moreover, when exploring the effect of air pollution, meteorological factors should be concurrently considered because the concentration and composition of air pollutants might be influenced by these factors, and the risk of cardiovascular disease could be associated with meteorological factors, such as ambient temperature19. For instance, the solubility of air pollutants is increased at lower temperatures, and the photolysis reaction could change the composition of air pollutants. Therefore, this study analyzed the effect of air pollutants on ischemic heart disease according to exposure periods prior to the development of ischemic heart disease. To evaluate this effect, we calculated the mean levels of air pollutants for time periods from 3 to 730 days of exposure. To minimize the confounding effects of meteorological factors, they were concurrently analyzed for their association with ischemic heart disease.
Materials and methods
Participant selection
This study was approved by the Ethics Committee of Hallym University (2017-I102) and was exempt from requiring informed consent20. All procedures were followed in accordance with the relevant guidelines. The Korean National Health Insurance Service-Health Screening Cohort (NHIS-HEALS), meteorological, and air pollution data were used (S1 description)20–22.
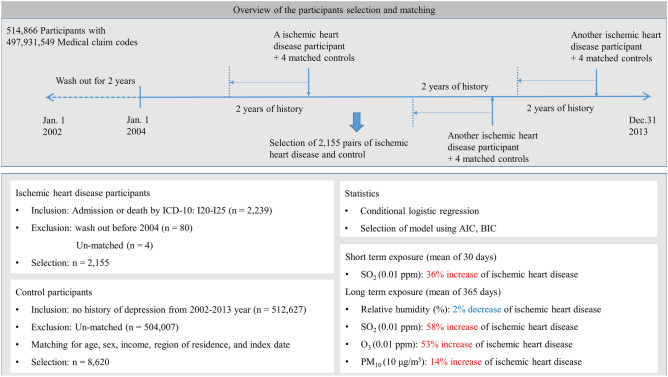
Participants with ischemic heart disease were selected from 514,866 patients with 497,931,549 medical claim codes (n = 2239)20–22. Among these participants, individuals were excluded if they were diagnosed with ischemic heart disease before 2004 (n = 80) to track previous exposure to meteorological factors in the last 2 years. The control group included those without a history of ischemic heart disease from 2002 through 2013 (n = 512,627)20–22. The control participants were 1:4 matched for age, sex, income, region of residence, and index date20.
The index date of ischemic heart disease participants was set as the time of diagnosis of ischemic heart disease20–22. Some ischemic heart disease participants were excluded because there were not enough matched control participants (n = 4). Collectively, 2155 ischemic heart disease participants were 1:4 matched with 8620 control participants (Fig. 1)20–22.
Figure 1.
A schematic illustration of the participant selection process used in the present study. Of 1,125,691 participants, 2155 ischemic heart disease participants were matched with 8620 control participants for age, group, sex, income group, and region of residence. Then, ischemic heart disease patients and control participants were matched according to the meteorological data and air pollution data before the index date.
We analyzed meteorological and air pollution data over a mean of 3 days, 5 days, 10 days, 15 days, 1 month (30 days), 2 months (60 days), 3 months (90 days), 6 months (180 days), 9 months (270 days), 1 year (365 days), 18 months (540 days), and 2 years (730 days) before the date of diagnosis or the index date in each participant according to their region of residence.
Variables
Independent variables
Daily mean temperature (°C), daily highest temperature (°C), daily lowest temperature (°C), relative humidity (%), ambient atmospheric pressure (hPa), SO2 (ppm), NO2 (ppm), O3 (ppm), CO (ppm), and PM10 (μg/m3) for 3 days, 5 days, 10 days, 15 days, 1 month (30 days), 2 months (60 days), 3 months (90 days), 6 months (180 days), 9 months (270 days), 1 year (365 days), 18 months (540 days), and 2 years (730 days) were analyzed as independent variables (S1 description)20. These data were gathered from Air Korea, which is managed by the Ministry of Environment of Korea23. The air pollution and meteorological factors measured at the closest points to the region of residence of participants were applied for analyses.
Dependent variable
Ischemic heart disease was classified using ICD-10 codes (I20-I25). Among the participants, those who were hospitalized because of ischemic heart disease or who died because of ischemic heart disease were included24.
Covariate
Age groups were classified in 5-year intervals: 40–44, 45–49, 50–54…, and 85 + years old. Income groups were divided into 5 classes (class 1 [lowest income]-5 [highest income]). The region of residence was grouped into urban and rural areas25.
Tobacco smoking, alcohol consumption, and obesity using BMI (body mass index, kg/m2) were included26.
Statistical analyses
The general characteristics of the ischemic heart disease and control groups were compared using the chi-square test20. The mean meteorological and air pollution data 30 days and 365 days before the index date were compared using independent t-tests.
To analyze the odds ratios (ORs) with the 95% confidence intervals (CIs) of meteorological and air pollution data for ischemic heart disease participants compared to control participants, a crude model (simple model), adjusted model (all insertion model), and final model (backward selection of variables) were calculated using conditional logistic regression20. As ORs of independent variables were calculated as continuous variables, they were displayed as SO2 per 0.01 ppm, NO2 per 0.1 ppm, O3 per 0.01 ppm, CO per 1 ppm, and PM10 per 10 μg/m3. In these analyses, age, sex, income, and region of residence were stratified. In the analyses of 3 days, 5 days, 10 days, 15 days, 30 days, 60 days, 90 days, 180 days, 270 days, 365 days, 540 days, and 730 days of exposure, we selected 30 days as the short-term exposure and 365 days as the long-term exposure20. The results of other days of exposure are displayed in the supplemental file (Supplementary Tables S2–S12). To select final models, Akaike information criterion and Baysian information criterion of air pollutants were analyzed (Supplementary Table S13). The correlations between meteorological and air pollutants were provided as supplemental tables (Supplementary Tables S14–S15).
For the subgroup analysis, we divided participants by age, sex, income, and region (< 60 years old and ≥ 60 years old; men and women; low income [income 1–3] and high income [income 4–5]; urban and rural, respectively) in the final model20.
Two-tailed analyses were performed, and significance was defined as P values less than 0.05. SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) was used for statistical analyses20.
Results
Regarding meteorological and air pollution data, SO2 for 30 days, temperature (mean, highest, and lowest), relative humidity, SO2, NO2 and CO for 365 days were different between the ischemic heart disease group and the control group (all P < 0.05, Table 1).
Table 1.
General characteristics of the participants.
| Characteristics | Total participants | ||
|---|---|---|---|
| IHD | Control | P-value | |
| Age (years old, n, %) | 1.000 | ||
| 40–44 | 12 (0.6) | 48 (0.6) | |
| 45–49 | 62 (2.9) | 248 (2.9) | |
| 50–54 | 139 (6.5) | 556 (6.5) | |
| 55–59 | 151 (7.0) | 604 (7.0) | |
| 60–64 | 176 (8.2) | 704 (8.2) | |
| 65–69 | 315 (14.6) | 1260 (14.6) | |
| 70–74 | 408 (18.9) | 1632 (18.9) | |
| 75–79 | 397 (18.4) | 1588 (18.4) | |
| 80–84 | 364 (16.9) | 1456 (16.9) | |
| 85 + | 131 (6.1) | 524 (6.1) | |
| Sex (n, %) | 1.000 | ||
| Male | 1447 (67.2) | 5788 (67.2) | |
| Female | 708 (32.9) | 2832 (32.9) | |
| Income (n, %) | 1.000 | ||
| 1 (lowest) | 475 (22.0) | 1900 (22.0) | |
| 2 | 304 (14.1) | 1216 (14.1) | |
| 3 | 308 (14.3) | 1232 (14.3) | |
| 4 | 411 (19.1) | 1644 (19.1) | |
| 5 (highest) | 657 (30.5) | 2628 (30.5) | |
| Region of residence (n, %) | 1.000 | ||
| Urban | 831 (38.6) | 3324 (38.6) | |
| Rural | 1324 (61.4) | 5296 (61.4) | |
| Charlson comorbidity index (n, %) | < 0.001* | ||
| 0 | 1938 (89.9) | 8352 (96.9) | |
| 1 | 34 (1.6) | 26 (0.3) | |
| 2 | 41 (1.9) | 41 (0.5) | |
| 3 | 34 (1.6) | 33 (0.4) | |
| ≥ 4 | 108 (5.0) | 168 (2.0) | |
| Obesity (BMI, kg/m2, n, %) | < 0.001* | ||
| < 18.5 (underweight) | 143 (6.6) | 376 (4.4) | |
| ≥ 18.5 to < 23 (normal) | 833 (38.7) | 3290 (38.2) | |
| ≥ 23 to < 25 (overweight) | 511 (23.7) | 2224 (25.8) | |
| ≥ 25 to < 30 (obese I) | 604 (28.0) | 2512 (29.1) | |
| ≥ 30 (obese II) | 64 (3.0) | 218 (2.5) | |
| Smoking status (n, %) | < 0.001* | ||
| Nonsmoker | 1310 (60.8) | 5746 (66.7) | |
| Past smoker | 262 (12.2) | 1242 (14.4) | |
| Current smoker | 583 (27.1) | 1632 (18.9) | |
| Alcohol consumption (n, %) | < 0.001* | ||
| < 1 time a week | 1682 (78.1) | 6412 (74.4) | |
| ≥ 1 time a week | 473 (22.0) | 2208 (25.6) | |
| Meteorological and air pollution data (mean, SD) | |||
| Mean temperature for 30 days (°C) | 12.2 (9.5) | 12.1 (9.5) | 0.868 |
| Highest temperature for 30 days (°C) | 17.4 (9.3) | 17.4 (9.3) | 0.937 |
| Lowest temperature for 30 days (°C) | 7.7 (9.9) | 7.6 (9.9) | 0.805 |
| Relative humidity for 30 days (%) | 65.2 (10.1) | 65.4 (10.0) | 0.308 |
| Ambient atmospheric pressure for 30 days (hPa) | 1006.3 (7.5) | 1006.3 (7.4) | 0.707 |
| SO2 for 30 days (ppb) | 5.7 (1.9) | 5.6 (1.9) | 0.016* |
| NO2 for 30 days (ppb) | 23.5 (8.1) | 23.8 (8.2) | 0.129 |
| O3 for 30 days (ppb) | 23.3 (8.2) | 23.1 (8.3) | 0.243 |
| CO for 30 days (ppb) | 571.4 (182.4) | 571.0 (179.3) | 0.940 |
| PM10 for 30 days (μg/m3) | 52.0 (14.5) | 51.9 (14.8) | 0.862 |
| Mean temperature for 365 days (°C) | 12.9 (1.3) | 12.8 (1.2) | 0.004* |
| Highest temperature for 365 days (°C) | 18.1 (1.1) | 18.0 (1.1) | 0.009* |
| Lowest temperature for 365 days (°C) | 8.4 (1.8) | 8.3 (1.7) | 0.009* |
| Relative humidity for 365 days (%) | 65.7 (4.5) | 65.9 (4.5) | 0.020* |
| Ambient atmospheric pressure for 365 days (hPa) | 1005.7 (4.6) | 1005.8 (4.5) | 0.435 |
| SO2 for 365 days (ppb) | 5.6 (1.1) | 5.5 (1.2) | 0.004* |
| NO2 for 365 days (ppb) | 23.3 (6.5) | 23.7 (6.7) | 0.021* |
| O3 for 365 days (ppb) | 23.7 (3.7) | 23.3 (3.7) | < 0.001* |
| CO for 365 days (ppb) | 567.0 (110.2) | 570.4 (105.2) | 0.201 |
| PM10 for 365 days (μg/m3) | 52.3 (7.2) | 52.2 (7.2) | 0.713 |
IHD ischemic heart disease, BMI body mass index (kg/m2), ppb parts per billion, ppm part per million (= 1000 ppb), SD standard deviation.
*Chi-square test or independent t-test. Significance at P < 0.05.
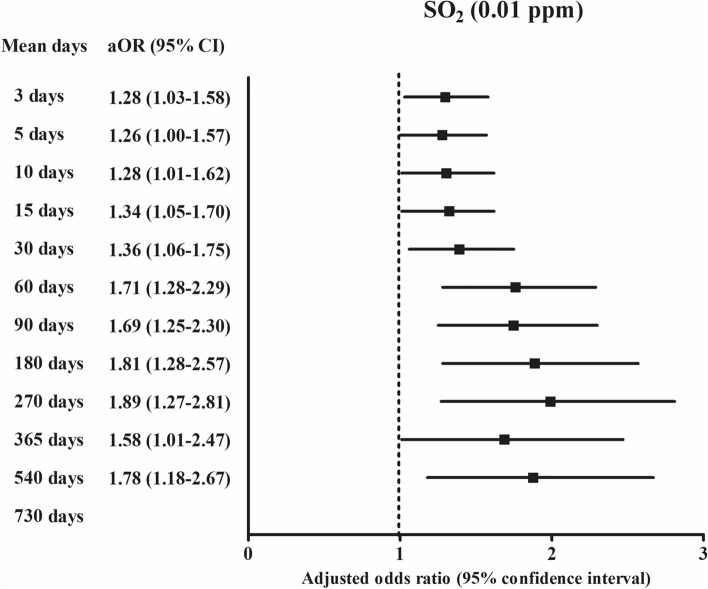
For 30 days of exposure, the OR was 1.36 (95% CI 1.06–1.75, Fig. 2) for SO2 (0.01 ppm) in the ischemic heart disease group compared with the control group using the final model (Table 2).
Figure 2.
The odds ratios (95% confidence interval) of SO2 (0.01 ppm) for 3 days, 5 days, 10 days, 15 days, 30 days, 60 days, 90 days, 180 days, 270 days, 365 days, and 540 days for ischemic heart disease.
Table 2.
Crude and adjusted odd ratios (95% confidence interval) of the meteorological and pollution matter (mean of 30 days before the index date) for ischemic heart disease.
| Characteristics | Odds ratio for ischemic heart disease (95% CI) | |||||
|---|---|---|---|---|---|---|
| Crudea | P-value | Adjusteda,b | P-value | Finala,c | P-value | |
| Mean temperature for 30 days (°C) | 1.00 (1.00–1.01) | 0.864 | 0.90 (0.65–1.24) | 0.506 | ||
| Highest temperature for 30 days (°C) | 1.00 (1.00–1.01) | 0.935 | 1.04 (0.89–1.21) | 0.660 | ||
| Lowest temperature for 30 days (°C) | 1.00 (1.00–1.01) | 0.798 | 1.09 (0.92–1.29) | 0.334 | ||
| Relative humidity for 30 days (%) | 1.00 (0.99–1.00) | 0.271 | 0.99 (0.98–1.00) | 0.045* | ||
| Ambient atmospheric pressure for 30 days (hPa) | 1.00 (0.99–1.01) | 0.697 | 1.00 (0.99–1.01) | 0.923 | ||
| SO2 for 30 days (0.01 ppm) | 1.36 (1.07–1.75) | 0.014* | 1.74 (1.18–2.56) | 0.005* | 1.36 (1.06–1.75) | 0.015* |
| NO2 for 30 days (0.1 ppm) | 0.59 (0.31–1.11) | 0.099 | 0.40 (0.15–1.07) | 0.066 | ||
| O3 for 30 days (0.01 ppm) | 1.04 (0.98–1.10) | 0.227 | 0.98 (0.89–1.09) | 0.727 | ||
| CO for 30 days (ppm) | 1.01 (0.77–1.32) | 0.939 | 1.02 (0.61–1.73) | 0.935 | ||
| PM10 for 30 days (10 μg/m3) | 1.00 (0.97–1.04) | 0.859 | 1.01 (0.96–1.07) | 0.593 | ||
*Conditional logistic regression model, Significance at P < 0.05.
aStratified model for age, sex, income, and region of residence.
bAdjusted model was adjusted for obesity, smoking status (current smoker compared to nonsmoker or past smoker), frequency of alcohol consumption (≥ 1 time a week compared to < 1 time a week), CCI score, mean temperature, highest temperature, lowest temperature, relative humidity, atmospheric pressure, SO2, NO2, O3, CO, and PM10.
cFinal model was adjusted for obesity, smoking status (current smoker compared to nonsmoker or past smoker), frequency of alcohol consumption (≥ 1 time a week compared to < 1 time a week), CCI score, relative humidity, SO2, NO2, O3, CO, and PM10 using the backward selection method.
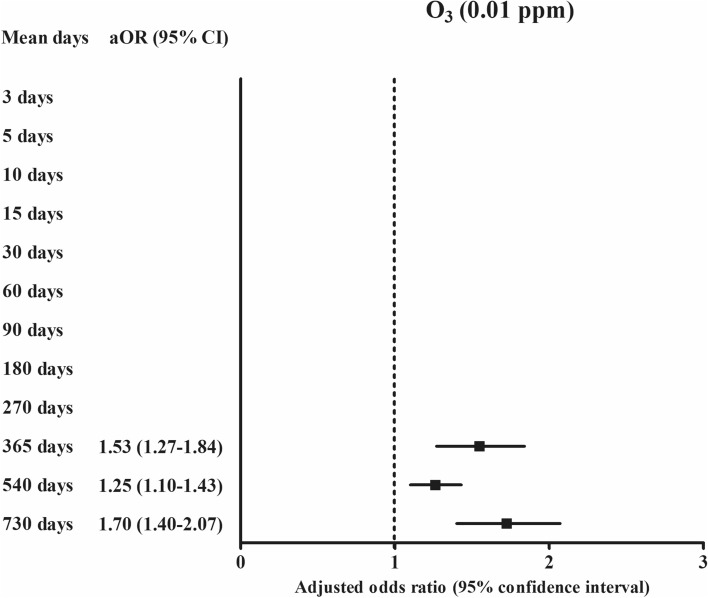
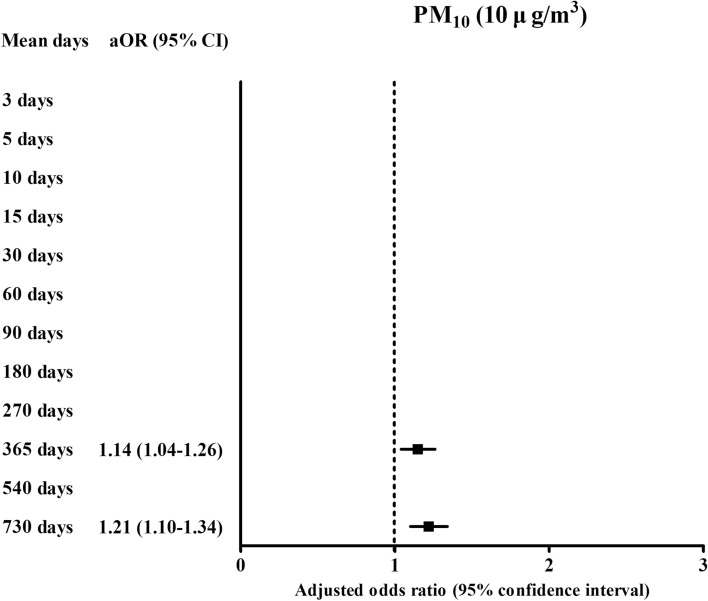
For one-year exposure, the ORs were 0.98 (95% CI 0.96–0.99) for relative humidity (%), 1.58 (95% CI 1.01–2.47, Fig. 2) for SO2 (0.01 ppm), 1.53 (95% CI 1.27–1.84, Fig. 3) for O3 (0.01 ppm), and 1.14 (95% CI 1.02–1.26, Fig. 4) for PM10 (10 μg/m3) in the ischemic heart disease group compared with the control group using the final model (Table 3).
Figure 3.
The odds ratios (95% confidence interval) of O3 (0.01 ppm) for 365 days, 540 days, and 730 days for ischemic heart disease.
Figure 4.
The odds ratios (95% confidence interval) of PM10 (10 μg/m3) for 365 days and 730 days for ischemic heart disease.
Table 3.
Crude and adjusted odd ratios (95% confidence interval) of the meteorological and pollution matter (mean of 365 days before the index date) for ischemic heart disease.
| Characteristics | Odds ratio for ischemic heart disease (95% CI) | |||||
|---|---|---|---|---|---|---|
| Crudea | P-value | Adjusteda,b | P-value | Finala,c | P-value | |
| Mean temperature for 365 days (°C) | 1.07 (1.03–1.12) | 0.001* | 0.89 (0.40–1.96) | 0.768 | ||
| Highest temperature for 365 days (°C) | 1.06 (1.02–1.11) | 0.009* | 1.00 (0.70–1.43) | 0.989 | ||
| Lowest temperature for 365 days (°C) | 1.06 (1.02–1.10) | 0.001* | 1.09 (0.72–1.66) | 0.689 | ||
| Relative humidity for 365 days (%) | 0.98 (0.96–0.99) | 0.002* | 0.97 (0.95–0.99) | 0.001* | 0.98 (0.96–0.99) | 0.002* |
| Ambient atmospheric pressure for 365 days (hPa) | 1.00 (0.99–1.01) | 0.413 | 1.01 (0.99–1.02) | 0.516 | ||
| SO2 for 365 days (0.01 ppm) | 1.84 (1.22–2.77) | 0.004* | 1.88 (1.12–3.18) | 0.017* | 1.58 (1.01–2.47) | 0.045* |
| NO2 for 365 days (0.1 ppm) | 0.35 (0.16–0.79) | 0.011* | 0.18 (0.04–0.90) | 0.037* | ||
| O3 for 365 days (0.01 ppm) | 1.31 (1.15–1.50) | < 0.001* | 1.27 (0.98–1.64) | 0.070 | 1.53 (1.27–1.84) | < 0.001* |
| CO for 365 days (ppm) | 0.73 (0.46–1.15) | 0.174 | 0.81 (0.38–1.70) | 0.569 | ||
| PM10 for 365 days (10 μg/m3) | 1.01 (0.95–1.09) | 0.701 | 1.19 (1.12–3.18) | 0.001* | 1.14 (1.04–1.26) | 0.007* |
*Conditional logistic regression model, Significance at P < 0.05.
aStratified model for age, sex, income, and region of residence.
bAdjusted model was adjusted for obesity, smoking status (current smoker compared to nonsmoker or past smoker), frequency of alcohol consumption (≥ 1 time a week compared to < 1 time a week), CCI score, mean temperature, highest temperature, lowest temperature, relative humidity, atmospheric pressure, SO2, NO2, O3, CO, and PM10.
cFinal model was adjusted for obesity, smoking status (current smoker compared to nonsmoker or past smoker), frequency of alcohol consumption (≥ 1 time a week compared to < 1 time a week), CCI score, relative humidity, SO2, NO2, O3, CO, and PM10 using the backward selection method.
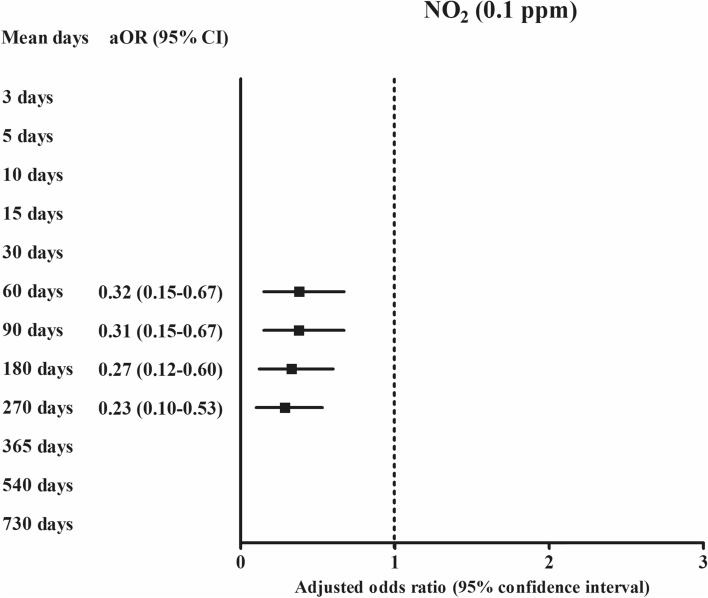
According to the duration of exposures, the exposure of SO2 (0.01 ppm) was positively related with ischemic heart disease in 3 days, 5 days, 10 days, 15 days, 30 days, 60 days, 90 days, 180 days, 270 days, 365 days, and 540 days of exposure (Fig. 2 and Supplementary Table S1). For PM10 (10 μg/m3), 365 days and 730 days of PM10 (10 μg/m3) exposure were positively related with ischemic heart disease (Fig. 4). For O3 (0.01 ppm), 365 days, 540 days, and 730 days of O3 (0.01 ppm) exposure were positively related with ischemic heart disease (Fig. 3). The exposure of NO2 (0.1 ppm) for 60 days, 90 days, 180 days, and 270 days was negatively related with ischemic heart disease (Fig. 5).
Figure 5.
The odds ratios (95% confidence interval) of NO2 (0.1 ppm) for 60 days, 90 days, 180 days, and 270 days for ischemic heart disease.
In the subgroup analyses using the final model, in the age groups < 60 years old and ≥ 60 years old, the odds for O3 and PM10 were higher in ischemic heart disease participants than in the control group after 1 year of exposure. In the age ≥ 60 years group, the odds for SO2 were higher in ischemic heart disease participants than in the control group after 30 days and one year of exposure. In men, individuals with low income, and urban groups, the odds for SO2 for 30 days of exposure and odds for O3 and PM10 for one year of exposure were higher in ischemic heart disease patients than in the control group. In the high-income and rural groups, the odds for SO2 for one year of exposure were higher in ischemic heart disease patients than in the control group (Table 4).
Table 4.
Adjusted odd ratios (95% confidence interval) of the meteorological and pollution matter for ischemic heart disease according to age and sex in the final model.
| Characteristics | Means of 30 days | Means of 365 days | ||
|---|---|---|---|---|
| Odd ratios (95% CI) | P-value | Odd ratios (95% CI) | P-value | |
| Age < 60 years old (n = 1820) | ||||
| O3 (0.01 ppm) | 2.21 (1.46–3.34) | < 0.001* | ||
| PM10 (10 μg/m3) | 1.28 (1.03–1.60) | 0.027* | ||
| Age ≥ 60 years old (n = 8955) | ||||
| SO2 (0.01 ppm) | 1.37 (1.04–1.79) | 0.025* | 1.67 (1.02–2.72) | 0.042* |
| Relative humidity (%) | 0.97 (0.96–0.99) | 0.001* | ||
| O3 (0.01 ppm) | 1.42 (1.16–1.75) | 0.001* | ||
| PM10 (10 μg/m3) | 1.12 (1.01–1.25) | 0.032* | ||
| Men (n = 7235) | ||||
| SO2 (0.01 ppm) | 1.45 (1.07–1.96) | 0.016* | ||
| O3 (0.01 ppm) | 1.54 (1.24–1.92) | < 0.001* | ||
| PM10 (10 μg/m3) | 1.19 (1.06–1.32) | 0.003* | ||
| Women (n = 3540) | ||||
| Relative humidity (%) | 0.95 (0.93–0.98) | < 0.001* | ||
| NO2 (0.1 ppm) | 0.09 (0.02–0.39) | 0.002* | ||
| Low income (n = 5435) | ||||
| SO2 (0.01 ppm) | 1.43 (1.00–2.04) | 0.050* | ||
| O3 (0.01 ppm) | 1.69 (1.32–2.18) | < 0.001* | ||
| PM10 (10 μg/m3) | 1.25 (1.10–1.41) | 0.001* | ||
| High income (n = 5340) | ||||
| Relative humidity (%) | 0.97 (0.95–0.99) | 0.001* | ||
| SO2 (0.01 ppm) | 2.09 (1.13–3.88) | 0.019* | ||
| NO2 (0.1 ppm) | 0.22 (0.07–0.69) | 0.010* | ||
| Urban (n = 4155) | ||||
| SO2 (0.01 ppm) | 1.62 (1.05–2.49) | 0.028* | ||
| Relative humidity (%) | 0.98 (0.96–0.99) | 0.009* | ||
| O3 (0.01 ppm) | 2.08 (1.60–2.70) | < 0.001* | ||
| PM10 (10 μg/m3) | 1.39 (1.21–1.60) | < 0.001* | ||
| Rural (n = 6620) | ||||
| Relative humidity (%) | 0.97 (0.95–0.99) | 0.008* | ||
| SO2 (0.01 ppm) | 1.71 (1.00–2.93) | 0.050* | ||
*Conditional logistic regression model; Significance at P < 0.05.
aStratified model for age, sex, income, and region of residence.
bFinal model was adjusted for obesity, smoking status (current smoker compared to nonsmoker or past smoker), frequency of alcohol consumption (≥ 1 time a week compared to < 1 time a week), CCI score, relative humidity, SO2, NO2, O3, CO, and PM10 using the backward selection method.
Discussion
Both short-term and long-term exposure to air pollutants were related to ischemic heart disease in the present study. The types of air pollutants that impacted ischemic heart disease differed according to exposure period. Short-term (30 days) exposure to SO2 was related to higher odds of ischemic heart disease. For long-term (365 days) exposure, higher levels of SO2, O3, and PM10 were associated with ischemic heart disease. In addition, the effects of air pollutants on ischemic heart disease were different according to the demographic factors of age and sex and the socioeconomic factors of income level and region of residence.
Short-term exposure to SO2 was associated with higher odds of ischemic heart disease in this study. In line with the present results, previous studies have reported elevated mortality related to short-term exposure to SO218,29. Although some prior studies demonstrated an association between exposure to PM10, SO2, and NO2 with the disease burden of ischemic heart disease (years of life lost), one time-series study reported that SO2, but not other air pollutants or PMs, was related to the increased mortality of ischemic heart disease (excess risk of death = 3.18%, 95% CI 1.19–5.17)18. They found that gaseous pollutants, such as SO2, had higher impacts on the risk of ischemic heart disease than PMs18. Oxidative stress and the inflammatory response have been suggested as possible pathophysiologic mechanisms for the impact of SO2 on ischemic heart disease30. Sulfate exposure for 2–7 days was associated with oxidative stress markers of urinary creatinine-indexed 8-epi-prostaglandin F2α in the Framingham heart study30.
Short-term exposure to other air pollutants, including NO2 and PM10, did not show an association with ischemic heart disease in the present study. Previous epidemiologic studies have suggested that the source or components of PMs are crucial for their hazardous impact on ischemic heart disease11. The PM2.5 from wind-blown soil or biomass combustion was not associated with ischemic heart mortality11. The present study could not differentiate the sources of PM10 because its heterogeneous composition could attenuate its adverse impacts on ischemic heart disease.
Long-term exposure to SO2, O3, and PM10 was related to higher odds of ischemic heart disease in this study. A large amount of previous epidemiologic data supports the long-term effects of air pollutants on the risk of ischemic heart disease31,32. The mortality of ischemic heart disease was 1.03-fold higher in patients who were exposed to a high level of PM2.5 in the form of diesel traffic-related elemental carbon (95% CI 1.00–1.06) from 2000 to 2005 in the US11. Multiple pathophysiologic mechanisms, including the systemic inflammatory response, prothrombotic pathway activation, oxidative stress, vascular dysfunction and remodeling, autonomic dysfunction, and epigenetic factors, have been proposed to mediate the impact of air pollutants on ischemic heart disease12. For instance, coronary artery calcification was proposed as one of the pathophysiologic mechanisms for the effect of air pollutants, including PMs and O3, on the risk of ischemic heart disease24,33. The coronary artery calcium score, which is considered an atherosclerotic marker, was associated with elevated levels of PM2.5 (27.2%, 95% CI 10.8–46.1%)31. Although the pathophysiologic mechanism of the effect of O3 on ischemic heart disease remains elusive, oxidizing activities could induce inflammation in the coronary artery, which might result in atherosclerotic plaque formation and narrowing of the arterial lumen with increasing wall thickness32. To support this hypothesis, it was reported that long-term exposure to O3 was related to increased thickness of the common carotid artery (5.6 µm, 95% CI 1.4–9.7) and carotid plaque burden (OR 1.2, 95% CI 1.1–1.4)32.
The relative humidity for one year was negatively associated with ischemic heart disease in this study. Previous studies have suggested the contributions of meteorological factors of temperature variability with the risk of ischemic heart disease, although no prior research investigated the association of humidity with ischemic heart disease34,35. The potential impact of humidity on the solubility of gaseous pollutants and moisture content, which may decrease the amount of air pollutant exposure, could mediate the decreased rate of ischemic heart disease in high humidity conditions.
The impacts of air pollutants were prominent in the old age group and men in this study. Previous studies have also suggested the higher susceptibility of older populations and men to the impacts of air pollutants on ischemic heart disease18,31. Preformed or subclinical atherosclerotic changes of the coronary artery could more easily progress due to the impacts of air pollutants on inflammation and atherosclerosis, although the synergistic or additive effects of air pollutants could not be determined in the current study. The high prevalence of ischemic heart disease in men compared to that in women could strengthen the statistical power in this population. In addition, populations with poor socioeconomic status showed a relationship between short-term exposure to SO2 and ischemic heart disease in this study. Several previous studies investigated socioeconomic disparities and the impact of a higher burden of air pollution on morbidities and mortalities in minorities, although the results had some heterogeneity according to the air pollution models36,37. Populations with poor socioeconomic status have been reported to be exposed to more air pollution because of the lack of availability of air conditioning and increased industrial exposure38–41. In addition to high exposure to air pollution, poor socioeconomic groups were reported to have increased susceptibility to air pollution due to underlying health statuses and reduced access to medical care38. The association of short-term exposure to SO2 and ischemic heart disease in the urban subgroup might be attributed to the higher level of air pollution in urban areas than in rural areas.
The analysis of a large, representative national cohort population strengthened the statistical power of the present study. The large study population enabled the selection of a control population that was matched for age, sex, income, and region of residence. Possible confounders were comprehensively considered in this study. In addition to past medical histories, lifestyle factors of smoking, alcohol consumption, and obesity were adjusted. Moreover, meteorological factors were concurrently considered along with air pollutants. The meteorological factors and air pollution data were collected and validated by the Korea Meteorological Administration. Based on these verified data, this study investigated both the short-term and long-term effects of air pollution on ischemic heart disease. However, a few limitations existed in the current study. Possible collinearity between air pollutants might exist, although we adjusted for these variables in the final models (Supplementary Tables S14–S15). The level of exposure to PM2.5 was not available in this cohort. Because the exposure to air pollutants was based on the registered region of residence, the migration of participants during follow-up periods could not be accounted for in the present study. In addition, indoor exposure to air pollutants could not be individually assessed. For the diagnosis of ischemic heart disease, we could not differentiate the types or severity of disease because this study was based on health claims data. Last, because this study was based on Koreans, ethnic differences should be considered when interpreting this study.
Conclusions
Short-term exposure to SO2 and long-term exposure to SO2, O3, and PM10 were associated with an increased risk of ischemic heart disease. The older, male, low-income, and urban groups demonstrated an apparent association between short-term exposure to SO2 and ischemic heart disease.
Supplementary Information
Acknowledgements
The manuscript was edited for proper English language, grammar, punctuation, spelling, and overall style by the highly qualified native English-speaking editors at American Journal Experts (EF94-7264-5CEE-C547-665P).
Author contributions
H.G.C. designed the study; J.H.W., C.M., and H.G.C. analyzed the data; S.Y.K., S.H.K., S.M.H., S.K., and H.G.C. drafted and revised the paper; and all authors approved the final version of the manuscript.
Funding
This work was supported in part by a research Grant (NRF-2018-R1D1A1A02085328 and 2020R1A2C4002594) from the National Research Foundation (NRF) of Korea.
Data availability
Releasing of the data by the researcher is not allowed legally. All data are available from the database of the National health Insurance Sharing Service (NHISS; https://nhiss.nhis.or.kr/). NHISS allows data access, at a particular cost, for any researcher who promises to follow the research ethics. Data of this article can be downloaded from the website after promising to follow the research ethics.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-84587-x.
References
- 1.Dalen JE, Alpert JS, Goldberg RJ, Weinstein RS. The epidemic of the 20(th) century: Coronary heart disease. Am. J. Med. 2014;127:807–812. doi: 10.1016/j.amjmed.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 2.DALYs, G. B. D. & Collaborators, H. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet392, 1859–1922, 10.1016/S0140-6736(18)32335-3 (2018). [DOI] [PMC free article] [PubMed]
- 3.Benjamin EJ, et al. Heart disease and stroke statistics-2018 update: A report from the American Heart Association. Circulation. 2018;137:e67–e492. doi: 10.1161/CIR.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 4.McEvoy JW, et al. Coronary artery calcium progression: An important clinical measurement? A review of published reports. J. Am. Coll. Cardiol. 2010;56:1613–1622. doi: 10.1016/j.jacc.2010.06.038. [DOI] [PubMed] [Google Scholar]
- 5.Gargiulo P, et al. Ischemic heart disease in systemic inflammatory diseases. An appraisal. Int. J. Cardiol. 2014;170:286–290. doi: 10.1016/j.ijcard.2013.11.048. [DOI] [PubMed] [Google Scholar]
- 6.Mandviwala T, Khalid U, Deswal A. Obesity and cardiovascular disease: A risk factor or a risk marker? Curr. Atheroscler. Rep. 2016;18:21. doi: 10.1007/s11883-016-0575-4. [DOI] [PubMed] [Google Scholar]
- 7.Roerecke M, et al. Heavy drinking occasions in relation to ischaemic heart disease mortality—An 11–22 year follow-up of the 1984 and 1995 US National Alcohol Surveys. Int. J. Epidemiol. 2011;40:1401–1410. doi: 10.1093/ije/dyr129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ambrose JA, Barua RS. The pathophysiology of cigarette smoking and cardiovascular disease: An update. J. Am. Coll. Cardiol. 2004;43:1731–1737. doi: 10.1016/j.jacc.2003.12.047. [DOI] [PubMed] [Google Scholar]
- 9.Dalton TP, et al. Dioxin exposure is an environmental risk factor for ischemic heart disease. Cardiovasc. Toxicol. 2001;1:285–298. doi: 10.1385/ct:1:4:285. [DOI] [PubMed] [Google Scholar]
- 10.Pope CA, 3rd, et al. Ischemic heart disease events triggered by short-term exposure to fine particulate air pollution. Circulation. 2006;114:2443–2448. doi: 10.1161/CIRCULATIONAHA.106.636977. [DOI] [PubMed] [Google Scholar]
- 11.Thurston GD, et al. Ischemic heart disease mortality and long-term exposure to source-related components of U.S. fine particle air pollution. Environ. Health Perspect. 2016;124:785–794. doi: 10.1289/ehp.1509777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Combes A, Franchineau G. Fine particle environmental pollution and cardiovascular diseases. Metabolism. 2019;100S:153944. doi: 10.1016/j.metabol.2019.07.008. [DOI] [PubMed] [Google Scholar]
- 13.Lu Y, et al. Assessing the association between fine particulate matter (PM2.5) constituents and cardiovascular diseases in a mega-city of Pakistan. Environ. Pollut. 2019;252:1412–1422. doi: 10.1016/j.envpol.2019.06.078. [DOI] [PubMed] [Google Scholar]
- 14.Zhang W, et al. Triggering of cardiovascular hospital admissions by fine particle concentrations in New York state: Before, during, and after implementation of multiple environmental policies and a recession. Environ. Pollut. 2018;242:1404–1416. doi: 10.1016/j.envpol.2018.08.030. [DOI] [PubMed] [Google Scholar]
- 15.Shamsipour M, et al. National and sub-national exposure to ambient fine particulate matter (PM2.5) and its attributable burden of disease in Iran from 1990 to 2016. Environ. Pollut. 2019;255:113173. doi: 10.1016/j.envpol.2019.113173. [DOI] [PubMed] [Google Scholar]
- 16.Li J, et al. Estimation of PM2.5 mortality burden in China with new exposure estimation and local concentration-response function. Environ. Pollut. 2018;243:1710–1718. doi: 10.1016/j.envpol.2018.09.089. [DOI] [PubMed] [Google Scholar]
- 17.Ljungman PLS, et al. Long-term exposure to particulate air pollution, black carbon, and their source components in relation to ischemic heart disease and stroke. Environ. Health Perspect. 2019;127:107012. doi: 10.1289/EHP4757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang J, et al. The burden of ischemic heart disease related to ambient air pollution exposure in a coastal city in South China. Environ. Res. 2018;164:255–261. doi: 10.1016/j.envres.2018.02.033. [DOI] [PubMed] [Google Scholar]
- 19.Sun Z, Chen C, Xu D, Li T. Effects of ambient temperature on myocardial infarction: A systematic review and meta-analysis. Environ. Pollut. 2018;241:1106–1114. doi: 10.1016/j.envpol.2018.06.045. [DOI] [PubMed] [Google Scholar]
- 20.Choi HG, Min C, Kim SY. Air pollution increases the risk of SSNHL: A nested case-control study using meteorological data and national sample cohort data. Sci. Rep. 2019;9:8270. doi: 10.1038/s41598-019-44618-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim SY, Min C, Oh DJ, Choi HG. Tobacco smoking and alcohol consumption are related to benign parotid tumor: A nested case-control study using a national health screening cohort. Clin. Exp. Otorhinolaryngol. 2019;12:412–419. doi: 10.21053/ceo.2018.01774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim SY, Kong IG, Min C, Choi HG. Association of air pollution with increased risk of peritonsillar abscess formation. JAMA Otolaryngol. Head Neck Surg. 2019;145:530–535. doi: 10.1001/jamaoto.2019.0742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Team, K. A. M. Air Korea.
- 24.Choi S, et al. Association of obesity or weight change with coronary heart disease among young adults in South Korea. JAMA Intern. Med. 2018;178:1060–1068. doi: 10.1001/jamainternmed.2018.2310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim SY, Min C, Oh DJ, Choi HG. Bidirectional association between GERD and asthma: Two longitudinal follow-up studies using a national sample cohort. J. Allergy Clin. Immunol. Pract. 2020;8:1005–1013. doi: 10.1016/j.jaip.2019.10.043. [DOI] [PubMed] [Google Scholar]
- 26.Kim SY, Oh DJ, Park B, Choi HG. Bell's palsy and obesity, alcohol consumption and smoking: A nested case-control study using a national health screening cohort. Sci. Rep. 2020;10:4248. doi: 10.1038/s41598-020-61240-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Quan H, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 2011;173:676–682. doi: 10.1093/aje/kwq433. [DOI] [PubMed] [Google Scholar]
- 28.Quan H, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 29.Li G, Zeng Q, Pan X. Disease burden of ischaemic heart disease from short-term outdoor air pollution exposure in Tianjin, 2002–2006. Eur. J. Prev. Cardiol. 2016;23:1774–1782. doi: 10.1177/2047487316651352. [DOI] [PubMed] [Google Scholar]
- 30.Li W, et al. Short-term exposure to air pollution and biomarkers of oxidative stress: The Framingham Heart Study. J. Am. Heart Assoc. 2016 doi: 10.1161/JAHA.115.002742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang M, et al. Association of estimated long-term exposure to air pollution and traffic proximity with a marker for coronary atherosclerosis in a nationwide study in China. JAMA Netw. Open. 2019;2:e196553. doi: 10.1001/jamanetworkopen.2019.6553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang M, et al. Long-term exposure to ambient ozone and progression of subclinical arterial disease: The multi-ethnic study of atherosclerosis and air pollution. Environ. Health Perspect. 2019;127:57001. doi: 10.1289/EHP3325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kaufman JD, et al. Association between air pollution and coronary artery calcification within six metropolitan areas in the USA (the Multi-Ethnic Study of Atherosclerosis and Air Pollution): A longitudinal cohort study. Lancet. 2016;388:696–704. doi: 10.1016/S0140-6736(16)00378-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tian Y, et al. Association between temperature variability and daily hospital admissions for cause-specific cardiovascular disease in urban China: A national time-series study. PLoS Med. 2019;16:e1002738. doi: 10.1371/journal.pmed.1002738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schwartz J, Samet JM, Patz JA. Hospital admissions for heart disease: The effects of temperature and humidity. Epidemiology. 2004;15:755–761. doi: 10.1097/01.ede.0000134875.15919.0f. [DOI] [PubMed] [Google Scholar]
- 36.Loizeau M, et al. Does the air pollution model influence the evidence of socio-economic disparities in exposure and susceptibility? Environ. Res. 2018;167:650–661. doi: 10.1016/j.envres.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 37.Fairburn J, Schule SA, Dreger S, Karla Hilz L, Bolte G. Social inequalities in exposure to ambient air pollution: A systematic review in the WHO European Region. Int. J. Environ. Res. Public Health. 2019 doi: 10.3390/ijerph16173127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lipfert FW. Air pollution and poverty: Does the sword cut both ways? J. Epidemiol. Community Health. 2004;58:2–3. doi: 10.1136/jech.58.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Soleas GJ, Diamandis EP, Goldberg DM. Resveratrol: A molecule whose time has come? And gone? Clin. Biochem. 1997;30:91–113. doi: 10.1016/s0009-9120(96)00155-5. [DOI] [PubMed] [Google Scholar]
- 40.Renaud S, de Lorgeril M. Wine, alcohol, platelets, and the French paradox for coronary heart disease. Lancet. 1992;339:1523–1526. doi: 10.1016/0140-6736(92)91277-f. [DOI] [PubMed] [Google Scholar]
- 41.Bonnefont-Rousselot D. Resveratrol and cardiovascular diseases. Nutrients. 2016 doi: 10.3390/nu8050250. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Releasing of the data by the researcher is not allowed legally. All data are available from the database of the National health Insurance Sharing Service (NHISS; https://nhiss.nhis.or.kr/). NHISS allows data access, at a particular cost, for any researcher who promises to follow the research ethics. Data of this article can be downloaded from the website after promising to follow the research ethics.