Abstract
INTRODUCTION
Migrant workers comprise about one-fifth of Singapore’s resident population and form a substantial and vital component of the nation’s workforce. However, limited data is available regarding the barriers that migrant workers face in accessing healthcare from the healthcare providers’ perspective.
METHODS
We conducted a survey on doctors working in four restructured hospitals in Singapore, to assess what they perceived to be barriers faced by migrant workers in accessing healthcare. We also assessed the doctors’ understanding of migrant-health-related policies in Singapore.
RESULTS
A total of 427 survey responses were collected. Most respondents were senior doctors (senior residents or consultants) who had been practising medicine for a median of ten years. Among doctors, the most common perceived barriers to migrant workers accessing healthcare were related to culture/language (92.3%) and finances (healthcare cost) (81.0%). Of the six questions asked pertaining to migrant healthcare policy in Singapore, the respondents achieved a median of four correctly answered questions (interquartile range 3–5), and about 55% were unaware or unsure of available resources for migrant workers.
CONCLUSION
Our study identified healthcare providers’ perceived barriers to the delivery of healthcare to migrant workers, which corroborate previously published data reported by migrant workers themselves. Further efforts should be directed towards diminishing these barriers and increasing the literacy of migrant health among healthcare workers.
Keywords: barriers, doctors, healthcare, migrant workers, Singapore
INTRODUCTION
Low-wage migrant workers in Singapore make up a large proportion of our population. As of December 2016, there were 1.15 million foreign workers holding either a Work Permit (workers in construction, manufacturing, marine/shipyard, process or service industries) or an S Pass (mid-level skilled workers).(1) This was approximately one-fifth of Singapore’s population of 5.5 million people.(2)
However, migrant workers are not entitled to the healthcare subsidies provided by the Singapore government, and do not qualify for the financing schemes available to Singaporeans and permanent residents.(3) Currently, under the Employment of Foreign Manpower Act, employers of low-wage migrant domestic and non-domestic workers are mandated by law to provide medical insurance coverage of at least SGD 15,000 a year for inpatient fees and day surgeries.(4) In addition, employers of migrant workers holding a Work Permit or S Pass are required legally to bear the costs of the provision of adequate medical treatment.(4) Technically, this should include outpatient care, and employers are expected to bear the costs when expenses are in excess of insurance coverage for inpatient care. Co-payment by the migrant worker may be permissible if certain conditions are met: medical treatment is not for work-related injuries; the co-pay amount is reasonable and does not exceed 10% of the worker’s monthly salary; duration of co-payment does not exceed six months; and the co-payment option is explicitly in the employment contract or collective agreement and has the worker’s full consent.(4,5) Healthcare costs due to injuries sustained during work are covered under the Work Injury Compensation Act (WICA), which mandates employers to purchase work injury compensation insurance for workers doing manual work (regardless of salary level) and for workers doing non-manual work with a salary of SGD 1,600 or less, with a minimum medical expenses coverage of SGD 36,000 a year.(6)
Despite the above policies, our recent survey of non-domestic migrant workers suggests that significant gaps still remain, resulting in significant barriers to accessing healthcare for migrant workers; furthermore, many had poor knowledge regarding their healthcare coverage and had experienced financial barriers in accessing healthcare.(7) Migrant workers often bear the costs of, or face barriers in outpatient care; inpatient insurance coverage may also be easily breached in the face of catastrophic illness.(7) Our survey’s findings were similar to those of a study by Lee et al, which reported poor knowledge about health-related insurance among male migrant workers and a greater likelihood for lower-income workers to delay or avoid seeking medical attention due to financial concerns.(8) However, these studies surveyed migrant workers who were largely well, with few having encountered major medical illnesses or hospitalisations. There is limited data on the experience of low-wage migrant workers within the tertiary healthcare setting, and the challenges faced by those who require hospitalisation or specialist care. Some of the challenges faced by migrant workers in Singapore have been highlighted by several reports published in the media, most of which revolve around the topic of inadequate issuance of sick leave to migrant workers(9,10) or of workers avoiding care due to cost concerns.(11) In 2012, Johnraj et al used the case studies of two low-wage migrant workers who had suffered catastrophic work injuries to illustrate the inadequacies of the WICA.(11)
Given the current paucity of information, particularly from the physician’s perspective, regarding potential barriers to care that low-wage migrant workers may experience in Singapore, and to complement our data pertaining to such barriers from the worker’s perspective,(7) we conducted a survey of doctors working in the tertiary care setting in Singapore to assess these barriers and to better understand potential factors affecting the care of migrant workers. As doctors play a large role in acting as healthcare advocates for their patients, we also assessed their understanding of migrant-health related policies in Singapore.
METHODS
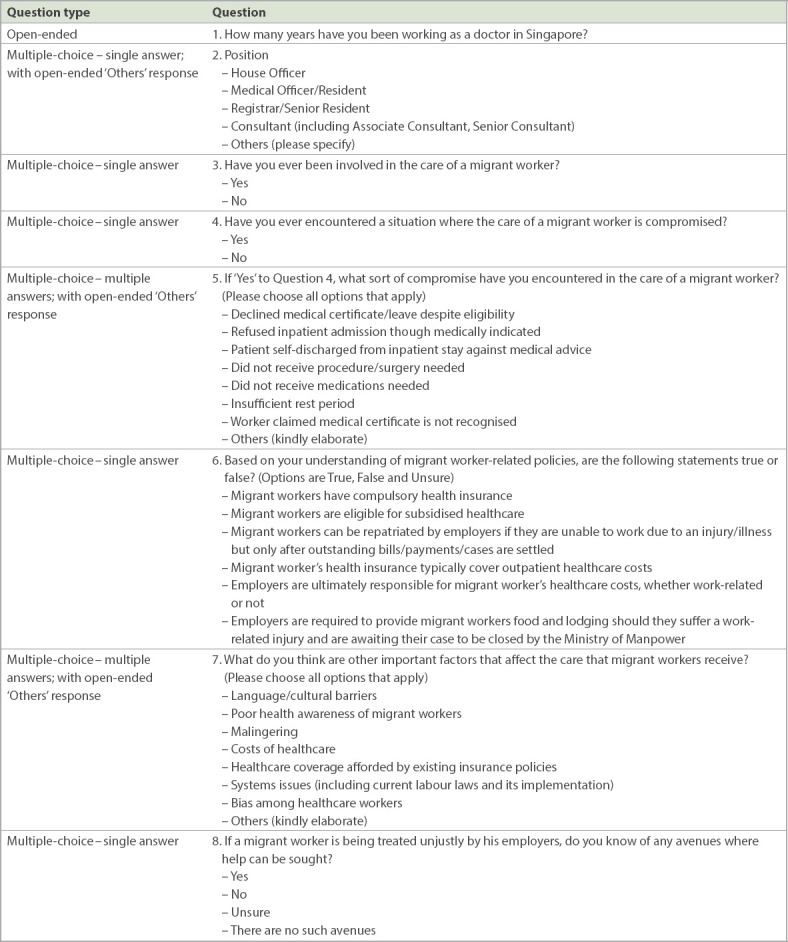
Survey questions (Table I) were designed to include brief information regarding each respondent’s working experience in Singapore, experience in treating migrant workers and knowledge of migrant health-related policies. The majority of questions were close-ended questions to encourage completion of the survey, with open-ended fields where respondents could provide additional responses.
Table I.
Online survey administered to doctors working in tertiary institutions in Singapore.
Questions were uploaded to an online survey site (www.surveymonkey.com) and a website link to the survey was generated. Approval was obtained from the Chairman of each tertiary hospital’s medical board before invitations to participate in the survey were sent via electronic mail to all the doctors working in the following hospitals: National University Hospital, Sengkang General Hospital, Singapore General Hospital and Tan Tock Seng Hospital. Responses were anonymous and no personal identifiers were collected. This study was approved by the National Healthcare Group’s Domain Specific Review Board (DSRB Reference Number: 2016/00499).
RESULTS
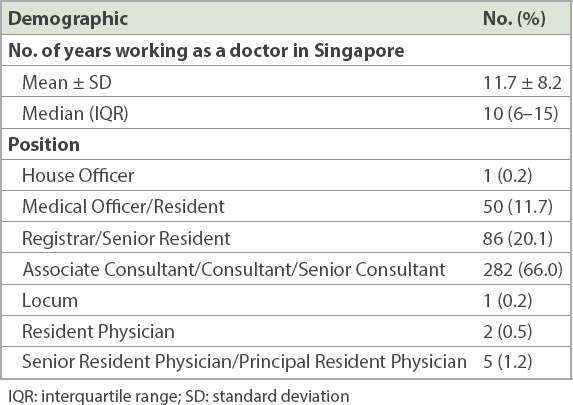
A total of 427 survey responses were collected between 18 August 2016 and 6 March 2017. The median number of years that respondents had worked as doctors in Singapore was 10 (interquartile range [IQR] 6 –15) years (Table II). A large number of respondents were senior doctors, with two-thirds holding the position of Associate Consultant, Consultant or Senior Consultant, and one-fifth holding the position of Registrar or Senior Resident.
Table II.
Demographics of respondents in online survey of Singapore doctors working in tertiary institutions (n = 427).
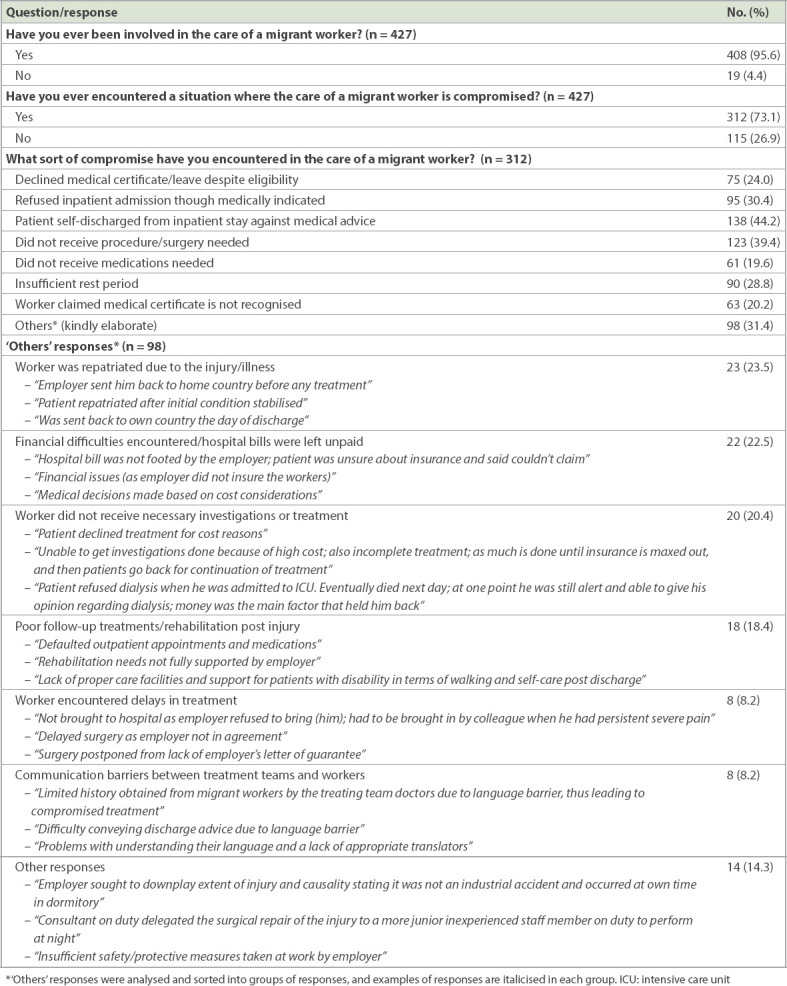
Almost all our respondents indicated that they had ever been involved in the care of migrant workers (n = 408, 95.6%; Table III). A large majority of doctors surveyed had encountered at least one situation in which the care of a migrant worker was compromised (n = 312, 73.1%). Of these, many had patients who self-discharged from inpatient stay against medical advice (n = 138, 44.2%), or did not receive procedures or surgeries that were indicated (n = 123, 39.4%). Other ways in which the care of migrant workers was compromised, in order of frequency reported, included: refusal of admission despite medical indications for it (30.4%); insufficient rest period, i.e. medical leave (28.8%); patients declining medical leave despite eligibility (24.0%); non-recognition of medical leave by employers (20.2%); and non-receipt of necessary medications (19.6%). Other free-text responses are also described in Table III.
Table III.
Experience with care of migrant workers among Singapore doctors working in tertiary institutions: results of online survey.
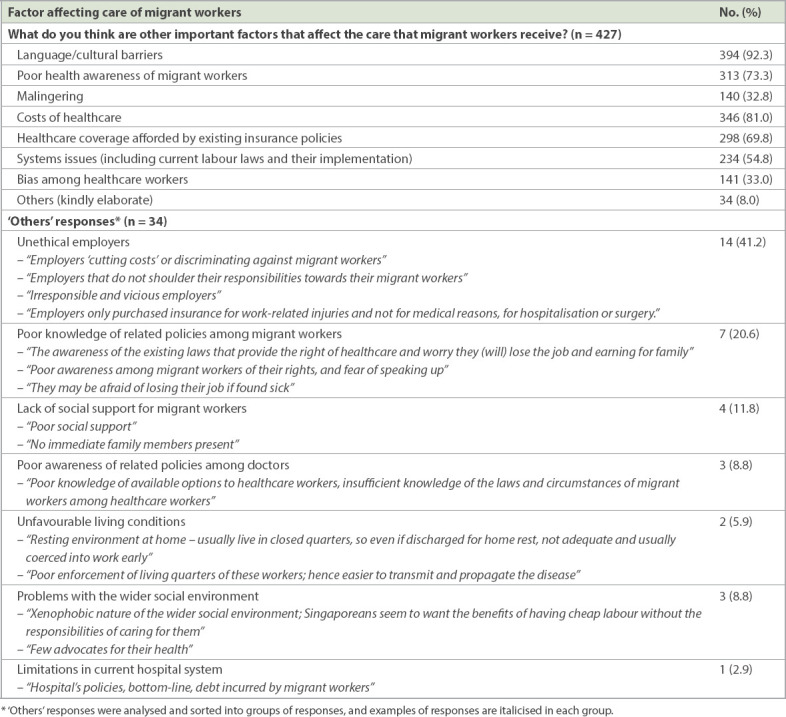
The most commonly highlighted factors that affected the care provided to migrant workers (Table IV) included language/cultural barriers (n = 394, 92.3%), costs of healthcare (n = 346, 81.0%), poor health awareness of migrant workers (n = 313, 73.3%), and healthcare coverage afforded by existing insurance policies (n = 298, 69.8%). Other factors affecting the care of migrants, in order of frequency, included: issues (e.g. current labour laws and their implementation) (54.8%), bias among healthcare workers (33.0%) and perceived malingering (32.8%). In addition, among the free-text responses received, employers that treated their workers unfairly and poor knowledge of related policies among migrant workers (n = 14 and n = 7, respectively) were the common themes.
Table IV.
Factors affecting care of migrant workers identified by Singapore doctors working in tertiary institutions: results of online survey.
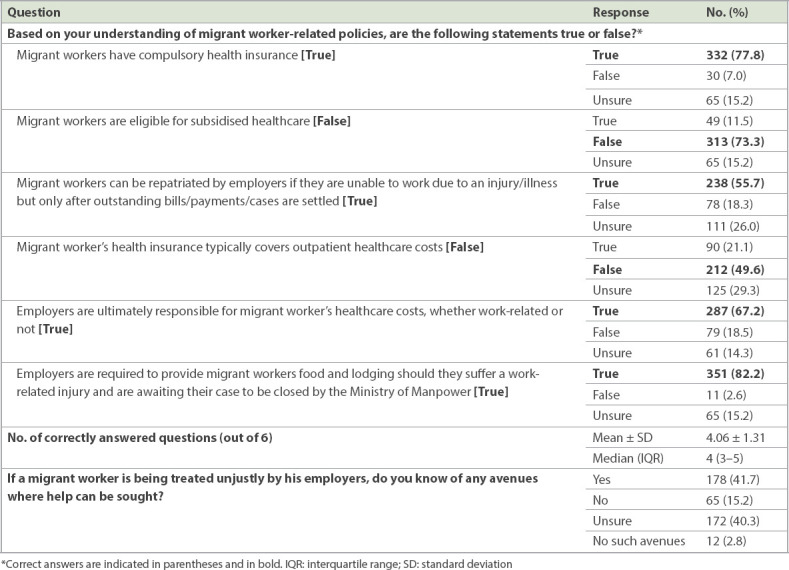
The percentage of doctors who selected correct responses for each of the six questions asked regarding migrant health policies (Table V) ranged from 49.6% to 82.2%. Only 77.8% of doctors were certain that migrant workers had compulsory health insurance, and a similar proportion (73.3%) knew that migrant workers were not eligible for subsidised health care. A significant proportion of respondents (21.1%) had the false impression that migrant workers’ insurance was able to cover outpatient costs, with only about half indicating that this was not true. In addition, one-third of doctors were either unsure about whether employers were eventually responsible for the healthcare costs of migrant workers, or thought that this was false. Under Singapore law, employers are indeed ultimately responsible for the cost of medical treatments for their migrant workers. Most doctors also did not know (15.2%) or were unsure (40.3%) of whether there were any avenues to seek help for migrant workers who were treated unfairly by their employers.
Table V.
Assessment of knowledge of migrant health policies among Singapore doctors working in tertiary institutions: results of online survey.
DISCUSSION
Migrants all over the world face various challenges as they transit and adapt to their receiving countries. Among these challenges are barriers to healthcare, which may be accentuated by cultural, language and socioeconomic factors, which may also vary depending on the healthcare policy and provisions in the receiving country. Singapore is a small city-state country that is highly dependent on migrant labour for its economic well-being. While official statistics on a per-country basis are not published by the Ministry of Manpower, the majority of migrant workers in Singapore hail from South India, Bangladesh and China.(7) While most migrant workers in Singapore are relatively young when they arrive,(7) migrant workers from these countries may stay in Singapore for up to 14–26 years,(12) and a substantial proportion of them go on to develop chronic diseases, such as hypertension and diabetes mellitus, and their attendant complications. Over the years, we have witnessed an increasing burden of chronic diseases at charity clinics serving these migrant workers (based on unpublished data from HealthServe and Karunya Community Clinics). Migrant workers in Singapore are also at risk of various occupational diseases (including work injuries, which can be life- or limb-threatening)(13) and various infectious diseases by virtue of their countries of origin, housing conditions or other behavioural factors.(14,15)
Data from this current survey on migrant worker healthcare, which was conducted among doctors from various restructured public hospitals, provides a parallel perspective and corroborates our survey findings of the migrant workers themselves.(7) Three main findings were gleaned from the current survey.
Firstly, culture and language remain significant healthcare barriers (92.3% of doctor-respondents). Navigating a complex medical system may be challenging for migrants due to language and cultural differences. Knowledge about healthcare coverage or entitlements may also be impaired because of a lack of clear information in their native language, especially if the details are not communicated clearly at the point of employment. In our previous survey among 433 non-domestic migrant workers, 22% were unsure if they had medical insurance coverage, and of those who knew they were insured, 60% were unsure if their insurance coverage included inpatient or outpatient costs. 73% reported not having received any insurance coverage information from their employers; of the 65 (15%) who did, only 21 (32%) received the information in their native language.(7) Efforts should be directed towards improving migrant workers’ understanding of healthcare provisions mandated by law and ensuring that insurance information is provided in the worker’s native language. Better delivery of healthcare information, including the wider use of educational materials in various languages spoken by migrants and more widespread use of language interpretation services (where appropriate), as well as continued education of healthcare providers to equip them to deliver culturally sensitive care, are important areas to focus on.
Secondly, financial factors pose a significant barrier to the delivery of healthcare to migrants. In the current study, 73.1% of doctor respondents reported encountering situations where healthcare delivery to a migrant worker was compromised, with financial barriers cited as a significant factor by 81.0% of respondents. In our recent companion survey among migrants,(7) 22% reported financial barriers to accessing healthcare, and on multivariable analysis, this was associated with a 3.9 times increased risk of psychological distress. Contributors to financial barriers may include the general lack of a mechanism for outpatient subsidies/coverage for low-wage migrant workers, possible breach of insurance payouts in the face of catastrophic illness and debt-fuelled migration (which often starts in the workers’ country of origin). While these issues are not easily resolved, a multilateral approach involving policymakers in both the sending and receiving countries, employers and insurers is needed. Suggested priority areas for further study and/or intervention have been detailed in our previous work.(7) While some improvements have been made in healthcare policy for migrant workers in Singapore (such as compulsory medical insurance for inpatient care and day surgery, which saw the minimum coverage raised from SGD 5,000 to SGD 15,000 in 2008), our survey highlights remaining barriers in the delivery of healthcare to migrant workers, from a healthcare provider’s perspective. It is hoped that this study, coupled with the findings from our recent migrant worker survey(7) and other recent studies,(8) will provide further data for lawmakers to improve healthcare policy, delivery and regulatory enforcement for our migrant workers in Singapore.
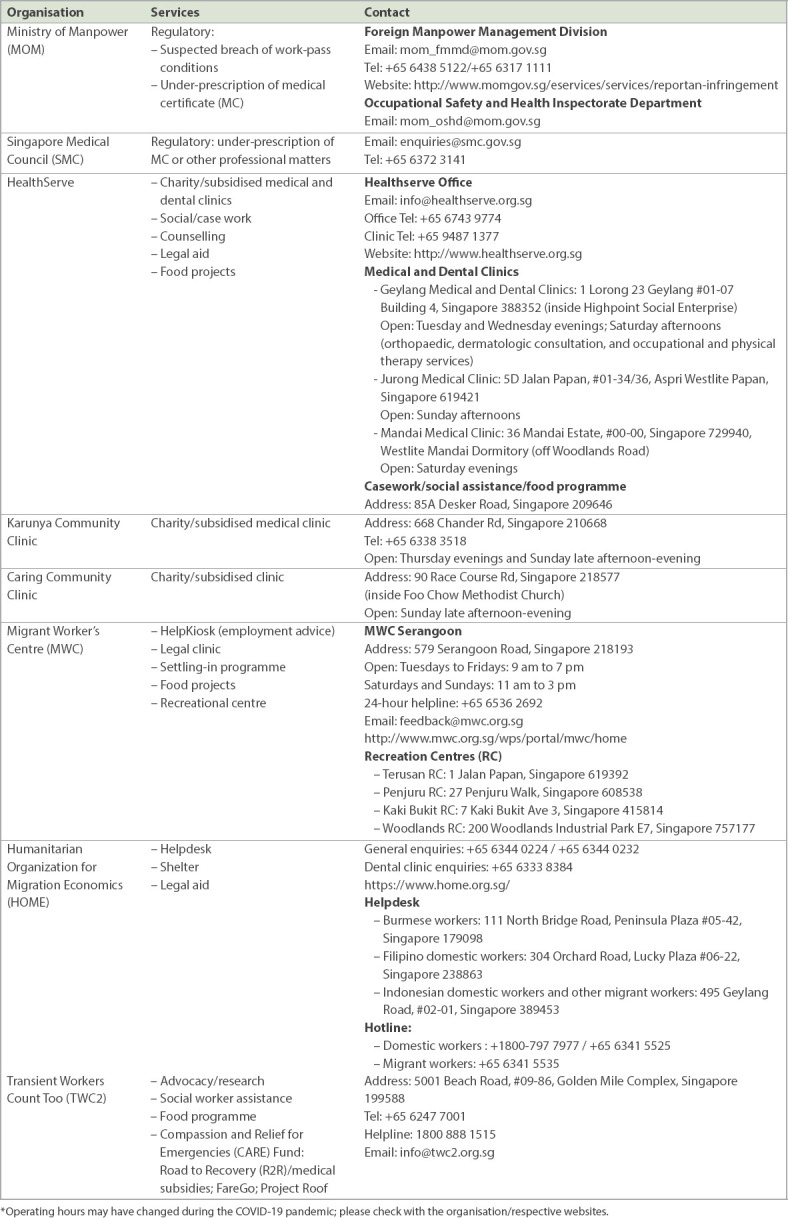
Lastly, akin to the lack of knowledge among migrants about healthcare coverage eligibility, doctors themselves were somewhat deficient in their knowledge of migrant health policies in Singapore (Table V). They answered a mean/median of 4–6 questions correctly, while half were unsure or wrong about migrant workers’ insurance coverage with regard to outpatient costs (migrant worker insurance in Singapore typically does not cover outpatient costs) and only about 67% answered correctly that employers were ultimately responsible for migrant workers’ medical treatment costs. About 42% of doctors were aware of avenues for redress should they encounter a case where a migrant worker was treated unfairly by the employer. When both healthcare workers (who should be advocates for patients’ care) and migrant workers have a deficit of knowledge on the provisions, laws and entitlements regarding migrant workers’ healthcare coverage, workers’ access to care or redress is likely to be impeded. Further efforts are urgently needed to improve this. Providers owe their patients a duty of care, and hence they should educate themselves and not remain ‘blissfully unaware’ of resources available to migrant workers and their entitlements under Singapore law. Table VI details some resources for migrant workers in Singapore that healthcare providers should be aware of, and we refer readers to a recently published article on practical guidance for doctors treating migrant workers in Singapore.(16) Encouragingly, migrant health has been incorporated into elective or service modules of the curriculum of our local medical, nursing and pharmacy schools. More efforts, however, should be directed toward incorporating migrant health into the core curriculum for all students of the health sciences locally, given that work-permit holders comprise about one-fifth of the resident population in Singapore.
Table VI.
Resources for migrant workers in Singapore.*
In conclusion, we identified various barriers to healthcare delivery to migrant workers in Singapore from the healthcare provider’s perspective. Among these, language/cultural and financial factors were cited as the most common barriers, but these are likely to be intertwined with multiple other factors such as prevailing healthcare policy, employer behaviour and the degree of knowledge/healthcare advocacy among healthcare providers. Further work is needed to overcome these barriers and improve migrant-health literacy among doctors, so that they may act as healthcare advocates for patients. In so doing, healthcare providers can contribute toward achieving universal health coverage and the promotion of a safe and secure working environment for all workers, as outlined in the United Nations (UN) 2030 Agenda for Sustainable Development (UN Sustainable Development Goals 3 and 8),(17) as well as creating a society where each migrant worker is valued and lives a life of dignity.
ACKNOWLEDGEMENTS
We would like to thank all the doctor-participants in this survey and the management of the various hospitals for their support of this survey.
REFERENCES
- 1.Ministry of Manpower Singapore. Foreign workforce numbers. [Accessed February 17 2019]. Available at:http://www.mom.gov.sg/documents-and-publications/foreign-workforce-numbers.
- 2.Department of Statistics Singapore. Yearbook of statistics Singapore. 2016. [Accessed August 19 2019]. Available at:http://www.singstat.gov.sg/docs/default-source/default-document-library/publications/publications_and_papers/reference/yearbook_2016/yos2016a.pdf .
- 3.Guinto RL, Curran UZ, Suphanchaimat R, Pocock NS. Universal health coverage in 'One ASEAN':are migrants included?Glob Health Action. 2015;8:25749. doi: 10.3402/gha.v8.25749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singapore Statutes Online. Employment of Foreign Manpower Act (Chapter 91a). Employment of Foreign Manpower (Work Passes) Regulations. 2012. [Accessed August 19 2019]. Available at:https://sso.agc.gov.sg/SL/EFMA1990-S569-2012 .
- 5.Ministry of Manpower Singapore. Medical insurance requirements for foreign worker. [Accessed August 6 2017]. Available at:http://www.mom.gov.sg/passes-and-permits/work-permit-for-foreign-worker/sector-specific-rules/medical-insurance.
- 6.Ministry of Manpower Singapore. Work injury compensation. [Accessed August 6 2017]. Available at:http://www.mom.gov.sg/workplace-safety-and-health/work-injury-compensation.
- 7.Ang JW, Chia C, Koh CJ, et al. Healthcare-seeking behaviour, barriers and mental health of non-domestic migrant workers in Singapore. BMJ Glob Health. 2017;2:e000213. doi: 10.1136/bmjgh-2016-000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee W, Neo A, Tan S, et al. Health-seeking behaviour of male foreign migrant workers living in a dormitory in Singapore. BMC Health Serv Res. 2014;14:300. doi: 10.1186/1472-6963-14-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhu M. Too injured to work:migrant workers fight for medical leave, compensation. Channel NewsAsia [online] [Accessed August 6 2017]. Available at:http://www.channelnewsasia.com/news/singapore/too-injured-to-work-migrant-workers-fight-for-medical-leave-comp-8001178.
- 10.Ho O. Worker with crushed finger gets just 1 day off. The Straits Times. 2016 Aug 2; [Google Scholar]
- 11.Johnraj MSP, Bacolod N, Phua KH. The Buck Stops Where?A Trilemma on HealthCare for Singapore's Foreign Workers. [Accessed February 17 2019]. Available at:https://lkyspp.nus.edu.sg/docs/default-source/case-studies/lkyspp-case-study-a-trilemma-healthcare-for-singapore's-foreign-workers.pdf?sfvrsn=8ecb9b0b_2 .
- 12.Ministry of Manpower Singapore. Sector-specific rules for Work Permit. [Accessed January 28 2019]. Available at:https://www.mom.gov.sg/passes-and-permits/work-permit-for-foreign-worker/sector-specific-rules/
- 13.Ong VY, Habibah AK, Lee FC. Safety among foreign workers and impact on emergency medicine services in Singapore. Singapore Med J. 2006;47:121–8. [PubMed] [Google Scholar]
- 14.Sadarangani SP, Lim PL, Vasoo S. Infectious diseases and migrant worker health in Singapore:a receiving country's perspective. J Travel Med. 2017;24(4) doi: 10.1093/jtm/tax014. doi:10.1093/jtm/tax014. [DOI] [PubMed] [Google Scholar]
- 15.Lai Y, Purnima P, Ho M, et al. Fatal case of diphtheria and risk for reemergence, Singapore. Emerg Infect Dis. 2018;24:2084–6. doi: 10.3201/eid2411.180198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chan J, Chia D. Practical advice for doctors treating foreign workers. [Accessed January 28 2019];SMA News. 2017 49:19–21[online]. Available at:https://www.sma.org.sg/UploadedImg/files/Publications%20-%20SMA%20News/4902/Insight.pdf . [Google Scholar]
- 17.Transforming our world:the 2030 Agenda for Sustainable Development. Sustainable Development Goals Knowledge Platform, United Nations [online] [Accessed February 17 2019]. Available at:https://sustainabledevelopment.un.org/post2015/transformingourworld .


