Abstract
COVID‐19 has overwhelmed the capacity of health care systems, limiting access to supportive and palliative care for patients with advanced cancer. Telemedicine has emerged as a tool to provide care continuity to patients while limiting the risk of contagion. However, implementing telemedicine in resource‐limited settings is challenging. We report the results of a multidisciplinary patient‐navigator‐led telemedicine supportive care program in Mexico City. One‐hundred sixty‐three telemedicine interventions were provided to 45 patients (median age 68, 57% female). A quarter of the patients had less than or equal to elementary school education, and 15% lived in a rural area. The most common interventions were psychological care (33%), pain and symptom control (25%), and nutritional counseling (13%). Half of the interventions were provided by video conferencing. The most common patient‐reported barrier was limited experience using communication technology. Our results demonstrate the feasibility of providing supportive and palliative care interventions using telemedicine in resource‐limited settings.
Short abstract
This article reports the results of a multidisciplinary patient‐navigator‐led telemedicine supportive care program in Mexico City, describing how a supportive and palliative care program was transformed into a telemedicine intervention for patients with advanced cancer to maintain care during the COVID‐19 pandemic.
Introduction
On March 11, the World Health Organization declared COVID‐19 a pandemic [1]. As of June 23, >9 million cases and 475,000 deaths had been reported worldwide [2]. In Mexico, COVID‐19 led to a health care system reorganization [3]: some hospitals were designated as COVID‐19 centers, and as a consequence, outpatient clinics were closed, elective surgeries were suspended, and patients needing emergency care were referred to non‐COVID hospitals.
Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán (INCMNSZ) is a public academic hospital in Mexico City, which was converted to a COVID‐19 center on March 20, 2020. Patients undergoing active cancer treatment at INCMNSZ maintained their oncology clinic visits and treatment appointments, although all other supportive care visits were suspended.
Offering continued supportive and palliative care represented a challenge, and telemedicine emerged as a potential solution [4]. Telemedicine is the use of communication and information technologies to provide clinical services [5] and represents an option to provide remote support to patients during the pandemic [6]. However, implementing telemedicine in resource‐limited settings might be challenging owing to disparities in access [7]. Here, we describe how we transformed a multidisciplinary supportive and palliative care program into a telemedicine intervention for patients with advanced cancer during the COVID‐19 pandemic.
Materials and Methods
In 2018, we implemented “Te Acompañamos,” a patient navigation program to increase access to supportive and palliative care for patients with advanced cancer at INCMNSZ. Currently, all consecutive patients with a recent diagnosis of advanced cancer seen at the oncology clinics at INCMNSZ are included in Te Acompañamos and undergo basal supportive and palliative care needs assessments (depression, anxiety, fatigue, pain, malnutrition, caregiver burden), which are reviewed by a multidisciplinary patient navigator (PN)‐led team (palliative care, physical therapy, geriatrics, psychology/psychiatry, oncology, and nutrition) that recommends tailored interventions. The PN then helps patients obtain the required interventions and engage in advance care planning, including advance directive completion. Up until INCMNSZ's conversion to a COVID‐19 center, Te Acompañamos had provided care for 337 patients with advanced cancer.
Upon INCMNSZ's conversion, we undertook adaptations to allow for Te Acompañamos to continue using telemedicine: (a) supportive care needs assessments were administered remotely; (b) the multidisciplinary team met weekly using Zoom to discuss patient needs and proposed interventions; (c) the PN presented patients with intervention plans remotely; and (d) if the interventions were accepted, team members implemented them remotely using various contact methods (video conferences, phone calls, messaging, etc.). All the patients with a recent diagnosis of advanced solid cancer who were already enrolled in Te Acompañamos were candidates for telemedicine interventions. In addition, new patients seen at the oncology clinics after INCMNSZ's conversion and who had a diagnosis of advanced cancer in the previous 3 months were also included. Before the interventions were implemented, patients were contacted to assess the availability of communication methods and received a brief training on how to use them. If needed, e‐mail accounts were created for them to receive recommendations and materials. Patients’ privacy and security were protected by instructing providers regarding the best clinical practice for telemedicine. For example, telemedicine interventions were recommended to occur in private settings, headphone use was encouraged, patients were advised to avoid high‐tone speakers, and recording was not allowed (both for the provider and for the patient). In addition, only non–public‐facing communication products using end‐to‐end encryption were used (Zoom, Google Hangouts video, or WhatsApp video chat).
After each intervention, providers were prospectively asked to complete an online multiple‐choice qualitative survey designed to assess barriers for telemedicine implementation. The survey was composed of 12 items (supplemental online Appendix 1), which included open‐ended questions for describing the intervention (type, cause of intervention, method used, length, and supportive material used), the findings during the consultation, and any follow‐up plans. Providers also answered whether the patient needed support to complete the intervention, who provided that support, and what barriers were identified before and during the intervention. Approval from the institutional review board at INCMNSZ was obtained.
We recorded the number and type of interventions that were provided remotely, as well as the communication methods used. In addition, we assessed potential barriers for successful implementation of the interventions. Descriptive statistics including means, medians, and standard deviations were used to analyze the data.
Results
Between March 27 and June 15, 163 supportive care interventions were provided to 45 patients (median number of interventions per patient 3; range 1–13). Median age was 68 years (range 33–90), and 57.7% were female. More than half (53.4%) had less than or equal to high school education (26.6% less than or equal to elementary school). The most common tumors were gastrointestinal (n = 22, 48%), followed by breast (n = 5, 11%).
Supportive care needs more commonly prompting interventions were pain (n = 52; 31.9%); anxiety (n = 31; 19%), fatigue (n = 29; 17.7%), depression (n = 24; 14.7%), and malnutrition (n = 20; 12.2%). Others included nausea (n = 12; 7.3%), caregiver burden (n = 11; 6.7%), abnormal geriatric screening (n = 8; 4.9%), and potential suicidal ideation (n = 4; 2.4%). The implemented interventions are shown in Table 1.
Table 1.
Telemedicine intervention characteristics
| Characteristic | n | % |
|---|---|---|
| Type of intervention | ||
| Psychological care | 54 | 33.1 |
| Pain and symptom control | 41 | 25.1 |
| Nutritional counseling | 20 | 12.6 |
| Physical therapy | 14 | 8.5 |
| End‐of‐life care | 13 | 7.9 |
| Geriatric assessment | 8 | 4.9 |
| Advance directive completion | 8 | 4.9 |
| Psychiatric care | 5 | 3.0 |
| Type of visit | ||
| First visit | 70 | 43 |
| Follow‐up care | 93 | 57 |
| Communication method | ||
| Live video conference | 77 | 47.2 |
| 36 | 46.7 | |
| WhatsApp/Zoom | 1 | 1.2 |
| Google Hangouts | 40 | 5.1 |
| Phone call | 73 | 44.7 |
| SMS/WhatsApp messaging | 23 | 14.1 |
| E‐mail | 1 | 0.6 |
| N/A | 4 | 2.4 |
| Length of the intervention, minutes | ||
| 0–15 | 38 | 23.3 |
| 16–30 | 58 | 35.6 |
| 31–45 | 37 | 22.7 |
| >45 | 29 | 17.8 |
| N/A | 1 | 0.6 |
| Assistance received to initiate communication | ||
| None | 81 | 49.6 |
| Siblings | 58 | 35.5 |
| Spouse/partner | 17 | 10.4 |
| Other | 14 | 8.5 |
| Participants in the intervention | ||
| Patient and provider alone | 76 | 46.6 |
| Family members | 80 | 49.0 |
| Other team personnel | 39 | 23.9 |
| Other | 1 | 0.6 |
| Materials provided | ||
| None | 106 | 65.0 |
| Videos (exercise routines) | 16 | 9.8 |
| Nutritional plan | 15 | 9.2 |
| Infographics | 15 | 9.2 |
| Medication prescriptions | 11 | 6.7 |
| Other | 5 | 3.0 |
Abbreviations: N/A, not applicable; SMS, short message service.
Methods used to deliver interventions varied according to patients’ preferences and intervention type (Table 1). The most common communication method was video conferencing (n = 77; 47.2%), followed by phone calls (n = 73; 44.7%). In half of cases (49.6%), patients started communication on their own, and the most common patient‐reported barrier for connecting via telemedicine was limited experience with the communication method (n = 46; 28.2%). During the interventions, the most frequent issues were interruptions (n = 24, 14.7%), problems with Internet connectivity (n = 21, 12.8%), and poor‐quality video/audio (n = 20, 12.2%). Figure 1 summarizes barriers to initiating and maintaining communication.
Figure 1.
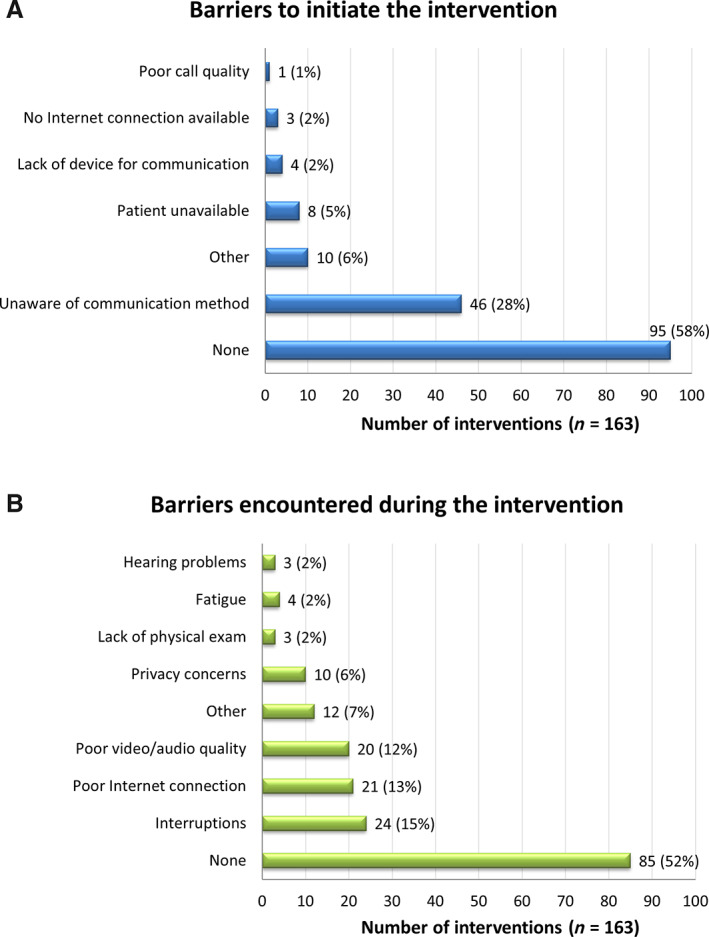
Telemedicine barriers. (A): To initiate communication. (B): During intervention.
Discussion
During the COVID‐19 pandemic, and despite the low availability of resources, the Te Acompañamos multidisciplinary supportive and palliative care program has provided a significant number of telemedicine interventions, even for patients with significant symptom burden (≥3 supportive care needs).
Telemedicine represents an effective modality for delivering supportive and palliative care [8]. However, implementing a telemedicine program in resource‐limited settings might be challenging owing to policy issues, concerns regarding malpractice‐related issues, lack of formal organizational structures and reimbursement mechanisms, poor interest from health care providers, technological barriers, prescription issues, and social/cultural limitations. However, we show that telemedicine interventions could be provided even though a significant proportion of our patients had low educational levels, lived in rural area, and/or were older adults [5].
The most common barriers reported by the providers were technological, including poor Internet connection and low technology awareness. Privacy issues also were reported, particularly during psychological care interventions, because patients often needed assistance from caregivers to maintain communication. In Mexico, the average number of people per household is four [9], and this overcrowding may contribute to a lack of privacy during real‐time telemedicine interventions. The increasing use of telemedicine during the COVID‐19 pandemic has raised concerns because some ways of remote communication between patients and providers might not fully comply with privacy regulations. In that regard, a recent notification by the U.S. Department of Health and Human Services recommends ensuring privacy by using non–public‐facing platforms and considers it acceptable to use software with end‐to end encryption that allows only individual users to communicate through it, such as Microsoft Teams, Updox, VSee, Zoom, Google Suite Hangouts, Cisco Webex Meeting, WhatsApp video chat, etc. [10]. That being said, it is important to mention that only provider‐reported barriers were collected in this study and that patient‐reported barriers could potentially differ, particularly regarding the patients’ opinion on privacy issues.
For telemedicine to work, patients must have access to electronic devices and to the Internet, which might be challenging in low‐income populations. However, although a significant proportion of people in Mexico have limited incomes, and < 50% of Mexicans own a computer, a significant proportion (75%) have an Internet connection and > 90% own a smartphone. In our study, the vast majority of patients received telemedicine interventions through a smartphone video conference or phone call [11].
Conclusion
Implementing a supportive and palliative care telemedicine program for patients with advanced cancer during the COVID‐19 pandemic is feasible in low‐ and middle‐income countries using readily available resources. Telemedicine represents an excellent method to maintain care continuity for patients with high symptom burden while limiting the risk of contagion for both patients and providers.
Disclosures
Yanin Chávarri‐Guerra: Roche (RF), Pfizer (travel expenses). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
Supporting information
See http://www.TheOncologist.com for supplemental material available online.
Appendix S1: Supporting information
Disclosures of potential conflicts of interest may be found at the end of this article.
No part of this article may be reproduced, stored, or transmitted in any form or for any means without the prior permission in writing from the copyright holder. For information on purchasing reprints contact Commercialreprints@wiley.com. For permission information contact permissions@wiley.com.
References
- 1. World Health Organization . WHO Timeline – COVID‐19. Available at https://www.who.int/news‐room/detail/27‐04‐2020‐who‐timeline‐‐‐covid‐19. Accessed June 23, 2020.
- 2. Johns Hopkins University . COVID‐19 Dashboard by the Center for Systems Science and Engineering (CSEE) at Johns Hopkins University (JHU). Available at https://coronavirus.jhu.edu/map.html. Accessed June 23, 2020.
- 3. BBC News Mundo . Confirman el pricer caso de coronavirus en Mexico. 29 febrero de 2020. Available at https://www.bbc.com/mundo/noticias-america-latina-51677751. Accessed June 23, 2020.
- 4. ESMO guidelines . Cancer Patient Management during the COVID‐19 Pandemic. Available at https://www.esmo.org/guidelines/cancer‐patient‐management‐during‐the‐covid‐19‐pandemic. Assessed June 23, 2020.
- 5. Bali S. Barriers to Development of Telemedicine in Developing Countries. Available at https://www.intechopen.com/books/telehealth/barriers‐to‐development‐of‐telemedicine‐in‐developing‐countries. Accessed June 23, 2020.
- 6. ASCO Special report: A guide to cancer care delivery during the COVID‐19 Pandemic . May 19, 2020. Available at https://www.asco.org/sites/new‐www.asco.org/files/content‐files/2020‐ASCO‐Guide‐Cancer‐COVID19.pdf. Accessed June 23, 2020.
- 7. Eberly LA, Khatana SAM, Nathan AS et al. Telemedicine outpatient cardiovascular care during the COVID‐19 pandemic: Bridging or opening the digital divide? Circulation 2020;142:510–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Calton B, Abedini N, Fratkin M. Telemedicine in the Time of Coronavirus. J Pain Symptom Manage 2020;60:e12–e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Instituto Nacional de Estadística y Geografía (INEGI) . Vivienda. Available at https://www.inegi.org.mx/temas/vivienda/ Accessed June 24, 2020.
- 10. U.S. Department of Health and Human Services . Notification of enforcement discretion for telehealth remote communications during the COVID‐19 nationwide public health emergency. Available at https://www.hhs.gov/hipaa/for‐professionals/special‐topics/emergency‐preparedness/notification‐enforcement‐discretion‐telehealth/index.html/. Accessed September 19, 2020.
- 11. Instituto Nacional de Estadñistica y Geografía (INEGI) . Encuestra sobre Disponibilidad y Uso de Tecnologías de la Información y la Comunicación en los Hogares 2018. Available at https://www.inegi.org.mx/programas/dutih/2018/. Accessed June 24, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
See http://www.TheOncologist.com for supplemental material available online.
Appendix S1: Supporting information


