Abstract
Objective
To evaluate the utility of a society-based robotic surgery training program for fellows in gynecologic oncology.
Methods
All participants underwent a 2-day robotic surgery training course between 2015–2017. The course included interactive didactic sessions with video, dry labs, and robotic cadaver labs. The labs encompassed a wide range of subject matter including troubleshooting, instrument variation, radical hysterectomies, and lymph node dissections. Participants completed a pre- and post-course survey using a 5-point Likert scale ranging from “not confident” to “extremely confident” on various measures. Statistical analysis was performed using SPSS Statistics v. 24.
Results
The response rate was high with 86% of the 70 participants completing the survey. Sixteen (26.7%) of these individuals were attending physicians and 44 (73.3%) were fellows. In general, there was a significant increase in confidence in more complex procedures and concepts such as radical hysterectomy (p=0.01), lymph node dissection (p=0.01), troubleshooting (p=0.001), and managing complications (p=0.004). Faculty comfort and practice patterns were cited as the primary reason (58.9%) for limitations during robotic procedures followed secondarily by surgical resources (34.0%).
Conclusion
In both gynecologic oncology fellows and attendings, this educational theory-based curriculum significantly improved confidence in the majority of procedures and concepts taught, emphasizing the value of hands-on skill labs.
Keywords: Robotics, Surgical Training, Surgical Education, Gynecologic Oncology
INTRODUCTION
Minimally invasive surgery was largely adopted in gynecologic cancers in the 1990s [1], and the Food and Drug Administration approved the robotic surgery platform for use in gynecologic surgery in 2005. Laparoscopy has some clear advantages over laparotomy including decreased recovery time, improved perioperative outcomes, shorter hospital stays, improved quality of life, and faster return to daily functions [2,3]. Robotic surgery has additional advantages over traditional laparoscopy, including 3-dimensional vision, instrumentation with wrist-like movements, elimination of hand tremors, resolution of the fulcrum effect, and increased accuracy and precision [4]. Ultimately, robotic surgery can allow surgeons to perform more complex procedures in a minimally invasive fashion while allowing greater precision [5]. The number of robot-assisted laparoscopic surgeries (RAS) have increased dramatically since their initial introduction. In 2012, RAS composed 1.5% of all surgical procedures, increasing to 15.1% in 2018 [6]. Despite this increase in robotic surgery, many training hospitals do not have a formalized robotic training program and the development of a simulation-based curriculum in training is needed [7,8].
Surgical training sessions have previously included didactic sessions, skills labs, virtual reality, cadaver training, and live hands-on sessions [8]. The goal of surgical simulation is to introduce complex surgical techniques in a controlled environment to facilitate uptake of new concepts and improve the surgical learning curve [9]. The goal is to allow surgeons to feel more comfortable performing a complex or rare procedure at an earlier stage. Simulation is also helpful in learning how to avoid and address potential complications [10].
There are various forms of surgical simulation, including electronic, wet labs, and dry labs [8,11]. Electronic robotic simulation is a virtual reality program that allows training on animated anatomy; whereas wet laboratories generally use a cadaver model to simulate a more realistic anatomic experience. Wet lab sessions tend to be expensive and require specialized facilities; thus, opportunities for repetitive training are limited. Dry laboratories use inanimate objects that are less realistic but useful for repetitive procedures and development of basic skill sets.
In a survey of gynecologic oncology programs in the United States, 95% of programs reported training their fellows in RAS, and many of these fellows plan to use it in their clinical practice after fellowship [12]. Previously, there has not been a standardized curriculum or training course for RAS in gynecologic oncology. In order to address these issues, a robotic training course was created to better equip gynecologic attendings and fellows with the skills needed to perform complex procedures using RAS. The goal of this study was to evaluate the outcomes of this standardized Society of Gynecologic Oncology (SGO) robotic training course.
MATERIALS AND METHODS
All participants were enrolled in a 2-day SGO robotic surgery training course between 2015–2017. The courses were held in Florida, California, and Georgia. All participants signed a consent prior to involvement in their respective course. The course curriculum was based on instructional theory and designed to include interactive didactic sessions with surgical video, dry labs, wet labs, and electronic robotic simulation (Table 1). The educational sessions and videos reviewed surgical practices and complications of robotic surgery including radical hysterectomies, omentectomy, port placement in thin versus obese patients, side versus perineal docking, and running an efficient operating room, among others. The labs encompassed a wide range of subject matter including troubleshooting, instrument variation, radical hysterectomies and other dissections, and lymph node dissections (Table 2 for all topics reviewed). Fellows were encouraged to attend the course with a supervising attending. Participants were asked to complete a pre- and post-course survey rating their confidence levels (Table 2). A 5-point Likert scale that ranged from “not confident” to “extremely confident” was used to measure confidence levels in participants. The course was paid for by SGO through an unrestricted grant from Intuitive. This grant covered renting space, the robotic systems, and obtaining cadavers. The instructors did not receive any honoraria. Statistical analysis including a paired t-test was performed using SPSS Statistics v. 24 (IBM Corp., Armonk, NY, USA).
Table 1. Robotic course outline.
| Day 1: Lectures and dry labs | Day 2: Cadaver lab | ||||
|---|---|---|---|---|---|
| Attendings and fellows | Fellows | ||||
| • Introduction/overview | • Cadaver lab 1 | ||||
| • Dry lab (docking and port placement) 1 | Port placement | ||||
| Suturing | Docking | ||||
| Pelvic vessel sealing | Third arm utilization | ||||
| Stapler | Advanced energy use | ||||
| Simulator | Pelvic lymph node dissection | ||||
| Table motion | Radical hysterectomy | ||||
| • Special topics lectures | • Cadaver lab 2 | ||||
| Sentinel lymph nodes (identification and dissection) | Para-aortic/pelvic lymph node dissection | ||||
| Robotic hysterectomy, omentectomy | Complications and management | ||||
| Uterine manipulators | Troubleshooting | ||||
| Side versus perineal docking | |||||
| Use of fourth arm | Attendings | ||||
| Running an efficient operating room | • Lectures | ||||
| • Dry lab 2 | Tips for teaching residents and fellows | ||||
| Troubleshooting exercises | Advanced robotics | ||||
| • Video review with faculty commentary | • Work with fellows in cadaver lab | ||||
Table 2. Confidence level questions and results.
| Concept and procedures | Average CL* | Relative increase (%) | p-value | 95% confidence interval | |
|---|---|---|---|---|---|
| Before | After | ||||
| Port placement & patient positioning | 3.36 | 4.15 | 23.5 | 0.079 | −1.81, 0.23 |
| Instrument selection & 3rd party products | 2.92 | 3.95 | 35.3 | 0.053 | −2.09, 0.03 |
| Docking and port placement | 3.28 | 4.20 | 28.0 | 0.016 | −1.43, −0.42 |
| Robotic hysterectomy | 3.53 | 4.17 | 18.1 | 0.086 | −1.51, −0.42 |
| Radical hysterectomy | 2.26 | 3.34 | 47.8 | 0.011 | −1.57, −0.60 |
| Lymph node dissection | 2.70 | 3.59 | 33.0 | 0.011 | −1.28, −0.48 |
| Robotic omentectomy | 2.16 | 3.02 | 39.8 | 0.051 | −1.73, 0.01 |
| Uterine manipulators | 3.78 | 4.19 | 10.8 | 0.068 | −0.90, 0.07 |
| Port placement in obese patients | 3.08 | 4.11 | 33.4 | 0.014 | −1.56, −0.50 |
| Port placement in thin patients | 3.20 | 4.10 | 28.1 | 0.025 | −1.51, −0.28 |
| Side docking versus perineal docking | 2.86 | 3.94 | 37.8 | 0.016 | −1.68, −0.48 |
| Running an efficient operating room | 2.84 | 3.67 | 29.2 | 0.030 | −1.46, −0.20 |
| Suturing | 3.46 | 4.06 | 17.3 | 0.075 | −1.34, 0.15 |
| Pelvic vessel sealing | 3.29 | 3.96 | 20.4 | 0.018 | −1.06, −0.20 |
| Complex cases | 2.55 | 3.35 | 31.4 | 0.025 | −1.36, −0.24 |
| 4th arm utilization | 3.13 | 4.00 | 27.8 | 0.010 | −1.25, −0.49 |
| Advanced energy use | 3.17 | 3.95 | 24.6 | 0.010 | −1.10, −0.44 |
| Pelvic lymph node dissection | 2.97 | 3.85 | 29.6 | 0.023 | −1.47, −0.30 |
| Para-aortic lymph node dissection | 2.16 | 3.29 | 52.3 | 0.027 | −1.94, −0.31 |
| Complications & management | 2.43 | 3.48 | 43.2 | 0.004 | −1.34, −0.76 |
| Troubleshooting | 2.44 | 3.79 | 38.9 | 0.001 | −1.52, −1.20 |
Bold p-value indicates significance.
*Confidence level based on 5-point scale.
CL, confidence level.
RESULTS
The response rate was high with 86% of the 70 participants completing the survey. The 16 (26.7%) of these individuals were attending physicians and 44 (73.3%) were fellows. On average, participants had performed 35.7 robotic hysterectomies (range 4–100) and 3.3 radical hysterectomies (range 0–16) in the preceding year.
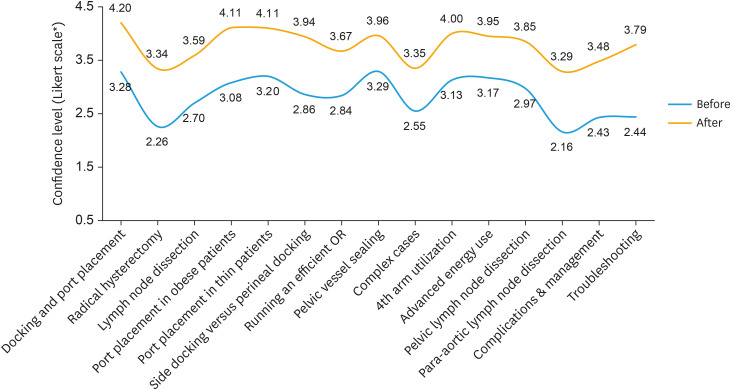
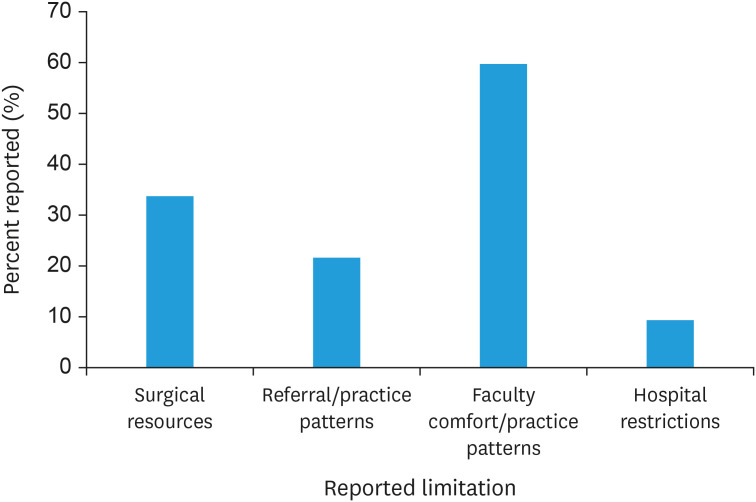
There was a trend of increased confidence in most areas with 15 of 21 being significant (Fig. 1). There was a significant increase in confidence in more complex procedures and concepts such as radical hysterectomy (p=0.01), lymph node dissection (p=0.01), troubleshooting (p=0.001), and managing complications (p=0.004; Table 2). There was no significant increase found in 6 areas including: port placement/patient positioning, uterine manipulators, instrument selection, simple robotic hysterectomy, robotic omentectomy, and suturing. Faculty comfort and practice patterns were cited as the primary reason (59.8%) for limitations in exposure to certain robotic procedures followed secondarily by surgical resources (33.8%) (Fig. 2).
Fig. 1.
Procedures/concepts with significantly improved confidence levels.
*Likert scale: 0 (less confident) to 5 (completely confident).
Fig. 2.
Reasons for limitations in robotic procedures.
*Individuals were asked to select 1 or more indications.
DISCUSSION
This study showed that in both gynecologic oncology fellows and attendings, this curriculum led to significantly improved confidence levels in the majority of procedures and concepts taught (Fig. 1). This highlights the fact that simulation programs may be beneficial in introducing complex surgical techniques and allowing for development of skills in a controlled environment. Participants specifically noted that “troubleshooting” and “management of complications” were particularly helpful. Areas where no significant improvement was found were more commonly performed tasks such as suturing, port placement, hysterectomy, and placing the uterine manipulator.
In order for surgical simulation to be beneficial, it must actually affect the surgeon's operative performance and have educational impact [13,14]. The simulation must be validated in some way in order to be able to evaluate if performance is improved. This validation includes assessing “the realism of the simulator,” “the ability to differentiate novice from experienced operators,” “the extent to which the results of the test coordinate with the gold standard,” and “the extent to which an assessment will predict future performance” [15]. The Global Evaluative Assessment of Robotic Skills metrics is one method that has been independently validated [16,17]. It scores trainees' performance in multiple areas, including depth perception, bimanual dexterity, efficiency, force sensitivity, autonomy, and robotic control. Studies using validated assessments such as these are important in evaluating if the simulation sessions are actually beneficial or just perceived to be. This is where electronic robotic simulators have an advantage given they are capable of providing statistical feedback to the performer [15]. While this study evaluated participants' perceived confidence, a formal validation of the simulator could be incorporated in future sessions.
While virtual reality simulators have a role, tasks such as troubleshooting, management of complications, and more complicated procedures may be better taught in a live setting given the hands-on nature of these subjects. This robotics course attempts to include all modalities of learning including interactive didactic sessions with video, dry labs, and robotic cadaver labs. This allows for learning to occur in a repetitive, yet realistic, fashion. Previous robotics courses have demonstrated that dedicated training sessions are vital in mastering surgical skills especially with complex procedures [18,19].
Another aspect of this study brought to light was that faculty comfort and practice patterns were cited as the primary reason (59.8%) for limitations during robotic procedures. As fellows are encouraged to participate with their faculty members in this course, this allows the opportunity for both entities to bring home new surgical skills. This is among the first courses to incorporate and assess the involvement of both fellows and invited faculty members. Surgical resources were noted to be the second most common reason (34%) for limitations of robotic procedures. This robotic training course allows surgeons to use various robotic surgical tools to evaluate if they would be useful in their home practices.
The main limitation of this study is the use of self-reported responses, which are inherently biased, rather than validated pre- and post-technical assessments. Additionally, while there was an excellent response rate, the sample size was small with only 70 participants included. The data includes aggregate information from fellows and attendings. However, the majority of the attendings had been practicing for 8 years or less and all individuals in the course were considered learners. Finally, the resources needed for this curriculum (cadavers, robotic simulators, etc.) would make it challenging to implement broadly outside of a focused course. A strength of the study is that the cohort represents a diverse group of institutions from all over the United States.
Robotic surgery has become a staple in gynecologic oncology, and while most fellowships have incorporated it into their training, there is currently no standardized method to evaluate training across programs. Confidence and understanding of the process is an important element in skill acquisition and mastery. This robotic surgical simulation course is an opportunity to evaluate and train individuals in more complicated techniques that may not present frequently in clinical practice. The goal of this study was to evaluate if there was a change in confidence in the participants but not the actual skill acquisition. Based on this survey, the educational theory-based curriculum in this study significantly improved confidence in the majority of procedures and concepts taught, emphasizing the value of hands-on skill labs. Overall, robotic surgery courses can augment traditional surgical education to ensure surgeons are kept up-to-date on procedures, troubleshooting, and society standards.
Footnotes
Presentation: Poster Presentation at the Society of Gynecologic Oncology 49th Annual Meeting on Women's Cancer, March 16, 2018, Honolulu, HI, USA.
Funding: Dr. Kim reports grants from Intuitive Surgical and personal fees from Ethicon. Dr. Cohen reports personal fees from the Society of Gynecologic Oncology and an educational grant from Intuitive Surgical.
Conflict of Interest: Dr. Kim reports grants from Intuitive Surgical, personal fees from Ethicon, outside the submitted work. Drs. Cohen, Kim, and Rossi report: The course was funded by an unrestricted educational grant from Intuitive Surgical. Drs. Boitano and Smith have nothing to disclose.
- Conceptualization: C.J.G., R.E.C., K.K.H.
- Data curation: B.T.K.L., S.H.J., K.K.H.
- Formal analysis: B.T.K.L.
- Investigation: C.J.G., R.E.C.
- Project administration: C.J.G., R.E.C., K.K.H.
- Writing - original draft: B.T.K.L.
- Writing - review & editing: S.H.J., C.J.G., R.E.C., K.K.H.
References
- 1.Childers JM, Brzechffa PR, Hatch KD, Surwit EA. Laparoscopically assisted surgical staging (LASS) of endometrial cancer. Gynecol Oncol. 1993;51:33–38. doi: 10.1006/gyno.1993.1242. [DOI] [PubMed] [Google Scholar]
- 2.Galaal K, Donkers H, Bryant A, Lopes AD. Laparoscopy versus laparotomy for the management of early stage endometrial cancer. Cochrane Database Syst Rev. 2018;10:CD006655. doi: 10.1002/14651858.CD006655.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Medeiros LR, Rosa DD, Bozzetti MC, Fachel JM, Furness S, Garry R, et al. Laparoscopy versus laparotomy for benign ovarian tumour. Cochrane Database Syst Rev. 2009:CD004751. doi: 10.1002/14651858.CD004751.pub3. [DOI] [PubMed] [Google Scholar]
- 4.Kho RM, Hilger WS, Hentz JG, Magtibay PM, Magrina JF. Robotic hysterectomy: technique and initial outcomes. Am J Obstet Gynecol. 2007;197:113.e1–113.e4. doi: 10.1016/j.ajog.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Zihni A, Gerull WD, Cavallo JA, Ge T, Ray S, Chiu J, et al. Comparison of precision and speed in laparoscopic and robot-assisted surgical task performance. J Surg Res. 2018;223:29–33. doi: 10.1016/j.jss.2017.07.037. [DOI] [PubMed] [Google Scholar]
- 6.Sheetz KH, Claflin J, Dimick JB. Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw Open. 2020;3:e1918911. doi: 10.1001/jamanetworkopen.2019.18911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shepherd W, Arora KS, Abboudi H, Shamim Khan M, Dasgupta P, Ahmed K. A review of the available urology skills training curricula and their validation. J Surg Educ. 2014;71:289–296. doi: 10.1016/j.jsurg.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Vetter MH, Green I, Martino M, Fowler J, Salani R. Incorporating resident/fellow training into a robotic surgery program. J Surg Oncol. 2015;112:684–689. doi: 10.1002/jso.24006. [DOI] [PubMed] [Google Scholar]
- 9.Liss MA, McDougall EM. Robotic surgical simulation. Cancer J. 2013;19:124–129. doi: 10.1097/PPO.0b013e3182885d79. [DOI] [PubMed] [Google Scholar]
- 10.Badash I, Burtt K, Solorzano CA, Carey JN. Innovations in surgery simulation: a review of past, current and future techniques. Ann Transl Med. 2016;4:453. doi: 10.21037/atm.2016.12.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tarr ME, Rivard C, Petzel AE, Summers S, Mueller ER, Rickey LM, et al. Robotic objective structured assessment of technical skills: a randomized multicenter dry laboratory training pilot study. Female Pelvic Med Reconstr Surg. 2014;20:228–236. doi: 10.1097/SPV.0000000000000067. [DOI] [PubMed] [Google Scholar]
- 12.Sfakianos GP, Frederick PJ, Kendrick JE, Straughn JM, Kilgore LC, Huh WK. Robotic surgery in gynecologic oncology fellowship programs in the USA: a survey of fellows and fellowship directors. Int J Med Robot. 2010;6:405–412. doi: 10.1002/rcs.349. [DOI] [PubMed] [Google Scholar]
- 13.Schout BM, Hendrikx AJ, Scheele F, Bemelmans BL, Scherpbier AJ. Validation and implementation of surgical simulators: a critical review of present, past, and future. Surg Endosc. 2010;24:536–546. doi: 10.1007/s00464-009-0634-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McDougall EM. Validation of surgical simulators. J Endourol. 2007;21:244–247. doi: 10.1089/end.2007.9985. [DOI] [PubMed] [Google Scholar]
- 15.Abboudi H, Khan MS, Aboumarzouk O, Guru KA, Challacombe B, Dasgupta P, et al. Current status of validation for robotic surgery simulators - a systematic review. BJU Int. 2013;111:194–205. doi: 10.1111/j.1464-410X.2012.11270.x. [DOI] [PubMed] [Google Scholar]
- 16.Goh AC, Goldfarb DW, Sander JC, Miles BJ, Dunkin BJ. Global evaluative assessment of robotic skills: validation of a clinical assessment tool to measure robotic surgical skills. J Urol. 2012;187:247–252. doi: 10.1016/j.juro.2011.09.032. [DOI] [PubMed] [Google Scholar]
- 17.Aghazadeh MA, Jayaratna IS, Hung AJ, Pan MM, Desai MM, Gill IS, et al. External validation of Global Evaluative Assessment of Robotic Skills (GEARS) Surg Endosc. 2015;29:3261–3266. doi: 10.1007/s00464-015-4070-8. [DOI] [PubMed] [Google Scholar]
- 18.Rusch P, Kimmig R, Lecuru F, Persson J, Ponce J, Degueldre M, et al. The Society of European Robotic Gynaecological Surgery (SERGS) pilot curriculum for robot assisted gynecological surgery. Arch Gynecol Obstet. 2018;297:415–420. doi: 10.1007/s00404-017-4612-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mark Knab L, Zenati MS, Khodakov A, Rice M, Al-Abbas A, Bartlett DL, et al. Evolution of a novel robotic training curriculum in a complex general surgical oncology fellowship. Ann Surg Oncol. 2018;25:3445–3452. doi: 10.1245/s10434-018-6686-0. [DOI] [PubMed] [Google Scholar]