Abstract
Background:
In the area of nephrology, the practical application of relative survival methodologies can provide information regarding the impact of outcomes for patients with kidney failure on dialysis compared with what would be expected in the absence of this condition.
Objective:
Compare the net survival of hemodialysis (HD) and peritoneal dialysis (PD) patients in a cohort of incident patients on chronic dialysis in Colombia, according to the dialysis therapy modality.
Design:
Observational, analytic, historical cohort.
Setting:
Renal Therapy Services (RTS) clinic network across Colombia.
Patients:
Patients over 18 years old with chronic kidney disease, incidents in dialytic therapy, which reached day 90 of therapy. Recruitment took place from January 1, 2008, to December 31, 2013, with a follow-up until December 31, 2018. The final cohort for analysis corresponds to a total of 12 508 patients, of which 5330 patients (42.6%) began HD and 7178 patients (57.4%) began PD.
Measurements:
Demographic, socioeconomic, and clinical variables were measured.
Methods:
Analyses were conducted according to the treatment assigned (PD or HD) at the time of the inception of the cohort and another approach of analysis was done with a subsample of those patients who never changed the initial modality. To calculate expected survival, life tables were constructed for Colombia for the years 2006 to 2018. Net survival estimates were made using the Pohar Perme estimator. The comparison of the net survival curves was done using the method developed by Pavlič and Perme, the log-rank type.
Results:
Net survival at 5 years compared with the general population was estimated at 0.53 (95% confidence interval 0.52-0.54) in the dialysis cohort. In intention-to-treat analyses of 7178 patients on PD and 5330 patients on HD, by global and Pohar-Perme methods, survival (expressed as a ratio of survival in patients on dialysis to survival in an age-, sex- and geographic-matched general Colombian population) was higher in patients on HD than in those on PD. In year 1, net survival by Pavlov-Perme on PD was 0.79 (95% confidence intervals [CI] 0.78 - 0.80) and on HD 0.85 (95% CI 0.84 - 0.86); in year 5, 0.36 (95% CI 0.34 – 0.38) and 0.57 (95% CI 0.55 – 0.59) for PD and HD respectively.
Limitation:
There may be imbalances among the populations analyzed (HD vs PD), in which one or more variables other than the type of therapy may influence the survival of the patients. In Colombia there are marginal levels of underreporting of demographic data in some subpopulations that may affect life-tables construction.
Conclusion:
An important difference was observed in terms of survival between the dialysis population and the population of reference without dialysis. Statistically significant differences were found in net survival between HD and PD, net survival was higher in patients on HD than in those on PD.
Keywords: chronic kidney disease, peritoneal dialysis, hemodialysis, net survival, survival analysis
Abrégé
Contexte:
En néphrologie, l’application pratique des méthodologies de survie relative peut fournir des renseignements sur l’impact des résultats des patients atteints d’insuffisance rénale suivant des traitements de dialyse comparativement à ce qui serait attendu en l’absence de cette affection.
Objectif:
Comparer la survie nette, selon la modalité de dialyse, dans une cohorte de patients colombiens traités par hémodialyse (HD) ou par dialyse péritonéale (DP) de façon chronique.
Type d’étude:
Étude de cohorte observationnelle, analytique et historique.
Cadre:
Le réseau Renal Therapy Services (RTS) de la Colombie.
Sujets:
Des patients adultes souffrant d’insuffisance chronique ayant nouvellement débuté la dialyse depuis plus de 90 jours. Le recrutement a eu lieu du 1er janvier 2008 au 31 décembre 2013, et le suivi s’est poursuivi jusqu’au 31 décembre 2018. L’analyse porte sur un total de 12 508 patients, dont 5 330 (42,6 %) avaient entrepris des traitements d’hémodialyse et 7 178 (57,4 %) de dialyse péritonéale.
Mesures:
Les données démographiques, socio-économiques et cliniques des patients.
Méthodologie:
Les analyses ont été menées en fonction du traitement attribué (DP ou HD) au moment de la création de la cohorte. Une autre analyse a été réalisée sur un sous-échantillon de patients n’ayant jamais changé la modalité depuis le début du traitement. Des tables de survie spécifiques à la Colombie entre les années 2006 et 2018 ont été élaborées pour calculer la survie attendue. Les estimations de survie nette ont été faites en utilisant l’estimateur de Pohar Perme. Et la méthode développée par Pavlič et Perme, soit le test du log-rank a servi à la comparaison des courbes de survie nette.
Résultats:
La survie nette après cinq ans, comparée à celle de la population générale, a été estimée à 0,53 (IC 95 %: 0,52 à 0,54) dans la cohorte de patients dialysés. Dans les analyses en intention de traiter portant sur 7 178 patients sous HD et 5 330 patients sous DP — réalisées par méthode globale et avec l’estimateur Pohar Perme — la survie (exprimée sous forme de rapport entre la survie de patients dialysés et la survie de Colombiens de la population générale du même âge, sexe et région géographique) s’est avérée plus élevée chez les patients sous HD que chez les patients sous DP. Au cours de la première année, la survie nette (Pavlov Perme) des patients sous DP s’établissait à 0,79 (IC 95 % : 0,78-0,80) et celle des patients sous HD à 0,85 (IC 95 % : 0,84-0,86); après cinq ans, elle était passée à 0,36 (IC 95 % : 0,34-0,38) pour les patients sous DP et à 0,57 (IC 95 % : 0,55-0,59) pour les patients sous HD.
Limites:
Il pourrait exister des disparités parmi les populations analysées (HD vs DP), où des variables autres que la modalité pourraient influencer la survie des patients. Il existe, dans certaines sous-populations de Colombie, des niveaux marginaux de sous-déclaration des données démographiques qui pourraient affecter l’élaboration des tables de survie.
Conclusion:
Une différence importante a été observée entre la survie des patients dialysés et celle d’une population de référence (personnes non dialysées). On a également constaté des différences statistiquement significatives entre le groupe sous HD et le groupe sous DP en ce qui concerne la survie nette, laquelle s’est avérée plus élevée chez les patients sous HD.
What was known before
There are some published studies using methods of relative survival for studying chronic kidney disease; however, few studies compare both modalities of dialysis using methods such as relative or net survival.
What this adds
This study represents a strong starting point for the application of the methods of net survival in nephrology, by estimating the net survival probabilities according to the modalities of dialysis in the Colombian network of renal centers.
Introduction
In recent decades, in a global context characterized by the increasing prevalence of chronic diseases, including chronic kidney disease (CKD), there has emerged a considerable interest in the assessment of health outcomes among dialysis modalities, including the comparison between survival outcomes of peritoneal dialysis (PD) and hemodialysis (HD). Although strong evidence has been built up on survival on dialysis, the question of whether a difference in survival exists between dialysis modes remains a controversial issue.1,2,3-10,11,12 In most of these studies, the outcome of the study is defined as all-cause mortality, which includes all deaths in the study cohort without distinguishing those by the disease of interest. In general, these approaches are not very useful for estimating the prognosis of CKD patients on dialysis therapy.
In survival analysis, when the interest lies in the study of cause-specific deaths, complications may arise due to problems in establishing the cause of death of a patient, the presence of many different causes of death in the cohort, or the difficulty in assigning death to a single cause.13 In this regard, the methods of analysis of relative survival can directly measure the excess mortality of a group of patients with a specific disease, when compared with the mortality of the general population, obtaining an estimate of net survival.14 This concept of net survival describes the net effect of a disease after removing the effects of competitive causes of death, originated from the general population.15 That is, it would be the survival that could be observed if the only causes of death were those directly or indirectly related to the disease of interest. In the area of nephrology, the practical application of relative survival methodologies can provide information regarding the impact of outcomes for patients with kidney failure on dialysis compared with what would be expected in the absence of this condition.
Renal Therapy Services (RTS) is a network of renal clinics located in Colombia, serving around 9000 dialysis patients (about 33% of the population on dialysis in Colombia) in 50 centers. It is important to highlight that 40% of this population on dialysis are treated in PD.
As outstanding characteristics of the RTS health care process, it must be said that there is no reuse of dialyzers, the proportion of patients with access for HD type arteriovenous fistula or AV graft is 82%, and the minimum standard of frequency and duration of HD is 4 hours 3 times a week. Regarding PD, the patient attends a monthly comprehensive evaluation, the nurse / PD patient ratio is 1:50, and the peritonitis rate is 0.21 episodes per patient-year.
The aim of this study is to compare the net survival of HD and PD patients in a cohort of incident patients on chronic dialysis in Colombia, according to the dialysis modality.
Materials and Methods
Type of Study
We conducted an observational, analytic, historical cohort study using data from medical records of RTS patients. This study was conducted using a prespecified protocol, approved by Renal Therapy Services Research Ethics Board in Bogotá, Colombia.
Population
Patients of RTS were included between January 1, 2008, and December 31, 2013, with a follow-up until December 31, 2018. To be admitted to the study cohort, patients had to be over 18 years old with chronic kidney disease, incident patients receiving dialysis therapy, and reached day 90 of therapy. The main outcome of the study was death from all causes. The causes of censorship on the right were change of health insurer, suspension or abandonment of treatment, kidney transplant, recovery of residual kidney function, completion of follow-up without the occurrence of death, and change of therapy censored after 30 days.
Procedures for Variable Measurement and Gathering of Information
Demographic, socioeconomic, and clinical variables were collected at the beginning of patient follow-up. Data collection was done directly from medical records. The electronic medical record has systematically parameterized predictive and outcome variables and has processes and procedures for quality control of clinical information that are validated monthly.
The specific death rates of the population were calculated using data from the population projections of the Colombian National Administrative Department of Statistics and the mortality data available in the Integral information system of Ministry of health. With the mortality and population information collected, life tables were constructed for the Colombian population, for the years 2006 to 2019, considering age, sex, and departments. A process of smoothing out the mortality rates was done using a functional demographic model.
Statistical Analysis
Quantitative variables were described by calculating medians and interquartile range. Qualitative variables were described as proportions. Calculations of 95% confidence intervals were performed. Comparison tests were performed using the chi-square test for qualitative variables and the Mann-Whitney test for quantitative variables.
The calculation of the global survival was done through Kaplan Meier’s method and the comparison of survival curves was done through the Log-rank method. To calculate expected survival, life tables were constructed for Colombia for the years 2006 to 2018. The calculation of net survival was performed by the Pohar Perme estimator. The net cumulative survival function was defined as the ratio between observed and expected survival in the general population, interpreted as the proportion of patients who survived from the start of follow-up until time t, representing the probability of surviving dialysis therapies in the absence of other causes of death. The comparison of the net survival curves was done using the method developed by Pavlič and Perme, the log-rank type.16 Age-standardized rates were reported.
Two approaches of analysis were carried out. First, the patients were analyzed according to the treatment assigned (PD or HD) at the time of the inception of the cohort, censoring at the moment of change of therapy. The other approach of analysis was done with a subsample of those patients who never changed the initial modality. The statistical analyses were conducted with the program R version 3.6.3, by the packages survival and relsurv.17-19
Results
Patients
A total of 12 508 patients were included in the analysis, of which 5330 patients (42.6%) began on HD and 7178 patients (57.4%) began on PD. A median follow-up time of 4.88 years was recorded for the total number of patients (95% confidence interval [CI] 4.72-5.05 years).
Regarding the sociodemographic characteristics at the beginning of the follow-up, statistically significant differences were found in age and sex. The main cause of renal disease was diabetes in 5540 patients (44.3%) (Table 1). In terms of comorbidities, statistically significant differences in the presence of diabetes and hypertension were reported (P < .001). The summary of the clinical laboratory variables is presented in Table 2. There were significant differences in the albumin levels between HD and PD cohorts (P < .001). The PD group had higher residual kidney function (P < .001) (Table 2).
Table 1.
Sociodemographic Characteristics by Therapy Modality, at the Beginning of the Follow-up.
| Characteristics | Hemodialysis (n = 5330) |
Peritoneal dialysis (n = 7178) |
P value |
|---|---|---|---|
| Age, median [interquartile range] | 63 [52, 72] | 60 [49, 70] | <.001* |
| Age <65 years, n (%) | 2914 (54.7) | 4475 (62.3) | <.001* |
| Age ≥65 years, n (%) | 2416 (45.3) | 2703 (37.7) | |
| Females, n (%) | 1974 (37.0) | 3271 (45.6) | <.001* |
| Socioeconomic level, n (%) | .002 | ||
| 1 | 1840 (34.5) | 2583 (36.0) | |
| 2 | 169 (3.2) | 287 (4.0) | |
| 3 | 2055 (38.6) | 2807 (39.1) | |
| 5 | 385 (7.2) | 455 (6.3) | |
| No data | 881 (16.5) | 1046 (14.6) | |
| Education level, n (%) | .159 | ||
| Illiterate | 373 (7.0) | 474 (6.6) | |
| Reads and writes | 1319 (24.7) | 1666 (23.2) | |
| Primary | 1935 (36.3) | 2598 (36.2) | |
| Secondary | 1314 (24.7) | 1897 (26.4) | |
| Technical | 112 (2.1) | 163 (2.3) | |
| University | 277 (5.2) | 380 (5.3) | |
| Rural residence, n (%) | 427 (8.0) | 882 (12.3) | < .001* |
| Contributive affiliation type, n (%) | 3599 (67.5) | 4998 (69.6) | .013* |
Statistically significant.
Table 2.
Clinical Characteristics by Therapy Modality, at the Beginning of the Follow-up.
| Characteristics | Hemodialysis (n = 5330) |
Peritoneal dialysis ( n = 7178) |
P value |
|---|---|---|---|
| Chronic kidney disease cause, n (%) | <.001* | ||
| Hypertension | 1296 (24.3) | 1668 (23.2) | |
| Diabetes | 2163 (40.6) | 3377 (47.0) | |
| Obstructive | 383 (7.2) | 229 (3.2) | |
| Polycystic kidney disease | 105 (2) | 135 (1.9) | |
| Tubulointerstitial | 33 (0.6) | 43 (0.6) | |
| Glomerular | 397 (7.4) | 729 (10.2) | |
| Pyelonephritis | 12 (0.2) | 11 (0.2) | |
| Unknown | 610 (11.4) | 701 (9.8) | |
| Others | 331 (6.2) | 285 (4.0) | |
| Diabetes, n (%) | 2557 (48.0) | 3843 (53.5) | <.001* |
| Hypertension, n (%) | 4204 (78.9) | 5914 (82.4) | <.001* |
| Ischemic cardiovascular disease, n (%) | 673 (12.6) | 837 (11.7) | .107 |
| Cerebrovascular disease, n (%) | 176 (3.3) | 232 (3.2) | .867 |
| Heart failure, n (%) | 725 (13.6) | 963 (13.4) | .783 |
| Body mass index (kg/m2), median [IQR] | 23.4 [20.8, 26.2] | 24 [21.5, 26.8] | <.001* |
| Weight (kg) | 62 [54, 70.8] | 63 [54.8, 72] | .006* |
| Charlson index, n (%) | .110 | ||
| No comorbidity (score 0-1) | 1381 (29) | 2079 (30.5) | |
| Moderate comorbidity (score 2-3) | 2473 (51.9) | 3403(50) | |
| High comorbidity (score >3) | 914 (19.2) | 1325 (19.5) | |
| No Charlson index data, n (%) | |||
| Hemoglobin (g/dL), median [IQR] | 10.4 [9.1, 11.7] | 11.5 [10.2, 12.6] | <.001* |
| Phosphorus (mg/dL), median [IQR] | 4.1 [3.3, 5] | 4.4 [3.7, 5.3] | <.001* |
| Albumin (g/dL), median [IQR] | 3.8 [3.5, 4.1] | 3.5 [3.1, 3.9] | <.001* |
| Albumin <3.5 g/dL, n (%) | 1085 (22.4) | 2890 (41.2) | <.001* |
| Albumin 3.5 to <4 g/dL, n (%) | 2067 (42.7) | 2773 (39.5) | |
| Albumin ≥4 g/dL, n (%) | 1960 (34.9) | 1359 (19.4) | |
| No albumin data, n (%) | 488 (9) | 156 (2.2) | |
| Parathyroid hormone (pg/mL), median [IQR] | 152 [73, 298] | 217.7 [118, 366.2] | <.001* |
| Ferritin (ng/mL), median [IQR] | 328 [156.7, 587.5] | 303.1 [152, 563] | .004* |
| Iron (µg/dL), median [IQR] | 45.6 [33, 61.5] | 53.4 [38, 72.6] | <.001* |
| Platelet count, median [IQR] | 245 000 [197 000, 309 000] | 282 000 [227 000, 347 000] | <.001* |
| Lymphocyte count, median [IQR] | 2540 [1790, 3790] | 2680 [1920, 4400] | <.001* |
| Lymphocyte platelet ratio, median [IQR] | 94.8 [56, 133] | 99.7 [50.3, 137.7] | .022* |
| Use of erythropoiesis-stimulating agents (ESA) (IU/kg), median [IQR] | 6000 [4000, 12 000] | 6000 [4000, 8000] | <.001* |
| ESA resistance index, median [IQR] | 12 [7.4, 19.8] | 8.4 [5, 13.3] | <.001* |
| nPCR (g/kg/day), median [IQR] | 0.9 [0.4, 1.2] | 0.9 [0.6, 1.2] | .819 |
| Malnutrition Index Inflammation, median [IQR] | 0 [0, 3] | 0 [0, 3] | <.001* |
| Residual diuresis (mL/day), median [IQR] | 0 [0, 975] | 700 [320, 1250] | <.001* |
| No residual diuresis (≤100 mL/day), n (%) | 3093 (76.9) | 929 (23.1) | <.001* |
| No residual diuresis data, n (%) | 199 (4) | 109 (1.5) |
Note. IQR = interquartile range; nPCR = normalized protein catabolic rate.
Statistically significant.
Survival Analysis
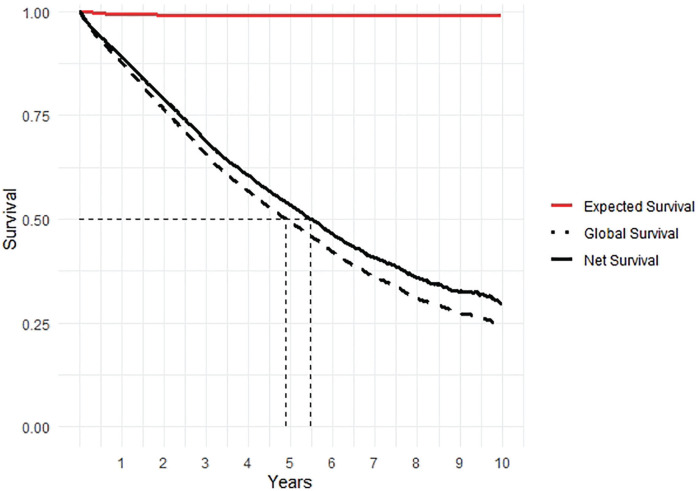
A total of 5042 deaths were reported, with a mortality rate of 14.1 deaths per 100 patients/year (95% CI 13.7-14.5). The median global survival time was reported to be 4.88 years (95% CI 4.72-5.05) and a net survival at 5 years of 0.53 (95% CI 0.52-0.54) in the total dialysis cohort (Figure 1).
Figure 1.
Survival curves of the patients in the cohort. Comparison of observed, expected, and net survival times.
Note. The figure compares survival observed, expected, and net survival curves. The median global survival time was 4.88 years (95% CI 4.72-5.05) and a net survival at 5 years of 0.53 (95% CI 0.52-0.54) in the dialysis chronic kidney disease cohort. The difference between the two survival measures at 5 years indicates that dialysis patients die 4% more from causes other than those related to dialysis. CI = confidence interval.
Analysis in Patients According to the Treatment Assigned at the Time of the Inception of the Cohort
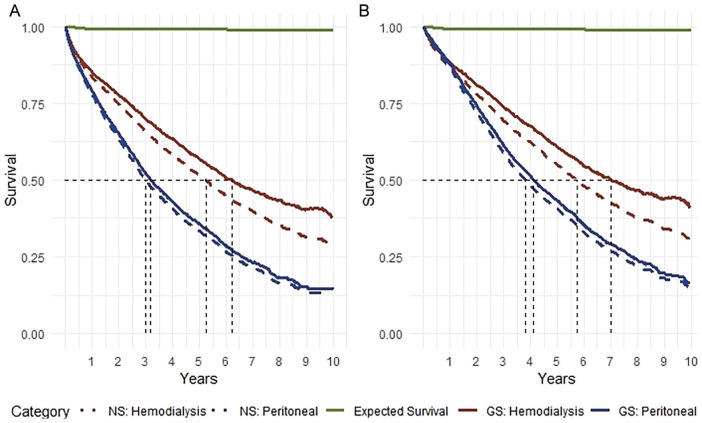
The median net survival time was 6.5 years (95% CI 6.1-7.1) for the HD group, compared with 3.19 years (95% CI 3.05-3.36) for the PD group (log-rank type P < .001). Net survival was higher in the HD group (85%, 95% CI 84-86%) compared with the PD group (79%, 95% CI 78-80%) (Table 3). Figure 2 shows the survival curves according to the therapy modality.
Table 3.
Global and Net Survival Function in Patients According to the Treatment Assigned at the Time of the Inception of the Cohort.
| Years | Peritoneal dialysis (n = 7178) |
Hemodialysis (n = 5330) |
||
|---|---|---|---|---|
| Global survivala | Net survival (95% CI) | Global survivala | Net survival (95% CI) | |
| 1 | 0.78 | 0.79 (0.78-0.80) | 0.83 | 0.85 (0.84-0.86) |
| 2 | 0.63 | 0.65 (0.64-0.66) | 0.75 | 0.78 (0.76-0.79) |
| 3 | 0.50 | 0.52 (0.51-0.54) | 0.66 | 0.70 (0.68-0.71) |
| 4 | 0.41 | 0.43 (0.41-0.45) | 0.59 | 0.63 (0.62-0.65) |
| 5 | 0.33 | 0.36 (0.34-0.38) | 0.52 | 0.57 (0.55-0.59) |
Note. CI = confidence interval.
In which the outcome is death from all causes.
Figure 2.
Survival curves by therapy modality.
Note. Comparison of observed, expected, and net survival times. (A) Analysis in patients according to the treatment assigned at the time of the inception of the cohort. (B) Analysis in patients who never changed the initial modality. The results of both approaches were consistent in showing differences in both mortality rates and net survival between peritoneal dialysis and hemodialysis. NS = net survival; GS = global survival.
Analysis in Patients Who Never Changed the Initial Modality
In patients who did not change therapy, 4344 deaths occurred, with a standardized mortality rate of 17.6 per 100 patients/year (95% CI 17-18.3) for the PD group and 12.3 per 100 patients/year (95% CI 11.7-13) for the HD group.
Net median survival time was 7 years (95% CI 6.3-7.8) for the HD group, compared with 4.1 (95% CI 3.9-4.3) years for the PD group (log-rank type P < .001). After the second year of follow-up, net survival was higher in the HD group (80.9%, 95% CI 79.5-82.3) compared with the PD group (73.9%, 95% CI 72.6-75.2) (Table 4).
Table 4.
Global and Net Survival Function in Patients Who Never Changed the Initial Modality.
| Year | Peritoneal dialysis (n = 6155) |
Hemodialysis (n = 4645) |
||
|---|---|---|---|---|
| Global survivala | Net survival (95% CI) | Global survivala | Net survival (95% CI) | |
| 1 | 0.87 | 0.87 (0.86-0.88) | 0.86 | 0.88 (0.87-0.89) |
| 2 | 0.72 | 0.73 (0.72-0.75) | 0.78 | 0.80 (0.79-0.82) |
| 3 | 0.59 | 0.61 (0.59-0.62) | 0.69 | 0.73 (0.71-0.75) |
| 4 | 0.49 | 0.51 (0.49-0.53) | 0.62 | 0.67 (0.65-0.69) |
| 5 | 0.41 | 0.43 (0.41-0.45) | 0.55 | 0.60 (0.58-0.63) |
Note. CI = confidence interval.
In which the outcome is death from all causes.
Discussion
The health outcomes of patients receiving chronic dialysis has been improving over the past 7 decades1,20,21; however, in terms of survival outcomes, there is still much to be improved. Chronic dialysis patients, as well as the general population, can be exposed to risks associated with their lifestyle, environment, accidents, and other determinants that can lead to deterioration in health status. Few studies have addressed the problem of comparing survival on dialysis with the general population without CKD.22-24 Our study estimated the global and net survival in a population of prevalent patients on chronic dialysis, while contrasting them against the expected population survival for Colombia.
The application of net survival methods is still under development in nephrology. One of the advantages of relative or net survival methods is that it is not necessary to know the causes of death of the people within the study because, when compared with the mortality rates of the general population, we can obtain a net measure of survival in the absence of causes of death different from those related to chronic renal disease and dialysis. Second, it allows dialysis outcomes to be comparable between different countries, health systems, and between different chronic diseases, since it manages to contrast the survival of a population with a specific pathology, against a reference population.22
A substantial body of evidence has been generated about the survival in HD and PD. With net survival methods, we found significant differences between net and expected survival. Our dialysis population had a 5-year net survival of 53.3% (95% CI 52%-54%), compared with a probability a 5-year general population survival of 99%. This difference reflects a window of opportunities in the improvement of survival of patients on chronic dialysis, among which we highlight actions at the level of public health, in dialysis technologies, patient follow-up, and other strategies to improve survival in this population.
Some studies have shown that global survival is similar or better in the first or second year for the PD group, being later improved by the HD group.2-4,7
Among the strengths of this study is the large number of patients included in the cohort, which is a representative sample of the country’s dialysis patients. The patients belong to a network of renal clinics, which allowed a strict 5-year follow-up, and an exhaustive quality control based on standardized processes in an electronic clinical record system. Another strength is the performance of a statistical analysis conducted under two approaches: by separating those patients who never changed the initial dialysis modality from the patients who had at least one dialysis modality change over the follow-up period. In terms of strengths related to methodology, it was the use of department-specific life tables, taking into account the great variability that exists among the country’s departments and favoring comparison of the survival of the cohort with a general population with more similar characteristics.25,26 On the other hand, considering the limited literature on the subject, this study opens a whole field of study in relative and net survival in nephrology.
A limitation of the present study is its observational design; thus, there may be imbalances among the populations analyzed (HD vs PD). This leads to the well-known phenomenon of confounding, in which one or more variables other than the type of therapy may influence the survival of the patients. More studies should be done with matching methodologies or multivariate methods to address this limitation. Given that life tables are constructed with secondary sources, the precision of these estimators will always depend on the quality of the registered demographic information, which in Colombia, in spite of being of good quality, has demonstrated marginal levels of underreporting in some subpopulations.
Conclusion
This study estimated the global and net survival in a population of prevalent patients on chronic dialysis, while contrasting them against the expected population survival for Colombia. An important difference was observed in terms of survival between the dialysis population and the population of reference without dialysis. Statistically significant differences were found in net survival between HD and PD, net suvival was higher in patients on HD than in those on PD, where an advantage was observed for the HD group. More studies are needed to address the problem of imbalance between the two populations and its consequent problem of confounding. This study represents a strong starting point for the application of the methods of net survival in the area of nephrology, considering that the latter can permit comparisons between countries and health systems, among other comparisons of significant impact on public health.
Acknowledgments
The authors express their gratitude to all the patients and nursing teams who participated in the study. They also thank Jasmin Vesga, MSc, NR, and Andrea Aldana, PE, for their involvement in verifying and cleaning the data.
Footnotes
Ethics Approval and Consent to Participate: This study was approved by Renal Therapy Services Research Ethics Board in Bogotá, Colombia.
Consent for Publication: All authors have given their consent for publication of this article.
Availability of Data and Materials: A secure database that meets the requirements of confidentiality that safeguards patient privacy is maintained as part of the study protocol. To ensure patient privacy is maintained, the data will not be made available.
Author Contributions: L.H.: Original research project conception and design, statistical analysis, and data interpretation. F.G.: Original research project conception and design, statistical analysis, and data interpretation. M.S.: Original research project conception and design, data acquisition, statistical analysis, and data interpretation. All authors have been involved in the drafting of the manuscript or revising it critically for important intellectual content and provided final approval of the version to be published. All authors verify that they have met all the journal’s requirements for authorship. All authors agree to be accountable for all aspects of the work, ensuring the accuracy and integrity of the publication. All authors approved the final manuscript draft submitted for publication.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Professor Gil is a full-time employee of Department of Clinical Epidemiology and Biostatistics, School of Medicine, Pontifical Javeriana University. Bogota, DC, Colombia, and Dr Sanabria is a full-time employee of Renal Therapy Services-Latin America, Bogotá, Colombia. Dr Herrera reports no conflict of interest.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Lina Herrera  https://orcid.org/0000-0002-2582-3869
https://orcid.org/0000-0002-2582-3869
Fabián Gil  https://orcid.org/0000-0001-6444-7248
https://orcid.org/0000-0001-6444-7248
References
- 1. Sanabria M, Muñoz J, Trillos C, et al. Dialysis outcomes in Colombia (DOC) study: a comparison of patient survival on peritoneal dialysis vs hemodialysis in Colombia. Kidney Int Suppl. 2008(108):S165-S172. [DOI] [PubMed] [Google Scholar]
- 2. Sens F, Schott-Pethelaz AM, Labeeuw M, Colin C, Villar E. Survival advantage of hemodialysis relative to peritoneal dialysis in patients with end-stage renal disease and congestive heart failure. Kidney Int. 2011;80(9):970-977. http://www.kidney-international.org. Accessed December 28, 2020. [DOI] [PubMed] [Google Scholar]
- 3. Thiery A, Séverac F, Hannedouche T, et al. Survival advantage of planned haemodialysis over peritoneal dialysis: a cohort study. Nephrol Dial Transplant. 2018;33(8):1411-1419. [DOI] [PubMed] [Google Scholar]
- 4. Han SS, Park JY, Kang S, et al. Dialysis modality and mortality in the elderly: a meta-analysis. Clin J Am Soc Nephrol. 2015;10(6):983-993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kumar VA, Sidell MA, Jones JP, Vonesh EF. Survival of propensity matched incident peritoneal and hemodialysis patients in a United States health care system. Kidney Int. 2014;86(5):1016–1022. http://www.kidney-international.org. Accessed December 28, 2020. [DOI] [PubMed] [Google Scholar]
- 6. Mehrotra R, Chiu YW, Kalantar-Zadeh K, Bargman J, Vonesh E. Similar outcomes with hemodialysis and peritoneal dialysis in patients with end-stage renal disease. Arch Intern Med. 2011;171(2):110-118. [DOI] [PubMed] [Google Scholar]
- 7. Kim H, Kim KH, Park K, et al. A population-based approach indicates an overall higher patient mortality with peritoneal dialysis compared to hemodialysis in Korea. Kidney Int. 2014;86(5):991-1000. http://www.kidney-international.org. Accessed December 28, 2020. [DOI] [PubMed] [Google Scholar]
- 8. Yang F, Khin LW, Lau T, et al. Hemodialysis versus peritoneal dialysis: a comparison of survival outcomes in South-East Asian patients with end-stage renal disease. PLoS One. 2015;10(10):e0140195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhou H, Sim JJ, Bhandari SK, et al. Early mortality among peritoneal dialysis and hemodialysis patients who transitioned with an optimal outpatient start. Kidney Int Rep. 2019;4(2):275-284. doi: 10.1016/j.ekir.2018.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sandoval C. Association between type of dialysis and survival in patients with chronic renal disease in Colombia. Analysis with Marginal Structural Models; 2017. [Google Scholar]
- 11. Waldum-Grevbo B, Leivestad T, Reisæter A V., Os I. Impact of initial dialysis modality on mortality: a propensity-matched study. BMC Nephrol. 2015;16(1):179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McDonald SP, Marshall MR, Johnson DW, Polkinghorne KR. Relationship between dialysis modality and mortality. J Am Soc Nephrol. 2008;20(1):155-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Silvia García Ortega MLGP. Supervivencia Relativa; 2014. http://masteres.ugr.es/moea/pages/tfm1314/tfmgarcia_ortega/!. Accessed December 28, 2020.
- 14. Nelson CP, Lambert PC, Squire IB, Jones DR. Relative survival: what can cardiovascular disease learn from cancer. Eur Heart J. 2008;29(7):941-947. https://academic.oup.com/eurheartj/article-abstract/29/7/941/483787. Accessed December 28, 2020. [DOI] [PubMed] [Google Scholar]
- 15. Mariotto AB, Noone AM, Howlader N, et al. Cancer survival: an overview of measures, uses, and interpretation. J Natl Cancer Inst Monogr. 2014;2014(49):145-186. https://uvirtual.javeriana.edu.co/bbcswebdav/pid-773344-dt-content-rid-6848094_1/courses/030130_1830_10128/MariottoAB2014.pdf. Accessed December 28, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pavlič K, Perme MP. On comparison of net survival curves. BMC Med Res Methodol. 2017;17(1):1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pohar M, Stare J. Making relative survival analysis relatively easy. Comput Biol Med. 2007;37(12):1741-1749. [DOI] [PubMed] [Google Scholar]
- 18. Pohar M, Stare J. Relative survival analysis in R. Comput Methods Programs Biomed. 2006;81(3):272-278. http://www.pauldickman.com/survival/handouts/93—RelativesurvivalanalysisinR.pdf. Accessed December 28, 2020. [DOI] [PubMed] [Google Scholar]
- 19. Pohar Perme M, Pavlič K. Nonparametric relative survival analysis with the R package relsurv. J Stat Softw. 2018;87(8):1–27. [Google Scholar]
- 20. Pippias M, Jager KJ, Kramer A, et al. The changing trends and outcomes in renal replacement therapy: data from the ERA-EDTA Registry. Nephrol Dial Transplant. 2016;31(5):831-841. https://academic.oup.com/ndt/article-lookup/doi/10.1093/ndt/gfv327. Accessed December 28, 2020. [DOI] [PubMed] [Google Scholar]
- 21. Neuen BL, Chadban SJ, Demaio AR, Johnson DW, Perkovic V. Chronic kidney disease and the global NCDs agenda. BMJ Glob Health. 2017;2(2):e000380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nordio M, Limido A, Maggiore U, Nichelatti M, Postorino M, Quintaliani G. Survival in patients treated by long-term dialysis compared with the general population. Am J Kidney Dis. 2012;59(6):819-828. https://linkinghub.elsevier.com/retrieve/pii/S0272638612001138. Accessed December 28, 2020. [DOI] [PubMed] [Google Scholar]
- 23. Gibertoni D, Mandreoli M, Rucci P, et al. Excess mortality attributable to chronic kidney disease. J Nephrol. 2016;29(5):663-671. [DOI] [PubMed] [Google Scholar]
- 24. Foster BJ, Laskin BL, Mitsnefes MM, Dahhou M, Zhang X. Changes in excess mortality from end stage renal disease in the United States from 1995 to 2013. Clin J Am Soc Nephrol. 2017;13(1):91-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Okuyama A, Shibata A, Nishimoto H. Critical points for interpreting patients’ survival rate using cancer registries: a literature review. J Epidemiol. 2017;28(2):61-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Stroup AM, Cho H, Scoppa SM, Weir HK, Mariotto AB. The impact of state-specific life tables on relative survival. J Natl Cancer Inst Monogr. 2014;2014(49):218-227. http://seer.cancer.gov/. Accessed December 28, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]