Abstract
Musculoskeletal injury is an uncommon but usually self-limited complication of vaccine administration. We present a case of progressive inflammatory monoarthritis of the shoulder characterized by bone erosion, bursitis, and severe synovitis caused by an influenza vaccine administered to the ipsilateral deltoid region. Clinical symptoms began within 2 hours of vaccination, with progressive decline in function over 6 weeks. Magnetic resonance imaging examinations performed 5 months apart demonstrated progressive erosive changes of the greater tuberosity, rotator cuff injury, and extensive enhancing synovitis of the glenohumeral joint and subacromial/subdeltoid bursa. After the exclusion of septic arthritis and osteomyelitis, the patient underwent nonoperative treatment and experienced near-complete recovery at 32 months. Although inflammatory arthritis of the shoulder following vaccination is rare, there have been previous reports of it. Clinicians and radiologists need to be aware of this potential complication to ensure an accurate diagnosis.
Abbreviations and Acronyms: CT, computed tomography; MRI, magnetic resonance imaging
Influenza vaccination in the United States has risen from 12.4 million vaccinations in 1981 to nearly 160 million in 2018,1 and it is expected to continue to increase in the future. Estimated benefits from these vaccinations include the aversion of 7.1 million influenza illnesses, 3.7 million fewer medical visits, 109,000 fewer hospitalizations, and 8000 fewer deaths in 2017-2018.2 These benefits are overwhelming relative to the most common postvaccination adverse effect of mild and transient muscle soreness. However, there has been a corresponding rise in the number of postvaccination adverse events reported to the Vaccine Adverse Event Reporting System, rising from 228 during the program’s inception in 1990 to nearly 12,000 in 2018 for all types of administered vaccines.3 In 2018, there were 10,230 reported influenza vaccination-related complications of varying severity, representing only 0.006% of influenza vaccine recipients.3 Of these reports, 27 influenza vaccine recipients (.000017%) described shoulder pain, injury, or synovitis that was usually self-limited. Given the widespread availability of the influenza vaccination to the general public, along with employer mandates, the relatively rare but more serious vaccine-related complications will likely be seen more frequently clinically and on advanced imaging studies.
Although rare, musculoskeletal injury is a potentially serious complication of vaccine administration. The shoulder is most commonly affected, presenting as bursitis, tendonitis, or adhesive capsulitis. These symptoms are thought to be most commonly related to improper injection techniques that result in intra-articular or intrabursal vaccine administration.4, 5, 6 Reports of associated bone destruction following vaccination are extremely rare. We present a case of progressive erosive arthritis and adhesive capsulitis of the glenohumeral joint following influenza vaccine administration into the ipsilateral deltoid region. The symptoms resolved over the course of 32 months with nonoperative management that included physical therapy and an ultrasound-guided intra-articular corticosteroid injection. We also discuss imaging features that aided in distinguishing an inflammatory from an infectious process.
Case Report
A 51-year-old man presented with acute onset of left shoulder pain that started within 2 hours of receiving an influenza vaccination in the ipsilateral deltoid region. The injection was administered with a 1-inch, 22-gauge needle in a location 1 cm distal to the lateral edge of the acromion. Of note, the patient was slender and physically fit with a weight of 59 kg and body mass index of 21 kg/m2. He had no significant medical history and no known allergies. He had previously received annual influenza vaccinations for more than 20 years without incident. Soon after the onset of pain, the shoulder became stiff with decreased internal and external rotation. Over the next month, he noted continued progressive loss of range of motion and sleep disruption owing to pain. Magnetic resonance imaging (MRI) obtained 6 weeks after the vaccination demonstrated a small focal area of cortical irregularity and indistinctness involving the posterolateral humeral head with surrounding bone marrow edema, suggestive of cortical erosion (Figure 1). A small amount of fluid and soft tissue thickening involving the overlying subacromial/subdeltoid bursa suggested mild focal bursitis. Increased T2 signal within the superficial fibers of the adjacent infraspinatus tendon was indicative of tendinopathy or tendon injury with bursal surface fibrillation. The findings were predominantly in close proximity to the site of vaccine administration. However, the edema within the infraspinatus tracked medially within the superficial fibers of the muscle belly. There was also mildly increased T2 signal within the inferior glenohumeral ligament, mild synovitis in the rotator interval, obliteration of the retrocoracoid fat, and thickening of the coracohumeral ligament, all of which are commonly seen in the clinical setting of adhesive capsulitis7 (Figure 1). A clinical diagnosis of adhesive capsulitis related to vaccine administration was made, and the patient was given ice, nonsteroidal anti-inflammatory drugs, and physical therapy.
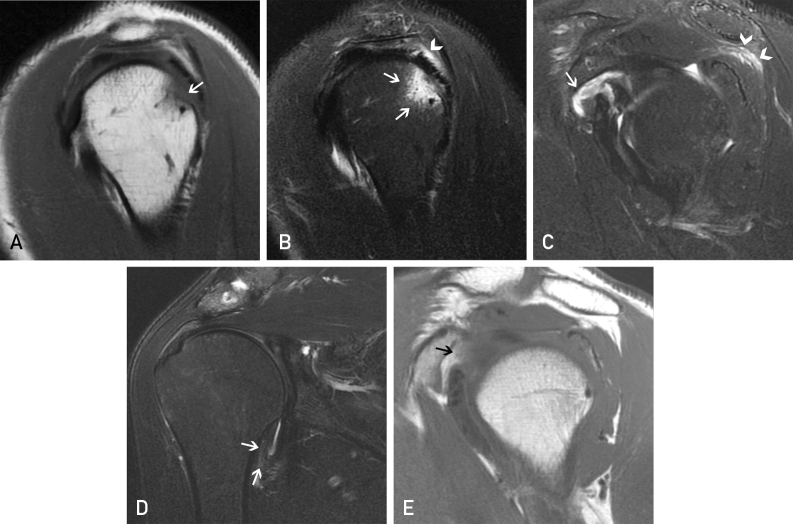
Figure 1.
Magnetic resonance imaging of the left shoulder obtained 6 weeks after vaccine administration and onset of symptoms. (A) Sagittal T1 and (B, C) sagittal fat-suppressed T2-weighted images demonstrate focal cortical irregularity and indistinctness of posterior margin of the greater tuberosity (arrow in A) with surrounding bone marrow edema within the posterolateral humeral head superiorly (arrows in B). There is also focal fluid and edema in the overlying subacromial/subdeltoid bursa and superficial fibers of the infraspinatus tendon (arrowhead in B). The edema within the infraspinatus tracks medially within the superficial and superior fibers of the muscle belly (arrowheads in C). There is evidence of synovitis in the rotator interval and subscapularis recess (arrow in C). (D) Coronal T2-weighted image demonstrates minimally increased T2 signal within the inferior glenohumeral ligament (arrows in D), and (E) sagittal T1 image demonstrates obliteration of the retrocoracoid fat and thickening of the coracohumeral ligament (arrow in E), findings that are suggestive of adhesive capsulitis in the appropriate clinical setting.
The patient had mild improvement in symptomatology initially but plateaued after 2 months. A follow-up evaluation 6 months after the onset of pain revealed classic findings of adhesive capsulitis on physical examination. There was no erythema, soft tissue swelling, or reported history of fever. However, radiographs, computed tomography (CT), and repeated MRI showed interval progression of the erosive changes involving the posterior margin of the greater tuberosity (Figure 2). MRI also revealed an increase in the surrounding bone marrow edema, enhancing glenohumeral and acromioclavicular joint synovitis, and progression of the imaging findings of capsulitis with an edematous and enhancing inferior glenohumeral ligament. The changes related to subacromial/subdeltoid bursitis had also increased, with increased bursal edema and moderate enhancement. Abnormal thickening and increased T2 signal within the infraspinatus tendon progressed, and there was new abnormal increased T2 signal extending anteriorly into the supraspinatus tendon without any interval trauma or inciting event after the initial MRI.
Figure 2.
Radiographic, computed tomographic, and magnetic resonance images from 6 months after vaccine administration and onset of symptoms and 5 months after the magnetic resonance imaging examination shown in Figure 1. (A) Anteroposterior radiograph of the left shoulder in internal rotation suggests progression of cortical erosion along the posterior greater tuberosity (arrows in A, B, and C). (B) Sagittal reformatted computed tomographic image and (C) coronal T1 magnetic resonance imaging confirm the progression of the erosive changes. (D) Coronal T2 and (E) post–gadolinium-enhanced coronal spoiled gradient recalled acquisition (SPGR) (E) demonstrate the enhancing bone marrow edema underlying the erosions (asterisks in D and E) and the enhancing synovitis and capsulitis (white arrows in D and E) and subacromial/subdeltoid bursitis (black arrows in D and E).
The significant radiologic progression over the 9 months following symptom-onset raised concern for an infectious or inflammatory process. The erythrocyte sedimentation rate, C-reactive protein, and white blood cell count were normal. Analysis of rheumatoid factor and cyclic citrullinated peptide antibodies had negative results. A glenohumeral joint aspiration did not yield any fluid. An indium white blood cell/sulfur colloid marrow scan and 3-phase technetium 99m-methyl diphosphonate bone scan showed a focal area of white blood cell activity in the humeral head that was matched by sulfur colloid uptake, indicating that white blood cell uptake was due to activated bone marrow rather than infection. In addition, there was only mildly increased activity in the left humeral head on delayed phase bone scan (Figure 3), which is also more consistent with an inflammatory or reactive process than osteomyelitis.
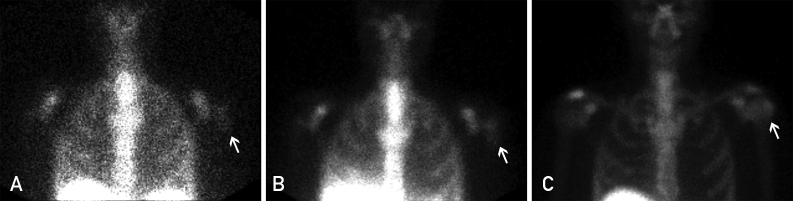
Figure 3.
Planar anteroposterior images of the shoulders from (A) indium-111 white blood cell scan 24 hours after injection, (B) Tc-99m sulfur colloid bone marrow scan approximately 1 hour after radiotracer injection, and (C) delayed phase planar anteroposterior image from 3-phase Tc-99m-methyl diphosphonate bone scan 3 hours after injection demonstrating a focus of increased white blood cell activity near the junction of the left humeral head and neck (arrow in A), which is matched by sulfur colloid uptake (arrow in B), indicating that the white blood cell activity is due to activated bone marrow rather than infection or osteomyelitis. In addition, the mildly increased uptake on the delayed phase images (arrow in C) is less intense than would be expected in the presence of osteomyelitis.
Given the lack of fluid (“dry tap”) on aspiration and the bone scan findings, septic arthritis and osteomyelitis were excluded from the differential diagnosis. He underwent an ultrasound-guided glenohumeral joint corticosteroid injection with 4 mL of bupivacaine and 40 mg of methylprednisolone. The patient reported a decrease in pain and improved range of motion within 6 weeks following the injection. Physical therapy was reinitiated 11 months after vaccination, and he regained near full range of motion over the following year. Follow-up radiographs (not shown) 32 months after the onset of symptoms demonstrated no further progression of erosive changes. He has received 3 subsequent annual influenza vaccinations without complication.
Discussion
Postvaccination injuries resulting in prolonged shoulder pain and dysfunction, as reported in our case, have been reported rarely in the medical literature. The first of these reported series described 2 patients who had received vaccinations “high into the deltoid muscle,”4 similar to our case, and the authors were the first to hypothesize that the “vaccine was injected into the subdeltoid bursa, causing a robust local immune and inflammatory response” that led to subacromial bursitis, bicipital tendonitis, and “inflammation of the shoulder capsule.” The authors concluded that “the upper third of the deltoid muscle should not be used for vaccine injections, and the diagnosis of vaccination-related shoulder dysfunction should be considered in patients presenting with severe or disabling shoulder pain following a vaccination.”
A subsequent report of a series of patients experiencing prolonged shoulder injury after vaccination5 postulated that the vaccine was inadvertently injected directly into the shoulder joint or bursa, where pre-existing antibody in the synovial tissues, present as a result of earlier naturally occurring infection or vaccination, could lead to a more prolonged inflammatory response.6,8 In our case, the vaccine was administered in a very proximal location, described by the patient as just distal (approximately 1 cm) to the lateral margin of the acromion, which might have been administered in an intrabursal or possibly intra-articular location in this lean patient.
Subsequently, there have been a few published case reports and small series for a total of 25 cases describing the MRI findings of prolonged postvaccination shoulder injury.5,9, 10, 11, 12, 13 Fourteen of the 25 cases documented the MRI findings of bursitis,5,12,14, 15, 16, 17, 18, 19 and 10 cases demonstrated bone marrow edema in the humeral head,5,10, 11, 12,14,16,18, 19, 20 8 of which followed influenza vaccination. Only 4 previous cases have demonstrated bone erosion on MRI after vaccination,10,11,19,20 3 of which followed influenza vaccination. The additional MRI findings in these prior reports included rotator cuff tendinosis and tendon tears.5,9,10,12,15,16,20 Our case is unique in that progressive erosive changes were demonstrated along with an increase in severity of changes suggesting bursitis, synovitis, and adhesive capsulitis on serial examinations over a 6-month period. In addition, subsequent stabilization of osseous erosions was evident on radiographic follow-up 32 months later, after the resolution of symptoms. The persistence of bone erosions demonstrated on subsequent radiographs obtained 32 months after the vaccination represents the longest duration of postvaccination imaging changes reported to-date. To our knowledge, there has been only one other documented case of refractory shoulder dysfunction with progressive erosive changes on MRI and CT following influenza vaccination.11 In that case, the patient did not respond well to conservative management, which included 2 ultrasound-guided intraarticular steroid injections and subsequent arthroscopic biopsy and debridement, with sampling of the posterior humeral head erosion. Analysis showed inflammatory destruction of the articular cartilage and bone, and marrow replacement by both fibrous and fibromyxoid tissue.
The current case uniquely illustrates nearly all of the previously reported postvaccine complications that have occurred around the shoulder, including osseous erosive changes of the humeral head, synovitis, bursitis, adhesive capsulitis, rotator cuff tendon injury, and tendinopathy. As in our case, the majority of previously reported vaccination-related and MRI-documented cases of shoulder injuries occurred in patients who reported that the injection was administered into the upper third of the deltoid. It has been well documented that vaccinations in this location pose a high risk for causing injury, particularly when injected at excessive depth or in a very thin patient, as the subdeltoid bursa extends an average of 4 cm distal to the tip of the acromion.4 Safe injection protocols emphasize proper patient positioning: abduction of the shoulder to 60 degrees by placing the hand on the ipsilateral hip, and locating the mid deltoid at the midpoint between the acromion and the deltoid tuberosity, which results in safe injection in the mid deltoid.21,22 In addition, selecting needle length appropriate for patient size minimizes the risk of intraarticular injection23 while maintaining a 90 degree angle between the needle and the skin. With proper attention to injection site, needle length, injection angle, and patient positioning, vaccination injection injuries are avoidable.
Conclusion
It is important for both clinicians and radiologists to be familiar with the possible severe or disabling complications that can arise from vaccine administration, especially when administered more proximally than is recommended in the upper third of the deltoid. The spectrum of imaging findings that can manifest in the shoulder include changes of adhesive capsulitis, erosive arthropathy, subacromial bursitis, and rotator cuff tendinopathy.
Acknowledgments
Coauthor Dean F. Leslie is the subject in this case report. The authors thank Sonia Watson, PhD, and Desiree Lanzino, PT, PhD, for their assistance in editing the manuscript. The Mayo Clinic Department of Radiology paid for the publication fees.
Footnotes
Potential Competing Interests: The authors report no competing interests.
Ethical approval: All procedures in studies involving human participants were in accordance with ethical standards of the institutional or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was waived.
References
- 1.Historical Reference of Seasonal Influenza Vaccine Doses Distributed. https://www.cdc.gov/flu/prevent/vaccinesupply.htm Available at:
- 2.2017-2018 Estimated Influenza Illnesses, Medical visits, and Hospitalizations Averted by Vaccination in the United States. https://www.cdc.gov/flu/vaccines-work/averted-estimates.htm Available at:
- 3.The Vaccine Adverse Event Reporting System (VAERS) https://wonder.cdc.gov/vaers.html Available at: [DOI] [PubMed]
- 4.Bodor M., Montalvo E. Vaccination-related shoulder dysfunction. Vaccine. 2007;25(4):585–587. doi: 10.1016/j.vaccine.2006.08.034. [DOI] [PubMed] [Google Scholar]
- 5.Atanasoff S., Ryan T., Lightfoot R., Johann-Liang R. Shoulder injury related to vaccine administration (SIRVA) Vaccine. 2010;28(51):8049–8052. doi: 10.1016/j.vaccine.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 6.Cooke T.D., Jasin H.E. The pathogenesis of chronic inflammation in experimental antigen-induced arthritis. I. The role of antigen on the local immune response. Arthritis Rheum. 1972;15(4):327–337. doi: 10.1002/art.1780150402. [DOI] [PubMed] [Google Scholar]
- 7.Gondim Teixeira P.A., Balaj C., Chanson A., Lecocq S., Louis M., Blum A. Adhesive capsulitis of the shoulder: Value of inferior glenohumeral ligament signal changes on T2-weighted fat-saturated images. AJR Am J Roentgenol. 2012;198(6):W589–W596. doi: 10.2214/AJR.11.7453. [DOI] [PubMed] [Google Scholar]
- 8.Cooke T.D., Hurd E.R., Ziff M., Jasin H.E. The pathogenesis of chronic inflammation in experimental antigen-induced arthritis. II. Preferential localization of antigen-antibody complexes to collagenous tissues. J Exp Med. 1972;135(2):323–338. doi: 10.1084/jem.135.2.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martin Arias L.H., Sanz Fadrique R., Sainz Gil M., Salgueiro-Vazquez M.E. Risk of bursitis and other injuries and dysfunctions of the shoulder following vaccinations. Vaccine. 2017;35(37):4870–4876. doi: 10.1016/j.vaccine.2017.07.055. [DOI] [PubMed] [Google Scholar]
- 10.Taylor B.C., Hinke D. Radiological case: Shoulder injury related to vaccine administration (SIRVA) Appl Radiol. 2014;December:30–31. [Google Scholar]
- 11.Erickson B.J., DiCarlo E.F., Brause B., Callahan L., Hannafin J. Lytic lesion in the proximal humerus after a flu shot: A case report. JBJS Case Connect. 2019;9(3):e0248. doi: 10.2106/JBJS.CC.18.00248. [DOI] [PubMed] [Google Scholar]
- 12.Hexter A.T., Gee E., Sandher D. Management of glenohumeral synovitis secondary to influenza vaccination. Shoulder Elbow. 2015;7(2):100–103. doi: 10.1177/1758573214560258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wright A., Patel R., Motamedi D. Influenza vaccine-related subacromial/subdeltoid bursitis: A case report. J Radiol Case Rep. 2019;13(6):24–31. doi: 10.3941/jrcr.v13i6.3656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuether G., Dietrich B., Smith T., Peter C., Gruessner S. Atraumatic osteonecrosis of the humeral head after influenza A-(H1N1) v-2009 vaccination. Vaccine. 2011;29(40):6830–6833. doi: 10.1016/j.vaccine.2011.07.052. [DOI] [PubMed] [Google Scholar]
- 15.Floyd M.W., Boyce B.M., Castellan R.M., McDonough E.B. Pseudoseptic arthritis of the shoulder following pneumococcal vaccination. Orthopedics. 2012;35(1):e101–e103. doi: 10.3928/01477447-20111122-31. [DOI] [PubMed] [Google Scholar]
- 16.Barnes M.G., Ledford C., Hogan K. A “needling” problem: Shoulder injury related to vaccine administration. J Am Board Fam Med. 2012;25(6):919–922. doi: 10.3122/jabfm.2012.06.110334. [DOI] [PubMed] [Google Scholar]
- 17.Uchida S., Sakai A., Nakamura T. Subacromial bursitis following human papilloma virus vaccine misinjection. Vaccine. 2012;31(1):27–30. doi: 10.1016/j.vaccine.2012.10.075. [DOI] [PubMed] [Google Scholar]
- 18.Okur G., Chaney K.A., Lomasney L.M. Magnetic resonance imaging of abnormal shoulder pain following influenza vaccination. Skeletal Radiol. 2014;43(9):1325–1331. doi: 10.1007/s00256-014-1875-9. [DOI] [PubMed] [Google Scholar]
- 19.Salmon J.H., Geoffroy M., Eschard J.P., Ohl X. Bone erosion and subacromial bursitis caused by diphtheria-tetanus-poliomyelitis vaccine. Vaccine. 2015;33(46):6152–6155. doi: 10.1016/j.vaccine.2015.09.090. [DOI] [PubMed] [Google Scholar]
- 20.Messerschmitt P.J., Abdul-Karim F.W., Iannotti J.P., Gobezie R.G. Progressive osteolysis and surface chondrolysis of the proximal humerus following influenza vaccination. Orthopedics. 2012;35(2):e283–e286. doi: 10.3928/01477447-20120123-26. [DOI] [PubMed] [Google Scholar]
- 21.Cook I.F. Subdeltoid/subacromial bursitis associated with influenza vaccination. Hum Vaccin Immunother. 2014;10(3):605–606. doi: 10.4161/hv.27232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cook I.F. An evidence based protocol for the prevention of upper arm injury related to vaccine administration (UAIRVA) Hum Vaccin. 2011;7(8):845–848. doi: 10.4161/hv.7.8.16271. [DOI] [PubMed] [Google Scholar]
- 23.Poland G.A., Borrud A., Jacobson R.M., et al. Determination of deltoid fat pad thickness. Implications for needle length in adult immunization. JAMA. 1997;277(21):1709–1711. [PubMed] [Google Scholar]