Abstract
Introduction
There has been an exponential increase in referrals for transmasculine patients seeking genital affirmation surgery. Despite transgender men’s equal interest in metoidioplasty and phalloplasty, research has primarily focused on phalloplasty.
Aim
To summarize and investigate the relationship between surgical technique, complications, and patient-satisfaction.
Methods
We performed a systematic review and meta-analysis of surgical techniques and physician- and patient-reported outcomes of gender-affirming clitoral release and metoidioplasty (PROSPERO# 158722) with literature from PubMed, Google Scholar, and ScienceDirect. Data were extracted using PRISMA guidelines. All searches, extractions, and grading were independently completed by 2 authors.
Main Outcome Measures
Main measures were surgical technique, patient satisfaction, voiding, urethral stricture, and urethral fistula.
Results and Conclusion
A total of 7 non-overlapping articles on metoidioplasty were identified, with a total of 403 patients. We identified 4 metoidioplasty techniques: Hage, Belgrade, labial ring flap, and extensive metoidioplasty. All techniques included urethral lengthening. The reported neophallus length ranged from 2 cm to 12 cm, with the smallest neophallus occurring with the labial ring flap technique and extensive metoidioplasty the largest. Across techniques, voiding while standing was reported in most patients, with the lowest rate reported with the labial ring flap (67%). Complications were impacted by surgical technique, with the lowest rates of fistula and stricture occurring with the Belgrade technique. Fistula rates ranged from 5% to 37%, while stricture ranged from 2% to 35% of patients. The Belgrade technique reported significantly lower rates of fistula and stricture (P = .000). The patient-reported outcomes were described for the Belgrade technique and extensive metoidioplasty. Both techniques showed high aesthetic and sexual satisfaction. Transgender individuals can achieve an aesthetically and sexually satisfactory neophallus using a variety of metoidioplasty techniques; however, urethral outcomes vary significantly by technique. The Belgrade technique reported the best outcomes, although data remains limited. Patient priorities should be used to determine surgical technique.
Jolly D, Wu CA, Boskey ER, et al. Is Clitoral Release Another Term for Metoidioplasty? A Systematic Review and Meta-Analysis of Metoidioplasty Surgical Technique and Outcomes. Sex Med 2021;9:100294
Key Words: Transsexualism, Metoidioplasty, Transgender Persons, Gender Affirmation Surgery, Transition, Urethral Lengthening, Urethroplasty
Introduction
Many transgender individuals seek gender affirmation surgery as part of their transition. Rates of referral to gender clinics have exponentially increased over time, particularly following expanded coverage for gender affirming care under the Affordable Care Act,1 with the growing number of surgeons offering different types of procedures.2 Surgeons have also begun to offer less conventional genital affirmation such as zero-depth vaginoplasty and clitoral release without urethral lengthening.3 For transmasculine individuals, the 2 standard options for genital affirmation remain phalloplasty and metoidioplasty.4 However, some transmasculine patients request alternative options for genital affirmation ranging from phalloplasty without urethral lengthening to the poorly defined “clitoral release.”
In the context of growing interest and options for masculine genital surgery, there is a need for an improved evidence base to inform decision-making. Despite metoidioplasty and phalloplasty being performed on transgender men at roughly equal rates,5 research has focused on outcomes and techniques of phalloplasty.6 While metoidioplasty techniques have been described by many authors,7,8 there has been no thorough evaluation of the aesthetic and functional outcomes of each surgical approach. This systematic review and meta-analysis of metoidioplasty and clitoral release techniques was designed to bring attention to the variety of options for masculinizing genital surgery beyond phalloplasty and to compare the outcomes of such procedures in greater detail than has been previously addressed in the literature. Specifically, we investigated the questions: what clitoral release techniques performed with transgender men have been described in the literature, and what is the relationship between surgical technique, complications, and patient-satisfaction?
Materials and methods
A systematic search was conducted in October 2019 using a combination of keywords related to clitoral release and metoidioplasty using multiple databases, searching different areas of the literature to avoid selection bias. Searched databases were PubMed, Google Scholar, and ScienceDirect. Databases were searched from inception through October 2019. No funding was utilized. In accordance with PRISMA-P 2015 guidelines,9 this protocol was registered in PROSPERO (registration number 158722). The search strategy investigated the PICOS: within all types of peer-reviewed studies written in the English language (S), how does surgical technique (C) impact physician- and patient-reported outcomes and satisfaction (O) among transgender men (P) seeking gender-affirming procedures involving excision of the suspensory clitoral ligaments (I)? The primary outcomes of interest were the proportion of patients who were able to void while standing and the proportions of patients who experienced urethral stricture and fistula, respectively. Search terms were derived from a combination of scoping searches and expert-knowledge of the field. Terms included combinations of terms for the clitoris, transgender, and metoidioplasty (eg, in PubMed, (“clitoris” [MeSH Terms] OR “clitoris” [All Fields]) AND (“transgender persons” [MeSH Terms] OR (“transgender” [All Fields] AND “persons” [All Fields]) OR (“transgender persons” [All Fields]) OR (“transgender” [All Fields]) OR (“transgendered” [All Fields]) OR (“transgenders” [All Fields]) AND (“metoidioplasty” [All Fields]). Identical searches were completed in all searched databases. All searches, screenings, and extractions were completed by 2 authors to account for individual bias.
Upon completion of the primary search, duplicates were removed, and a first screening was completed using the titles and abstracts of all identified articles. Articles were included for a full-text screening if they discussed clitoral release and mentioned gender-affirmation or being transgender. A full-text screening was then completed with all articles that passed the first screening. Included articles were all English-language, peer-reviewed, primary data sources that included the release of the clitoral chorda for transgender individuals seeking gender affirmation surgery. There were no restrictions on minimum follow-up time nor on the quality of the literature due to the paucity of the literature. Articles were excluded if they were review articles, not about gender affirmation, focused on revisions to failed procedures, did not differentiate complications between transgender and cisgender men, contained data that were already published in an included study, or were about phalloplasty following metoidioplasty. References from any review articles identified were hand-searched to ensure that all possible publications were identified.
Extracted information regarding surgical technique included general study information, sample size, age, number of stages, whether urethral lengthening was included, and flap types used. The physician-reported outcomes included length of neophallus, whether voiding while standing was achieved, urethral complications, and other complications. The patient-reported outcomes included overall satisfaction, aesthetic satisfaction, and sexual satisfaction. The quality of evidence for all primary outcomes of interest was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system.10 Risk of individual bias at the study level was assessed through the use of the Murad et al11 tool for case series as no included study contained a control group for comparison. All data were extracted independently from the included full-text articles by 2 authors. Upon completion of data extraction by both authors, the extracted data were compared; any conflicts in the extracted data were resolved through a review from a third author. Extracted information has been qualitatively summarized in the tables below where possible. All complications are described with both the raw number and proportion of patients in the study sample. 3 meta-analyses were performed upon completion of the systematic review through random-effects modeling to determine if surgical technique impacted the proportion of patients who were able to void while standing and proportions of urethral stricture and fistula, respectively. Random effects modeling was used to account for potentially confounding factors such as variation in technique within a given study. All studies included in the systematic review were included in the meta-analysis as they included data on urethral stricture and fistula. One study was excluded from the voiding meta-analysis for lack of reported data. The alpha level was set at 0.05. Measures of consistency have been provided through I2 for all meta-analyses. All quantitative data were analyzed in Stata 16 (Statacorp LLC, 2019, College Park, TX, USA).
Results
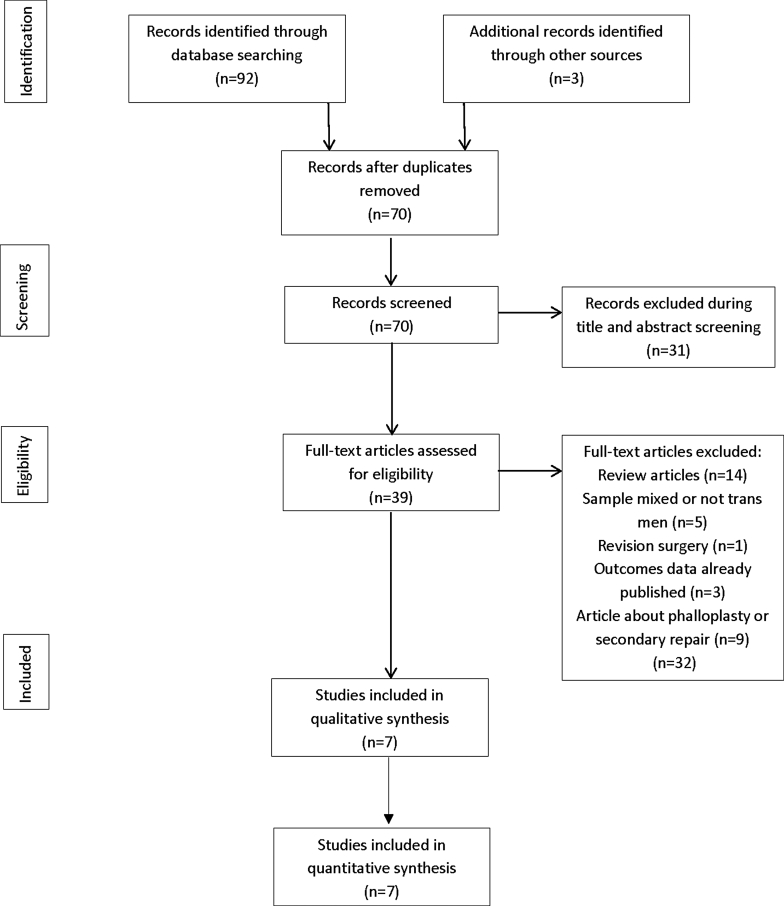
95 articles, 70 of which were not duplicates, were initially identified from searching titles and abstracts (Figure 1). Following identification, a first screening was completed to exclude all papers that did not mention metoidioplasty or gender-affirming clitoral release in the title or abstract. A second round of screening was conducted using the full-text articles to find a total of 11 articles with primary data related to clitoral release and metoidioplasty procedures for 403 patients. All articles primarily pertained to metoidioplasty, with only 1 mentioning clitoral release,12 even peripherally. Of the 11 identified articles, 3 were excluded for overlapping data with other included studies,13, 14, 15 and 1 was excluded for being a revision surgery,16 leaving a total of 7 primary articles for extraction. In all cases where there was overlapping data, the most recent article was used for abstraction. All identified studies were observational cohort studies with no control group (eg, case series) (Table 1). The risk of bias varied widely within individual studies from low to high.
Figure 1.
PRISMA flow diagram for study selection.
Table 1.
Summary characteristics and risk of bias (Murad et al tool) for all included studies
| Authors | Year | Technique | Sample type | Dates of study | Sample age | Follow-up time (in months) | Risk of individual bias |
|---|---|---|---|---|---|---|---|
| Vukadinovic et al.20 | 2014 | Belgrade | Prospective cohort | March 2008–January 2013 | 29 (18–41) | 30 | Low; study represents the whole experience of the center during the study period, has adequate follow-up time, clearly describes outcomes, and provides sufficient details about outcomes of interest. |
| Djordjevic et al.19 | 2009 | Belgrade | Retrospective cohort | September 2002–April 2007 | 31 (18–54) | 32 (14–69) | Low; study represents the whole experience of the center during the study period, has adequate follow-up time, clearly describes outcomes, and provides sufficient details about outcomes of interest. |
| Perovic and Djordjevic18 | 2003 | Belgrade | Retrospective cohort | September 1995–April 2002 | 26.2 (18–33) | 47 (6–72) | Moderate; study represents the whole experience of the center during the study period, has adequate follow-up time, describes the outcomes of interest but does not provide sufficient detail about management nor severity of complications. |
| Stojanovic et al.21 | 2017 | Belgrade | Retrospective cohort | January 2007–March 2016 | 31.5 (18–43) | 44 (10–92) | Low; study represents the whole experience of the center during the study period, has adequate follow-up time, clearly describes outcomes, and provides sufficient details about outcomes of interest. |
| Takamatsu and Harashina12 | 2009 | Labial ring flap | Retrospective cohort– | 2005–2007 | 18–33 | 7 (3–96) | Moderate; study represents the whole experience of the center during the study period, clearly describes outcomes and provides sufficient details about the outcomes of interest but does not have a sufficient follow-up time to adequately assess for complications |
| Cohanzad22 | 2016 | Extensive | Retrospective cohort– | 2007–2014 | 28 (20–40) | 68 ± 15 | High; while the follow-up period is adequate, the study has a small sample and only reports on outcomes for a small subsect of the already small sample with a poor description of outcomes |
| Hage and Van Turnhout17 | 2006 | Hage | Retrospective cohort | December 1991–March 1999 | 30 (19–53) | 96 (54–132) | Low; study represents the whole experience of the center during the study period, has adequate follow-up time, clearly describes outcomes, and provides sufficient details about outcomes of interest. |
Surgical Technique
Several surgical techniques for metoidioplasty were identified (Table 1). No specific techniques for clitoral release were identified. The Hage technique was the first metoidioplasty technique developed.15 All patients received masculinizing hormone therapy for a minimum of 1.2 years prior to surgery.17 Hysterectomy was completed as a preparatory surgery or during metoidioplasty. This technique refined existing hypospadias methods to create a new single-stage approach for masculinizing gender confirmation (Table 2), using local tissue rearrangements from the vaginal wall, release of the clitoral shaft, and recreating the neourethra.
Table 2.
Summary and surgical characteristics with complications and physical outcomes for all included studies
| Authors | Year | Technique | Sample size | Follow-up time (in months) | Single stage | Urethral lengthening | Vaginectomy | Urethral plate release | Buccal mucosa graft | Labia minora flap | Dorsal clitoral flap | Labial ring flap | Vaginal flap | Length of neophallus (cm) Mean (range) |
Voiding while standing, n(%) | Urethral fistula, n(%) | Urethral stricture, n(%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Vukadinovic et al.20 | 2014 | Belgrade | 97 | 30 | 97 | 97 | 97 | 97 | 97 | 97 | - | - | - | 7 (range not specified) | 97 (100) | 6 (6.2) | 2 (2.1) |
| Djordjevic et al.19 | 2009 | Belgrade | 82 | 32 (14–69) | 82 | 82 | 82 | 82 | 82 | 82 | - | - | 5.7 (4–10) | 82 (100) | 7 (8.5) | 2 (2.4) | |
| Perovic and Djordjevic18 | 2003 | Belgrade | 22 | 47 (6–72) | 22 | 22 | 22 | 22 | - | - | 22 | - | - | 5.7 (4–10) | 22 (100) | 3 (14.2) | 2 (9.1) |
| Stojanovic et al.21 | 2017 | Belgrade | 79 | 44 (10–92) | 79 | 79 | 79 | 79 | 79 | 79 | - | - | - | 6.8 (5–9.8) | 79 (100) | 4 (5.1) | 3 (3.8) |
| Takamatsu and Harashina12 | 2009 | Labial ring flap | 43 | 7 (3 – 96) | 43 | 43 | 7 | - | - | - | 43 | - | 2–5 (mean not specified) | +VC: 5 (71.43) No VC: 24 (66.67) |
+VC: 1 (14.3) No VC: 11 (30.6) |
+VC: 1 (14.3) No VC: 2 (28.6) |
|
| Cohanzad22 | 2016 | Extensive | 10 | 68 ± 15 | 10 | 2 | - | - | - | 2 | - | - | - | 8.7 (6–12) | 2 (100) | - | - |
| Hage and Van Turnhout17 | 2006 | Hage | 70 | 96 (54–132) | 70 | 70 | 70 | - | - | 70 | - | - | 70 | - | - | 26 (37.1) | 25 (35.7) |
Similar to the Hage technique, the Belgrade technique employed a single-stage procedure with a presurgical masculinizing hormone regimen and hysterectomy either at the time of the procedure or before.18, 19, 20, 21 Colpocleisis, removing all vaginal mucosa except for part of the ventral wall, which is preserved for urethral lengthening, was performed first. The ventral chordae and clitoral ligaments were released to straighten and lengthen the clitoris. Urethral lengthening was completed with a combination of local flaps (Table 2), with later refinements of the technique favoring a combination of buccal mucosa graft and labia minora flaps.13
Later refinements to the technique added an additional step to induce clitoral enlargement through twice-a-day dihydrotestosterone topical gel application for 3 months preoperatively in combination with vacuum device created from 2 syringes joined with a silicon tube.19 The Belgrade technique has also recently been performed in combination with other gender confirmation surgeries such as masculinizing chest reconstruction.21
Labial ring flap metoidioplasty was developed to account for cases of poor development of the labia minora, clitoral body, or narrow vagina.12 A small circle was designed around the urethral meatus and vaginal opening to create a labial ring. The clitoris was then straightened and lengthened, an anterior vaginal flap was joined to the ring flap to create the neourethra, where the lateral surfaces of the labia minora were sutured together to complete the creation of the phallus.
Cohanzad describes an alternative technique, known as “extensive metoidioplasty,” to provide a more masculine-appearance than that of “conventional” metoidioplasty (eg, Hage or Belgrade).22 All patients were on masculinizing hormones for between 3 months to 1 year prior to surgery. This technique involves extensive dissection of the crura to near-total detachment from the pubic bone to provide additional length. The labia minora were tubularized to create the neourethra, with no anastomosis to the native urethra in the first stage. At the 6-week mark, patients were fit for a penile enhancement protocol that was used post-operatively for at least a year to further increase the size of the neophallus.23 All cases who did not have urethroplasty at the time of metoidioplasty had it performed in a second stage.
Patient-Reported Outcomes
There was no consistency in how patient-reported outcomes were measured across studies, so outcomes could not be tabulated. The patient-reported outcomes were not provided for the labial ring flap or the Hage technique. Where reported, the patient-reported outcomes pertained to aesthetic and sexual outcomes. Among the 280 Belgrade cases where outcomes were assessed, most cases reported being satisfied with their genitals after surgery. Aesthetic satisfaction was high, with 96% reporting complete (83.5) or partial satisfaction (12.3).20 All reported cases could achieve an erection, but the size of the erection was not sufficient for penetration. Erogenous sensation, quality of erection, and arousal following surgery were completely satisfactory to all patients.21 With extensive metoidioplasty, 70 percent of patients were able to achieve an erection large and rigid enough for penetration of a partner.22 All patients reported being completely satisfied with the appearance of their genitals.
Physician-Reported Outcomes
Physician-reported outcomes for this analysis included complications, the ability to void while standing, and neophallus length. Neophallus lengths ranged from 2 centimeters to 12 centimeters, with most being between 5 to 7 centimeters. Extensive metoidioplasty produced the greatest length, while the labial ring flap technique produced the smallest. The length of the neophallus was not described for the Hage technique (Table 2).
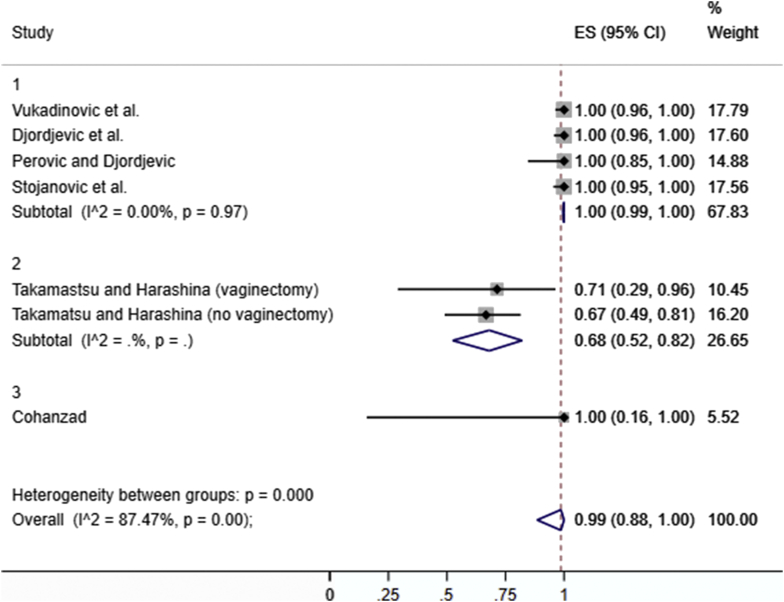
Voiding while standing was achieved among all patients who had metoidioplasty with the Belgrade technique and extensive metoidioplasty. The labial ring technique produced a phallus that was capable of voiding while standing in two-thirds of patients who did not have vaginectomy and 71% of those who did have vaginectomy. Voiding was not described for the Hage technique. There is very low-quality evidence evaluating the proportion of patients who can void while standing (Table 3). Meta-analysis indicated minimal within-group heterogeneity (I2 = 0.00%), with high rates of between-group heterogeneity (I2 = 87.47%, P = .000) (Figure 2), suggesting significant differences by technique.
Table 3.
Quality of Evidence (GRADE) for all physician-reported outcomes
| Outcomes | Number of participants | Quality of the evidence (GRADE) | Proportion of patients overall with outcome (95% CI) |
|---|---|---|---|
| Urethral Stricture | 395 | ++; Low due to inadequate follow-up of labial ring flap and high overall heterogeneity | .08 (.01–.18) |
| Urethral Fistula | 395 | ++; Low due to inadequate follow-up of labial ring flap and high overall heterogeneity | .14 (.06–.26) |
| Voiding | 325 | +; Very low due to inadequate follow-up of labial ring flap, missing data from Hage | .99 (.88–1.00) |
Figure 2.
Forest plot of the patients who were able to void while standing for the identified techniques.
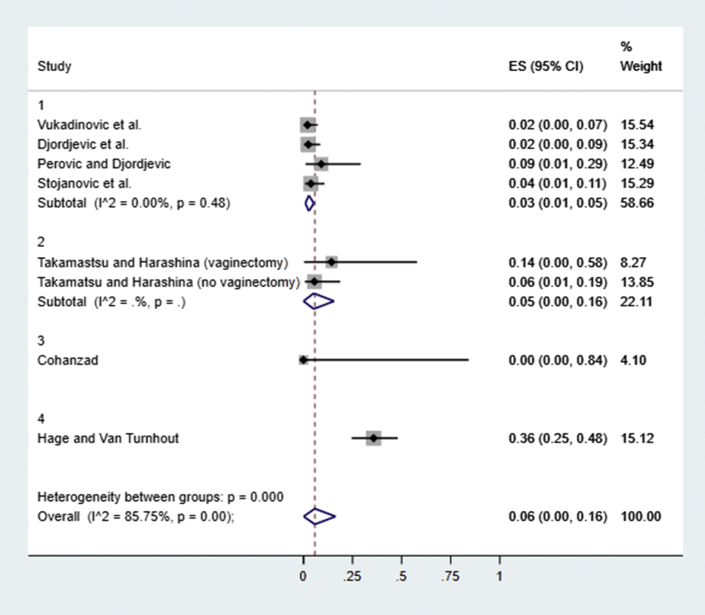
A meta-analysis of urethral stricture by surgical technique yielded very low rates of within-group heterogeneity (I2 = 0.00%), with high rates of between-group heterogeneity (I2 = 85.75%, P = .000), indicating significant differences in stricture by surgical technique (Figure 3). The Belgrade technique yielded the lowest rates of stricture, occurring in about 3% (95% CI: 1–5, reported range: 2.1–9.1) of all patients (Table 2). The labial ring flap technique yielded stricture among 5% (95% CI: 0–16, reported range: 14.3–28.6) of patients. Stricture occurred in 36% (95% CI: 25–48) of metoidioplasties performed with the Hage technique. Extensive metoidioplasty reported no urethral stricture; however, the urethral extension was only completed in 2 patients, and thus, the true proportion may fall between 0% and 84% of patients. These data suggest limited, low-quality evidence that the Belgrade technique may have the lowest rate of urethral stricture (Table 3).
Figure 3.
Forest plot of the patients who experienced urethral stricture for the identified techniques.
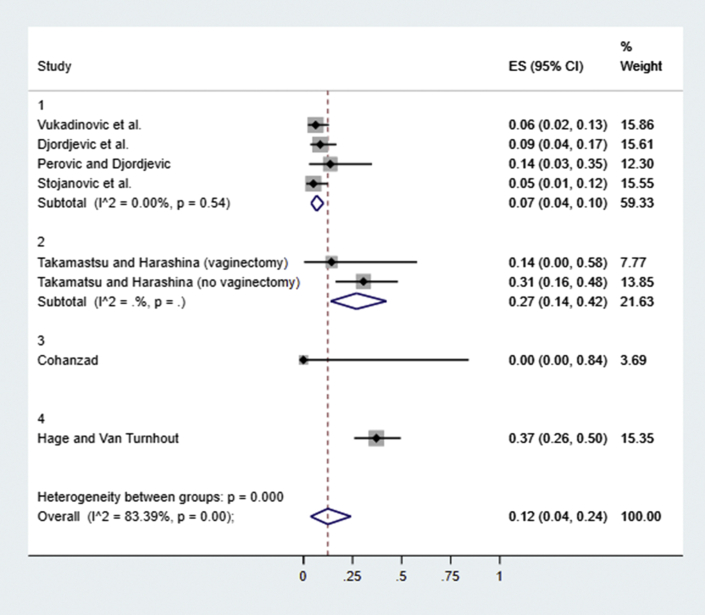
Similarly, meta-analysis of urethral fistula indicated no detectable within-group heterogeneity (I2 = 0.00%) and high between-group heterogeneity (I2 = 85.74%, P = .000), suggesting significant differences in rates of urethral fistulae by surgical technique (Figure 4). Among the analyzed techniques, the Belgrade technique yielded the lowest rates of urethral fistula, which occurred in approximately 7% (95% CI: 4–10, reported range: 5.1–14.2) of patients. Other techniques had significantly higher rates of fistula, occurring in about 27% (95% CI: 14–42, reported range: 14.3–30.6) and 37% (95% CI: 26–50) of transgender men who had metoidioplasty with the labial ring flap and Hage techniques, respectively. No fistulae were reported with extensive metoidioplasty, but the limited sample size (n = 2) makes it difficult to ascertain the true proportion of fistulae occurring with this technique (95% CI: 0–84). As with urethral stricture, there is limited, low-quality evidence to suggest that the Belgrade technique may yield lower rates of urethral fistula among identified techniques of masculinizing metoidioplasty.
Figure 4.
Forest plot of the patients who experienced urethral fistula for the identified techniques.
Discussion
There is limited, very low to low-quality evidence suggesting that metoidioplasty can be a good option for genital affirmation in transmasculine patients who are seeking to void while standing but who are not concerned about phallus size or penetrating a partner. Our search suggests that there are a variety of metoidioplasty techniques that may be used to produce functional genitals with a satisfactorily masculine appearance. Nearly all identified procedures involved urethral lengthening, and all included other procedures that fall under the definition of metoidioplasty. To our knowledge, no stand-alone procedure for clitoral release has been described in the literature, although at least 1 surgeon mentions it in their online advertising,24 and multiple patients have requested it in isolation at our clinic. Therefore, despite the fact that in the literature, “clitoral release” is synonymous with metoidioplasty, in clinical practice, it is not. Indeed, patients asking for clitoral release may specifically want to avoid the urologic procedures integral to metoidioplasty in order to reduce complication rates. Thus, it is critical that providers are aware of the potential ambiguity of the term.
Complications and functional outcomes of metoidioplasty appear to be significantly impacted by the technique used for the procedure. The limited published literature suggests the Belgrade technique produces a masculine neophallus that allows most, if not all, patients to void while standing, with low complication rates and high patient satisfaction.20 These findings were supported by the results of our meta-analysis, which suggested the lowest rates of urethral stricture and fistula occur with the Belgrade technique. It is possible that such a difference is the result of using the buccal mucosa that reduces the tension on the urethral plate and is similar to naturally occurring urethral mucosa.25 However, high rates of patient satisfaction and low rates of complications were not limited to the Belgrade technique; no patients who underwent extensive metoidioplasty reported urethral complications, all reported high rates of aesthetic satisfaction, and most reported the ability to penetrate a partner,22 suggesting that extensive metoidioplasty may provide a viable, safe alternative to the Belgrade technique. In addition, despite having a higher rate of urethral complications and a reduced rate of voiding while standing compared to other described techniques, the labial ring flap technique still produced a satisfactory result among most patients.12 As the labial ring flap is intended to be used with patients with poorly developed labia minora, such as the Japanese population for which it was developed, it may serve as an important alternative technique. Furthermore, due to the relatively minor differences in urethral construction across the identified techniques as described in the Results, it is possible that a factor other than surgical technique influenced the significant differences seen with urethral complications.
Limitations
These findings should be interpreted as preliminary. 2 of the 3 of the included studies examining techniques other than Belgrade were at moderate to high risk of bias, with small sample sizes and short follow-up times. As reported in other studies, such data concerns can skew analytic results.26,27 In addition, over half of the articles identified were published by the Serbian authors who pioneered and refined the Belgrade technique. The high volume of papers published with the same authors may have influenced the results of this analysis, as might the fact that those authors report on substantially more cases than seen in other studies. Numerous analyses, across surgical procedures, have suggested that experience with a technique is correlated with decreased complication rates, and so the reduced complication rates seen among the Belgrade patients may well reflect high surgical volume rather than factors directly related to technique.28,29 Additionally, as the Serbian authors also see a number of international patients, the follow-up time for individual patients may have been shorter than the total time reported in the studies, as some patients may have returned to their homes, thus reducing the rates of complications reported. As all of the reports were based on the experiences of single surgical teams, it was impossible to differentiate whether outcome differences were the result of the technique or the skills and experience of the involved surgeons. The high rate of overall heterogeneity in the data limits the quality of evidence.
Conclusion
This review provides evidence in support of metoidioplasty as a safe, satisfactory option for genital affirmation in transmasculine patients who are seeking the procedure. Providers offering metoidioplasty should be aware of potential urethral complications such as stricture and fistula that are relatively common with this procedure. Counseling about how urethral complications may affect both short- and long-term recovery is therefore critical. The results of our analysis provide the beginnings of an evidence-base for clinicians to make data-driven clinical decisions around technique and flap choice. However, further research is clearly needed in order to more accurately compare complication rates across surgical procedures and flap types.
Surgeons planning to offer metoidioplasty and/or “clitoral release” should be aware of the variety in language that patients may use to request genital affirmation procedures and be certain to clarify individuals’ goals and desires. It is important to look beyond language to identify clear surgical goals with the patient so that an ideal surgical course can be identified. In particular, it is important for surgeons to be aware that there is not an established meaning for the term “clitoral release,” and patients seeking “clitoral release” may or may not be interested in various components of a metoidioplasty, such as urethral lengthening or scrotoplasty. There is a need for further research to understand the diversity of goals patients have for these procedures, as well as the intersection between technique and patient-reported outcomes.
Statement of authorship
Divya Jolly: Writing - Original Draft, Formal Analysis, Conceptualization, Methodology, Investigation, Resources, Writing - Review & Editing, Funding Acquisition, Project Administration, Writing - Conceptualization; Catherine A. Wu: Writing - Original Draft, Formal Analysis, Conceptualization, Methodology, Investigation, Resources, Writing - Review & Editing, Funding Acquisition, Project Administration; Elizabeth R. Boskey: Writing - Original Draft, Formal Analysis, Conceptualization, Methodology, Investigation, Resources, Writing - Review & Editing, Funding Acquisition, Project Administration, Writing - Conceptualization; Amir H. Taghinia: Conceptualization, Methodology, Investigation, Resources, Writing - Review & Editing, Funding Acquisition, Resources, Writing - Conceptualization; David A. Diamond: Conceptualization, Methodology, Investigation, Resources, Writing - Review & Editing, Funding Acquisition, Writing - Conceptualization; Oren Ganor: Conceptualization, Methodology, Investigation, Resources, Writing - Review & Editing, Funding Acquisition, Writing - Original Draft, Formal Analysis, Project Administration, Writing - Conceptualization.
Footnotes
Conflict of Interest: The authors report no conflicts of interest.
Funding: None.
References
- 1.Canner J.K., Harfouch O., Kodadek L.M. Temporal Trends in gender-affirming surgery among transgender patients in the United States. JAMA Surg. 2018;153:609–616. doi: 10.1001/jamasurg.2017.6231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Colebunders B., Brondeel S., D’Arpa S. An Update on the surgical Treatment for transgender patients. Sex Med Rev. 2017;5:103–109. doi: 10.1016/j.sxmr.2016.08.001. [DOI] [PubMed] [Google Scholar]
- 3.Jiang D., Witten J., Berli J. Does depth Matter? Factors affecting choice of Vulvoplasty over vaginoplasty as gender-affirming genital surgery for transgender Women. J Sex Med. 2018;15:902–906. doi: 10.1016/j.jsxm.2018.03.085. [DOI] [PubMed] [Google Scholar]
- 4.Hadj-Moussa M., Agarwal S., Ohl D.A., Kuzon W.M. Masculinizing Genital Gender Confirmation Surgery. Sex Med Rev. 2019;7:141–155. doi: 10.1016/j.sxmr.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 5.James S.E., Herman J.L., Rankin S. National Center for Transgender Equality; Washington, DC: 2016. The report of the 2015 U.S. Transgender Survey. [Google Scholar]
- 6.Frey J.D., Poudrier G., Chiodo M.V. A systematic review of metoidioplasty and Radial Forearm flap phalloplasty in female-to-male transgender genital reconstruction: is the “ideal” neophallus an achievable goal? Plast Reconstr Surg Glob Open. 2016;4:e1131. doi: 10.1097/GOX.0000000000001131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bizic M.R., Stojanovic B., Joksic I. Metoidioplasty. Urol Clin North Am. 2019;46:555–566. doi: 10.1016/j.ucl.2019.07.009. [DOI] [PubMed] [Google Scholar]
- 8.Djordjevic M.L., Stojanovic B., Bizic M. Metoidioplasty: techniques and outcomes. Transl Androl Urol. 2019;8:248–253. doi: 10.21037/tau.2019.06.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moher D., Shamseer L., Clarke M. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guyatt G., Oxman A.D., Akl E.A. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 11.Murad M.H., Sultan S., Haffar S. Methodological quality and synthesis of case series and case reports. BMJ Evid-based Med. 2018;23:60–63. doi: 10.1136/bmjebm-2017-110853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Takamatsu A., Harashina T. Labial ring flap: a new flap for metaidoioplasty in female-to-male transsexuals. J Plast Reconstr Aesthet Surg JPRAS. 2009;62:318–325. doi: 10.1016/j.bjps.2008.11.038. [DOI] [PubMed] [Google Scholar]
- 13.Djordjevic M.L., Bizic M.R. Comparison of two different methods for urethral lengthening in female to male (metoidioplasty) surgery. J Sex Med. 2013;10:1431–1438. doi: 10.1111/jsm.12108. [DOI] [PubMed] [Google Scholar]
- 14.Djordjevic M.L., Bizic M., Stanojevic D. Urethral Lengthening in metoidioplasty (female-to-male sex reassignment surgery) by combined buccal mucosa graft and labia minora flap. Urology. 2009;74:349–353. doi: 10.1016/j.urology.2009.02.036. [DOI] [PubMed] [Google Scholar]
- 15.Hage J.J. Metaidoioplasty: an alternative phalloplasty technique in transsexuals. Plast Reconstr Surg. 1996;97:161. doi: 10.1097/00006534-199601000-00026. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt M., Grohmann M., Huemer G.M. Pedicled superficial inferior epigastric artery perforator flap for salvage of failed metoidioplasty in female-to-male transsexuals. Microsurgery. 2015;35:403–406. doi: 10.1002/micr.22361. [DOI] [PubMed] [Google Scholar]
- 17.Hage J.J., Van Turnhout A.A.W.M. Long-term outcome of metaidoioplasty in 70 female-to-male transsexuals. Ann Plast Surg. 2006;57:312–316. doi: 10.1097/01.sap.0000221625.38212.2e. [DOI] [PubMed] [Google Scholar]
- 18.Perovic S.V., Djordjevic M.L. Metoidioplasty: a variant of phalloplasty in female transsexuals. BJU Int. 2003;92:981–985. doi: 10.1111/j.1464-410x.2003.04524.x. [DOI] [PubMed] [Google Scholar]
- 19.Djordjevic M.L., Stanojevic D., Bizic M. Metoidioplasty as a single stage sex reassignment surgery in female transsexuals: Belgrade experience. J Sex Med. 2009;6:1306–1313. doi: 10.1111/j.1743-6109.2008.01065.x. [DOI] [PubMed] [Google Scholar]
- 20.Vukadinovic V., Stojanovic B., Majstorovic M. The role of clitoral anatomy in female to male sex reassignment surgery. ScientificWorldJournal. 2014;2014:437378. doi: 10.1155/2014/437378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stojanovic B., Bizic M., Bencic M. One-stage gender-confirmation surgery as a viable surgical procedure for female-to-male transsexuals. J Sex Med. 2017;14:741–746. doi: 10.1016/j.jsxm.2017.03.256. [DOI] [PubMed] [Google Scholar]
- 22.Cohanzad S. Extensive metoidioplasty as a technique capable of creating a Compatible Analogue to a natural Penis in female transsexuals. Aesthet Plast Surg. 2016;40:130–138. doi: 10.1007/s00266-015-0607-4. [DOI] [PubMed] [Google Scholar]
- 23.Cohanzad S. Penile Improvement protocol in Postoperative Management of patients Undergoing metoidioplasty. Aesthet Plast Surg. 2016;40:947–953. doi: 10.1007/s00266-016-0700-3. [DOI] [PubMed] [Google Scholar]
- 24.GrS Montreal | Metaiodoplasty. GRS Montr n.d. https://www.grsmontreal.com/en/surgeries/female-to-male/12-metaiodoplasty.html Available at:
- 25.Tabassi K.T., Rana T.M. Tubularized Incised plate urethroplasty using buccal mucosa graft for Repair of penile hypospadias. Urol J. 2012;9:514–521. [PubMed] [Google Scholar]
- 26.Moher D., Pham B., Jones A. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? The Lancet. 1998;352:609–613. doi: 10.1016/S0140-6736(98)01085-X. [DOI] [PubMed] [Google Scholar]
- 27.Sterne J.A.C., Gavaghan D., Egger M. Publication and related bias in meta-analysis: Power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000;53:1119–1129. doi: 10.1016/s0895-4356(00)00242-0. [DOI] [PubMed] [Google Scholar]
- 28.Mahmoudi E., Lu Y., Chang S.-C. The Associations of Hospital volume, surgeon volume, and surgeon experience with complications and 30-day Rehospitalization after free tissue Transfer: a National population study. Plast Reconstr Surg. 2017;140:403–411. doi: 10.1097/PRS.0000000000003515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Naveiro-Fuentes M., Rodríguez-Oliver A., Fernández-Parra J. Effect of surgeon’s experience on complications from laparoscopic hysterectomy. J Gynecol Obstet Hum Reprod. 2018;47:63–67. doi: 10.1016/j.jogoh.2017.11.004. [DOI] [PubMed] [Google Scholar]