Abstract
Neuropilin-1 is a transmembrane glycoprotein that has been implicated in several processes including angiogenesis and immunity. Recent evidence has also shown that it is implied in the cellular internalization of the severe acute respiratory syndrome coronavirus (SARS-CoV-2), which causes the coronavirus disease 2019 (COVID-19). We hypothesized that specific microRNAs can target Neuropilin-1. By combining bioinformatic and functional approaches, we identified miR-24 as a regulator of Neuropilin-1 transcription. Since Neuropilin-1 has been shown to play a key role in the endothelium-mediated regulation of the blood-brain barrier, we validated miR-24 as a functional modulator of Neuropilin-1 in human brain microvascular endothelial cells (hBMECs), which are the most suitable cell line for an in vitro blood–brain barrier model.
Keywords: ACE2, Akt, blood–brain barrier, brain, coronavirus, CD304, COVID-19, endothelium, epigenetics, hBMEC, microRNA, miR-24-3p, neurology, non-coding RNA, NRP1, SARS-CoV-2, vascular permeability, VEGF, VEGF165R
1. Introduction
Neuropilins are single-pass transmembrane, non-tyrosine kinase surface glycoproteins that are expressed in all vertebrates with versatile roles in a wide range of physiological processes including angiogenesis, immunity, development, and axonal guidance [1,2,3,4,5]. The family includes two homologous isoforms, Neuropilin-1 and Neuropilin-2, encoded by distinct genes on different chromosomes (10p12 and 2q34, respectively) [6]. Both isoforms are upregulated in a number of clinical disorders, including cancer, where they increase the oncogenic activities of malignant cells by promoting survival, inducing angiogenesis and lymphangiogenesis, and contribute to therapy resistance [7]. Neuropilin-1 has been shown to regulate the endothelium-dependent inflammatory responses at the level of the blood–brain barrier [8].
MicroRNAs (miRNAs, miRs) are small non-coding RNAs involved in post-transcriptional gene regulation [9,10,11,12]. They play crucial regulatory roles in a number of biological processes [13,14,15,16,17,18,19,20]. Of note, miRNAs represent a very attractive therapeutic strategy to manipulate various processes as their activity can be efficiently modulated with innovative and personalized technologies [21,22]. We, and others, have identified a number of miRNAs involved in the regulation of endothelial function [23,24,25,26,27,28].
The main aim of this study was to identify miRNAs that specifically target Neuropilin-1 in human brain endothelial cells. We were able to pinpoint and validate hsa-miR-24-3p (indicated for brevity as miR-24) as a main regulator of Neuropilin-1 transcription.
2. Materials and Methods
2.1. Cell Culture and Reagents
All reagents were purchased from Millipore-Sigma (Burlington, MA, USA), unless otherwise stated. Human brain microvascular endothelial cells (hBMECs) were obtained from Neuromics (Minneapolis, MN, USA; catalog number: #HEC02). These cells have been proved to be the most suitable human cell line for an in vitro blood–brain barrier (BBB) model [29].
Cells were cultured in a standard humidified atmosphere (37 °C) containing 5% CO2. In some experiments, cells were transfected with pcDNA3.1-Neuropilin-1 plasmids (GenScript, Piscataway, NJ, USA).
2.2. Identification of miRNAs Targeting Neuropilin-1
To identify miRNAs targeting the 3′-UTR of Neuropilin-1, we used the online target prediction tool Targetscan 7.2, as previously described by our research group [28,30,31,32,33].
2.3. Biological Validation of miR-24 as a Regulator of Neuropilin-1
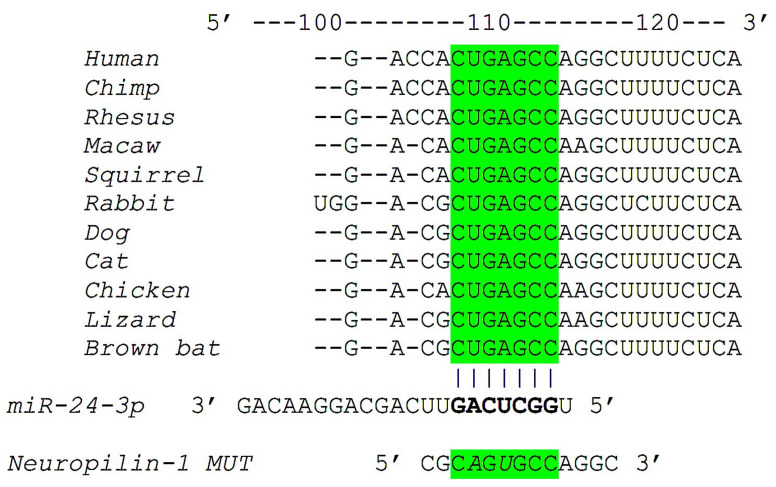
To evaluate the effects of miR-24 on Neuropilin-1 gene transcription, we used a luciferase reporter containing the 3’-UTR of the predicted miRNA interaction site, both wild-type and mutated, in hBMECs cells. The mutant construct of Neuropilin-1 3′-UTR (Neuropilin-1 MUT, as shown in Figure 1), harboring a substitution of two nucleotides within the predicted miR-24 binding sites of Neuropilin-1 3′-UTR was obtained through means of the NEBaseChanger and Q5 site-directed mutagenesis kit (New England Biolabs, Ipswich, MA, USA) as we described [30,32].
Figure 1.
Identification of miR-24 as modulator of Neuropilin-1. Complementary nucleotides between the target region of Neuropilin-1 3′-UTR (in green) and hsa-miR-24-3p are highly conserved across different species.
We transfected hBMECs with the 3′-UTR reporter plasmid (0.05 μg) and miR-24 mirVanaTM mimics (ThermoFisher Scientific, Waltham MA, USA) or miR-24 miRIDIAN hairpin inhibitors (PerkinElmer, Waltham MA, USA), as well as a non-targeting negative control (scramble), all used at a final concentration of 50 nMol/L, using Lipofectamine RNAiMAX (ThermoFisher Scientific) [32]. Firefly and Renilla luciferase activities were measured 48 h after transfection, using a Luciferase Reporter Assay System (Promega, Madison, WI, USA), normalizing Firefly luciferase to Renilla luciferase activity [32].
Levels of miR-24 were measured via TaqMan miRNA assays (ThermoFisher Scientific), according to the manufacturer’s instructions, and normalized to the level of U6 as we previously described and validated [28,30]. Cellular expression of Neuropilin-1 was determined by RT-qPCR, as we described [28,30,33], normalizing to endogenous glyceraldehyde 3-phosphate dehydrogenase (GAPDH). Sequences of oligonucleotide primers (Merck KGaA, Darmstadt, Germany) are reported in Table 1.
Table 1.
Sequences of oligonucleotide primers and product sizes.
| Gene | Primer | Sequence (5′–3′) | Amplicon (bp) |
|---|---|---|---|
| Neuropilin-1 | Forward | CCA CAG TGG AAC AGG TGA TG | 114 |
| Reverse | ACA CAC ACA GGC GTT AGC TG | ||
| GAPDH | Forward | GGC TCC CTT GGG TAT ATG GT | 94 |
| Reverse | TTG ATT TTG GAG GGA TCT CG |
GAPDH: glyceraldehyde 3-phosphate dehydrogenase.
2.4. Western Blot
Immunoblots were obtained as we previously described and validated [28,30,31] using the Odyssey system (LI-COR Biosciences, Lincoln, NE, USA); the intensity of bands was quantified using the FIJI software.
The following antibodies were used: Neuropilin-1 (catalog number: #ST0530, Novus Biologicals, Bio-Techne, Minneapolis, MN, USA); Akt (catalog number: #sc-5298, Santa Cruz Biotechnology, Dallas, TX, USA); pAktSer473 (catalog number: #9271, Cell Signaling, Danvers, MA, USA); β Actin (catalog number: #ab8229, abcam, Cambridge, MA, USA).
2.5. Endothelial Permeability Assay
The in vitro permeability assay was performed as we previously described [34]. Briefly, hBMECs transfected with miR-24 mimic or miR scramble were grown on 0.4-mm fibronectin-coated (R&D Systems, Inc., Minneapolis, MN, USA) Transwell filters (Corning Inc., Corning, NY, USA). After 48 h, the medium in the upper well was replaced by FITC-dextran 70 kD (0.5 mg/mL in PB).
Cells were stimulated in the lower well with PBS alone or PBS containing 50 ng/mL VEGF-A165 (R&D Systems). The entity of endothelial permeabilization was determined measuring at 520 nm the fluorescence of Dextran that passed in the bottom chamber through the cell monolayer.
2.6. Statistical Analysis
All data are expressed as means ± standard error of means (SEM). Statistical analyses were carried out using GraphPad 8 (Prism, San Diego, CA, USA). Statistical significance, set at p < 0.05, was tested using the two-way ANOVA followed by Tukey–Kramer multiple comparison test or the nonparametric Mann–Whitney U test, as appropriate.
3. Results
3.1. Identification of miR-24 as a Specific Modulator of Neuropilin-1
A bioinformatic screening resulted in the identification of hsa-miR-24 as a highly conserved miRNA potentially capable of repressing Neuropilin-1 mRNA expression. The complementary nucleotides between the target region of Neuropilin-1 3’ untranslated region (3′-UTR) and miR-24 are evolutionarily highly conserved across different species, including humans, nonhuman primates, and rodents (Figure 1).
3.2. Neuropilin-1 Is a Molecular Target of miR-24
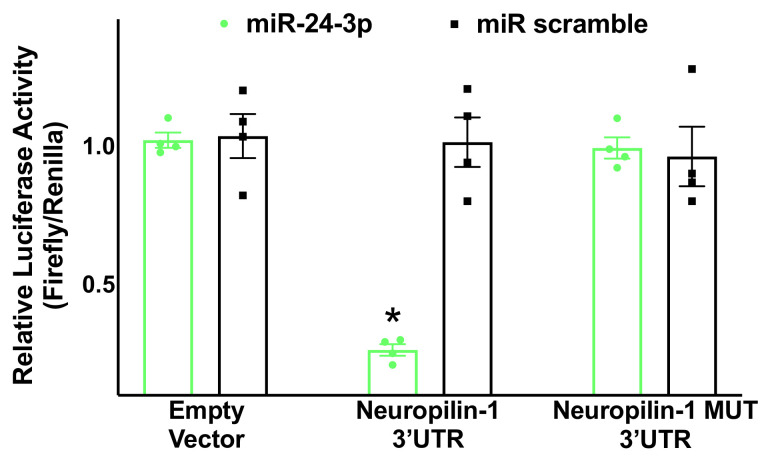
The proposed relationship was substantiated by an experimental validation of seed complementarity, confirming through a luciferase assay the interaction between miR-24 and the 3′-UTR of Neuropilin-1 in hBMECs (Figure 2).
Figure 2.
Validation of Neuropilin-1 targeting by miR-24. Luciferase activity was measured in hBMECs 48 h after transfection, using the vector without Neuropilin-1 3′-UTR (empty vector), the vector containing the wild-type Neuropilin-1 3′-UTR, and the vector containing a mutated Neuropilin-1 3′-UTR (Neuropilin-1 MUT); a non-targeting miRNA (miR scramble) has been employed as further control. Means ± S.E.M; * p < 0.05.
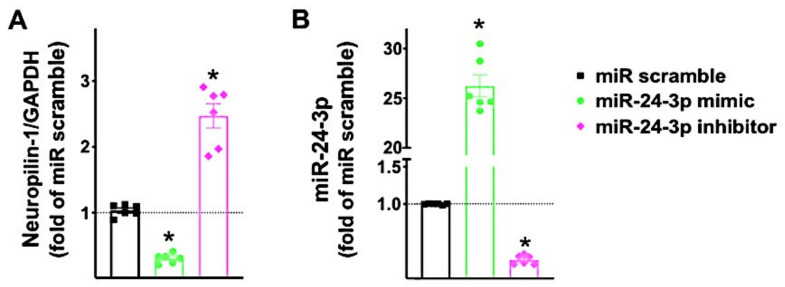
3.3. miR-24 Regulates Neuropilin-1 Transcription Levels in Human Endothelial Cells
After having validated that miR-24 targets Neuropilin-1 3’UTR, we verified the effects of miR-24 mimic and miR-24 inhibitor on the transcription levels of Neuropilin-1 in hBMECs (Figure 3). These results were confirmed by immunoblot in terms of protein levels (Supplementary Figure S1).
Figure 3.
Neuropilin-1 expression in human brain endothelial cells is reduced by miR-24 and increased by miR-24 inhibitor. Neuropilin-1 mRNA levels (A) were measured in hBMECs transfected with miR-24 mimic, inhibitor, or scramble (negative control) for 48 h; miR-24 expression was assessed as well (B). Means ± S.E.M; * p < 0.05.
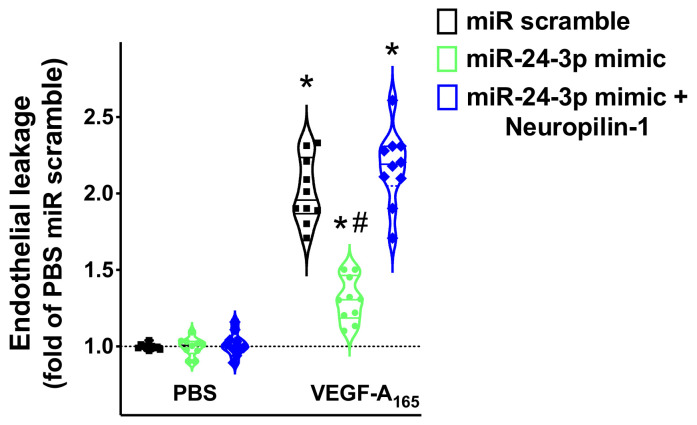
3.4. miR-24 Regulates Neuropilin-1 Mediated Endothelial Permeability
Several investigators have demonstrated that Neuropilin-1 is involved in EC permeability [35,36,37]. To assess the functional role of miR-24 on Neuropilin-1 mediated endothelial permeability, we performed an in vitro permeability assay, following an experimental protocol that we have recently described [34].
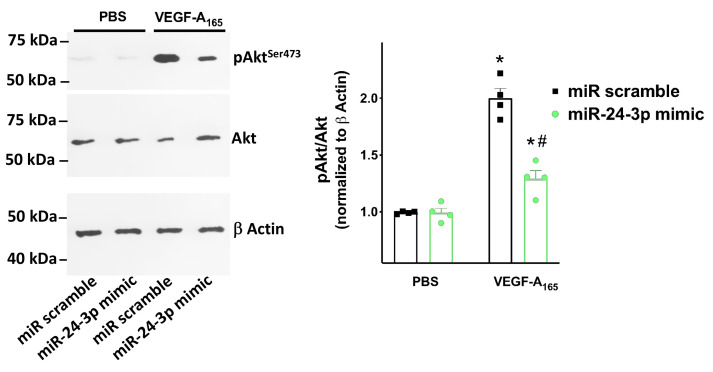
As shown in Figure 4, we found that miR-24 significantly reduced the permeability of hBMECs in response to VEGF165, an established agonist of Neuropilin-1 [4,38,39], and Neuropilin-1 overexpression rescued such an impaired response. Moreover, miR-24 mimic reduced VEGF165 induced Akt phosphorylation (Figure 5).
Figure 4.
Targeting Neuropilin-1 by miR-24 significantly reduces endothelial permeability. Endothelial leakage triggered by VEGF-A165 (50 ng/mL) was measured in hBMECs transfected with miR-24-3p mimic, miR scramble, or combining miR-24-3p mimic and Neuropilin-1 overexpression; * p < 0.05 vs. PBS, # p < 0.05 vs. miR-scramble. PBS: Phosphate-buffered saline.
Figure 5.
Targeting Neuropilin-1 by miR-24 significantly reduces Akt activation. Akt phosphorylation in Ser473 (representative immunoblots from 4 experimental assays) triggered by VEGF-A165 (50 ng/mL) was measured in hBMECs transfected with miR-24-3p mimic or miR scramble * p < 0.05 vs. PBS, # p < 0.05 vs. miR-scramble. PBS: Phosphate-buffered saline.
4. Discussion
In the present study, we have demonstrated for the first time that miR-24 directly targets the 3’UTR of Neuropilin-1. To the best of our knowledge, we also provide the first evidence of the actual expression of Neuropilin-1 in human brain endothelial cells.
Our findings are consistent with previous research showing that Neuropilin-1 is expressed by pulmonary endothelial cells [40] and by tumor-associated vascular endothelial cells (TAVECs) [41]. Our data on miR-24 are in agreement with previous studies exploring the functional role of miR-24 in endothelial cells. Indeed, miR-24-3p has been shown to regulate angiogenesis in rodents, zebrafish embryos, and in diabetic patients by modulating endothelial function [42,43]. Additionally, miR-24 has been demonstrated to reduce endothelium-dependent inflammatory responses [44].
Neuropilin-1 is a transmembrane receptor that is abundant in the respiratory and olfactory epithelium and in olfactory-related regions such as the olfactory tubercles and para-olfactory gyri [45]. Two independent studies recently published in Science have demonstrated that Neuropilin-1 represents a crucial co-factor necessary for the entry of the severe acute respiratory syndrome coronavirus (SARS-CoV-2)—which causes the coronavirus disease 2019 (COVID-19)—in human cells [46,47]. The first one, led by Ludovico Cantuti-Castelvetri [46] has shown that Neuropilin-1 significantly potentiates SARS-CoV-2 infectivity; the second one, led by James L. Daly, has proven via biochemical approaches and x-ray crystallography that the cleaved Spike protein of SARS-CoV-2 directly binds Neuropilin-1 [47].
Mounting evidence has shown that SARS-CoV-2 can directly target endothelial cells [48,49,50,51,52,53,54,55,56,57], an aspect initially reported by our group in March 2020 by simply observing the systemic manifestations in COVID-19 patients [48,49,58], and later corroborated by autoptic findings [59,60,61,62,63] and by the analysis of amputation specimens [64]. Intriguingly, brain endothelial cells show a distinct pro-inflammatory response when exposed to SARS-CoV-2 spike protein subunits [65] and infected vascular endothelial cells have been shown to spread SARS-CoV-2 to glial cells in the central nervous system [66]. Furthermore, COVID-19 has been associated with a wide spectrum of neurological symptoms and Neuropilin-1 has been proposed as a key factor in the neurological manifestation of COVID-19 by enhancing the entry of SARS-CoV-2 into the brain [66,67,68,69,70,71].
The most studied ligands of Neuropilin-1 are vascular endothelial growth factor (VEGF), semaphorins, complement split products, and furin-cleaved substrates [1,2,3,4,72]. Interestingly, augmented VEGF levels have been reported in bronchial alveolar lavage fluid from COVID-19 patients [73] and asymptomatic COVID-19 have lower serum VEGF levels compared to symptomatic patients [74]. In line with these observations, the interaction between Neuropilin-1 and VEGF has been recently shown to be implied in nociception [75].
Neuropilin-1 could also be involved in the relationship between COVID-19 and diabetes mellitus. Various studies have demonstrated that severe COVID-19 disproportionately affects patients with diabetes [76,77]. Of note, among the proposed SARS-CoV-2 cell-entry and amplification factors assessed in a cryopreserved human diabetic kidney single-nucleus RNA sequencing dataset [78], only Neuropilin-1 was found to be significantly upregulated [46]. In agreement with these reports, hyperglycemia has been shown to downregulate miR-24 expression in plasma and tissue and knocking miR-24 down in mice leads to increased expression and secretion of von Willebrand factor in endothelial cells, accompanied by a significantly enhanced platelet tethering [79], thereby suggesting a pathophysiologic role for this miRNA in the thromboembolic complications described in COVID-19 [49,80,81,82].
In addition to endothelial cells, Neuropilin-1 is expressed in immune cells, including T cells, B cells, macrophages, dendritic cells, and mast cells, where it regulates development, migration, recruitment, and communication between different immune cells [83]. Despite emerging evidence for the immune regulatory functions of Neuropilin-1, its exact molecular pathways remain not fully understood. Nevertheless, it is likely that Neuropilin-1 could be also involved in the cytokine storm and the subsequent hyper-inflammatory state observed in COVID-19 patients [84,85,86], although further dedicated studies in this sense are necessary.
Our study should be interpreted in light of some limitations. For instance, we only performed in vitro experiments testing the association between miR-24 and Neuropilin-1 mRNA, and we did not verify the actual effects of miR-24 on SARS-CoV-2 infection. Since most of the findings were obtained using exogenously expressed miRNAs, further studies are required to evaluate the translational potential of our results. Nonetheless, our findings are consistent with the observation of miR-24 expression in endothelial cells [42,43,44,87] and its roles as a regulator of various cerebrovascular phenomena, including angiogenesis in gliomas [88,89] and vasospasm following subarachnoid hemorrhage [90]. The study also has some strengths, including the fact that the 3′-UTR of Neuropilin-1 that is targeted by miR-24 is highly conserved among species, from primates to rodents.
In conclusion, our data show for the first time that Neuropilin-1 is a direct target of miR-24 in human brain endothelial cells.
Supplementary Materials
The following are available online at https://www.mdpi.com/2311-553X/7/1/9/s1, Figure S1: Neuropilin-1 protein expression is regulated by miR-24-3p.
Author Contributions
G.S. designed the study and wrote the manuscript; P.M., J.G., X.W., S.S.J., and A.M. performed and analyzed experimental assays and contributed to discussion. All authors have read and agreed to the published version of the manuscript.
Funding
The Santulli Lab is supported in part by the National Institutes of Health (NIH: R01-DK123259, R01-HL146691, R01-DK033823, R56-AG066431, T32-HL144456, R00-DK107895, to G.S.) and by the AHA (20POST-35211151) to J.G.
Institutional Review Board Statement
Not applicable since the study does not involve humans or animals.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data herein presented are available in this article and Supplementary Material.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.He Z., Tessier-Lavigne M. Neuropilin is a receptor for the axonal chemorepellent semaphorin III. Cell. 1997;90:739–751. doi: 10.1016/S0092-8674(00)80534-6. [DOI] [PubMed] [Google Scholar]
- 2.Kolodkin A.L., Levengood D.V., Rowe E.G., Tai Y.T., Giger R.J., Ginty D.D. Neuropilin is a semaphorin III receptor. Cell. 1997;90:753–762. doi: 10.1016/S0092-8674(00)80535-8. [DOI] [PubMed] [Google Scholar]
- 3.Soker S., Takashima S., Miao H.Q., Neufeld G., Klagsbrun M. Neuropilin-1 is expressed by endothelial and tumor cells as an isoform-specific receptor for vascular endothelial growth factor. Cell. 1998;92:735–745. doi: 10.1016/S0092-8674(00)81402-6. [DOI] [PubMed] [Google Scholar]
- 4.Oh H., Takagi H., Otani A., Koyama S., Kemmochi S., Uemura A., Honda Y. Selective induction of neuropilin-1 by vascular endothelial growth factor (VEGF): A mechanism contributing to VEGF-induced angiogenesis. Proc. Natl. Acad. Sci. USA. 2002;99:383–388. doi: 10.1073/pnas.012074399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pellet-Many C., Frankel P., Jia H., Zachary I. Neuropilins: Structure, function and role in disease. Biochem. J. 2008;411:211–226. doi: 10.1042/BJ20071639. [DOI] [PubMed] [Google Scholar]
- 6.Rossignol M., Gagnon M.L., Klagsbrun M. Genomic organization of human neuropilin-1 and neuropilin-2 genes: Identification and distribution of splice variants and soluble isoforms. Genomics. 2000;70:211–222. doi: 10.1006/geno.2000.6381. [DOI] [PubMed] [Google Scholar]
- 7.Dumond A., Pages G. Neuropilins, as relevant oncology target: Their role in the tumoral microenvironment. Front. Cell. Dev. Biol. 2020;8:662. doi: 10.3389/fcell.2020.00662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Y., Cao Y., Mangalam A.K., Guo Y., LaFrance-Corey R.G., Gamez J.D., Atanga P.A., Clarkson B.D., Zhang Y., Wang E., et al. Neuropilin-1 modulates interferon-gamma-stimulated signaling in brain microvascular endothelial cells. J. Cell. Sci. 2016;129:3911–3921. doi: 10.1242/jcs.190702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santulli G. MicroRNAs distinctively regulate vascular smooth muscle and endothelial cells: Functional implications in angiogenesis, atherosclerosis, and in-stent restenosis. Adv. Exp. Med. Biol. 2015;887:53–77. doi: 10.1007/978-3-319-22380-3_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stavast C.J., Erkeland S.J. The non-canonical aspects of MicroRNAs: Many roads to gene regulation. Cells. 2019;8:1465. doi: 10.3390/cells8111465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van der Kwast R., Quax P.H.A., Nossent A.Y. An emerging role for isomiRs and the microRNA epitranscriptome in Neovascularization. Cells. 2019;9:61. doi: 10.3390/cells9010061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Santulli G. Exosomal MicroRNA: The revolutionary endogenous innerspace nanotechnology. Sci. Transl. Med. 2018;10:eaav9141. doi: 10.1126/scitranslmed.aav9141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Godlewski J., Lenart J., Salinska E. MicroRNA in brain pathology: Neurodegeneration the other side of the brain cancer. Noncoding RNA. 2019;5:20. doi: 10.3390/ncrna5010020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wronska A., Kurkowska-Jastrzebska I., Santulli G. Application of MicroRNAs in diagnosis and treatment of cardiovascular disease. Acta. Physiol. 2015;213:60–83. doi: 10.1111/apha.12416. [DOI] [PubMed] [Google Scholar]
- 15.Wong W.K.M., Sorensen A.E., Joglekar M.V., Hardikar A.A., Dalgaard L.T. Non-Coding RNA in pancreas and beta-cell development. Noncoding RNA. 2018;4:41. doi: 10.3390/ncrna4040041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dama E., Melocchi V., Mazzarelli F., Colangelo T., Cuttano R., Di Candia L., Ferretti G.M., Taurchini M., Graziano P., Bianchi F. Non-Coding RNAs as Prognostic Biomarkers: A miRNA signature specific for aggressive early-stage lung adenocarcinomas. Noncoding RNA. 2020;6:48. doi: 10.3390/ncrna6040048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Creemers E.E., Tijsen A.J., Pinto Y.M. Circulating MicroRNAs: Novel biomarkers and extracellular communicators in cardiovascular disease? Circ. Res. 2012;110:483–495. doi: 10.1161/CIRCRESAHA.111.247452. [DOI] [PubMed] [Google Scholar]
- 18.Fay E.J., Langlois R.A. MicroRNA-attenuated virus vaccines. Noncoding RNA. 2018;4:25. doi: 10.3390/ncrna4040025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bar C., Chatterjee S., Falcao Pires I., Rodrigues P., Sluijter J.P.G., Boon R.A., Nevado R.M., Andres V., Sansonetti M., de Windt L., et al. Non-coding RNAs: Update on mechanisms and therapeutic targets from the ESC Working Groups of Myocardial Function and Cellular Biology of the Heart. Cardiovasc. Res. 2020;116:1805–1819. doi: 10.1093/cvr/cvaa195. [DOI] [PubMed] [Google Scholar]
- 20.Slota J.A., Booth S.A. MicroRNAs in neuroinflammation: Implications in disease pathogenesis, biomarker discovery and therapeutic applications. Noncoding RNA. 2019;5:35. doi: 10.3390/ncrna5020035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Christopher A.F., Kaur R.P., Kaur G., Kaur A., Gupta V., Bansal P. MicroRNA therapeutics: Discovering novel targets and developing specific therapy. Perspect. Clin. Res. 2016;7:68–74. doi: 10.4103/2229-3485.179431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Santulli G. In: MicroRNA: From Molecular Biology to Clinical Practice. Santulli G., editor. Springer Nature; New York, NY, USA: 2016. [Google Scholar]
- 23.Yang Y., Liu Y., Li Y., Chen Z., Xiong Y., Zhou T., Tao W., Xu F., Yang H., Yla-Herttuala S., et al. MicroRNA-15b targets VEGF and inhibits angiogenesis in proliferative diabetic retinopathy. J. Clin. Endocrinol. Metab. 2020;105:3404–3415. doi: 10.1210/clinem/dgaa538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Widlansky M.E., Jensen D.M., Wang J., Liu Y., Geurts A.M., Kriegel A.J., Liu P., Ying R., Zhang G., Casati M., et al. MiR-29 contributes to normal endothelial function and can restore it in cardiometabolic disorders. EMBO. Mol. Med. 2018;10:e8046. doi: 10.15252/emmm.201708046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Santulli G. MicroRNAs and Endothelial (Dys) Function. J. Cell. Physiol. 2016;231:1638–1644. doi: 10.1002/jcp.25276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang S., Aurora A.B., Johnson B.A., Qi X., McAnally J., Hill J.A., Richardson J.A., Bassel-Duby R., Olson E.N. The endothelial-specific MicroRNA miR-126 governs vascular integrity and angiogenesis. Dev. Cell. 2008;15:261–271. doi: 10.1016/j.devcel.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rafehi H., El-Osta A. HDAC inhibition in vascular endothelial cells regulates the expression of ncRNAs. Noncoding RNA. 2016;2:4. doi: 10.3390/ncrna2020004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Santulli G., Wronska A., Uryu K., Diacovo T.G., Gao M., Marx S.O., Kitajewski J., Chilton J.M., Akat K.M., Tuschl T., et al. A selective microRNA-based strategy inhibits restenosis while preserving endothelial function. J. Clin. Investig. 2014;124:4102–4114. doi: 10.1172/JCI76069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eigenmann D.E., Xue G., Kim K.S., Moses A.V., Hamburger M., Oufir M. Comparative study of four immortalized human brain capillary endothelial cell lines, hCMEC/D3, hBMEC, TY10, and BB19, and optimization of culture conditions, for an in vitro blood-brain barrier model for drug permeability studies. Fluids. Barriers. CNS. 2013;10:33. doi: 10.1186/2045-8118-10-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Matarese A., Gambardella J., Lombardi A., Wang X., Santulli G. MiR-7 Regulates GLP-1-Mediated Insulin Release by Targeting beta-Arrestin 1. Cells. 2020;9:1621. doi: 10.3390/cells9071621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang X., Morelli M.B., Matarese A., Sardu C., Santulli G. Cardiomyocyte-derived exosomal microRNA-92a mediates post-ischemic myofibroblast activation both in vitro and ex vivo. ESC. Heart. Fail. 2020;7:284–288. doi: 10.1002/ehf2.12584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matarese A., Gambardella J., Sardu C., Santulli G. MiR-98 regulates TMPRSS2 expression in human endothelial cells: Key implications for COVID-19. Biomedicines. 2020;8:642. doi: 10.3390/biomedicines8110462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morelli M.B., Shu J., Sardu C., Matarese A., Santulli G. Cardiosomal microRNAs are essential in post-infarction myofibroblast phenoconversion. Int. J. Mol. Sci. 2019;21:201. doi: 10.3390/ijms21010201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gambardella J., Sorriento D., Bova M., Rusciano M., Loffredo S., Wang X., Petraroli A., Carucci L., Mormile I., Oliveti M., et al. Role of endothelial G Protein-coupled receptor kinase 2 in angioedema. Hypertension. 2020;76:1625–1636. doi: 10.1161/HYPERTENSIONAHA.120.15130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Becker P.M., Waltenberger J., Yachechko R., Mirzapoiazova T., Sham J.S., Lee C.G., Elias J.A., Verin A.D. Neuropilin-1 regulates vascular endothelial growth factor-mediated endothelial permeability. Circ. Res. 2005;96:1257–1265. doi: 10.1161/01.RES.0000171756.13554.49. [DOI] [PubMed] [Google Scholar]
- 36.Roth L., Prahst C., Ruckdeschel T., Savant S., Westrom S., Fantin A., Riedel M., Heroult M., Ruhrberg C., Augustin H.G. Neuropilin-1 mediates vascular permeability independently of vascular endothelial growth factor receptor-2 activation. Sci. Signal. 2016;9:42. doi: 10.1126/scisignal.aad3812. [DOI] [PubMed] [Google Scholar]
- 37.Fantin A., Lampropoulou A., Senatore V., Brash J.T., Prahst C., Lange C.A., Liyanage S.E., Raimondi C., Bainbridge J.W., Augustin H.G., et al. VEGF165-induced vascular permeability requires NRP1 for ABL-mediated SRC family kinase activation. J. Exp. Med. 2017;214:1049–1064. doi: 10.1084/jem.20160311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tymecka D., Lipinski P.F.J., Fedorczyk B., Puszko A., Wilenska B., Perret G.Y., Misicka A. Structure-activity relationship study of tetrapeptide inhibitors of the Vascular Endothelial Growth Factor A binding to Neuropilin-1. Peptides. 2017;94:25–32. doi: 10.1016/j.peptides.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 39.Narazaki M., Tosato G. Ligand-induced internalization selects use of common receptor neuropilin-1 by VEGF165 and semaphorin3A. Blood. 2006;107:3892–3901. doi: 10.1182/blood-2005-10-4113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Han X., Zhou Z., Fei L., Sun H., Wang R., Chen Y., Chen H., Wang J., Tang H., Ge W., et al. Construction of a human cell landscape at single-cell level. Nature. 2020;581:303–309. doi: 10.1038/s41586-020-2157-4. [DOI] [PubMed] [Google Scholar]
- 41.Hsieh S.H., Ying N.W., Wu M.H., Chiang W.F., Hsu C.L., Wong T.Y., Jin Y.T., Hong T.M., Chen Y.L. Galectin-1, a novel ligand of neuropilin-1, activates VEGFR-2 signaling and modulates the migration of vascular endothelial cells. Oncogene. 2008;27:3746–3753. doi: 10.1038/sj.onc.1211029. [DOI] [PubMed] [Google Scholar]
- 42.Fiedler J., Jazbutyte V., Kirchmaier B.C., Gupta S.K., Lorenzen J., Hartmann D., Galuppo P., Kneitz S., Pena J.T., Sohn-Lee C., et al. MicroRNA-24 regulates vascularity after myocardial infarction. Circulation. 2011;124:720–730. doi: 10.1161/CIRCULATIONAHA.111.039008. [DOI] [PubMed] [Google Scholar]
- 43.Xu Y., Ouyang L., He L., Qu Y., Han Y., Duan D. Inhibition of exosomal miR-24-3p in diabetes restores angiogenesis and facilitates wound repair via targeting PIK3R3. J. Cell. Mol. Med. 2020;24:13789–13803. doi: 10.1111/jcmm.15958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zheng Y., Li Y., Liu G., Qi X., Cao X. MicroRNA-24 inhibits the proliferation and migration of endothelial cells in patients with atherosclerosis by targeting importin-alpha3 and regulating inflammatory responses. Exp. Ther. Med. 2018;15:338–344. doi: 10.3892/etm.2017.5355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Davies J., Randeva H.S., Chatha K., Hall M., Spandidos D.A., Karteris E., Kyrou I. Neuropilin1 as a new potential SARSCoV2 infection mediator implicated in the neurologic features and central nervous system involvement of COVID19. Mol. Med. Rep. 2020;22:4221–4226. doi: 10.3892/mmr.2020.11510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cantuti-Castelvetri L., Ojha R., Pedro L.D., Djannatian M., Franz J., Kuivanen S., van der Meer F., Kallio K., Kaya T., Anastasina M., et al. Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science. 2020;370:856–860. doi: 10.1126/science.abd2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Daly J.L., Simonetti B., Klein K., Chen K.E., Williamson M.K., Anton-Plagaro C., Shoemark D.K., Simon-Gracia L., Bauer M., Hollandi R., et al. Neuropilin-1 is a host factor for SARS-CoV-2 infection. Science. 2020;370:861–865. doi: 10.1126/science.abd3072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Santulli G., Morelli M., Gambardella J. Is Endothelial Dysfunction the Concealed Cornerstone of COVID-19? BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sardu C., Gambardella J., Morelli M.B., Wang X., Marfella R., Santulli G. Hypertension, Thrombosis, Kidney Failure, and Diabetes: Is COVID-19 an Endothelial Disease? A Comprehensive Evaluation of Clinical and Basic Evidence. J. Clin. Med. 2020;9:1417. doi: 10.13140/RG.2.2.17295.74407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gambardella J., Santulli G. What is linking COVID-19 and endothelial dysfunction? Updates on nanomedicine and bioengineering from the 2020 AHA Scientific Sessions. Eur. Heart. J. Cardiovasc. Pharmacother. 2020;30:pvaa145. doi: 10.1093/ehjcvp/pvaa145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kaur S., Tripathi D.M., Yadav A. The Enigma of Endothelium in COVID-19. Front. Physiol. 2020;11:989. doi: 10.3389/fphys.2020.00989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Evans P.C., Rainger G.E., Mason J.C., Guzik T.J., Osto E., Stamataki Z., Neil D., Hoefer I.E., Fragiadaki M., Waltenberger J., et al. Endothelial dysfunction in COVID-19: A position paper of the ESC Working Group for Atherosclerosis and Vascular Biology, and the ESC Council of Basic Cardiovascular Science. Cardiovasc. Res. 2020;116:2177–2184. doi: 10.1093/cvr/cvaa230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Libby P., Luscher T. COVID-19 is, in the end, an endothelial disease. Eur. Heart J. 2020;41:3038–3044. doi: 10.1093/eurheartj/ehaa623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ward S.E., Curley G.F., Lavin M., Fogarty H., Karampini E., McEvoy N.L., Clarke J., Boylan M., Alalqam R., Worrall A.P., et al. Von Willebrand factor propeptide in severe coronavirus disease 2019 (COVID-19): Evidence of acute and sustained endothelial cell activation. Br. J. Haematol. 2020 doi: 10.1111/bjh.17273. [DOI] [PubMed] [Google Scholar]
- 55.Fraser D.D., Patterson E.K., Slessarev M., Gill S.E., Martin C., Daley M., Miller M.R., Patel M.A., Dos Santos C.C., Bosma K.J., et al. Endothelial Injury and Glycocalyx Degradation in Critically Ill Coronavirus Disease 2019 Patients: Implications for Microvascular Platelet Aggregation. Crit. Care. Explor. 2020;2:e0194. doi: 10.1097/CCE.0000000000000194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Loo J., Spittle D.A., Newnham M. COVID-19, immunothrombosis and venous thromboembolism: Biological mechanisms. Thorax. 2021 doi: 10.1136/thoraxjnl-2020-216243. [DOI] [PubMed] [Google Scholar]
- 57.Castro R.A., Frishman W.H. Thrombotic Complications of COVID-19 Infection: A Review. Cardiol. Rev. 2021;29:43–47. doi: 10.1097/CRD.0000000000000347. [DOI] [PubMed] [Google Scholar]
- 58.Sardu C., Gambardella J., Morelli M., Wang X., Marfella R., Santulli G. Is COVID-19 an Endothelial Disease? Clinical and Basic Evidence. Preprints. 2020:2020040204. doi: 10.20944/preprints202004.0204.v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ackermann M., Verleden S.E., Kuehnel M., Haverich A., Welte T., Laenger F., Vanstapel A., Werlein C., Stark H., Tzankov A., et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N. Engl. J. Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Varga Z., Flammer A.J., Steiger P., Haberecker M., Andermatt R., Zinkernagel A.S., Mehra M.R., Schuepbach R.A., Ruschitzka F., Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fox S.E., Li G., Akmatbekov A., Harbert J.L., Lameira F.S., Brown J.Q., Vander Heide R.S. Unexpected Features of Cardiac Pathology in COVID-19 Infection. Circulation. 2020;142:1123–1125. doi: 10.1161/CIRCULATIONAHA.120.049465. [DOI] [PubMed] [Google Scholar]
- 62.Stahl K., Brasen J.H., Hoeper M.M., David S. Direct evidence of SARS-CoV-2 in gut endothelium. Intensive Care Med. 2020;46:2081–2082. doi: 10.1007/s00134-020-06237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bosmuller H., Traxler S., Bitzer M., Haberle H., Raiser W., Nann D., Frauenfeld L., Vogelsberg A., Klingel K., Fend F. The evolution of pulmonary pathology in fatal COVID-19 disease: An autopsy study with clinical correlation. Virchows Arch. 2020;477:349–357. doi: 10.1007/s00428-020-02881-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ilonzo N., Kumar S., Borazan N., Hansen T., Rao A., Lantis J., Faries P., Ting W. Endotheliitis in COVID-19-positive patients after extremity amputation for acute thrombotic events. Ann. Vasc. Surg. 2020;30 doi: 10.1016/j.avsg.2020.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Buzhdygan T.P., DeOre B.J., Baldwin-Leclair A., Bullock T.A., McGary H.M., Khan J.A., Razmpour R., Hale J.F., Galie P.A., Potula R., et al. The SARS-CoV-2 spike protein alters barrier function in 2D static and 3D microfluidic in-vitro models of the human blood-brain barrier. Neurobiol. Dis. 2020;146:105131. doi: 10.1016/j.nbd.2020.105131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zubair A.S., McAlpine L.S., Gardin T., Farhadian S., Kuruvilla D.E., Spudich S. Neuropathogenesis and Neurologic Manifestations of the Coronaviruses in the Age of Coronavirus Disease 2019: A Review. JAMA Neurol. 2020;77:1018–1027. doi: 10.1001/jamaneurol.2020.2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Desai I., Manchanda R., Kumar N., Tiwari A., Kumar M. Neurological manifestations of coronavirus disease 2019: Exploring past to understand present. Neurol. Sci. 2021;11:1–13. doi: 10.1007/s10072-020-04964-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tandon M., Kataria S., Patel J., Mehta T.R., Daimee M., Patel V., Prasad A., Chowdhary A.A., Jaiswal S., Sriwastava S. A Comprehensive Systematic Review of CSF analysis that defines Neurological Manifestations of COVID-19. Int. J. Infect. Dis. 2021;9 doi: 10.1016/j.ijid.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Paniz-Mondolfi A., Bryce C., Grimes Z., Gordon R.E., Reidy J., Lednicky J., Sordillo E.M., Fowkes M. Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) J. Med. Virol. 2020;92:699–702. doi: 10.1002/jmv.25915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rhea E.M., Logsdon A.F., Hansen K.M., Williams L.M., Reed M.J., Baumann K.K., Holden S.J., Raber J., Banks W.A., Erickson M.A. The S1 protein of SARS-CoV-2 crosses the blood-brain barrier in mice. Nat. Neurosci. 2020 doi: 10.1038/s41593-020-00771-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mayi B.S., Leibowitz J.A., Woods A.T., Ammon K.A., Liu A.E., Raja A. The role of Neuropilin-1 in COVID-19. PLoS Pathog. 2021;17:e1009153. doi: 10.1371/journal.ppat.1009153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Teesalu T., Sugahara K.N., Kotamraju V.R., Ruoslahti E. C-end rule peptides mediate neuropilin-1-dependent cell, vascular, and tissue penetration. Proc. Natl. Acad. Sci. USA. 2009;106:16157–16162. doi: 10.1073/pnas.0908201106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ray P.R., Wangzhou A., Ghneim N., Yousuf M.S., Paige C., Tavares-Ferreira D., Mwirigi J.M., Shiers S., Sankaranarayanan I., McFarland A.J., et al. A pharmacological interactome between COVID-19 patient samples and human sensory neurons reveals potential drivers of neurogenic pulmonary dysfunction. Brain Behav. Immun. 2020;89:559–568. doi: 10.1016/j.bbi.2020.05.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Long Q.X., Tang X.J., Shi Q.L., Li Q., Deng H.J., Yuan J., Hu J.L., Xu W., Zhang Y., Lv F.J., et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat. Med. 2020;26:1200–1204. doi: 10.1038/s41591-020-0965-6. [DOI] [PubMed] [Google Scholar]
- 75.Moutal A., Martin L.F., Boinon L., Gomez K., Ran D., Zhou Y., Stratton H.J., Cai S., Luo S., Gonzalez K.B., et al. SARS-CoV-2 spike protein co-opts VEGF-A/neuropilin-1 receptor signaling to induce analgesia. Pain. 2021;162:243–252. doi: 10.1097/j.pain.0000000000002097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fang L., Karakiulakis G., Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir. Med. 2020;8:e21. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rubino F., Amiel S.A., Zimmet P., Alberti G., Bornstein S., Eckel R.H., Mingrone G., Boehm B., Cooper M.E., Chai Z., et al. New-Onset Diabetes in Covid-19. N. Engl. J. Med. 2020;383:789–790. doi: 10.1056/NEJMc2018688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wilson P.C., Wu H., Kirita Y., Uchimura K., Ledru N., Rennke H.G., Welling P.A., Waikar S.S., Humphreys B.D. The single-cell transcriptomic landscape of early human diabetic nephropathy. Proc. Natl. Acad. Sci. USA. 2019;116:19619–19625. doi: 10.1073/pnas.1908706116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Xiang Y., Cheng J., Wang D., Hu X., Xie Y., Stitham J., Atteya G., Du J., Tang W.H., Lee S.H., et al. Hyperglycemia repression of miR-24 coordinately upregulates endothelial cell expression and secretion of von Willebrand factor. Blood. 2015;125:3377–3387. doi: 10.1182/blood-2015-01-620278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Flumignan R.L., Tinôco J.D.S., Pascoal P.I., Areias L.L., Cossi M.S., Fernandes M.I., Costa I.K., Souza L., Matar C.F., Tendal B., et al. Prophylactic anticoagulants for people hospitalised with COVID-19. Cochrane Database Syst. Rev. 2020;10 doi: 10.1002/14651858.CD013739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.McFadyen J.D., Stevens H., Peter K. The Emerging Threat of (Micro) Thrombosis in COVID-19 and Its Therapeutic Implications. Circ. Res. 2020;127:571–587. doi: 10.1161/CIRCRESAHA.120.317447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Vinayagam S., Sattu K. SARS-CoV-2 and coagulation disorders in different organs. Life. Sci. 2020;260:118431. doi: 10.1016/j.lfs.2020.118431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chaudhary B., Khaled Y.S., Ammori B.J., Elkord E. Neuropilin 1: Function and therapeutic potential in cancer. Cancer Immunol. Immunother. 2014;63:81–99. doi: 10.1007/s00262-013-1500-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Thepmankorn P., Bach J., Lasfar A., Zhao X., Souayah S., Chong Z.Z., Souayah N. Cytokine storm induced by SARS-CoV-2 infection: The spectrum of its neurological manifestations. Cytokine. 2020;138:155404. doi: 10.1016/j.cyto.2020.155404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nigrovic P.A. COVID-19 cytokine storm: What is in a name? Ann. Rheum. Dis. 2021;80:3–5. doi: 10.1136/annrheumdis-2020-219448. [DOI] [PubMed] [Google Scholar]
- 86.Brunetti L., Diawara O., Tsai A., Firestein B.L., Nahass R.G., Poiani G., Schlesinger N. Colchicine to Weather the Cytokine Storm in Hospitalized Patients with COVID-19. J. Clin. Med. 2020;9:2961. doi: 10.3390/jcm9092961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Connor K.L., Teenan O., Cairns C., Banwell V., Thomas R.A., Rodor J., Finnie S., Pius R., Tannahill G.M., Sahni V., et al. Identifying cell-enriched miRNAs in kidney injury and repair. JCI Insight. 2020;5 doi: 10.1172/jci.insight.140399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dai D., Huang W., Lu Q., Chen H., Liu J., Hong B. miR24 regulates angiogenesis in gliomas. Mol. Med. Rep. 2018;18:358–368. doi: 10.3892/mmr.2018.8978. [DOI] [PubMed] [Google Scholar]
- 89.Zhang J., Liu L., Xue Y., Ma Y., Liu X., Li Z., Li Z., Liu Y. Endothelial Monocyte-Activating Polypeptide-II Induces BNIP3-Mediated Mitophagy to Enhance Temozolomide Cytotoxicity of Glioma Stem Cells via Down-Regulating MiR-24-3p. Front. Mol. Neurosci. 2018;11:92. doi: 10.3389/fnmol.2018.00092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Li H.T., Wang J., Li S.F., Cheng L., Tang W.Z., Feng Y.G. Upregulation of microRNA24 causes vasospasm following subarachnoid hemorrhage by suppressing the expression of endothelial nitric oxide synthase. Mol. Med. Rep. 2018;18:1181–1187. doi: 10.3892/mmr.2018.9050. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data herein presented are available in this article and Supplementary Material.