Abstract
This study was conducted to determine the prevalence and determinants of medication adherence among patients with HIV/AIDS in southern Vietnam. Methods: A cross-sectional study was conducted in a hospital in southern Vietnam from June to December 2019 on patients who began antiretroviral therapy (ART) for at least 6 months. Using a designed questionnaire, patients were considered adherent if they took correct medicines with right doses, on time and properly with food and beverage and had follow-up visits as scheduled. Multivariable logistic regression was used to identify determinants of adherence. Key findings: A total of 350 patients (from 861 medical records) were eligible for the study. The majority of patients were male (62.9%), and the dominant age group (≥35 years old) accounted for 53.7% of patients. Sexual intercourse was the primary route of transmission of HIV (95.1%). The proportions of participants who took the correct medicine and at a proper dose were 98.3% and 86.3%, respectively. In total, 94.9% of participants took medicine appropriately in combination with food and beverage, and 75.7% of participants were strictly adherent to ART. The factors marital status (odds ratio (OR) = 2.54; 95%CI = 1.51–4.28), being away from home (OR = 1.7; 95%CI = 1.03–2.78), substance abuse (OR = 2.7; 95%CI = 1.44–5.05), general knowledge about ART (OR = 2.75; 95%CI = 1.67–4.53), stopping medication after improvement (OR = 4.16; 95%CI = 2.29–7.56) and self-assessment of therapy adherence (OR = 9.83; 95%CI = 5.44–17.77) were significantly associated with patients’ adherence. Conclusions: Three-quarters of patients were adherent to ART. Researchers should consider these determinants of adherence in developing interventions in further studies.
Keywords: human immunodeficiency virus (HIV), acquired immune deficiency syndrome (AIDS), antiretroviral therapy (ART), medication adherence, Vietnam
1. Introduction
The global human immunodeficiency virus (HIV) epidemic is one of the major worldwide health issues. In recent years, thanks to a myriad of efforts, the pandemic has been alleviated; there were 690,000 acquired immune deficiency syndrome (AIDS)-related deaths at the end of 2019, down from a peak of 2.2 million in the mid-2000s [1,2]. Of note, the estimated 1.7 million HIV patients worldwide in 2019 marked a 23% decline in new infections since 2010 [2].
In Vietnam, new HIV infections significantly reduced from 16,000 cases in 2010 to 5200 cases in 2019 [2]. The decrease of 67.5% in new infections and 40% in AIDS-related deaths over a 10-year period speaks to the effectiveness of the nationwide testing and treatment program. Additionally, the 2019 HIV/AIDS prevention and control report highlighted that nearly 95% had an HIV load below the detection threshold (<200 copies/mL) in the first 9 months of 2019 [3].
In addition to the effectiveness of antiretroviral therapy (ART), patients’ adherence to medical treatment plays a critical role in those positive health outcomes. Prior research has emphasized the significant correlation of optimal ART adherence with being virally suppressed [4,5,6]. Hence, the assessment of adherence to ART and evaluation of maintenance-associated factors in patients are critical.
There are few studies figuring out the correlation between patients’ characteristics and their medical adherence as well as the current status of ART adherence at a provincial level in Vietnam. Our research, therefore, was conducted to determine the characteristics of HIV/AIDS patients, assess the therapy adherence rate and investigate the factors associated with ART adherence of HIV/AIDS patients in a provincial hospital in Vietnam in 2019.
2. Materials and Methods
Our cross-sectional study was conducted on all patients having HIV/AIDS in an outpatient clinic of a provincial hospital in Vietnam from June to December 2019. Eligible patients had confirmed HIV-positive results and were aware of their HIV status. By using a systematic random sampling method, participants were selected from a patient list in numerical order. The sample size was 334 patients, which was calculated using the formula for a single proportion with the estimated HIV/AIDS treatment adherence rate in Vietnam, which was 0.68, type I error probability of 5% and a confidence level of 95%. An additional 5% were elected to tolerate some participants who were lost to follow-up or discontinued treatment; thus, there were 350 patients in this study.
Patients who were 18 years of age or older were included in the study if they had undergone (ART) for at least 6 months. Additionally, the outpatient department-treated cases with complete medical records and HIV-positive test results were also included. We excluded patients with (1) mental health issues that affect their abilities to respond, (2) follow-up incapability or (3) that were deceased at the time of the study. Any patient who did not agree to sign the patient’s consent was also excluded.
The data collection began with screening and filtering medical records of patients (≥18 years old) who had at least a 6-month follow-up. A list of 802 eligible patients was formed and every 2nd person on that list would be chosen as a participant. After systematic random sampling from the list, patients’ information was extracted and filled in a specific research form with an ID. In the next step, the patients who came to the outpatient clinic at the time of research and had medical IDs coinciding with those in our form were invited to an interview. A pilot survey was performed on 30 participants who were not included in the sample to verify the appropriateness and efficacy of the proposed data collecting methods. Data collection, coding and patient interviews were conducted and strictly controlled by the research team to ensure data consistency.
Patient adherence was measured and assessed by using a questionnaire which was taken as reference from the AIDS Clinical Trials Group (ACTG) Adherence and WebAd-Q Questionnaire [7,8]. In addition to the patient’s general information, the queries focused on their (1) adherence behaviors, (2) current medical status, (3) awareness of HIV care and treatment and (4) the support from medical services.
Patients were considered as having good knowledge of ART if they obtained 8 points (1 point for each correct answer) in the “treatment adherence knowledge” section from the questionnaire [9]. Queries in this section were about whether patients knew (1) what ARV (antiretroviral) drugs were, (2) how long it took for ARV treatment, (3) how many types of drugs that ARV was combined with, (4) how to take ARV drugs, (5) the side effects of drugs, (6) how to deal with the side effects, (7) how to deal with missing doses and (8) how to calculate the time to take the missing dose after remembering.
The adherence rate was determined as the number of adherent patients divided by the total number of patients at the time of the study. Patients were assessed as “adherent” when they fulfilled all the following criteria: (1) take drugs correctly with appropriate dose as prescribed, (2) on time and (3) suitably with food and drink, and (4) adherent with clinic visits [10]. Patients were considered non-adherent when they did not meet at least one of those requirements. In terms of factors associated with patients’ non-adherence, prior studies indicated that the most common causes were alcohol consumption, drug and substance abuse, working away from home and lack of good knowledge about ART adherence and family support [11,12,13]. Thus, in addition to patients’ knowledge and adherence, our questionnaire also considered the aforementioned factors.
Descriptive statistics were used to summarize categorical (proportions and frequencies) and continuous variables (means, max, min and standard deviations). The analysis results were presented in the form of a corresponding table. To analyze data and assess the difference between groups, the chi-square test with odds ratios (OR) and 95% confidence intervals (CIs) was performed. Univariable analysis results which were p-values ≤ 0.1 were analyzed by multivariable logistic regression with the Forward likelihood ratio (LR) method and also by the Backward LR method with the comparison standard based on the likelihood ratio to confirm the data accuracy. The goodness of fit for logistic regression models was evaluated by the Hosmer–Lemeshow test. Data were entered using Microsoft Excel and results were processed using SPSS version 20.0 (IBM Corp., New York, the United States). The outcomes were statistically significant if the p-values were ≤ 0.05.
Ethical approval for this study was obtained from the Medical Ethics Councils of Can Tho University of Medicine and Pharmacy and the provincial hospital (Approval number: 21/HDDD) in February 2019. Patients were clearly informed of the purpose and procedure of the study and voluntarily signed an informed consent form. Personal information of participants was kept strictly confidential in accordance with The Human Immunodeficiency Virus and Acquired Immune Deficiency Syndrome (Prevention and Control) Act.
3. Results
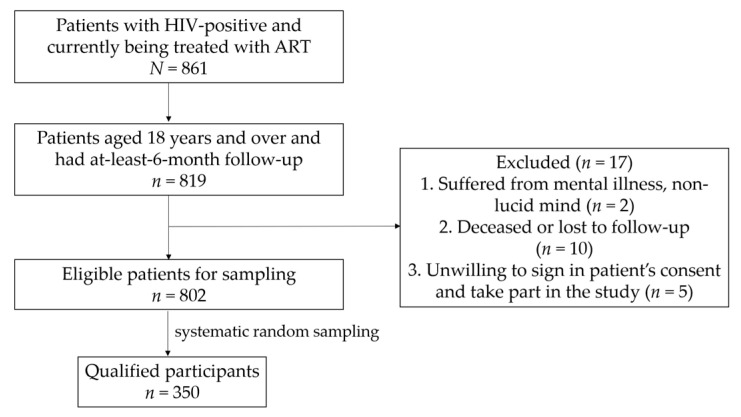
The number of patients with HIV who were being treated in the hospital was 861, of whom 95% were 18 years of age or older and had at least 6 months of follow-up on ART (Figure 1).
Figure 1.
Diagram of the research steps.
From the aforementioned group, 17 patients were excluded due to the exclusion criteria. After systematic random sampling from the list and selecting an additional 5%, 350 patients were included for this study.
3.1. Demographic and ART-Related Characteristics of Patients with HIV
In our study, the majority of patients were male (62.9%), and the dominant age group (≥35 years old) accounted for 53.7% (Table 1). In total, 47.4% of participants were married while the rest were single, divorced, separated or widowed. The number of patients who lived far away from the clinic (home-to-clinic distance ≥ 20 km) and worked far from their homes was 242 (69.1%) and 135 (38.6%), respectively.
Table 1.
Study population characteristics.
| Characteristics | Frequency and Percentage (n, %) | Adherence | p-Value ** | |
|---|---|---|---|---|
| Yes (n, %) | No (n, %) | |||
| Age | ||||
| ≥35 years old | 188 (53.7) | 151 (80.3) | 37 (19.7) | 0.03 |
| <35 years old | 162 (46.3) | 114 (70.4) | 48 (29.6) | |
| Gender | ||||
| Male | 220 (62.9) | 165 (75.0) | 55 (25.0) | 0.685 |
| Female | 130 (37.1) | 100 (76.9) | 30 (23.1) | |
| Marital status | ||||
| Married | 166 (47.4) | 140 (84.3) | 26 (15.7) | <0.001 |
| Single | 184 (52.6) | 125 (67.9) | 59 (32.1) | |
| Currently living with | ||||
| Relatives, friends | 295 (84.3) | 225 (76.3) | 70 (23.7) | 0.574 |
| Alone | 55 (15.7) | 40 (72.7) | 15 (27.3) | |
| Home-to-clinic distance | ||||
| <20 km | 108 (30.9) | 74 (68.5) | 34 (31.5) | 0.036 |
| ≥20 km | 242 (69.1) | 191 (78.9) | 51 (21.1) | |
| Level of education | ||||
| Upper secondary | 206 (58.9) | 161 (78.2) | 45 (21.8) | 0.203 |
| Lower secondary | 144 (41.1) | 104 (72.2) | 40 (27.8) | |
| Occupation | ||||
| Employment | 285 (81.4) | 216 (75.8) | 69 (24.2) | 0.945 |
| Unemployment | 65 (18.6) | 49 (75.4) | 16 (24.6) | |
| Work away from home | ||||
| Yes | 135 (38.6) | 94 (69.6) | 41 (30.4) | 0.035 |
| No | 215 (61.4) | 171 (79.5) | 44 (20.5) | |
| HIV transmission route | ||||
| Sexual behaviors | 333 (95.1) | 255 (76.6) | 78 (23.4) | 0.142 * |
| Drug abuse and mother–child | 17 (4.9) | 10 (58.8) | 7 (41.2) | |
| Clinical stage during treatment | ||||
| Stage I, II | 341 (97.4) | 257 (75.4) | 84 (24.6) | 0.693 * |
| Stage III, IV | 9 (2.6) | 8 (88.9) | 1 (11.1) | |
| CD4 count (cells/mm3) | ||||
| ≥200 | 283 (83.7) | 212 (74.9) | 71 (25.1) | 0.272 |
| <200 | 55 (16.3) | 45 (81.8) | 10 (18.2) | |
| Opportunistic infection | ||||
| Yes | 10 (2.9) | 5 (50.0) | 5 (50.0) | 0.067 * |
| No | 340 (97.1) | 260 (76.5) | 80 (23.5) | |
| Hepatitis B and C virus coinfection | ||||
| Yes | 312 (89.1) | 236 (75.6) | 76 (24.4) | 0.927 |
| No | 38 (10.9) | 29 (76.3) | 9 (23.7) | |
| ART regimen | ||||
| First-line ART | 340 (97.1) | 256 (75.3) | 84 (24.7) | 0.461 * |
| Second-line ART | 10 (2.9) | 9 (90.0) | 1 (10.0) | |
| Viral load (copies/mL) | ||||
| <20 cps | 305 (89.7) | 230 (75.4) | 75 (24.6) | 0.821 |
| >20 cps | 35 (10.3) | 27 (77.1) | 8 (22.9) | |
| Dosing times | ||||
| Once a day | 299 (85.4) | 224 (74.9) | 75 (25.1) | 0.399 |
| Twice a day | 51 (14.6) | 41 (80.4) | 10 (19.6) | |
| Drug abuse | ||||
| Yes | 244 (69.7) | 173 (70.9) | 71 (29.1) | 0.001 |
| No | 106 (30.3) | 92 (86.8) | 14 (13.2) | |
| Drug side effects | ||||
| Yes | 304 (86.9) | 228 (75.0) | 76 (25.0) | 0.423 |
| No | 46 (13.1) | 37 (80.4) | 9 (19.6) | |
| General knowledge about ART | ||||
| Yes | 217 (62.0) | 180 (82.9) | 37 (17.1) | <0.001 |
| No | 133 (38.0) | 85 (63.9) | 48 (36.1) | |
| Patients with stress, anxiety, depression | ||||
| Yes | 160 (45.7) | 128 (80.0) | 32 (20.0) | 0.086 |
| No | 190 (54.3) | 137 (72.1) | 53 (27.9) | |
| Patients’ quality of life after treatment | ||||
| Better | 239 (68.3) | 197 (82.4) | 42 (17.6) | <0.001 |
| Normal | 111 (31.7) | 68 (61.3) | 43 (38.7) | |
| Patients want to stop using drugs after improvement | ||||
| Yes | 56 (16.0) | 28 (50.0) | 28 (50.0) | <0.001 |
| No | 294 (84.0) | 237 (80.6) | 57 (19.4) | |
| Prompting of medication | ||||
| Self-managing | 293 (83.7) | 229 (78.2) | 64 (21.8) | 0.016 |
| Spouses, parents, siblings | 57 (16.3) | 36 (63.2) | 21 (36.8) | |
| Waiting time for medical examination | ||||
| Fast | 143 (40.9) | 120 (83.9) | 23 (16.1) | 0.003 |
| Normal | 207 (59.1) | 145 (70.0) | 62 (30.0) | |
| Satisfaction of medical services | ||||
| Very satisfied | 188 (53.7) | 160 (85.1) | 28 (14.9) | <0.001 |
| Satisfied | 162 (46.3) | 105 (64.8) | 57 (35.2) | |
| Feeling uncomfortable with treatment adherence | ||||
| Yes | 37 (10.6) | 27 (73.0) | 10 (27.0) | 0.681 |
| No | 313 (89.4) | 238 (76.0) | 75 (24.0) | |
| Self-assessment of adherence to treatment | ||||
| High adherence | 282 (80.6) | 240 (85.1) | 42 (14.9) | <0.001 |
| Medium and low adherence | 68 (19.4) | 25 (36.8) | 43 (63.2) | |
| Treatment period (months) | ||||
| Months (mean ± SD) | 350 (100) | 48.89 ± 36.13 | 51.25 ± 33.22 | 0.593 *** |
The chi-square test was performed to determine the relationship between adherence and related factors. * Fisher’s Exact Test. ** p-value ≤ 0.05 was considered statistically significant. *** Univariable regression logistic.
Sexual intercourse was the primary route of transmission of HIV (95.1%) (Table 1). Only 10 (2.9%) patients were at risk for opportunistic infection whereas a much larger proportion (89.1%) of HIV participants were co-infected with both hepatitis B virus (HBV) and hepatitis C virus (HCV) previously. The proportion of HIV patients that had a history of drug abuse accounted for 30.3%.
The rate of medication adherence increased with age; patients who were over 35 years old had better compliance than those who were younger (p = 0.03) (Table 1). Furthermore, there was a significant correlation between marital status and high adherence in patients, particularly for those who were married (p = 0.001). Intriguingly, patients who had not partaken in substance abuse were more likely to be well-adherent than those who were addicted (p = 0.001). However, there was no significant difference between the treatment adherence and side effects of medicines in patients, the period of treatment or with the gender of participants (p > 0.05).
3.2. The Proportion of Adherence to ART
The majority of patients were strictly adherent to their prescription (Table 2). The proportions of participants who took the right medicine and the appropriate dose were 98.3% and 86.3%, respectively. Furthermore, 87.4% of patients took ARV drugs on time, and 94.9% of participants took medicine appropriately in combination with food and beverage. The percentage of patients who kept up with their medical appointments was 99.4%. Notably, 75.7% of the patients had high adherence to ART (fulfilled all four criteria).
Table 2.
Adherence to antiretroviral therapy (ART) among patients with HIV.
| Adherence Assessment | Frequency (n = 350) | Percentage (%) |
|---|---|---|
| Take the right medicine | ||
| Yes | 344 | 98.3 |
| No | 6 | 1.7 |
| Take correct dose | ||
| Yes | 302 | 86.3 |
| No | 48 | 13.7 |
| Take medicine on time | ||
| Yes | 306 | 87.4 |
| No | 44 | 12.6 |
| Take medicine properly in combination with eating and drinking | ||
| Yes | 332 | 94.9 |
| No | 18 | 5.1 |
| Routine follow-up | ||
| Yes | 348 | 99.4 |
| No | 2 | 0.6 |
| Adherence to treatment | ||
| Yes | 265 | 75.7 |
| No | 85 | 24.3 |
3.3. Determinants of Patients’ Adherence
The multivariable logistic regression was analyzed with 13 factors of which simple regression analysis results were p-values ≤ 0.1. The factors that showed significant differences (p-value ≤ 0.05) between patients’ features and ART adherence were as follows: marital status, working away from home, substance use status, general knowledge about ART treatment, stopping use of ARV drugs after improvement and self-assessment of adherence with therapy (Table 3).
Table 3.
Univariable and multivariable regression analyses of the correlation between patients’ characteristics and ART adherence.
| Features | Univariable Regression Logistic | Multivariable Regression Logistic | ||
|---|---|---|---|---|
| OR (95%CI) | p-Value | OR (95%CI) | p-Value | |
| Marital Status | ||||
| Married | 2.54 (1.51–4.28) | <0.001 | 2.29 (1.25–4.19) | 0.007 |
| Single * | - | - | - | - |
| Work away from home | ||||
| No | 1.7 (1.03–2.78) | 0.036 | 2.15 (1.19–3.89) | 0.011 |
| Yes * | - | - | - | - |
| Drug abuse | ||||
| No | 2.7 (1.44–5.05) | 0.002 | 2.03 (1.01–4.08) | 0.048 |
| Yes * | - | - | - | - |
| General knowledge about ART treatment | ||||
| Yes | 2.75 (1.67–4.53) | <0.001 | 1.99 (1.1–3.64) | 0.026 |
| No * | - | - | - | - |
| Stop using drugs after improvement | ||||
| No | 4.16 (2.29–7.56) | <0.001 | 2.16 (1.04–4.46) | 0.039 |
| Yes * | - | - | - | - |
| Self-assessment of adherence to treatment | ||||
| High adherence | 9.83 (5.44–17.77) | <0.001 | 5.97 (3.07–11.61) | <0.001 |
| Medium and low adherence * | - | - | - | - |
(*): reference group.
A multivariate logistic regression analysis was used on 13 variables: (1) age, (2) marital status, (3) work away from home, (4) opportunistic infection, (5) drug abuse, (6) general knowledge about ART treatment, (7) patients with stress, anxiety or depression, (8) patients’ quality of life after treatment, (9) patients wanting to stop using drugs after improvement, (10) prompting of medication, (11) waiting time for medical examination, (12) satisfaction with medical services and (13) self-assessment of adherence to treatment by the Forward LR method.
4. Discussion
In our study, the adherence rate of participants was 75.7%. The factors marital status, being away from home, substance abuse, general knowledge about ART, stopping medication after improvement and self-assessment of therapy adherence were significantly associated with adherence in patients with HIV.
Adherence to therapy was considered the most pivotal element which could greatly affect patients’ health outcomes. Our study calculated that the adherence rate of participants with HIV was 75.7% (Table 2). This finding is similar to the studies carried out in other provinces with reported adherence rates of 71.8% and 77% [14,15]. Yet, two prior cross-sectional studies in Vietnam showed reported adherences of 62.9% and 68.4%, which were lower than our findings [16,17]. The reasons for the discrepancy in the adherence rates might be the sample sizes of their studies, which were smaller than ours.
In a detailed look, the proportion of patients who did not take enough dosage accounted for 13.7%, which was slightly higher than that of other research (11.3% and 9.5%) [16,17]. Yet, our results showed a lower adherence rate in terms of taking drugs on time (12.6%) than that of those two studies (22.7% and 28.5%). The measurement methods and the sampling intervals of the questionnaire may cause these differences.
Our multivariable regression analysis indicated that married patients were more strictly adherent to therapy than those who were single (p < 0.001 and p = 0.007 in univariable and multivariable regression analyses, respectively) (Table 3). Patients with HIV were supported not only in psychological well-being and financial status but also with medical care and daily activities. The significant correlation between partner support and adherence to ART was well documented; women were more likely to have low adherence if they had an unsupportive male partner [18,19].
Our research also attributed poor adherence to working away from home (p = 0.011). Various work-related reasons that lead to non-adherence were revealed [13]. Particularly, the most common causes were due to an intense schedule and fear of stigma at the patients’ workplaces. Moreover, internalized HIV-related stigma was proven to result in sub-optimal ART adherence [20]. Thus, individuals who worked away from their homes tended to be poorly adherent to treatment in comparison with those who did not.
Additionally, the recent use of alcohol or other stimulants has been a major barrier to ART adherence. Our findings were consistent with other research in the United States, Africa and Uganda [21,22,23,24]. The non-adherence in men with frequent use of alcohol was due to cognitive impairment and the intentional skipping of medication when drinking [25]. To sum up, having a comprehensive understanding of patients’ behaviors which lead to their poor adherence could be informative in intervening treatment and medication scheduling.
The direct interview method in our research minimized the ability of question misunderstanding and data replication. Besides, our investigation took reference from established and prevalent questionnaires which were considered to be effective in the assessment. In addition, the relatively large sample size allowed us to have statistical efficiency in examining ART-related factors in a multivariable regression analysis. Yet, the data might not be generalized at the national level since we conducted our investigation on one provincial hospital. Additionally, selection bias may have occurred in our study due to the exclusion of lost-to-follow-up patients with HIV and non-participating patients. These non-participants may require special attention after this study; a follow-up study will focus on psychological barriers and stigmatization of this group of patients.
The identification of factors associated with non-adherence in patients plays a critical role in addressing ART-related issues. Our research showed that various reasons contribute to non-adherence, e.g., drug abuse, being away from home and medication’s adverse effects. Thus, understanding those barriers could have major benefits for both the patients and healthcare providers in strengthening HIV care and treatment strategies. Further research should consider more methods and approaches as well as strategies of management to improve treatment adherence in HIV patients.
5. Conclusions
Three-quarters of patients were adherent to ART in southern Vietnam. Various factors were demonstrated to be correlated with patients’ adherence. Researchers should consider these determinants of adherence in developing interventions in further studies to improve treatment outcomes.
6. Patents
This section is not mandatory but may be added if there are patents resulting from the work reported in this manuscript.
Acknowledgments
We would like to send our gratitude to all of the patients who participated in the survey and to all other colleagues and medical staff at the clinic for supporting us in this research.
Author Contributions
A.N.T., P.M.N. and T.N. were responsible for the study concept and study design. A.N.T. and T.N. were involved in data acquisition. All authors (P.M.N., A.N.T., X.D.P., A.N.L., T.N.P.N., C.X.D., L.V.N., T.H.N., S.T.P., K.T., and T.N.) were involved in analysis and interpretation of data. A.N.T., P.M.N. and T.N. drafted the manuscript, and all authors revised it critically for important intellectual content. A.N.T., P.M.N. and T.N. are guarantors and take full responsibility for the integrity of the data and the accuracy of the data analysis. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical approval for this study was obtained from the Medical Ethics Councils of Can Tho University of Medicine and Pharmacy and the provincial hospital (Approval number: 21/HDDD) in February 2019.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data sharing is not applicable.
Conflicts of Interest
The authors declare that there is no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Global HIV & AIDS Statistics—2020 Fact Sheet. Unaids.org. [(accessed on 12 August 2020)]; Available online: https://www.unaids.org/en/resources/fact-sheet.
- 2.UNAIDS Data 2020. Unaids.org. [(accessed on 12 August 2020)]; Available online: https://www.unaids.org/en/resources/documents/2020/unaids-data.
- 3.Vietnam Ministry of Health . Report on Results of HIV/AIDS Prevention and Control in 2019 and Key Tasks in 2020. Vietnam Ministry of Health; Hanoi, Vietnam: 2020. [Google Scholar]
- 4.Schaecher K.L. The importance of treatment adherence in HIV. Am. J. Manag. Care. 2013;19(Suppl. 12):s231–s237. [PubMed] [Google Scholar]
- 5.Shrestha R., Altice F.L., Copenhaver M.M. HIV-related stigma, motivation to adhere to antiretroviral therapy, and medication adherence among HIV-positive methadone-maintained patients. J. Acquir. Immune Defic. Syndr. 2019;80:166–173. doi: 10.1097/QAI.0000000000001891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tennant S.J., Hester E.K., Caulder C.R., Lu Z.K., Bookstaver P.B. Adherence among rural HIV-infected patients in the deep south: A comparison between single-tablet and multi-tablet once-daily regimens. J. Int. Assoc. Provid. AIDS Care. 2015;14:64–71. doi: 10.1177/2325957414555228. [DOI] [PubMed] [Google Scholar]
- 7.Monnette A., Zhang Y., Shao H., Shi L. Concordance of adherence measurement using self-reported adherence questionnaires and medication monitoring devices: An updated review. Pharmacoeconomics. 2018;36:17–27. doi: 10.1007/s40273-017-0570-9. [DOI] [PubMed] [Google Scholar]
- 8.Vale F.C., Santa-Helena E.T.D., Santos M.A., Carvalho W.M.D.E.S., Menezes P.R., Basso C.R., Silva M.H., Alves A.M., Nemes M.I.B. Development and validation of the WebAd-Q Questionnaire to monitor adherence to HIV therapy. Rev. Saude Publica. 2018;52:62. doi: 10.11606/S1518-8787.2018052000337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Du T.N. Bachelor’s Thesis. Can Tho University of Medicine and Pharmacy; Can Tho City, Vietnam: 2015. Study the Adherence of Antiretroviral Therapy and other Relevant Factors in HIV/AIDS Patients at Can Tho Preventive Health Center, Ninh Kieu District, Can Tho City in 2014. [Google Scholar]
- 10.Ministry of Health of Vietnam . Guidance on HIV Treatment and Care. Ha Noi Medical Publishing House; Ha Noi City, Vietnam: 2019. [(accessed on 12 August 2020)]. Clinical Guideline. Available online: http://vaac.gov.vn/Cms_Data/Contents/Vaac/Folders/DocumentLaw/Vanban/~contents/FGV2HFDVQ9CURN2F/Huong-dan-Dieu-tri-va-cham-soc-HIV-dang-web.pdf. [Google Scholar]
- 11.Bukenya D., Mayanja B.N., Nakamanya S., Muhumuza R., Seeley J. What causes non-adherence among some individuals on long term antiretroviral therapy? Experiences of individuals with poor viral suppression in Uganda. AIDS Res. Ther. 2019;16:2. doi: 10.1186/s12981-018-0214-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Inzaule S.C., Hamers R.L., Kityo C., Rinke de Wit T.F., Roura M. Long-term antiretroviral treatment adherence in HIV-infected adolescents and adults in Uganda: A qualitative study. PLoS ONE. 2016;11:e0167492. doi: 10.1371/journal.pone.0167492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.George S., McGrath N. Social support, disclosure and stigma and the association with non-adherence in the six months after antiretroviral therapy initiation among a cohort of HIV-positive adults in rural KwaZulu-Natal, South Africa. AIDS Care. 2019;31:875–884. doi: 10.1080/09540121.2018.1549720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dan N.H. Master’s Thesis. Can Tho University of Medicine and Pharmacy; Can Tho City, Vietnam: 2012. Investigating the ART Adherence Rate of HIV/AIDS Patients in an Outpatient Clinic of Vinh Long General Hospital in 2012. [Google Scholar]
- 15.Nam V.T. Determination of rates and factors related to adherence to ART in HIV/AIDS patients in Can Tho City in 2009; Proceedings of the 4th National Scientific Conference on HIV/AIDS; Ha Noi City, Vietnam. 2–3 December 2010; Ha Noi City, Vietnam: Ministry of Health of Vietnam; 2019. [Google Scholar]
- 16.Quy N.N. Master’s Thesis. Ha Noi University of Pharmacy; Ha Noi City, Vietnam: 2018. Investigating the ARV Drug Usage and Adherence of Patients at an Outpatient Department in Tran Yen–Yen Bai Health Centre. [Google Scholar]
- 17.Xuyen N.T. Master’s Thesis. Ha Noi University of Pharmacy; Ha Noi City, Vietnam: 2017. Survey the Use of ARV Drug and Adherence of Patients at an Outpatient Clinic in Bac Giang Center for Disease Control. [Google Scholar]
- 18.Hamilton M.M., Razzano L.A., Martin N.B. The relationship between type and quality of social support and HIV medication adherence. J. HIV AIDS Soc. Serv. 2007;6:39–63. doi: 10.1300/J187v06n01_04. [DOI] [Google Scholar]
- 19.Roberts S.T., Nair G., Baeten J.M., Palanee-Philips T., Schwartz K., Reddy K., Kabwigu S., Kiweewa F.M., Govender V., Gaffoor Z., et al. Impact of male partner involvement on women’s adherence to the dapivirine vaginal ring during a phase III HIV prevention trial. AIDS Behav. 2020;24:1432–1442. doi: 10.1007/s10461-019-02707-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turan B., Rice W.S., Crockett K.B., Johnson M., Neilands T.B., Ross S.N., Kempf M.C., Konkle-Parker D., Wingood G., Tien P.C., et al. Longitudinal association between internalized HIV stigma and antiretroviral therapy adherence for women living with HIV: The mediating role of depression. AIDS. 2019;33:571–576. doi: 10.1097/QAD.0000000000002071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosen M.I., Black A.C., Arnsten J.H., Goggin K., Remien R.H., Simoni J.M., Golin C.E., Bangsberg D.R., Liu H. Association between use of specific drugs and antiretroviral adherence: Findings from MACH 14. AIDS Behav. 2013;17:142–147. doi: 10.1007/s10461-011-0124-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heestermans T., Browne J.L., Aitken S.C., Vervoort S.C., Klipstein-Grobusch K. Determinants of adherence to antiretroviral therapy among HIV-positive adults in sub-Saharan Africa: A systematic review. BMJ Glob. Health. 2016;1:e000125. doi: 10.1136/bmjgh-2016-000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sohler N., Slawek D., Earnshaw V., Jost J., Lee A., Mancini J., Mompremier A., Cunningham C.O. Drug use and HIV medication adherence in people living with HIV. Subst. Abus. 2020:1–7. doi: 10.1080/08897077.2019.1706695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sileo K.M., Kizito W., Wanyenze R.K., Chemusto H., Reed E., Stockman J.K., Musoke W., Mukasa B., Kiene S.M. Substance use and its effect on antiretroviral treatment adherence among male fisherfolk living with HIV/AIDS in Uganda. PLoS ONE. 2019;14:e0216892. doi: 10.1371/journal.pone.0216892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sileo K.M., Kizito W., Wanyenze R.K., Chemusto H., Musoke W., Mukasa B., Kiene S.M. A qualitative study on alcohol consumption and HIV treatment adherence among men living with HIV in Ugandan fishing communities. AIDS Care. 2019;31:35–40. doi: 10.1080/09540121.2018.1524564. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable.