Abstract
Organoids are three-dimensional structures that are derived from the self-organization of stem cells as they differentiate in vitro. The plasticity of stem cells is one of the major criteria for generating organoids most similar to the tissue structures they intend to mimic. Stem cells are cells with unique properties of self-renewal and differentiation. Depending on their origin, a distinction is made between pluripotent (embryonic) stem cells (PSCs), adult (or tissue) stem cells (ASCs), and those obtained by somatic reprogramming, so-called induced pluripotent stem cells (iPSCs). While most data since the 1980s have been acquired in the mouse model, and then from the late 1990s in humans, the process of somatic reprogammation has revolutionized the field of stem cell research. For domestic animals, numerous attempts have been made to obtain PSCs and iPSCs, an approach that makes it possible to omit the use of embryos to derive the cells. Even if the plasticity of the cells obtained is not always optimal, the recent progress in obtaining reprogrammed cells is encouraging. Along with PSCs and iPSCs, many organoid derivations in animal species are currently obtained from ASCs. In this study, we present state-of-the-art stem cell research according to their origins in the various animal models developed.
Keywords: Pluripotent stem cells, Adult stem cells, Induced pluripotent stem cells, Organoids
Introduction
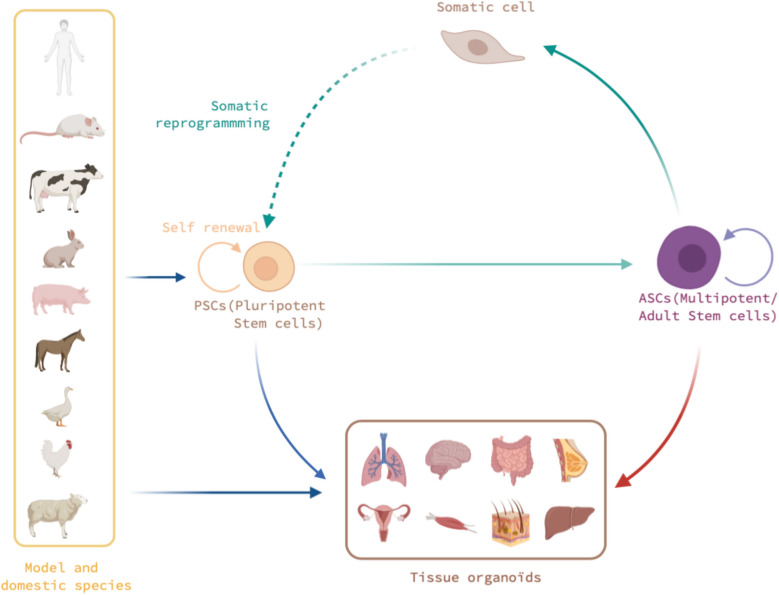
In part I, we present a summary of the state-of-the-art models of pluripotent stem cells (PSCs), adult stem cells (ASCs), and stem cells induced in two original murine and human models with the data available in the mammalian agricultural domestic species of interest, and also in birds. A schematic figure illustrates the interactions between stem cells, organoids, and species (Figure 1). In part II, we summarize the main fields of application of organoids, the use of which will be described in more detail in the following chapters, which are dedicated to several tissues of interest.
Figure 1.
Schematic illustration of the various stem cells that could be used to generate 3D organoids, depending on their origin and species. Pluripotent stem cells (PSCs) exhibit unique self-renewal and differentiation properties. Derived from embryos or obtained through somatic reprogramming, PSCs have been obtained in model species (human, rodents) and in some domestic birds and mammals. Currently, the PSCs isolated from these mammalian species do not exhibit the same cell plasticity or differentiation properties as those of model and avian species. Multipotent stem cells are usually assimilated to the adult stem cells (ASCs) found in embryonic and adult tissues, such as hematopoietic, intestinal, neural, or dermal stem cells. These cells are presently the major sources for deriving organoids in domestic animals. Among the organoids of interest, we will illustrate in the next chapters of this review those developed for the brain, intestines, liver, lungs, mammary glands, muscles, reproductive system, and skin.
Part I: organoids and 3D structures established in mouse and human models
Definition
An organoid is defined as a three-dimensional structure that self-organizes from a PSC or an ASC and has the capacity to self-renew and to differentiate to give rise to the different constitutive morphotypes of the tissue it aims to mimic and to reproduce at least some of its physiological functions. This functional notion becomes preponderant in the definition of an organoid derived from stem cells and differentiates organoids from explants, which maintain the preexisting functions of an already developed tissue. This same notion of functionality of organoids also differentiates them from embryoid bodies, obtained by the aggregation of PSC cells but according to a mode of non-directed differentiation and which do not self-organize. Different types of stem cells can generate organoids, depending on their developmental or tissue origin [1]. In a very general description, the main steps to generate an organoid are the initial proliferation of stem and precursor cells in a 3D structure and then their induction in an environment which allows it to differentiate under the effect of inducers (media, growth factors, chemical molecules, etc. …). These changes in culture conditions are either put together or sequentially to guide stem cell differentiation. The whole process ensures the development and maturation of the organoid which then presents several cellular morphtypes representative of the tissue. Cancer stem cells can also help produce 3D tumors in certain conditions, but are not considered in the context presented here.
Embryonic PSCs
One of the goals of cell culture is to mimic the functions of the tissue from which the cells are taken. Whether it is healthy or pathological tissue, the objective is to have an in vitro model to study the physiological functions or the pathological state of the tissue. Numerous cell lines have been isolated and characterized, including stem cells derived either from embryos to obtain embryonic stem cells (ESCs) or from tissues to obtain ASCs. ESCs were first isolated in the 1980s in the mouse model [2, 3]. Characterized by their self-renewal and their potential for differentiation in vitro, mouse ESCs (mESCs) also have the unique property of contributing to the somatic and germinal chimerism of an embryo when they are injected into a preimplantation blastocyst. Non-human and human primate ESCs were first obtained in the 1990s [4, 5] from the culture of preimplantation embryos. The culture conditions remain the critical point in the establishment of these cells and their plasticity, depending on the species. In the 2000s, epiblast stem cells (EpiSCs) were isolated from a postimplantation mouse embryo [6, 7]. These cells no longer have the property of contributing to chimerism in vivo even if they retain the properties of differentiating in vitro in the three embryonic lineages (the ectoderm, the endoderm, and the mesoderm). This property of colonization of the embryo and, in particular, of germinal colonization is currently considered as one of the most stringent criteria, making it possible to distinguish ESCs in a state known as “naive” versus the “primed” state, whose archetype are EpiSCs [8]. Numerous publications have characterized these two types of stem cells, which also differ in their culture conditions and in their molecular and epigenetic characterization [9–11].
The existence of these same stages in species other than rodents is still widely debated, especially in human and non-human primate models, for which many works have tried to define culture conditions to obtain and maintain naive cells [12]. In particular, the use of different cocktails of small molecules that inhibit signaling pathways have been described, which make it possible to obtain naive cells [13–15].
In other species, ESCs have been isolated, but this strict definition of germ colonization is currently restricted to rodents. We can therefore undoubtedly qualify these cells as embryonic stem (ES)-like cells in the absence of this fundamental property, in particular for mammalian species other than rodents. These “ES-like” cells have been isolated, amplified, and established in lines with self-renewal and differentiation properties in many species, including agricultural species such as pigs [16–19], cows [20, 21], sheep and goats [22–24], horses [25, 26] and rabbits [27, 28]. PSCs have been obtained and validated in birds, such as chickens [29, 30], and in fish such as medaka [31, 32] and zebrafish [33]. Most of these cells were characterized by their proliferation and differentiation potential in vitro and by the presence of certain markers, such as surface antigens, including SSEA1, SSEA3, and SSEA4, antigens initially identified in mice but whose cross-reactivity with other species has been found to be important in identifying these cells [34, 35]. Among these cells, very few have the property of colonization of the embryo, even at the somatic level, with the notable exceptions of chicken [29, 30] and zebrafish cells [33].
More recently, using strategies similar to those developed for human cells based on cocktails of inhibitory molecules, studies have been conducted of obtaining ESCs in bovine and porcine species even if chimera experiments were not reported [18, 20, 21]. In addition, recent molecular analyses carried out at the level of cells isolated from preimplantation embryos have made it possible to better define the markers associated with these early stages in species such as cattle, pigs, and rabbits and to compare them with mouse, primate, and human models [36–38]. These studies should help the development of cells with properties close to or identical in their developmental properties to those of murine naive cells.
Adult stem cells
ASCs are multipotent cells that can generate all the specialized cell types that are present in the specific tissue or organ from which they have been isolated. They have been isolated progressively from most human tissues because of the characterization of numerous markers specific to each tissue niche. Hematopoietic stem cells were the first to be identified, purified, and characterized in the 1960s by the pioneering work of Till and McCullough [39]. Mesenchymal stem cells were also very quickly identified in the same bone marrow tissue, and their presence in a multitude of tissues was confirmed subsequently, even if the nature of the markers to identify them varies. Neural stem cells were also identified in the 1960s from fetal brain tissue and later, in the 1990s, in adult brain tissue. The isolation of neurospheres under well-defined culture media conditions allowed their culture [40]. Progressively, stem cells from other tissues have been isolated and characterized, notably with the pioneering work of H. Clevers on the intestinal and epithelial stem cells of numerous organs and the identification of LGR5 as a marker for many of these cells [41]. To date, stem cells have been identified in most organs [42, 43], including the skin [44], muscles [45], the intestine [46], the liver [47], the lungs [48, 49], the mammary glands [50], and the reproductive system, for which the reproductive cells also have very particular properties of self-renewal and differentiation. Organoids derived from ASCs are generated without genetic modification by transcription factors, unlike organoids derived from iPSCs.
Induced PSCs
The arrival of somatic reprogramming technology in 2006 truly revolutionized the field of stem cell research [51–53]. Induced PSCs (iPSCs) share properties similar to ESCs without the inconvenience of the ethical issues (at least for the human species). Initially demonstrated in the mouse model, the concept was extended quickly to non-human primates, humans [54], and many other species, including rabbits [55, 56], sheep and cattle [57–60], pigs [18, 61–63], dogs [64, 65], cats [66], horses [67, 68], and even some endangered species such as the snow leopard [69]. However, in these animal species, it is difficult to validate the status of the reprogrammed cells [70] because the developmental potential of the reprogrammed cells is rarely tested. In non-mammalian species, the results are scarcer for avian cells [71–73] and tests on other species [72]. Nevertheless, the main interest in iPSCs, in particular for humans but also for agricultural species, lies in obtaining cells with properties similar to ESCs, but without going through the derivation from embryos. Even if the conditions of derivation and maintenance by different culture media are not yet conducive to obtaining the most plastic cells possible in agricultural species, progress is being made constantly, providing hope to obtaining such cells in a timely and reasonable manner.
The concept of somatic reprogramming is to introduce a cocktail of genes –including transcription factors involved in the control of pluripotency–into a somatic cell, thus leading to its reprogramming to a pluripotent cell. The first canonical combination (OSKM, OCT4, SOX2, KLF4, and c-MYC genes) was described by S. Yamanaka’s team in 2006. Subsequently, other combinations and genes have been identified gradually, such as the OCT4, SOX2, NANOG, and LIN28 (OSNL) combination [54] and actors such as Nr5a2 [74], ESRRB [75], GLIS1 [76], ZIC3 [77], TBX3 [78], H1f00 [79], NKX3.2 [80], and miR302 [81]. These factors either participate directly in the reprogramming process or increase the reprogramming efficiency [82, 83]. Surprisingly, it was recently reported that the absence of OCT4 may favor reprogramming [84]. The mechanisms controlling the epigenetic barriers that exist between somatic and pluripotent cells have also been taken into account to better understand and facilitate reprogramming [85–87]. Many methods and molecules have been described to have a positive or negative impact in the reprogramming stages [88–90].
Initial establishment of organoids
The self-renewing and differentiating properties of ESCs or iPSCs as well as ASCs are the two critical properties for the generation of organoids. The pioneering work of the laboratory of Y. Sasai [91] and then of H. Clevers [41] was quickly popularized by the development of numerous approaches for the production of organoids in most tissues. Initially developed from tissue stem cells, more complex protocols also appeared from PSCs. Most of these studies were carried out in mouse and human models and, so far, little data are available for other species, especially those of agricultural interest [92].
In this review, we focus on the achievements and projects carried out in non-human and rodent species, with special focus on species of agricultural interest.
Part II: biological issues addressed by 3D organoids
In recent years, the significant development of 3D organoid approaches has allowed various applications. Human organoids were first presented as tools to study tissue development with pioneering achievements (retina, intestine, etc.) [93]. Soon after, they were used as models to mimic and reproduce certain pathologies in vitro [43, 94]. In particular, the development of brain organoids has paved the way for the modeling of many neurodegenerative pathologies, for which access to brain tissue is almost impossible. The possibility of deriving reprogrammed human-induced PSCs (hiPSCs) from patient biopsies, modifying them, and obtaining isogenic cells by reversing mutations through genome editing approaches, for example, has also allowed numerous studies and publications for a large spectrum of pathologies that affect the nervous system [94–98]. The same hiPSCs from patients with genetic diseases have been used to generate brain organoids and to model the impact of the mutation that is observed in the patient during the development of these structures with examples such as the RETT syndrome or amyotrophic lateral sclerosis [97–99].
If the analysis of mutations is a privileged axis at both the developmental and pathological levels for congenital genetic alterations in particular, the organoid approach also makes a contribution to obtain models for studies in oncology, in particular, through the potential development of personalized medicine to adapt treatment for individual patients with cancer. This new methodology has already been implemented in the intestine, kidney, prostate, ovary, bladder, pancreas, liver, breast, and brain [100–103] and new models and uses are likely to emerge. Through the development of tumoroids derived from patient biopsies, it may be possible to test the most efficient molecules on diseased organoids in parallel with healthy organoids obtained from the same patient and therefore to better adapt a targeted antitumor treatment and target tumoral cells in the patients. The published results are encouraging [104–106]. Unthinkable only a few years ago, the first demonstrations are underway to screen certain anticancer agents and adapt treatment to each patient.
Owing to their near-physiological state, organoids are promising innovative tools for toxicological studies. Their low ethical concerns, as compared with in vivo animal studies, also argue in favor of their use in this field. They have already been used to assess the toxicity of many substances in humans. It is probable that animal-based organoids will also be used more widely in the future to predict the adverse effects of drugs in the target species. Similarly, toxicological screening approaches are particularly concerned by this 3D organoid approach to better define the toxicological threshold of a molecule in an environment different from that of an adherent line or culture without complexity, therefore trying to fit with what is observed in a tissue. If the difficulty is to operate with a “floating” structure and one that takes longer to obtain than the simple seeding of an adherent cell line, the answers are more relevant as to the availability of the molecules tested within the tissue.
Studies of infectious diseases have been limited by the paucity of functional models that mimic normal physiology and pathophysiology in a species-specific manner. The development of brain, lung, and intestine organoids, among others, of human and animal species constitutes a considerable advance that facilitates studies of host–pathogen interactions. Breakthroughs in their understanding, for viruses as well as bacteria and parasites, are greatly expected. In the dedicated sections, examples will be given of some of the major discoveries that have been made in this field thanks to organoids. Another area that has received special attention is the development of approaches to study pathogen–host relationships, whether these pathogens are bacteria [107], parasites [108], or viruses [109, 110], by targeting different tissue models via brain organoids [109], intestinal organoids [111], or pulmonary organoids [107, 111, 112], among others. For example, approaches to the infection of cerebral organoids by the Zika virus have highlighted the tropism of this virus for neuronal precursors and therefore make an a priori link with the microcephaly observed in infants following the infection of mothers [109, 113, 114]. More recently, the same approach was put forward to follow the impact of the viral spread of largely unknown viruses, such as SARS-Cov-2. The tissue complexity reproduced at the organoid scale makes it possible to study the propagation of the pathogen in all the tissue components, in particular to reproduce the kinetics of contamination [115–117]. In an original manner, the organoids, in this case intestinal, can make it possible to compare different susceptibilities to SARS-Cov-2 between human and bat models [118]. Mention should also be made of studies on microbiota–host interactions, whether these are normal or pathogenic. The study of microbiota has become important in many developmental and pathological aspects and in several tissues, although the intestine remains the reference tissue for these approaches. The skin, the lungs, etc., also have their own microbiota and having in vitro models to test the balance and imbalance of these ecosystems is relevant.
Conclusion
In the rapidly developing field of organoids, the human model is still the most studied, but many new developments concern agricultural animals. At this level, having physiological in vitro models that closely mimic whole tissues, but are different from explants that require repeated biopsies, will be an advantage. The development of organoids also responds to the increasingly significant and important societal demand to limit animal testing.
Acknowledgements
We thank A. Jouneau and M. Coulpier for their valuable comments and S. Campredon for the Figure.
Abbreviations
- ASCs
Adult stem cells
- EpiSCs
Epiblast stem cells
- ESCs
Embryonic stem cells
- iPSCs
Induced pluripotent stem cells
- PSCs
Pluripotent stem cells
Authors’ contributions
BP wrote the manuscript. The author read and approved the final manuscript.
Funding
This work was supported by grants from ANR, the project CRB-ANIM-ANR-11-INBS-0003 to BP.
Competing interests
The author declares that he has no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rossi G, Manfrin A, Lutolf MP. Progress and potential in organoid research. Nat Rev Genet. 2018;19(11):671–687. doi: 10.1038/s41576-018-0051-9. [DOI] [PubMed] [Google Scholar]
- 2.Evans MJ, Kaufman MH. Establishment in culture of pluripotential cells from mouse embryos. Nature. 1981;292:154–156. doi: 10.1038/292154a0. [DOI] [PubMed] [Google Scholar]
- 3.Martin GR. Isolation of a pluripotent cell line from early mouse embryos cultured in medium conditioned by teratocarcinoma stem cells. Proc Natl Acad Sci USA. 1981;78:7634–7638. doi: 10.1073/pnas.78.12.7634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thomson JA, Kalishman J, Golos TG, Durning M, Harris CP, Becker RA, Hearn JP. Isolation of a primate embryonic stem cell line. Proc Natl Acad Sci USA. 1995;92:7844–7848. doi: 10.1073/pnas.92.17.7844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, Marshall VS, Jones JM. Embryonic stem cell lines derived from human blastocysts. Science. 1998;282:1145–1147. doi: 10.1126/science.282.5391.1145. [DOI] [PubMed] [Google Scholar]
- 6.Tesar PJ, Chenoweth JG, Brook FA, Davies TJ, Evans EP, Mack DL, Gardner RL, McKay RD. New cell lines from mouse epiblast share defining features with human embryonic stem cells. Nature. 2007;448:196–199. doi: 10.1038/nature05972. [DOI] [PubMed] [Google Scholar]
- 7.Brons IG, Smithers LE, Trotter MW, Rugg-Gunn P, Sun B, de Sousa C, Lopes SM, Howlett SK, Clarkson A, Ahrlund-Richter L, Pedersen RA, Vallier L. Derivation of pluripotent epiblast stem cells from mammalian embryos. Nature. 2007;448:191–195. doi: 10.1038/nature05950. [DOI] [PubMed] [Google Scholar]
- 8.Nichols J, Smith A. Naive and primed pluripotent states. Cell Stem Cell. 2009;4:487–492. doi: 10.1016/j.stem.2009.05.015. [DOI] [PubMed] [Google Scholar]
- 9.Martello G, Sugimoto T, Diamanti E, Joshi A, Hannah R, Ohtsuka S, Göttgens B, Niwa H, Smith A. Esrrb is a pivotal target of the Gsk3/Tcf3 axis regulating embryonic stem cell self-renewal. Cell Stem Cell. 2012;11:491–504. doi: 10.1016/j.stem.2012.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marks H, Kalkan T, Menafra R, Denissov S, Jones K, Hofemeister H, Nichols J, Kranz A, Stewart AF, Smith A, Stunnenberg HG. The transcriptional and epigenomic foundations of ground state pluripotency. Cell. 2012;149:590–604. doi: 10.1016/j.cell.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tosolini M, Brochard V, Adenot P, Chebrout M, Grillo G, Navia V, Beaujean N, Francastel C, Bonnet-Garnier A, Jouneau A. Contrasting epigenetic states of heterochromatin in the different types of mouse pluripotent stem cells. Sci Rep. 2018;8:5776. doi: 10.1038/s41598-018-23822-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nakamura T, Okamoto I, Sasaki K, Yabuta Y, Iwatani C, Tsuchiya H, Seita Y, Nakamura S, Yamamoto T, Saitou M. A developmental coordinate of pluripotency among mice, monkeys and humans. Nature. 2016;537:57–62. doi: 10.1038/nature19096. [DOI] [PubMed] [Google Scholar]
- 13.Gafni O, Weinberger L, Mansour AA, Manor YS, Chomsky E, Ben-Yosef D, Kalma Y, Viukov S, Maza I, Zviran A, Rais Y, Shipony Z, Mukamel Z, Krupalnik V, Zerbib M, Geula S, Caspi I, Schneir D, Shwartz T, Gilad S, Amann-Zalcenstein D, Benjamin S, Amit I, Tanay A, Massarwa R, Novershtern N, Hanna JH. Derivation of novel human ground state naive pluripotent stem cells. Nature. 2013;504:282–286. doi: 10.1038/nature12745. [DOI] [PubMed] [Google Scholar]
- 14.Guo G, von Meyenn F, Santos F, Chen Y, Reik W, Bertone P, Smith A, Nichols J. Naive pluripotent stem cells derived directly from isolated cells of the human inner cell mass. Stem Cell Rep. 2016;6:437–446. doi: 10.1016/j.stemcr.2016.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bredenkamp N, Yang J, Clarke J, Stirparo GG, von Meyenn F, Dietmann S, Baker D, Drummond R, Ren Y, Li D, Wu C, Rostovskaya M, Eminli-Meissner S, Smith A, Guo G. Wnt inhibition facilitates RNA-mediated reprogramming of human somatic cells to naive pluripotency. Stem Cell Rep. 2019;13:1083–1098. doi: 10.1016/j.stemcr.2019.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park JK, Kim HS, Uh KJ, Choi KH, Kim HM, Lee T, Yang BC, Kim HJ, Ka HH, Kim H, Lee CK. Primed pluripotent cell lines derived from various embryonic origins and somatic cells in pig. PLoS ONE. 2013;8:e52481. doi: 10.1371/journal.pone.0052481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hou DR, Jin Y, Nie XW, Zhang ML, Ta N, Zhao LH, Yang N, Chen Y, Wu ZQ, Jiang HB, Li YR, Sun QY, Dai YF, Li RF. Derivation of porcine embryonic stem-like cells from in vitro-produced blastocyst-stage embryos. Sci Rep. 2016;6:25838. doi: 10.1038/srep25838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gao X, Nowak-Imialek M, Chen X, Chen D, Herrmann D, Ruan D, Chen ACH, Eckersley-Maslin MA, Ahmad S, Lee YL, Kobayashi T, Ryan D, Zhong J, Zhu J, Wu J, Lan G, Petkov S, Yang J, Antunes L, Campos LS, Fu B, Wang S, Yong Y, Wang X, Xue SG, Ge L, Liu Z, Huang Y, Nie T, Li P, Wu D, Pei D, Zhang Y, Lu L, Yang F, Kimber SJ, Reik W, Zou X, Shang Z, Lai L, Surani A, Tam PPL, Ahmed A, Yeung WSB, Teichmann SA, Niemann H, Liu P. Establishment of porcine and human expanded potential stem cells. Nat Cell Biol. 2019;21:687–699. doi: 10.1038/s41556-019-0333-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Choi KH, Lee DK, Oh JN, Kim SH, Lee M, Woo SH, Kim DY, Lee CK. Pluripotent pig embryonic stem cell lines originating from in vitro-fertilized and parthenogenetic embryos. Stem Cell Res. 2020;49:102093. doi: 10.1016/j.scr.2020.102093. [DOI] [PubMed] [Google Scholar]
- 20.Wu X, Song M, Yang X, Liu X, Liu K, Jiao C, Wang J, Bai C, Su G, Liu X, Li G. Establishment of bovine embryonic stem cells after knockdown of CDX2. Sci Rep. 2016;6:28343. doi: 10.1038/srep28343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bogliotti YS, Wu J, Vilarino M, Okamura D, Soto DA, Zhong C, Sakurai M, Sampaio RV, Suzuki K, Izpisua Belmonte JC, Ross PJ. Efficient derivation of stable primed pluripotent embryonic stem cells from bovine blastocysts. Proc Natl Acad Sci USA. 2018;115:2090–2095. doi: 10.1073/pnas.1716161115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Kumar A, Malakar D, Akshey YS, Jena MK, Dutta R. Isolation and characterization of embryonic stem cell-like cells from in vitro produced goat (Capra hircus) embryos. Anim Biotechnol. 2011;22:181–196. doi: 10.1080/10495398.2011.622189. [DOI] [PubMed] [Google Scholar]
- 23.Behboodi E, Bondareva A, Begin I, Rao K, Neveu N, Pierson JT, Wylie C, Piero FD, Huang YJ, Zeng W, Tanco V, Baldassarre H, Karatzas CN, Dobrinski I. Establishment of goat embryonic stem cells from in vivo produced blastocyst-stage embryos. Mol Reprod Dev. 2011;78:202–211. doi: 10.1002/mrd.21290. [DOI] [PubMed] [Google Scholar]
- 24.Vilarino M, Alba Soto D, Soledad Bogliotti Y, Yu L, Zhang Y, Wang C, Paulson E, Zhong C, Jin M, Carlos Izpisua Belmonte J, Wu J, Juan Ross P. Derivation of sheep embryonic stem cells under optimized conditions. Reproduction. 2020;160:761–772. doi: 10.1530/REP-19-0606. [DOI] [PubMed] [Google Scholar]
- 25.Li X, Zhou SG, Imreh MP, Ahrlund-Richter L, Allen WR. Horse embryonic stem cell-like cell lines from the proliferation of inner cell mass cells. Stem Cells Dev. 2006;15:523–531. doi: 10.1089/scd.2006.15.523. [DOI] [PubMed] [Google Scholar]
- 26.Paris DB, Stout TA. Equine embryos and embryonic stem cells: defining reliable markers of pluripotency. Theriogenology. 2010;74:516–524. doi: 10.1016/j.theriogenology.2009.11.020. [DOI] [PubMed] [Google Scholar]
- 27.Wang S, Tang X, Niu Y, Chen H, Li B, Li T, Zhang X, Hu Z, Zhou Q, Ji W. Generation and characterization of rabbit embryonic stem cells. Stem Cells. 2007;25:481–489. doi: 10.1634/stemcells.2006-0226. [DOI] [PubMed] [Google Scholar]
- 28.Tancos Z, Nemes C, Polgar Z, Gocza E, Daniel N, Stout TA, Maraghechi P, Pirity MK, Osteil P, Tapponnier Y, Markossian S, Godet M, Afanassieff M, Bosze Z, Duranthon V, Savatier P, Dinnyes A. Generation of rabbit pluripotent stem cell lines. Theriogenology. 2012;78:1774–1786. doi: 10.1016/j.theriogenology.2012.06.017. [DOI] [PubMed] [Google Scholar]
- 29.Pain B, Clark ME, Shen M, Nakazawa H, Sakurai M, Samarut J, Etches RJ. Long-term in vitro culture and characterisation of avian embryonic stem cells with multiple morphogenetic potentialities. Development. 1996;122:2339–2348. doi: 10.1242/dev.122.8.2339. [DOI] [PubMed] [Google Scholar]
- 30.Aubel P, Pain B. Chicken embryonic stem cells: establishment and characterization. Methods Mol Biol. 2013;1074:137–150. doi: 10.1007/978-1-62703-628-3_11. [DOI] [PubMed] [Google Scholar]
- 31.Hong Y, Winkler C, Schartl M. Pluripotency and differentiation of embryonic stem cell lines from the medakafish (Oryzias latipes) Mech Dev. 1996;60:33–44. doi: 10.1016/s0925-4773(96)00596-5. [DOI] [PubMed] [Google Scholar]
- 32.Hong Y, Winkler C, Liu T, Chai G, Schartl M. Activation of the mouse Oct4 promoter in medaka embryonic stem cells and its use for ablation of spontaneous differentiation. Mech Dev. 2004;121:933–943. doi: 10.1016/j.mod.2004.03.028. [DOI] [PubMed] [Google Scholar]
- 33.Fan L, Collodi P. Zebrafish embryonic stem cells. Methods Enzymol. 2006;418:64–77. doi: 10.1016/S0076-6879(06)18004-0. [DOI] [PubMed] [Google Scholar]
- 34.Koh S, Piedrahita JA. From "ES-like" cells to induced pluripotent stem cells: a historical perspective in domestic animals. Theriogenology. 2014;81:103–111. doi: 10.1016/j.theriogenology.2013.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ezashi T, Yuan Y, Roberts RM. Pluripotent stem cells from domesticated mammals. Annu Rev Anim Biosci. 2016;4:223–253. doi: 10.1146/annurev-animal-021815-111202. [DOI] [PubMed] [Google Scholar]
- 36.Bernardo AS, Jouneau A, Marks H, Kensche P, Kobolak J, Freude K, Hall V, Feher A, Polgar Z, Sartori C, Bock I, Louet C, Faial T, Kerstens HHD, Bouissou C, Parsonage G, Mashayekhi K, Smith JC, Lazzari G, Hyttel P, Stunnenberg HG, Huynen M, Pedersen RA, Dinnyes A. Mammalian embryo comparison identifies novel pluripotency genes associated with the naïve or primed state. Biol Open. 2018;7:bio033282. doi: 10.1242/bio.033282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu D, Wang X, He D, Sun C, He X, Yan L, Li Y, Han JJ, Zheng P. Single-cell RNA-sequencing reveals the existence of naive and primed pluripotency in pre-implantation rhesus monkey embryos. Genome Res. 2018;28:1481–1493. doi: 10.1101/gr.233437.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ramos-Ibeas P, Sang F, Zhu Q, Tang WWC, Withey S, Klisch D, Wood L, Loose M, Surani MA, Alberio R. Pluripotency and X chromosome dynamics revealed in pig pre-gastrulating embryos by single cell analysis. Nat Commun. 2019;10:500. doi: 10.1038/s41467-019-08387-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Becker AJ, McCulloch EA, Till JE. Cytological demonstration of the clonal nature of spleen colonies derived from transplanted mouse marrow cells. Nature. 1963;197:452–454. doi: 10.1038/197452a0. [DOI] [PubMed] [Google Scholar]
- 40.Tropepe V, Sibilia M, Ciruna BG, Rossant J, Wagner EF, van der Kooy D. Distinct neural stem cells proliferate in response to EGF and FGF in the developing mouse telencephalon. Dev Biol. 1999;208:166–188. doi: 10.1006/dbio.1998.9192. [DOI] [PubMed] [Google Scholar]
- 41.Sato T, Vries RG, Snippert HJ, van de Wetering M, Barker N, Stange DE, van Es JH, Abo A, Kujala P, Peters PJ, Clevers H. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature. 2009;459:262–265. doi: 10.1038/nature07935. [DOI] [PubMed] [Google Scholar]
- 42.Clevers H. Stem cells. What is an adult stem cell? Science. 2015;350:1319–1320. doi: 10.1126/science.aad7016. [DOI] [PubMed] [Google Scholar]
- 43.Clevers H, Watt FM. Defining adult stem cells by function, not by phenotype. Annu Rev Biochem. 2018;87:1015–1027. doi: 10.1146/annurev-biochem-062917-012341. [DOI] [PubMed] [Google Scholar]
- 44.Blanpain C, Fuchs E. Epidermal stem cells of the skin. Annu Rev Cell Dev Biol. 2006;22:339–373. doi: 10.1146/annurev.cellbio.22.010305.104357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Seale P, Asakura A, Rudnicki MA. The potential of muscle stem cells. Dev Cell. 2001;1:333–342. doi: 10.1016/s1534-5807(01)00049-1. [DOI] [PubMed] [Google Scholar]
- 46.van der Flier LG, Clevers H. Stem cells, self-renewal, and differentiation in the intestinal epithelium. Annu Rev Physiol. 2009;71:241–260. doi: 10.1146/annurev.physiol.010908.163145. [DOI] [PubMed] [Google Scholar]
- 47.Miyajima A, Tanaka M, Itoh T. Stem/progenitor cells in liver development, homeostasis, regeneration, and reprogramming. Cell Stem Cell. 2014;14:561–574. doi: 10.1016/j.stem.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 48.Barkauskas CE, Chung MI, Fioret B, Gao X, Katsura H, Hogan BL. Lung organoids: current uses and future promise. Development. 2017;144:986–997. doi: 10.1242/dev.140103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rock JR, Hogan BL. Epithelial progenitor cells in lung development, maintenance, repair, and disease. Annu Rev Cell Dev Biol. 2011;27:493–512. doi: 10.1146/annurev-cellbio-100109-104040. [DOI] [PubMed] [Google Scholar]
- 50.Inman JL, Robertson C, Mott JD, Bissell MJ. Mammary gland development: cell fate specification, stem cells and the microenvironment. Development. 2015;142:1028–1042. doi: 10.1242/dev.087643. [DOI] [PubMed] [Google Scholar]
- 51.Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–676. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 52.Takahashi K, Yamanaka S. A decade of transcription factor-mediated reprogramming to pluripotency. Nat Rev Mol Cell Biol. 2016;17:183–193. doi: 10.1038/nrm.2016.8. [DOI] [PubMed] [Google Scholar]
- 53.Karagiannis P, Eto K. Ten years of induced pluripotency: from basic mechanisms to therapeutic applications. Development. 2016;143:2039–2043. doi: 10.1242/dev.138172. [DOI] [PubMed] [Google Scholar]
- 54.Yu J, Vodyanik MA, Smuga-Otto K, Antosiewicz-Bourget J, Frane JL, Tian S, Nie J, Jonsdottir GA, Ruotti V, Stewart R, Slukvin II, Thomson JA. Induced pluripotent stem cell lines derived from human somatic cells. Science. 2007;318:1917–1920. doi: 10.1126/science.1151526. [DOI] [PubMed] [Google Scholar]
- 55.Honda A, Hatori M, Hirose M, Honda C, Izu H, Inoue K, Hirasawa R, Matoba S, Togayachi S, Miyoshi H, Ogura A. Naive-like conversion overcomes the limited differentiation capacity of induced pluripotent stem cells. J Biol Chem. 2013;288:26157–26166. doi: 10.1074/jbc.M113.502492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Osteil P, Tapponnier Y, Markossian S, Godet M, Schmaltz-Panneau B, Jouneau L, Cabau C, Joly T, Blachère T, Gócza E, Bernat A, Yerle M, Acloque H, Hidot S, Bosze Z, Duranthon V, Savatier P, Afanassieff M. Induced pluripotent stem cells derived from rabbits exhibit some characteristics of naïve pluripotency. Biol Open. 2013;2:613–628. doi: 10.1242/bio.20134242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Liu J, Balehosur D, Murray B, Kelly JM, Sumer H, Verma PJ. Generation and characterization of reprogrammed sheep induced pluripotent stem cells. Theriogenology. 2012;77:338–46.e1. doi: 10.1016/j.theriogenology.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 58.Sandmaier SE, Nandal A, Powell A, Garrett W, Blomberg L, Donovan DM, Talbot N, Telugu BP. Generation of induced pluripotent stem cells from domestic goats. Mol Reprod Dev. 2015;82:709–721. doi: 10.1002/mrd.22512. [DOI] [PubMed] [Google Scholar]
- 59.Sumer H, Liu J, Malaver-Ortega LF, Lim ML, Khodadadi K, Verma PJ. NANOG is a key factor for induction of pluripotency in bovine adult fibroblasts. J Anim Sci. 2011;89:2708–2716. doi: 10.2527/jas.2010-3666. [DOI] [PubMed] [Google Scholar]
- 60.Talluri TR, Kumar D, Glage S, Garrels W, Ivics Z, Debowski K, Behr R, Niemann H, Kues WA. Derivation and characterization of bovine induced pluripotent stem cells by transposon-mediated reprogramming. Cell Reprogram. 2015;17:131–140. doi: 10.1089/cell.2014.0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ezashi T, Telugu BP, Alexenko AP, Sachdev S, Sinha S, Roberts RM. Derivation of induced pluripotent stem cells from pig somatic cells. Proc Natl Acad Sci USA. 2009;106:10993–10998. doi: 10.1073/pnas.0905284106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rodríguez A, Allegrucci C, Alberio R. Modulation of pluripotency in the porcine embryo and iPS cells. PLoS ONE. 2012;7:e49079. doi: 10.1371/journal.pone.0049079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Congras A, Barasc H, Canale-Tabet K, Plisson-Petit F, Delcros C, Feraud O, Oudrhiri N, Hadadi E, Griscelli F, Bennaceur-Griscelli A, Turhan A, Afanassieff M, Ferchaud S, Pinton A, Yerle-Bouissou M, Acloque H. Non integrative strategy decreases chromosome instability and improves endogenous pluripotency genes reactivation in porcine induced pluripotent-like stem cells. Sci Rep. 2016;6:27059. doi: 10.1038/srep27059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shimada H, Nakada A, Hashimoto Y, Shigeno K, Shionoya Y, Nakamura T. Generation of canine induced pluripotent stem cells by retroviral transduction and chemical inhibitors. Mol Reprod Dev. 2010;77:2. doi: 10.1002/mrd.21117. [DOI] [PubMed] [Google Scholar]
- 65.Menon DV, Patel D, Joshi CG, Kumar A. The road less travelled: the efficacy of canine pluripotent stem cells. Exp Cell Res. 2019;377:94–102. doi: 10.1016/j.yexcr.2019.01.025. [DOI] [PubMed] [Google Scholar]
- 66.Dutton LC, Dudhia J, Guest DJ, Connolly DJ. Inducing pluripotency in the domestic cat (Felis catus) Stem Cells Dev. 2019;28:1299–1309. doi: 10.1089/scd.2019.0142. [DOI] [PubMed] [Google Scholar]
- 67.Nagy K, Sung HK, Zhang P, Laflamme S, Vincent P, Agha-Mohammadi S, Woltjen K, Monetti C, Michael IP, Smith LC, Nagy A. Induced pluripotent stem cell lines derived from equine fibroblasts. Stem Cell Rev Rep. 2011;7:693–702. doi: 10.1007/s12015-011-9239-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Breton A, Sharma R, Diaz AC, Parham AG, Graham A, Neil C, Bruce Whitelaw C, Milne E, Donadeu FX. Derivation and characterization of induced pluripotent stem cells from equine fibroblasts. Stem Cells Dev. 2013;22:611–621. doi: 10.1089/scd.2012.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Verma R, Liu J, Holland MK, Temple-Smith P, Williamson M, Verma PJ. Nanog is an essential factor for induction of pluripotency in somatic cells from endangered felids. Biores Open Access. 2013;21:72–76. doi: 10.1089/biores.2012.0297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.De Los AA, Ferrari F, Xi R, Fujiwara Y, Benvenisty N, Deng H, Hochedlinger K, Jaenisch R, Lee S, Leitch HG, Lensch MW, Lujan E, Pei D, Rossant J, Wernig M, Park PJ, Daley GQ. Hallmarks of pluripotency. Nature. 2015;525:469–478. doi: 10.1038/nature15515. [DOI] [PubMed] [Google Scholar]
- 71.Lu Y, West FD, Jordan BJ, Jordan ET, West RC, Yu P, He Y, Barrios MA, Zhu Z, Petitte JN, Beckstead RB, Stice SL. Induced pluripotency in chicken embryonic fibroblast results in a germ cell fate. Stem Cells Dev. 2014;23:1755–1764. doi: 10.1089/scd.2014.0080. [DOI] [PubMed] [Google Scholar]
- 72.Rosselló RA, Chen CC, Dai R, Howard JT, Hochgeschwender U, Jarvis ED. Mammalian genes induce partially reprogrammed pluripotent stem cells in non-mammalian vertebrate and invertebrate species. Elife. 2013;2:e00036. doi: 10.7554/eLife.00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fuet A, Montillet G, Jean C, Aubel P, Kress C, Rival-Gervier S, Pain B. NANOG is required for the long-term establishment of avian somatic reprogrammed cells. Stem Cell Rep. 2018;11:1272–1286. doi: 10.1016/j.stemcr.2018.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Heng JC, Feng B, Han J, Jiang J, Kraus P, Ng JH, Orlov YL, Huss M, Yang L, Lufkin T, Lim B, Ng HH. The nuclear receptor Nr5a2 can replace Oct4 in the reprogramming of murine somatic cells to pluripotent cells. Cell Stem Cell. 2010;6:167–174. doi: 10.1016/j.stem.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 75.Feng B, Jiang J, Kraus P, Ng JH, Heng JC, Chan YS, Yaw LP, Zhang W, Loh YH, Han J, Vega VB, Cacheux-Rataboul V, Lim B, Lufkin T, Ng HH. Reprogramming of fibroblasts into induced pluripotent stem cells with orphan nuclear receptor Esrrb. Nat Cell Biol. 2009;11:197–203. doi: 10.1038/ncb1827. [DOI] [PubMed] [Google Scholar]
- 76.Maekawa M, Yamaguchi K, Nakamura T, Shibukawa R, Kodanaka I, Ichisaka T, Kawamura Y, Mochizuki H, Goshima N, Yamanaka S. Direct reprogramming of somatic cells is promoted by maternal transcription factor Glis1. Nature. 2011;474:225–229. doi: 10.1038/nature10106. [DOI] [PubMed] [Google Scholar]
- 77.Declercq J, Sheshadri P, Verfaillie CM, Kumar A. Zic3 enhances the generation of mouse induced pluripotent stem cells. Stem Cells Dev. 2013;22:2017–2025. doi: 10.1089/scd.2012.0651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Han J, Yuan P, Yang H, Zhang J, Soh BS, Li P, Lim SL, Cao S, Tay J, Orlov YL, Lufkin T, Ng HH, Tam WL, Lim B. Tbx3 improves the germ-line competency of induced pluripotent stem cells. Nature. 2010;463:1096–1100. doi: 10.1038/nature08735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kunitomi A, Yuasa S, Sugiyama F, Saito Y, Seki T, Kusumoto D, Kashimura S, Takei M, Tohyama S, Hashimoto H, Egashira T, Tanimoto Y, Mizuno S, Tanaka S, Okuno H, Yamazawa K, Watanabe H, Oda M, Kaneda R, Matsuzaki Y, Nagai T, Okano H, Yagami KI, Tanaka M, Fukuda K. H1foo has a pivotal role in qualifying induced pluripotent stem cells. Stem Cell Rep. 2016;6:825–833. doi: 10.1016/j.stemcr.2016.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mai T, Markov GJ, Brady JJ, Palla A, Zeng H, Sebastiano V, Blau HM. NKX3-1 is required for induced pluripotent stem cell reprogramming and can replace OCT4 in mouse and human iPSC induction. Nat Cell Biol. 2018;20:900–908. doi: 10.1038/s41556-018-0136-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Anokye-Danso F, Trivedi CM, Juhr D, Gupta M, Cui Z, Tian Y, Zhang Y, Yang W, Gruber PJ, Epstein JA, Morrisey EE. Highly efficient miRNA-mediated reprogramming of mouse and human somatic cells to pluripotency. Cell Stem Cell. 2011;8:376–388. doi: 10.1016/j.stem.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hochedlinger K, Plath K. Epigenetic reprogramming and induced pluripotency. Development. 2009;136:509–523. doi: 10.1242/dev.020867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Stadtfeld M, Hochedlinger K. Induced pluripotency: history, mechanisms, and applications. Genes Dev. 2010;24:2239–2263. doi: 10.1101/gad.1963910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Velychko S, Adachi K, Kim KP, Hou Y, MacCarthy CM, Wu G, Schöler HR. Excluding Oct4 from Yamanaka cocktail unleashes the developmental potential of iPSCs. Cell Stem Cell. 2019;25:737–753.e4. doi: 10.1016/j.stem.2019.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhuang Q, Li W, Benda C, Huang Z, Ahmed T, Liu P, Guo X, Ibañez DP, Luo Z, Zhang M, Abdul MM, Yang Z, Yang J, Huang Y, Zhang H, Huang D, Zhou J, Zhong X, Zhu X, Fu X, Fan W, Liu Y, Xu Y, Ward C, Khan MJ, Kanwal S, Mirza B, Tortorella MD, Tse HF, Chen J, Qin B, Bao X, Gao S, Hutchins AP, Esteban MA. NCoR/SMRT co-repressors cooperate with c-MYC to create an epigenetic barrier to somatic cell reprogramming. Nat Cell Biol. 2018;20:400–412. doi: 10.1038/s41556-018-0047-x. [DOI] [PubMed] [Google Scholar]
- 86.Miles DC, de Vries NA, Gisler S, Lieftink C, Akhtar W, Gogola E, Pawlitzky I, Hulsman D, Tanger E, Koppens M, Beijersbergen RL, van Lohuizen M. TRIM28 is an epigenetic barrier to induced pluripotent stem cell reprogramming. Stem Cells. 2017;35:147–157. doi: 10.1002/stem.2453. [DOI] [PubMed] [Google Scholar]
- 87.Chen J, Wang Y, Wang C, Hu JF. Li W (2020) LncRNA functions as a new emerging epigenetic factor in determining the fate of stem cells. Front Genet. 2020;11:277. doi: 10.3389/fgene.2020.00277.eCollection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.David L, Polo JM. Phases of reprogramming. Stem Cell Res. 2014;12:754–761. doi: 10.1016/j.scr.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 89.Mor N, Rais Y, Sheban D, Peles S, Aguilera-Castrejon A, Zviran A, Elinger D, Viukov S, Geula S, Krupalnik V, Zerbib M, Chomsky E, Lasman L, Shani T, Bayerl J, Gafni O, Hanna S, Buenrostro JD, Hagai T, Masika H, Vainorius G, Bergman Y, Greenleaf WJ, Esteban MA, Elling U, Levin Y, Massarwa R, Merbl Y, Novershtern N, Hanna JH. Neutralizing Gatad2a-Chd4-Mbd3/NuRD complex facilitates deterministic induction of naive pluripotency. Cell Stem Cell. 2018;23:412–425.e10. doi: 10.1016/j.stem.2018.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zviran A, Mor N, Rais Y, Gingold H, Peles S, Chomsky E, Viukov S, Buenrostro JD, Scognamiglio R, Weinberger L, Manor YS, Krupalnik V, Zerbib M, Hezroni H, Jaitin DA, Larastiaso D, Gilad S, Benjamin S, Gafni O, Mousa A, Ayyash M, Sheban D, Bayerl J, Aguilera-Castrejon A, Massarwa R, Maza I, Hanna S, Stelzer Y, Ulitsky I, Greenleaf WJ, Tanay A, Trumpp A, Amit I, Pilpel Y, Novershtern N, Hanna JH. Deterministic somatic cell reprogramming involves continuous transcriptional changes governed by Myc and epigenetic-driven modules. Cell Stem Cell. 2019;24:328–341.e9. doi: 10.1016/j.stem.2018.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Eiraku M, Watanabe K, Matsuo-Takasaki M, Kawada M, Yonemura S, Matsumura M, Wataya T, Nishiyama A, Muguruma K, Sasai Y. Self-organized formation of polarized cortical tissues from ESCs and its active manipulation by extrinsic signals. Cell Stem Cell. 2008;3:519–532. doi: 10.1016/j.stem.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 92.Augustyniak J, Bertero A, Coccini T, Baderna D, Buzanska L, Caloni F. Organoids are promising tools for species-specific in vitro toxicological studies. J Appl Toxicol. 2019;39:1610–1622. doi: 10.1002/jat.3815. [DOI] [PubMed] [Google Scholar]
- 93.Bissell MJ. Goodbye flat biology–time for the 3rd and the 4th dimensions. J Cell Sci. 2017;130:3–5. doi: 10.1242/jcs.200550. [DOI] [PubMed] [Google Scholar]
- 94.Lancaster MA, Renner M, Martin CA, Wenzel D, Bicknell LS, Hurles ME, Homfray T, Penninger JM, Jackson AP, Knoblich JA. Cerebral organoids model human brain development and microcephaly. Nature. 2013;501:373–379. doi: 10.1038/nature12517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Soldner F, Hockemeyer D, Beard C, Gao Q, Bell GW, Cook EG, Hargus G, Blak A, Cooper O, Maisam M, Isacson O, Jaenisch R. Parkinson’s disease patient-derived induced pluripotent stem cells free of viral reprogramming factors. Cell. 2009;136:964–977. doi: 10.1016/j.cell.2009.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Soldner F, Jaenisch R. Stem cells, genome editing, and the path to translational medicine. Cell. 2018;175:615–632. doi: 10.1016/j.cell.2018.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Marchetto MC, Carromeu C, Acab A, Yu D, Yeo GW, Mu Y, Chen G, Gage FH, Muotri AR. A model for neural development and treatment of Rett syndrome using human induced pluripotent stem cells. Cell. 2010;143:527–539. doi: 10.1016/j.cell.2010.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wainger BJ, Kiskinis E, Mellin C, Wiskow O, Han SS, Sandoe J, Perez NP, Williams LA, Lee S, Boulting G, Berry JD, Brown RH, Jr, Cudkowicz ME, Bean BP, Eggan K, Woolf CJ. Intrinsic membrane hyperexcitability of amyotrophic lateral sclerosis patient-derived motor neurons. Cell Rep. 2014;7:1–11. doi: 10.1016/j.celrep.2014.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Di Lullo E, Kriegstein AR. The use of brain organoids to investigate neural development and disease. Nat Rev Neurosci. 2017;18:573–584. doi: 10.1038/nrn.2017.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Drost J, Clevers H. Organoids in cancer research. Nat Rev Cancer. 2018;18:407–418. doi: 10.1038/s41568-018-0007-6. [DOI] [PubMed] [Google Scholar]
- 101.Tuveson D, Clevers H. Cancer modeling meets human organoid technology. Science. 2019;364:952–955. doi: 10.1126/science.aaw6985. [DOI] [PubMed] [Google Scholar]
- 102.Xu Q, Junttila S, Scherer A, Giri KR, Kivelä O, Skovorodkin I, Röning J, Quaggin SE, Marti HP, Shan J, Samoylenko A, Vainio SJ. Renal carcinoma/kidney progenitor cell chimera organoid as a novel tumorigenesis gene discovery model. Dis Model Mech. 2017;10:1503–1515. doi: 10.1242/dmm.028332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.da Silva B, Mathew RK, Polson ES, Williams J, Wurdak H. Spontaneous glioblastoma spheroid infiltration of earlystage cerebral organoids models brain tumor invasion. SLAS Discov. 2018;23:862–868. doi: 10.1177/2472555218764623. [DOI] [PubMed] [Google Scholar]
- 104.Ganesh K, Wu C, O’Rourke KP, Szeglin BC, Zheng Y, Sauvé CG, Adileh M, Wasserman I, Marco MR, Kim AS, Shady M, Sanchez-Vega F, Karthaus WR, Won HH, Choi SH, Pelossof R, Barlas A, Ntiamoah P, Pappou E, Elghouayel A, Strong JS, Chen CT, Harris JW, Weiser MR, Nash GM, Guillem JG, Wei IH, Kolesnick RN, Veeraraghavan H, Ortiz EJ, et al. A rectal cancer organoid platform to study individual responses to chemoradiation. Nat Med. 2019;25:1607–1614. doi: 10.1038/s41591-019-0584-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yan HHN, Siu HC, Law S, Ho SL, Yue SSK, Tsui WY, Chan D, Chan AS, Ma S, Lam KO, Bartfeld S, Man AHY, Lee BCH, Chan ASY, Wong JWH, Cheng PSW, Chan AKW, Zhang J, Shi J, Fan X, Kwong DLW, Mak TW, Yuen ST, Clevers H, Leung SY. A comprehensive human gastric cancer organoid biobank captures tumor subtype heterogeneity and enables therapeutic screening. Cell Stem Cell. 2018;23:882–897.e11. doi: 10.1016/j.stem.2018.09.016. [DOI] [PubMed] [Google Scholar]
- 106.van de Wetering M, Francies HE, Francis JM, Bounova G, Iorio F, Pronk A, van Houdt W, van Gorp J, Taylor-Weiner A, Kester L, McLaren-Douglas A, Blokker J, Jaksani S, Bartfeld S, Volckman R, van Sluis P, Li VS, Seepo S, Sekhar Pedamallu C, Cibulskis K, Carter SL, McKenna A, Lawrence MS, Lichtenstein L, Stewart C, Koster J, Versteeg R, van Oudenaarden A, Saez-Rodriguez J, Vries RG, et al. Prospective derivation of a living organoid biobank of colorectal cancer patients. Cell. 2015;161:933–945. doi: 10.1016/j.cell.2015.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Heo I, Dutta D, Schaefer DA, Iakobachvili N, Artegiani B, Sachs N, Boonekamp KE, Bowden G, Hendrickx APA, Willems RJL, Peters PJ, Riggs MW, O’Connor R, Clevers H. Modelling Cryptosporidium infection in human small intestinal and lung organoids. Nat Microbiol. 2018;3:814–823. doi: 10.1038/s41564-018-0177-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Duque-Correa MA, Maizels RM, Grencis RK, Berriman M. Organoids-new models for host-helminth interactions. Trends Parasitol. 2020;36:170–181. doi: 10.1016/j.pt.2019.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Qian X, Nguyen HN, Song MM, Hadiono C, Ogden SC, Hammack C, Yao B, Hamersky GR, Jacob F, Zhong C, Yoon KJ, Jeang W, Lin L, Li Y, Thakor J, Berg DA, Zhang C, Kang E, Chickering M, Nauen D, Ho CY, Wen Z, Christian KM, Shi PY, Maher BJ, Wu H, Jin P, Tang H, Song H, Ming GL. Brain-region-specific organoids using mini-bioreactors for modeling ZIKV exposure. Cell. 2016;165:1238–1254. doi: 10.1016/j.cell.2016.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Porotto M, Ferren M, Chen YW, Siu Y, Makhsous N, Rima B, Briese T, Greninger AL, Snoeck HW, Moscona A. Authentic modeling of human respiratory virus infection in human pluripotent stem cell-derived lung organoids. mBio. 2019;10:e00723–e819. doi: 10.1128/mBio.00723-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bartfeld S. Modeling infectious diseases and host-microbe interactions in gastrointestinal organoids. Dev Biol. 2016;420:262–270. doi: 10.1016/j.ydbio.2016.09.014. [DOI] [PubMed] [Google Scholar]
- 112.Dutta D, Clevers H. Organoid culture systems to study host-pathogen interactions. Curr Opin Immunol. 2017;48:15–22. doi: 10.1016/j.coi.2017.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Garcez PP, Loiola EC, Madeiro da Costa R, Higa LM, Trindade P, Delvecchio R, Nascimento JM, Brindeiro R, Tanuri A, Rehen SK. Zika virus impairs growth in human neurospheres and brain organoids. Science. 2016;352:816–818. doi: 10.1126/science.aaf6116. [DOI] [PubMed] [Google Scholar]
- 114.Dang J, Tiwari SK, Lichinchi G, Qin Y, Patil VS, Eroshkin AM, Rana TM. Zika virus depletes neural progenitors in human cerebral organoids through activation of the innate immune receptor TLR3. Cell Stem Cell. 2016;19:258–265. doi: 10.1016/j.stem.2016.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lamers MM, Beumer J, van der Vaart J, Knoops K, Puschhof J, Breugem TI, Ravelli RBG, Paul van Schayck J, Mykytyn AZ, Duimel HQ, van Donselaar E, Riesebosch S, Kuijpers HJH, Schipper D, van de Wetering WJ, de Graaf M, Koopmans M, Cuppen E, Peters PJ, Haagmans BL, Clevers H. SARS-CoV-2 productively infects human gut enterocytes. Science. 2020;369:50–54. doi: 10.1126/science.abc1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Han Y, Yang L, Duan X, Duan F, Nilsson-Payant BE, Yaron TM, Wang P, Tang X, Zhang T, Zhao Z, Bram Y, Redmond D, Houghton S, Nguyen D, Xu D, Wang X, Uhl S, Huang Y, Johnson JL, Xiang J, Wang H, Pan FC, Cantley LC, tenOever BR, Ho DD, Evans T, Schwartz RE, Chen HJ, Chen S. Identification of candidate COVID-19 therapeutics using hPSC-derived lung organoids. BioRxiv. 2020 doi: 10.1101/2020.05.05.079095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Dickson I. Organoids demonstrate gut infection by SARS-CoV-2. Nat Rev Gastroenterol Hepatol. 2020;17:383. doi: 10.1038/s41575-020-0317-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Zhou J, Li C, Liu X, Chiu MC, Zhao X, Wang D, Wei Y, Lee A, Zhang AJ, Chu H, Cai JP, Yip CC, Chan IH, Wong KK, Tsang OT, Chan KH, Chan JF, To KK, Chen H, Yuen KY. Infection of bat and human intestinal organoids by SARS-CoV-2. Nat Med. 2020;26:1077–1083. doi: 10.1038/s41591-020-0912-6. [DOI] [PubMed] [Google Scholar]