Abstract
To assess non-compliance and potential changes in seasonal flu vaccination coverage before and during the Covid-19 pandemic in patients with autoimmune rheumatic diseases (ARDs). Consecutive patients with ARDs followed-up in 2 tertiary hospitals were telephone-interviewed (December 12–30, 2020) regarding seasonal flu vaccination during the 2019/20 and 2020/21 time periods. Self-reported disease flares that occurred after flu vaccination, as well as reasons for non-vaccination were recorded. One thousand fifteen patients were included. The rate of flu vaccination increased from 76% before to 83% during the COVID-19 pandemic (p = 0.0001). The rate of self-reported disease flares was < 1% among vaccinated patients. Reasons for not vaccination in both periods, respectively, included: ‘was not recommended by their rheumatologists’ (35.0vs.12.2%, p < 0.0001), ‘did not feel that they would have any benefit’ (36.9 vs. 32.6%), felt unsafe to do so (27.5 vs. 30.2%), or other reasons (18.9 vs. 23.8%). By multivariate analysis, age [OR = 1.03 (95% CI 1.02–1.04)] vs. [1.04 (95% CI 1.02–1.05)] and treatment with biologics [OR = 1.66 (95% CI 1.22–2.24) vs. [1.68 (95% CI 1.19–2.38)] were independent factors associated with vaccination in both periods. These findings, although are temporally encouraging, emphasize the need for continuous campaigns aiming at increasing patients’ and physicians’ awareness about the benefits of vaccination.
Keywords: Vaccination, Influenza, Autoimmune rheumatic diseases, Covid-19
Introduction
The higher risk for infections in patients with autoimmune rheumatic diseases (ARDs) is well established [1, 2]. In this context, vaccinations are of paramount importance in this population. As outlined in EULAR recommendations, flu vaccination should be strongly considered for the majority of patients with ARDs [3] since it has been shown that is associated with reduced mortality, hospitalizations risk and influenza-related complications [3, 4].
Vaccination rates in ARD patients vary and few studies have assessed the factors that are associated with non-compliance. Covid-19 pandemic, added another factor of complexity as it has generated some degree of uncertainty in these patients [5]. Covid-19 virus entered our lives, suddenly, in December 2019, when a cluster of patients with lower respiratory tract infection was described in the province of Wuhan, in China [6]. Covid-19 is the seventh member of the corona-viruses that can infect humans [6] and its name is derived from the spikes that are present on its surface (Fig. 1). Although its origin is not clear, a close homology to two bat-derived coronaviruses has been identified [7, 8]. Clinically, is mainly expressed with fever, headache, anosmia, fatigue and cough and not infrequently, leads to admission in the intensive care unit [9–12].
Fig. 1.
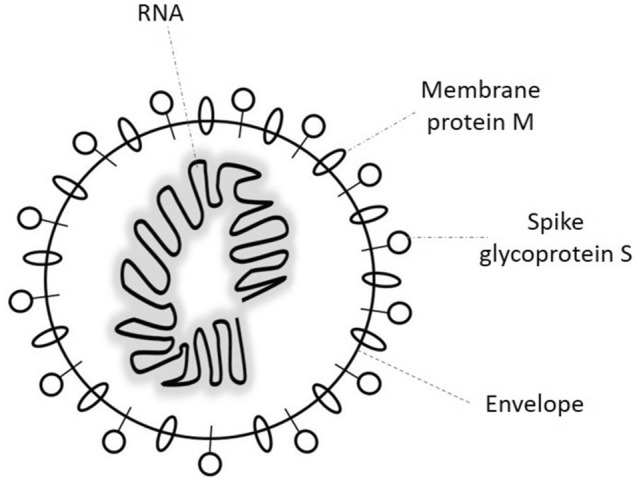
Schematic depiction of the novel coronavirus
Aim of our study was to assess potential changes in influenza vaccination during the Covid-19 pandemic among ARD patients and investigate the factors associated with non-compliance.
Patients and methods
In our cross-sectional, observational study, patients with ARDs who had been examined at least once during the last year in the outpatient rheumatology clinics of two tertiary hospitals were telephone-interviewed from 12/12/2020 to 30/12/2020.
Patients were consecutively enrolled, following an alphabetical order of their surname in our files. Patients with a diagnosis of osteoarthritis, crystal arthropathies and metabolic bone diseases were excluded. The following parameters were recorded: age, sex, level of education (1st level: elementary school, 2nd level: high school, 3rd level: college/university), employment status, smoking status, follow-up time (from disease diagnosis to enrollment in the study) and type of ARD (inflammatory arthritides: rheumatoid arthritis, spondyloarthropathies; connective tissue diseases: systemic lupus erythematosus, systemic sclerosis, dermatomyositis, Sjogren’s syndrome, anti-phospholipid syndrome, myositis; autoinflammatory diseases: adult-onset Still’s disease, familial mediterannean fever; vasculitides: ANCA-associated vasculitis, Behcet’s disease, giant cell arteritis), current treatment for ARDs (glucocorticoids, non-biologic immunosuppressives, targeted synthetic agents and biologics) and the presence of certain co-morbidities (hypertension, coronary heart disease, diabetes mellitus, chronic kidney disease, chronic obstructive pulmonary disease [COPD], history of malignancies and/or chemotherapy during the last 6 months).
A specific questionnaire, constructed by the investigators of this study specifically for this purpose, was used and included the following: Firstly, patients were asked if they had the inflenza vaccine in the periods 2019/20 and 2020/21 and if so, whether they had a disease flare that could be linked to vaccination. If they haven’t been vaccinated, they were asked why that occured; the following options were given: (a) believe that flu-vaccination is not helpful, (b) do not feel safe to have the vaccination, (c) was not suggested by their doctor (d) was not their priority, due to the covid pandemic (for 2020/21), (e) other reasons (including forgot to take the vaccine, previously allergic on vaccination etc.).
Comparisons were made between patients who were vaccinated and those who did not, in the two different time periods (2019/20 and 2020/21). Also, patients who did not take the vaccine in 2019/20, but decided to get vaccinated in 2020/21, were compared with those who did not change their vaccination behaviour.
The current study was conducted according to the Declaration of Helsinki and was approved by the Scientific Council of the hospital (No: 2020/14/4).
Statistics
Fisher’s exact and Mann–Whitney tests were used for categorical and continuous characteristics, respectively. Normality of data distribution was evaluated with Kolmogorov–Smirnov test. For parameters not normally distributed, results were expressed as median (range). Logistic regression analysis were performed using “vaccinated in the period 2019/20”, “vaccinated in the period 2020/21”, “vaccinated in both periods” as dependent variables, in three different models. Age, sex and parameters that demonstrated statistical significance in the univariate analyses served as independent variables. Statistical package SPSS 21.0 was used.
Results
Patient characteristics
In total, 1046 patients were called. From those, 1015 (97%) patients responded. They were 75% females, with a median (range) age of 58 (18–82) years and a mean disease duration of 7 (0.5–50) years (Table 1). The majority had inflammatory arthritides (59.6%) or connective tissue diseases (29.9%). Half of them were current or previous smokers. Their treatments and comorbidities are also shown in Table 1.
Table 1.
Patient characteristics
| Patient characteristics | |
|---|---|
| N | 1015 |
| Age (years), median (range) | 58 (18–82) |
| Females, n (%) | 758 (74.7%) |
| Disease duration, years, median (range) | 7 (0.5–50) |
|
Type of ARD, n (%) Inflammatory arthritis Connective tissue diseases Auto-inflammatory diseases Primary systemic vasculitides |
605 (59.6%) 304 (29.9%) 20 (2.0%) 86 (8.5%) |
|
Educational status, n (%) 1st level 2nd level 3rdlevel |
210 (20.7%) 444 (43.7%) 361 (35.6%) |
|
Employment status, n (%) Unemployed Employed Retired |
176 (17.4%) 468 (46.1%) 371 (36.5%) |
|
Smoking, n (%) Never Previous Current |
499 (49.2%) 268 (26.4%) 248 (24.4%) |
| Therapy | |
| Glucocorticoids, n (%) | 371 (36.6%) |
| Non-biologics, n (%) | 667 (65.7%) |
| Biologics, n (%) | 575 (56.7%) |
| Co-morbidities | |
| Hypertension, n (%) | 358 (35.3%) |
| Coronary artery disease | 64 (6.3%) |
| Heart failure, n (%) | 18 (1.8%) |
| Diabetes mellitus, n (%) | 99 (9.7%) |
| Chronic Kidney Disease, n (%) | 67 (6.6%) |
| Chronic Obstructive Pulmonary Disease, n (%) | 44 (4.3%) |
| Neoplasia history, n (%) | 74 (7.3%) |
| Chemotherapy, n (%) | 4 (0.4%) |
n number, SD standard deviation
Vaccination rates, reported disease flares and reasons for non-vaccination
In the 2019–20 period, 76.0% (771/1015) of ARD patients were vaccinated against the flu while the respective figure climbed to 83.1% (843/1015) during the COVID-19 pandemic period (2020/21, p = 0.0001). The respective rates of self-reported disease flares after vaccination were < 1% (2019/20: 0.3%, 2/771, 2020/21: 0.7%, 6/843).
The main reasons for non-vaccination in these 2 time periods were the belief that this would not be helpful (2019–20:36.9%, 2020–21:32.6%, p = 0.41), the fear of side effects (2019/20:27.5%, 2020/21:30.2%, p = 0.58), the absence of a recommendation from the treating physician (2019/20:35%, 2020/21:12%, p = 0.0001) and other reasons including forgetfulness about the vaccination (2019/20:18.9%, 2020/21:23.8%, p = 0.22).
Comparison of patients’ characteristics between those who did and those who did not vaccinate
During the two consecutive time periods (2019/20 and 2020/21), older patients, those on biologics and those with certain comorbidities such as hypertension and diabetes mellitus were most likely to get vaccinated (Table 2). Similarly, comparing patients who were vaccinated in both time periods (2019/2021) (n = 774) with those who were never vaccinated (n = 145), it was recorded that the former were older, more commonly on biologics or had comorbidities like hypertension, diabetes and COPD (Table 3).
Table 2.
Comparison of patients’ characteristics between those who were vaccinated and those who did not, during the 2 vaccination periods (2019–20 and 2020–21)
| Vaccination period 2019–20 | Vaccination period 2020–21 | |||||
|---|---|---|---|---|---|---|
| Yes (n = 771) | No (n = 244) | p | Yes (n = 843) | No (n = 172) | p | |
| Age (years), median (range) | 60 (18–82) | 50 (19–80) | 0.0001 | 59 (18–82) | 48 (21–80) | 0.0001 |
| Female gender, n (%) | 571 (74.1) | 187 (87.4) | 0.448 | 629 | 129 | 1.000 |
| Disease duration (years), median (range) | 7 (0.5–50) | 6 (0.5–48) | 0.02 | 7 (0.5–50) | 7 (0.5–48) | 0.686 |
|
Type of ARD Inflammatory arthritis Connective tissue diseases Auto-inflammatory diseases Vasculitis |
465 225 16 65 |
140 79 4 21 |
0.781 |
510 242 16 75 |
95 62 4 11 |
0.219 |
| Higher Educational status, n (%) | 253 (32.8) | 108 (44.3) | 0.001 | 292 (34.6) | 69 (40.1) | 0.190 |
| Unemployed, n (%) | 131 (17.0) | 45 (18.4) | 0.628 | 147 (17.4) | 29 (16.9) | 0.912 |
| Current smokers, n (%) | 186 (24.1) | 62 (25.4) | 0.670 | 205 (24.3) | 43 (25.0) | 0.846 |
| Therapy | ||||||
| Glucocorticoids, n (%) | 287 (37.2) | 84 (34.4) | 0.127 | 317 (37.6) | 52 (30.2) | 0.018 |
| Non-biologics, n (%) | 514 (66.7) | 153 (62.7) | 0.426 | 553 (65.6) | 110 (64.0) | 0.736 |
| Biologics, n (%) | 450 (58.4) | 115 (47.1) | 0.003 | 486 (57.7) | 79 (45.9) | 0.009 |
| Co-morbidities | ||||||
| Hypertension, n (%) | 305 (39.6) | 53 (21.7) | 0.0001 | 318 (37.7) | 40 (23.2) | 0.0001 |
| Coronary artery disease, n (%) | 55 (7.1) | 9 (3.7) | 0.068 | 57 (6.8) | 7 (4.1) | 0.229 |
| Heart failure, n (%) | 15 (1.9) | 3 (1.2) | 0.586 | 15 (1.8) | 3 (1.7) | 1.000 |
| Diabetes mellitus, n (%) | 85 (11.0) | 14 (5.7) | 0.013 | 91 (10.8) | 8 (4.7) | 0.011 |
| Chronic Kidney Disease, n (%) | 58 (7.5) | 9 (3.7) | 0.038 | 60 (7.1) | 7 (4.1) | 0.177 |
| Chronic Obstructive Pulmonary Disease, n (%) | 40 (5.2) | 4 (1.6) | 0.018 | 41 (4.9) | 3 (1.7) | 0.097 |
| Neoplasia history, n (%) | 59 (7.7) | 15 (6.1) | 0.482 | 60 (7.1) | 14 (8.1) | 0.630 |
| Chemotherapy, n (%) | 4 (0.5) | 0 (0.0) | 0.578 | 3 (0.4) | 1 (0.6) | 0.525 |
Significant values (p < 0.05) are marked with bold.
n number, SD standard deviation
Table 3.
Comparison of patients who were never vaccinated vs. those who vaccinated at both time periods
| Never vaccinated (n = 145) | Vaccinated at both time periods (n = 774) | p | |
|---|---|---|---|
| Age (years), median (range) | 49 (21–80) | 60 (18–82) | 0.0001 |
| Female gender, n (%) | 109 (75.2%) | 551 (71.1%) | 0.836 |
| Disease duration(years), median (range) | 7 (0.5–48) | 7 (0.5–50) | 0.516 |
|
Type of ARD Inflammatory arthritis Connective tissue diseases Auto-inflammatory diseases Vasculitis |
81 53 3 8 |
451 216 15 62 |
0.267 |
| Higher Educational status, n (%) | 57 (39.3%) | 240 (31.0%) | 0.103 |
| Unemployed, n (%) | 25 (17.2%) | 127 (16.4%) | 1.000 |
| Current smokers, n (%) | 46 (31.7%) | 185 (23.9%) | 0.09 |
| Therapy | |||
| Glucocorticoids, n (%) | 44 (30.3%) | 278 (35.6%) | 0.110 |
| Non-biologics, n (%) | 94 (64.8%) | 496 (64.1%) | 0.701 |
| Biologics, n (%) | 64 (44.1%) | 440 (56.9%) | 0.001 |
| Co-morbidities | |||
| Hypertension, n (%) | 35 (24.1%) | 335 (38.8%) | 0.0001 |
| Coronary artery disease, n (%) | 6 (4.1%) | 54 (7.0%) | 0.207 |
| Heart failure, n (%) | 3 (2.1%) | 15 (1.9%) | 1.000 |
| Diabetes mellitus, n (%) | 7 (4.8%) | 84 (10.9%) | 0.016 |
| Chronic Kidney Disease, n (%) | 7 (4.8%) | 58 (7.5%) | 0.294 |
| Chronic Obstructive Pulmonary Disease, n (%) | 2 (1.4%) | 39 (5.0%) | 0.05 |
| Neoplasia history, n (%) | 12 (8.3%) | 57 (7.4%) | 0.737 |
| Chemotherapy, n (%) | 0 (0%) | 3 (0.3%) | 1.000 |
Significant values (p < 0.05) are marked with bold
By multivariate analysis, it was found that vaccination was associated for both periods, assessed individually or combined, with age [2019/20: OR = 1.03 (95% CI 1.02–1.04), 2020/21: OR = 1.04 (95% CI 1.02–1.05), 2019/21: OR = 1.04 (1.02–1.05)] and treatment with biologics [2019–20: OR = 1.66 (95% CI 1.22–2.24), 2020/21: OR = 1.68. (95% CI 1.19–2.38), 2019/21: OR = 1.90 (1.30–2.77)].
Change in vaccination behaviour
Twenty-seven (2.7%) patients had the vaccine in 2019/20 but not during the COVID-19 period (2020/21). Only 7.4% did that because they thought that flu-vaccine was not their priority due to the COVID-19 pandemic. The most common reason was they forgot/had other reasons (63.0%) while the rest did not do it for safety concerns (18.5%), did not think that flu-vaccine was helpful (7.4%) and not recommended by their rheumatologist (3.7%).
On the other hand, 99 patients (9.8%) had their vaccine during the COVID-19 period but not in the previous year. These newly vaccinated patients compared to the patients that they did not change their vaccination behaviour (n = 889), were younger, had a shorter disease duration, were more frequently of higher education level and had less commonly hypertension (Table 4).
Table 4.
Comparison of patients who were newly vaccinated vs. those who did not change their vaccination behavior
| Newly vaccinated patients (in 2020–21 but not in 2019–20 period) | |||
|---|---|---|---|
| Yes (n = 99) | No (n = 889) | p | |
| Age (years), median (range) | 52 (19–80) | 58 (18–82) | 0.0001 |
| Female gender, n (%) | 78 (78.8%) | 660 (74.2%) | 0.394 |
| Disease duration(years), median (range) | 4 (0.5–40) | 7 (0.5–50) | 0.007 |
|
Type of ARD Inflammatory arthritis Connective tissue diseases Auto-inflammatory diseases Vasculitis |
59 26 1 13 |
532 229 18 70 |
0.274 |
| Higher Educational status, n (%) | 51 (51.5%) | 297 (33.4%) | 0.001 |
| Unemployed, n (%) | 20 (20.2%) | 152 (17.1%) | 0.405 |
| Current smokers, n (%) | 25 (25.2%) | 231 (26.0%) | 1.000 |
| Therapy | |||
| Glucocorticoids, n (%) | 39 (39.4%) | 322 (36.3%) | 0.582 |
| Non-biologics, n (%) | 59 (59.6%) | 590 (66.3%) | 0.182 |
| Biologics, n (%) | 51 (51.5%) | 504 (56.7%) | 0.338 |
| Co-morbidities | |||
| Hypertension, n (%) | 18 (18.2%) | 335 (37.7%) | 0.0001 |
| Coronary artery disease, n (%) | 3 (3.1%) | 61 (6.7%) | 0.193 |
| Heart failure, n (%) | 0 (0%) | 18 (2%) | 0.244 |
| Diabetes mellitus, n (%) | 7 (7%) | 91 (10.2%) | 0.379 |
| Chronic Kidney Disease, n (%) | 2 (2%) | 65 (7.3%) | 0.06 |
| Chronic Obstructive Pulmonary Disease, n (%) | 2 (2%) | 42 (4.6%) | 0.305 |
| Neoplasia history, n (%) | 3 (3.1%) | 71 (7.8%) | 0.102 |
| Chemotherapy, n (%) | 0 (0%) | 3 (0.3%) | 1.000 |
Significant values (p < 0.05) are marked with bold
SD standard deviation
Discussion
Vaccination against flu is strongly recommended in patients with ARD [3]. The effect that COVID-19 could have had in flu-vaccination uptake has not been studied so far. This is the first study showing that in a real-world population with ARDs, coverage for flu vaccination has increased during the Covid-19 pandemic era. In fact, there was a statistically significant increase from 76 to 83.1%. In a recent survey of the Italian general population, the rate of those who were willing to get the flu vaccine the 2020/21 period was 44%, compared to 27% of individuals who had the vaccine in 2019/20 [13].
The uptake of influenza vaccination varies across different countries and time periods, reflecting diversities in the studies’ design, health-system and culture differences, as well as the increasing awareness about vaccinations [14–17]. The majority of the studies, pertain RA, in which vaccination rates ranges from 25 to 90% [18]. In a registry-based study with RA patients a few years ago in Greece showed that the coverage for influenza vaccine was only 54% [19]. Also, recent studies investigating the vaccination rate in patients with other non-rheumatic chronic disorders showed that 40–55% were vaccinated [20, 21]. It seems, therefore, that campaigns ran by rheumatology societies about vaccinations have a significant effect in the care of ARD patients over the last years.
In concert with other studies [14–16], we found that vaccination uptake was higher by patients who have other comorbidities and by older people. Reassuringly, we found that younger people changed their behaviour for flu vaccination during the last year.
In addition, we found that only a small percentage of the patients (0.26–0.7%) experienced a flare of their disease after vaccination. This is consistent with most studies which have shown that although transient autoantibody development can be observed, flu vaccination did not alter disease activity in ARD patients [3, 22–25].
Regarding the reasons for non-vaccination in our study, the fear of adverse effects and the notion that the flu vaccine is not helpful were equally important. Noteworthy, one third of the patients, before the Covid-19 pandemic, were not vaccinated because this was not suggested by their doctor. This, however, has dramatically changed the last year. Lack of awareness and fear for flu vaccinations have been identified by other studies, focused in inflammatory arthritis, as major causes of non-vaccination in similar percentages (i.e. 20–30%, each) [16, 26].
Our study has certain advantages and limitations. It is a large, real-world study covering the whole spectrum of ARDs in contrast to other studies [14, 16]. Having that in mind, the high percentage of females (75%) in our cohort can be explained. In fact, the majority of patients with inflammatory arthritis and connective tissue diseases in our cohort, suffered from rheumatoid arthritis and systemic lupus erythematosus or scleroderma, respectively. In these diseases, female population predominates. Second, it is not registry-based but data were obtained from telephone-interviews. Said that it should be stressed that our questionnaire, was not externally validated, but it was specifically designed for this purpose by the investigators of this study. We acknowledge that our patients were followed in tertiary academic rheumatology clinics and therefore their adherence to national and international guidelines (including those for vaccinations) might be higher compared to the rest of the patient population. Finally, data for 2019/20 were retrospectively collected while there was no physician documented diagnosis of a disease flare.
In conclusion, we show that the flu vaccination rate increased significantly during the COVID-19 pandemic in a large, real-life cohort of patients with ARDs. This could have been in part due to the higher recommendation rate by their caring rheumatologists. These findings, although are temporally encouraging, emphasize the need for continuous campaigns aiming at increasing patients’ and physicians’ awareness about the benefits of vaccination.
Authors' contributions
GEF: study design, data analysis and interpretation, drafting the manuscript. GG: study design, data analysis and interpretation, revising the manuscript. JM: data acquisition, revising the manuscript. AA: data acquisition, data analysis and interpretation, revising the manuscript. V-KB: data acquisition, data analysis and interpretation, revising the manuscript. GE: study design, data acquisition, data analysis and interpretation, drafting the manuscript. KF: data acquisition, data analysis and interpretation, revising the manuscript. AK: data acquisition, data analysis and interpretation, revising the manuscript. EK: data acquisition, data analysis and interpretation, revising the manuscript. SP: data acquisition, data analysis and interpretation, revising the manuscript. MP: data acquisition, data analysis and interpretation, revising the manuscript. KT: study design, data acquisition, data analysis and interpretation, revising the manuscript. MGT: study design, data acquisition, data analysis and interpretation, revising the manuscript. DP: study inception, study design, data acquisition, data analysis and interpretation, revising the manuscript. DV: study inception, study design, data acquisition, data analysis and interpretation, revising the manuscript. PPS: study inception, study design, data acquisition, data analysis and interpretation, revising the manuscript.
Funding
This study has not received any funding.
Data availability
All data are presented in the manuscript. Further details are available at reasonable request.
Declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This study was conducted according to the Declaration of Helsinki and was approved by the Scientific Council of the “Laiko” hospital (No: 2020/14/4).
Informed consent
All patients have provided informed consent to participate into the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
George E. Fragoulis, Email: geofragoul@yahoo.gr
Ioannis Grigoropoulos, Email: grigoropoulosioannis@gmail.com.
Evgenia Mavrea, Email: jenny.mavrea96@gmail.com.
Aikaterini Arida, Email: aridakater@yahoo.gr.
Vassiliki-Kalliopi Bournia, Email: lily_bournia@hotmail.com.
Gerasimos Evangelatos, Email: gerevag@gmail.com.
Kalliopi Fragiadaki, Email: po_fragiadaki@yahoo.gr.
Anastasios Karamanakos, Email: tkar_84@hotamail.com.
Evrydiki Kravvariti, Email: euridicek@gmail.com.
Stylianos Panopoulos, Email: sty.panopoulos@gmail.com.
Maria Pappa, Email: mariak.pappa@yahoo.com.
Konstantinos Thomas, Email: costas_thomas@yahoo.com.
Maria G. Tektonidou, Email: mtektonidou@gmail.com
Dimitrios Paraskevis, Email: dparask@med.uoa.gr.
Dimitrios Vassilopoulos, Email: dvassilop@med.uoa.gr.
Petros P. Sfikakis, Email: psfikakis@med.uoa.g
References
- 1.Thomas K, Vassilopoulos D. Immunization in patients with inflammatory rheumatic diseases. Best Pract Res Clin Rheumatol. 2016;30:946–963. doi: 10.1016/j.berh.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 2.Fragoulis GE, Sipsas NV. When rheumatology and infectious disease come together. Ther Adv Musculoskelet Dis. 2019 doi: 10.1177/1759720X19868901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Furer V, Rondaan C, Heijstek MW, Agmon-Levin N, van Assen S, Bijl M, Breedveld FC, D'Amelio R, Dougados M, Kapetanovic MC, van Laar JM, de Thurah A, Landewe RB, Molto A, Muller-Ladner U, Schreiber K, Smolar L, Walker J, Warnatz K, Wulffraat NM, Elkayam O. 2019 update of EULAR recommendations for vaccination in adult patients with autoimmune inflammatory rheumatic diseases. Ann Rheum Dis. 2020;79:39–52. doi: 10.1136/annrheumdis-2019-215882. [DOI] [PubMed] [Google Scholar]
- 4.Nakafero G, Grainge MJ, Myles PR, Mallen CD, Zhang W, Doherty M, Nguyen-Van-Tam JS, Abhishek A. Effectiveness of inactivated influenza vaccine in autoimmune rheumatic diseases treated with disease-modifying anti-rheumatic drugs. Rheumatology (Oxford) 2020;59:3666–3675. doi: 10.1093/rheumatology/keaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fragoulis GE, Evangelatos G, Arida A, Bournia VK, Fragiadaki K, Karamanakos A, Kravvariti E, Laskari K, Panopoulos S, Pappa M, Tektonidou MG, Sfikakis PP. Treatment adherence of patients with systemic rheumatic diseases in COVID-19 pandemic. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217935. [DOI] [PubMed] [Google Scholar]
- 6.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W, China Novel Coronavirus I. Research T A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, Chen J, Meng Y, Wang J, Lin Y, Yuan J, Xie Z, Ma J, Liu WJ, Wang D, Xu W, Holmes EC, Gao GF, Wu G, Chen W, Shi W, Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abate SM, Ahmed Ali S, Mantfardo B, Basu B. Rate of Intensive Care Unit admission and outcomes among patients with coronavirus: a systematic review and Meta-analysis. PLoS ONE. 2020;15:e0235653. doi: 10.1371/journal.pone.0235653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS, China Medical Treatment Expert Group for C Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lechien JR, Chiesa-Estomba CM, Place S, Van Laethem Y, Cabaraux P, Mat Q, Huet K, Plzak J, Horoi M, Hans S, Rosaria Barillari M, Cammaroto G, Fakhry N, Martiny D, Ayad T, Jouffe L, Hopkins C, Saussez S, YO-IFOS C-TFo, Clinical and epidemiological characteristics of 1420 European patients with mild-to-moderate coronavirus disease 2019. J Intern Med. 2020;288:335–344. doi: 10.1111/joim.13089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Popov GT, Baymakova M, Vaseva V, Kundurzhiev T, Mutafchiyski V. Clinical Characteristics of Hospitalized Patients with COVID-19 in Sofia, Bulgaria. Vector Borne Zoonotic Dis. 2020;20:910–915. doi: 10.1089/vbz.2020.2679. [DOI] [PubMed] [Google Scholar]
- 13.Domnich A, Cambiaggi M, Vasco A, Maraniello L, Ansaldi F, Baldo V, Bonanni P, Calabro GE, Costantino C, de Waure C, Gabutti G, Restivo V, Rizzo C, Vitale F, Grassi R. Attitudes and Beliefs on Influenza Vaccination during the COVID-19 Pandemic: Results from a Representative Italian Survey. Vaccines (Basel) 2020 doi: 10.3390/vaccines8040711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Costello R, Winthrop KL, Pye SR, Brown B, Dixon WG. Influenza and pneumococcal vaccination uptake in patients with rheumatoid arthritis treated with immunosuppressive therapy in the UK: a retrospective cohort study using data from the clinical practice research datalink. PLoS ONE. 2016;11:e0153848. doi: 10.1371/journal.pone.0153848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nakafero G, Grainge MJ, Myles PR, Mallen CD, Zhang W, Doherty M, Nguyen-Van-Tam JS, Abhishek A. Predictors and temporal trend of flu vaccination in auto-immune rheumatic diseases in the UK: a nationwide prospective cohort study. Rheumatology (Oxford) 2018;57:1726–1734. doi: 10.1093/rheumatology/key156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nguyen M, Lindegaard H, Hendricks O, Friis-Moller N. Factors associated with influenza and pneumococcal vaccine uptake among rheumatoid arthritis patients in Denmark invited to participate in a pneumococcal vaccine trial (Immunovax_RA) Scand J Rheumatol. 2017;46:446–453. doi: 10.1080/03009742.2016.1242774. [DOI] [PubMed] [Google Scholar]
- 17.Papadopoulou D, Trontzas P. A survey to evaluate the implementation of vaccine recommendations among rheumatologists practicing in Greece. Mediterr J Rheumatol. 2017;28:41–47. doi: 10.31138/mjr.28.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gosselin Boucher V, Colmegna I, Gemme C, Labbe S, Pelaez S, Lavoie KL. Interventions to improve vaccine acceptance among rheumatoid arthritis patients: a systematic review. Clin Rheumatol. 2019;38:1537–1544. doi: 10.1007/s10067-019-04430-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomas K, Lazarini A, Kaltsonoudis E, Drosos A, Repa A, Sidiropoulos P, Fragkiadaki K, Tektonidou M, Sfikakis P, Tsatsani P, Gazi S, Katsimbri P, Boumpas D, Argyriou E, Boki K, Evangelatos G, Iliopoulos A, Karagianni K, Sakkas L, Melissaropoulos K, Georgiou P, Grika E, Vlachoyiannopoulos P, Dimitroulas T, Garyfallos A, Georganas C, Vounotrypidis P, Ntelis K, Areti M, Kitas GD, Vassilopoulos D. AB1201 increasing rates of influenza vaccination coverage in rheumatoid arthritis patients: data from a multicenter, longitudinal cohort study of 1,406 patients. Ann Rheum Dis. 2020;79:1892–1892. doi: 10.1136/annrheumdis-2020-eular.4812. [DOI] [Google Scholar]
- 20.Papaioannou A, Konstantinidi AE, Primikiri E, Asimakopoulou F, Aravantinos D, Mavromichali Z. Influenza vaccination rate among high risk group patients in primary health care in Greece. Cent Eur J Public Health. 2020;28:297–301. doi: 10.21101/cejph.a5237. [DOI] [PubMed] [Google Scholar]
- 21.Machado A, Kislaya I, Santos AJ, Gaio V, Gil AP, Barreto M, Namorado S, Antunes L, Matias Dias C, Nunes B. Factors associated to repeated influenza vaccination in the Portuguese adults with chronic conditions. Vaccine. 2018;36:5265–5272. doi: 10.1016/j.vaccine.2018.07.041. [DOI] [PubMed] [Google Scholar]
- 22.Holvast A, Stegeman CA, Benne CA, Huckriede A, Wilschut JC, Palache AM, Kallenberg CG, Bijl M. Wegener's granulomatosis patients show an adequate antibody response to influenza vaccination. Ann Rheum Dis. 2009;68:873–878. doi: 10.1136/ard.2008.092924. [DOI] [PubMed] [Google Scholar]
- 23.Saad CG, Borba EF, Aikawa NE, Silva CA, Pereira RM, Calich AL, Moraes JC, Ribeiro AC, Viana VS, Pasoto SG, Carvalho JF, Franca IL, Guedes LK, Shinjo SK, Sampaio-Barros PD, Caleiro MT, Goncalves CR, Fuller R, Levy-Neto M, Timenetsky Mdo C, Precioso AR, Bonfa E. Immunogenicity and safety of the 2009 non-adjuvanted influenza A/H1N1 vaccine in a large cohort of autoimmune rheumatic diseases. Ann Rheum Dis. 2011;70:1068–1073. doi: 10.1136/ard.2011.150250. [DOI] [PubMed] [Google Scholar]
- 24.Setti M, Fenoglio D, Ansaldi F, Filaci G, Bacilieri S, Sticchi L, Ferrera A, Indiveri F, Ghio M. Flu vaccination with a virosomal vaccine does not affect clinical course and immunological parameters in scleroderma patients. Vaccine. 2009;27:3367–3372. doi: 10.1016/j.vaccine.2009.01.078. [DOI] [PubMed] [Google Scholar]
- 25.Perdan-Pirkmajer K, Thallinger GG, Snoj N, Cucnik S, Zigon P, Kveder T, Logar D, Praprotnik S, Tomsic M, Sodin-Semrl S, Ambrozic A. Autoimmune response following influenza vaccination in patients with autoimmune inflammatory rheumatic disease. Lupus. 2012;21:175–183. doi: 10.1177/0961203311429817. [DOI] [PubMed] [Google Scholar]
- 26.Murray K, Low C, O'Rourke A, Young F, Callanan I, Feeney E, Veale DJ. A quality improvement intervention failed to significantly increase pneumococcal and influenza vaccination rates in immunosuppressed inflammatory arthritis patients. Clin Rheumatol. 2020;39:747–754. doi: 10.1007/s10067-019-04841-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are presented in the manuscript. Further details are available at reasonable request.


