Summary
Pancreatic malignant exocrine tumors represent the most important cause of cancer-related death for pancreatic neoplasms. The most common tumor type in this category is represented by pancreatic ductal adenocarcinoma (PDAC), an ill defined, stroma-rich, scirrhous neoplasm with glandular differentiation. Here we present the relevant characteristics of the most important PDAC variants, namely adenosquamous carcinoma, colloid carcinoma, undifferentiated carcinoma, undifferentiated carcinoma with osteoclast-like giant cells, signet ring carcinoma, medullary carcinoma and hepatoid carcinoma. The other categories of malignant exocrine tumors, characterized by fleshy, stroma-poor, circumscribed neoplasms, include acinar cell carcinoma (pure and mixed), pancreatoblastoma, and solid pseudopapillary neoplasms. The most important macroscopic, histologic, immunohistochemical and molecular hallmarks of all these tumors, highlighting their key diagnostic/pathological features are presented. Lastly, standardized indications regarding gross sampling and how to compile a formal pathology report for pancreatic malignant exocrine tumors will be provided.
Key words: pancreatic cancer, pancreatic ductal adenocarcinoma, PDAC, acinar, solid pseudopapillary
Introduction
Malignant exocrine tumors of the pancreas represent the most common pancreatic tumors, with pancreatic ductal adenocarcinoma (PDAC) in first place for both incidence and mortality rate. Due to the important clinical implications that follow a diagnosis of malignant exocrine tumor of the pancreas, pathologists should be aware of the most important diagnostic features and hallmarks of this group of tumors.
In this review, we will present this topic starting from the sampling protocols of pancreatic resection specimens, and arriving to describe the most important clinical, macroscopic, histologic, immunohistochemical and molecular characteristics of PDAC, acinar cell carcinoma, pancreatoblastoma and solid pseudopapillary neoplasm.
The most important aim of this manuscript is providing to pathologists a serviceable and practical guideline for the correct approach to malignant exocrine tumors of the pancreas, which may be encountered during routine diagnostic activity. Finally, a schematic list of the most important points, which should be described in the final pathology report, is provided.
Gross sampling
The pancreatoduodenectomy specimen is one of the most challenging surgical samples for pathologists. It requires experience and knowledge of anatomical landmarks so that adequate information regarding resection margins, origin/size of tumor and number of lymph nodes is collected (at least 12 lymph nodes per specimen according to the recent 2017 UICC/AJCC staging handbook) 1.
In patients with resectable PDAC of the pancreatic head, a R0 resection (i.e.: tumor-free resection margins) is a very important prognostic factor 2-5. However, R1 resection rates vary greatly between surgical series and the prognostic differences between R0 and microscopic R1 of the pancreatic neck margin/radial margins have not been confirmed by all studies 2-5. The main reason for these differences is that for many years non-standardized sampling protocols with little attention to circumferential margin status have been performed. Along this line, sampling protocols for pancreatic specimens have been under scrutiny for some years as the importance of standardization in specimen handling and sample selection have come to light 6.
A representative image of gross sampling is provided in Figure 1.
Figure 1.
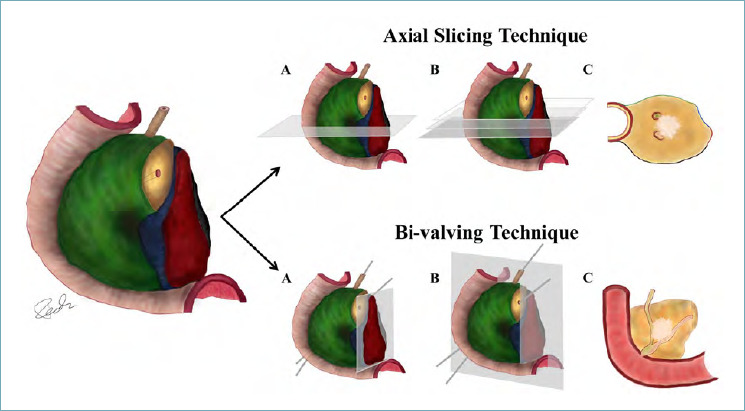
These images show the different sampling techniques for duodeno-pancreatic head resections. Margins are inked in different colors: green - anterior surface; blue - superior mesenteric vein groove; red - uncinate process/medial/retroperitoneal/superior mesenteric artery margin; black (minimum portion shown) - posterior surface. - Axial Slicing Technique (upper panel): (A) initially, a horizontal section perpendicular to the duodenum and passing through the ampulla is performed; (B) parallel sections are then obtained; (C) complete section of duodenum with pancreatic head, main pancreatic duct, bile duct and tumor (whitish area). The circumferential margins/surfaces are shown with respective colors. - Bi-valving Technique (lower panel): (A) the red uncinate process/medial/retroperitoneal/superior mesenteric artery margin is shaved and then bread-sliced and submitted entirely; (B) a horizontal section passing on a plane which passes through the probed bile duct and pancreatic duct is shown. Further sections can be parallel (or even perpendicular); (C) complete section of the bi-valved specimen showing the tumour (whitish area), which arises from the pancreas and invades the bile duct and the main pancreatic duct.
PANCREATODUODENECTOMY SPECIMEN HANDLING AND SAMPLING PROTOCOLS
Pancreatoduodenectomy specimens may vary with regards to which organs/parts of organs are present in the specimen such as: the distal portion of stomach in Whipple’s procedure (while pylorus preserving pancreatectomies will only have the duodenal bulb as the proximal margin), gall bladder and extrahepatic bile ducts, partial or complete venous resections (of the superior mesenteric vein or portal vein), which should be annotated by surgeons.
Once the specimen is received (ideally fresh specimens for better evaluation and biobanking), the stomach/duodenum/jejunum should be opened along the free margin, to aid adequate fixation. A standardized sampling protocol may also include circumferential margin multicolor inking, which has proven to be a potentially important step for resection margin/surface identification 7. In the last decade, two main standardized sampling protocols have been proposed, both with advantages and disadvantages with regards to surface/margin recognition, complexity of cut up, distinction between tumor origin (pancreatic origin versus ampullary versus distal cholangiocarcinoma or cystic tumors) and lymph node yield.
The protocol proposed by Verbeke, axially slices the specimen perpendicularly to the long axis of the duodenum at the ampulla 8. Further slicing is continued cranially and caudally, in parallel to the first slice, until thin complete sections of all the pancreatic head are obtained. The main advantages of this protocol are the optimal evaluation of the circumferential margins/surfaces and an acceptable lymph node yield 9.
The bi-valving protocol according to Adsay involves sectioning the specimen in two halves following the plane between probes inserted in the pancreatic duct and the common bile duct 10. This method of sampling is also known as bi-valving. Prior to further sectioning, the inked pancreatic retroperitoneal margin (or superior mesenteric vessel margin) is orange peeled and fully submitted for histology with a bread-slicing sampling. The bi-valved specimen is then further sectioned (either axially, multi-valved or bread loafed). Lymph node harvesting is performed by orange-peeling of the circumferential margins/surfaces and this correlates with a high lymph node yield. Further advantages of this technique are the optimal evaluation of primary site of tumor (pancreatic, ampullary or common bile duct) and the complete evaluation of the retroperitoneal margin.
The pancreatoduodenectomy specimen requires multiple samples, including a tumor-representative sampling, the relationship of tumor with adjacent structures (e.g. common bile duct), transection margins (pancreatic, common bile duct, gastric/duodenal) and, above all in cases of extensive tumor infiltration, the circumferential resection margin(s)/surfaces. Attention must be paid in the case of resection for precursors of pancreatic cancer (e.g.: intraductal papillary mucinous neoplasm), in which an infiltration may be very focal, thus an extensive sampling is required 11. Along this line, an extensive sampling is also of importance in the setting of post-neoadjuvant therapy, where a precise gross definition of tumor boundaries is not often recognizable 12.
Among various issues frequently encountered during routine sampling activity, the most frequent regard the potential misunderstanding about specific nomenclature of circumferential margins/surfaces. Indeed, the superior mesenteric vessel margin can be also named as uncinate margin; the posterior aspect of the head of the pancreas can be intended both as a margin, behind the pancreatic transection margin, and as a surface, towards the duodenum 13. Another possible issue includes the definition/concept of “positive” margin, since it can represent a direct invasion of neoplastic cells on the margin, but can be also defined as a distance < 1 mm between tumor cells and the margin 14.
DISTAL PANCREATECTOMY SPECIMEN HANDLING AND SAMPLING PROTOCOL
Distal pancreatectomy specimens do not present significant issues in orientation and landmark identification typical in pancreatic head specimens. Indeed, the spleen and the pancreatic transection margin permit left to right orientation, while the splenic artery and vein, which run along the posterior-superior groove of the pancreatic body and tail, permit cranial to caudal orientation. Inking with different colors is not mandatory, but can be useful for distinguishing anterior/posterior surfaces and the superior/inferior aspects. The specimen should be sliced in sections, parallel to the transection margin. This method permits the identification of the distance between the tumor and the transection margin, as well as aspects of adipose tissue infiltration and splenic vessels invasion. Lymph nodes can be retrieved from the peri-pancreatic soft tissue and from the splenic hilum; the most important site for lymph node sampling is along the course of splenic vessels.
SURGICAL RESECTIONS AFTER NEO-ADJUVANT THERAPY
Surgical resections after neoadjuvant therapy are becoming one of the most frequent scenario in pancreatic pathology, above all in specialized centers. These resections are often warp and diffusely whitish, with tumor area with blurred borders or even not visible. In such cases, an extensive sampling should be performed, and in cases of not identifiable tumor areas or of small tumor beds, they should be entirely included. Sometimes surgical resections include complex vessel resections (e.g.: celiac trunk, splenic-portal-mesenteric confluence), which should be correctly isolated during gross sampling and described in the final pathology report 15.
Pancreatic ductal adenocarcinoma
DEFINITION AND TERMINOLOGY
Pancreatic ductal adenocarcinoma (PDAC) is the most common type of pancreatic cancer 16. It is a malignant neoplasm composed of infiltrating glands that resembles pancreatic ducts. Synonyms include duct cell adenocarcinoma, infiltrating duct carcinoma or tubular adenocarcinoma 16.
CLINICAL AND GROSS FEATURES
About two-thirds of PDAC arise in the pancreatic head, with the rest affecting equally the body and/or the tail of the gland equally. Clinical features include back pain, dyspepsia, weight loss and new-onset diabetes; jaundice is a symptom typical of pancreatic head tumors. Rarely, acute pancreatitis and migratory thrombophlebitis may be seen in PDAC patients. Important risk factors for PDAC are tobacco smoking, obesity and alcohol consumption. The highest rates of PDAC incidence have been reported among black people in the USA. An increased risk for PDAC is also described for patients with chronic pancreatitis and diabetes mellitus, and for patients with a previously resected PDAC 16,17.
From a macroscopic point of view, PDAC are usually a firm and poorly defined whitish mass with irregular borders. Usually they infiltrate surrounding structures, including peri-pancreatic adipose tissue, the duodenal wall, the distal choledocus and the ampulla of Vater. Cancers < 2 cm are quite rare (about 10% of PDAC) 16,18. The most recent TNM staging system is mainly based on tumor size, with pT1 for tumors with a diameter ≤ 2 cm, pT2 for tumors ranging from 2,1 to 4 cm, pT3 for tumors > 4 cm, and pT4 for tumors involving celiac axis, superior mesenteric artery, and/or common hepatic artery, regardless of size 19.
PRECURSORS OF PANCREATIC DUCTAL ADENOCARCINOMA
Precursors of PDAC include: Pancreatic Intraepithelial Neoplasm (PanIN), Intraductal Papillary Mucinous Neoplasm (IPMN), Intraductal Oncocytic papillary Neoplasms (IOPN), Intraductal Tubulopapillary Neoplasm (ITPN), and Mucinous Cystic Neoplasm (MCN) 16,20-23. All these lesions can progress into the invasive counterpart, which is represented by PDAC. PanIN is a microscopic, non-infiltrative epithelial neoplasm confined to the pancreatic ducts; it can show a flat or a micropapillary epithelium 16,20. PanINs are classified with a two-tiered grading system: low grade and high grade dysplasia PanIN 15,24. Due to their microscopic nature, PanINs are asymptomatic. Notably, high-grade PanINs represent the main precurosor of PDAC 16,20. From the molecular point of view, KRAS mutations have been described as an early event in PanIN formation and PDAC carcinogenesis, as well as SMAD4 and TP53 mutations represent late events in this model (high-grade PanIN) 16,20-23.
IPMNs are intraductal neoplasms of the pancreas, with papillary mucinous epithelium. They are by definition > 5 mm and can involve Wirsung’s duct (main duct IPMN), branch ducts (branch duct IPMN) or both (mixed IPMN) 16,20-23. Main duct IPMN present a higher risk of malignant transformation and of metachronous recurrences compared to branch duct 25,26. Based on the type of epithelium, IPMNs can be subdivided into intestinal, gastric and pancreatic-biliary; notably, in the current WHO classification, IOPN are considered separately from the other IPMN subtypes 16,20. Similarly to PanIN, the dysplasia of IPMN is also classified as low- and high-grade. High-grade IPMN can progress to invasive PDAC, which can be indistinguishable from conventional PDAC, with the exception of colloid carcinoma, a distinct PDAC subtype producing abundant extracellular mucin, which originates from intestinal-type IPMN 26-28. From a genetic point of view, the most important alterations in IPMN include KRAS and GNAS mutations, and microsatellite instability, which is more common in the intestinal subtype 16,22,29.
IOPN is a grossly exophytic, intraductal neoplasm composed by oncocytic glandular epithelium, which is more frequent in females. The most important distinctive features are the almost exclusive presence of high grade dysplasia and the lack of the most frequent somatic mutations of IPMN 16.
Macroscopically, the lesions are characterized by large, solid or papillary mass, which lack mucin. Microscopically, the lesion is constituted by complex, arborizing papillae, lined by cuboidal cells with eosinophilic granular cytoplasm, filled with mitochondria, intracytoplasmic lumen and large nuclei. Almost all IOPNs show high grade dysplasia, whereas invasive carcinoma occurs in only 30% of cases. Immunohistochemically, IOPNs show MUC6 and MUC1 positivity, with focal positivity for MUC5AC, whereas immunostaining for MUC2 and CDX2 is restricted to sparse goblet cells. IOPNs lack the common somatic mutations of IPMN, like KRAS and GNAS, whereas they can show mutations in ERBB4 and the distinctive PRKACA/B gene fusions. The 5-year disease-specific survival approaches 100%.
ITPN are intraductal neoplasms of the pancreas, with a typical tubulopapillary appearance and usually with high-grade dysplasia 16. From the histologic point of view, ITPN form nodules of back-to-back tubular glands, with a large, cribriform architecture; an associated invasive carcinoma is found in up to 70% of cases 16. From a molecular point of view, ITPN are very peculiar, with no KRAS mutations; they show more frequently KMT2 and PIK3-pathway gene mutations (PI3KCA, PTEN), and a subset of ITPN harbor FGFR2 fusions 16,20-23.
MCNs are cyst-forming and mucin-producing epithelial neoplasm; they are associated with the presence of an ovarian-like sub-epithelial stroma 16,20-23. MCNs usually affect middle-aged women and arise in the body-tail region of the pancreas. They typically do not communicate with the Wirsung’s duct. Similarly to PanIN and IPMN, the dysplasia of MCN is also classified into low- and high-grade. From a molecular point of view, KRAS, TP53 and RNF43 mutations are the most common mutations in MCN 16,20.
Although there is no useful immunohistochemical panel for the diagnosis of PanIN and MCN, for IPMN and ITPN there are some mucin-based stains that can be of much help in supporting diagnosis and identifying the correct histologic subtype (Tab. I) 16,20.
Table I.
Immunohistochemical markers for IPMN/IOPN/ITPN classification.
| Type of lesion | Subtype | MUC1 | MUC2 | MUC5AC | MUC6 | CDX2 |
|---|---|---|---|---|---|---|
| IPMN | G | negative | negative | positive | negative | negative |
| PB | positive | negative | positive | positive | negative | |
| INT | negative | positive | positive | negative | positive | |
| IOPN | positive | negative | positive | positive | negative | |
| ITPN | positive | negative | negative | positive | negative |
Abbreviations: IPMN: intraductal papillary mucinous neoplasm; IOPN: intraductal oncocytic papillary neoplasm; ITPN: intraductal tubulo-papillary neoplasm; G: gastric; PB: pancreatic-biliary; INT: intestinal.
Note: if the positivity of a marker is very intense at the immunohistochemical level and very important for diagnostic purposes, it is indicated in bold.
One of the most difficult challenges in pancreatic pathology regards the identification of foci of micro-infiltration originating from precursor lesions. The hallmark of an invasive component is represented by the presence of desmoplastic stroma around invasive, atypical glands. Notably, an important diagnostic pitfall is represented by the differential diagnosis between mucin extravasation in the periphery of lesions vs. true stromal invasion. The assessment of eventual micro-invasive areas should be established by experienced pancreatic pathologists or at least discussed at a multi-headed microscope.
MICROSCOPIC DESCRIPTION WITH DIAGNOSTIC HALLMARKS
Most PDACs are composed of well to moderately differentiated duct-like and glandular structures, invading the pancreatic parenchyma 16. They are characterized by an irregular growth pattern, which is typically associated with a usually marked desmoplastic stromal reaction. Indeed, PDACs exhibit an abundant stroma and consequently can be considered as hypocellular tumors. A very important feature, which can be easily used to discriminate neoplastic/infiltrative glands vs. normal ducts is represented by the fact that neoplastic glands are very commonly ruptured with areas of epithelial denudation of the gland, while normal ducts show a continuous epithelial lining. Histologically, PDAC are graded into a 3-tiered system: well, moderate and poorly differentiated PDAC, based on combined assessment of the degree of glandular differentiation, mucin production, mitotic activity and nuclear features 16. Representative images of PDAC grading are provided in Figure 2, as well as a case of PDAC in the neoadjuvant setting, where no grading should be applied because it is unreliable due to iatrogenic modifications of tissues.
Figure 2.
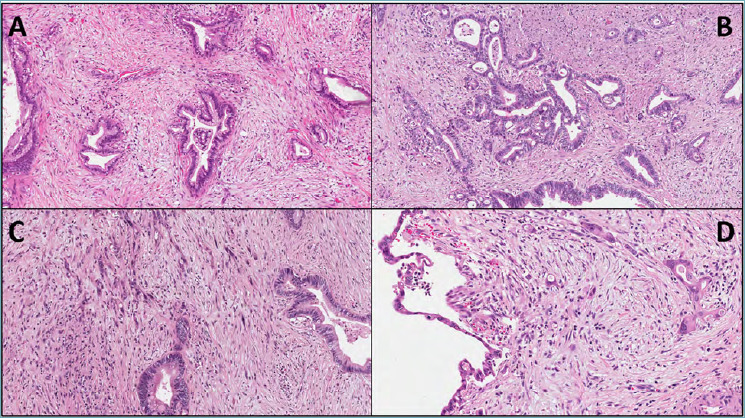
(A,B,C) Representative images of the grading system for pancreatic ductal adenocarcinoma: G1 (A, original magnification 20X), G2 (B, original magnification 20X) and G3 (C, original magnification 20X). D) In the setting of neo-adjuvant therapy, pancreatic ductal adenocarcinoma should not be graded, due to the unreliability of grading for the iatrogenic modifications of tissues, including therapy-induced cell atypia (original magnification 20X).
Well-differentiated PDACs are composed of haphazardly arranged invading and medium-size duct-like and glandular structures, with angular or irregular shapes 16,30. Neoplastic cells are generally columnar or cuboidal, forming a single cell layer with eosinophilic cytoplasm; the nuclei are round or oval and may be even four times larger than non-neoplastic nuclei 16,30. This comparison is often feasible since in many PDACs some normal ducts are trapped within the tumor mass. The nuclear membranes are well-delineated and the nucleoli, which generally are two or more, are often prominent; mitoses are not common. Lymphatic and blood vessel invasion/embolization, perineural infiltration as well as lymph node metastases represent very common findings 16,30. A peculiar morphological aspect of lymph node metastasis, which is the extra-nodal extension of neoplastic cells in the peripheral adipose tissue, has recently been associated with worse prognosis in many cancer types, including PDAC 31-33.
Moderately differentiated PDACs are similar to the well-differentiated counterpart: glandular and duct-like structures, as well as the cellular and nuclear size, however, have a greater variation. Usually, tumor glands are smaller and neoplastic cells are larger, with more mitotic figures; mucin production appears to be less evident compared to well-differentiated PDAC 16,30.
Poorly differentiated PDACs are composed of small glands with irregular shape and of individual atypical cells; from the architectural point of view, poorly differential PDAC are densely packed tumors, sometimes with an arrangement in solid sheets and nests 16,30. Neoplastic cells exhibit pronounced nuclear pleomorphism, scanty or no mucin production and high mitotic activity. Areas with neoplastic cells organized in small aggregates or infiltrating as single elements are common, and represent so-called PDAC tumor budding, strictly correlated with the activation of the process of epithelial-mesenchymal transition 34,35.
Some important morphologic features represent true diagnostic PDAC hallmarks. They include the irregular structural tumor pattern, the abundant desmoplastic stromal reaction and the presence of “ruptured” or “incomplete” glands 16,30. Furthermore, vascular and perineural invasions are both highly diagnostic of an infiltrating tumor. Another diagnostic PDAC hallmark is represented by neoplastic gland topographic location: indeed, the infiltrating malignant glands are often found in abnormal locations, such as immediately adjacent to muscular blood vessels 30,36. This criterion is helpful in the differential diagnosis with chronic pancreatitis and for supporting the diagnosis of PDAC in case of low-atypia (e.g.: in surgical specimens after neo-adjuvant therapies, where the degree of cellular atypia may be very mild) 16,30.
VARIANTS OF PANCREATIC DUCTAL ADENOCARCINOMA
The 2019 WHO classification distinguishes different PDAC variants, which are: adenosquamous carcinoma, colloid carcinoma, medullary carcinoma, poorly cohesive carcinoma/signet-ring cell carcinoma, hepatoid carcinoma, large cell rhabdoid carcinoma, undifferentiated carcinoma and undifferentiated carcinoma with osteoclast-like giant cells 16. Although some PDAC variants may show some peculiar macroscopic aspects, there are no definitive criteria to provide such a distinction by gross examination. At the same time, it has to be noted that colloid carcinoma is characterized by large pools of mucin, and undifferentiated carcinoma with osteoclast-like giant cells frequently shows foci of hemorrhage and/or necrosis. The other variants do not display peculiar gross aspects.
From a microscopic point of view, there are some specific features that characterize the different PDAC variants. Representative images of the most important variants are presented in Figure 3.
Figure 3.
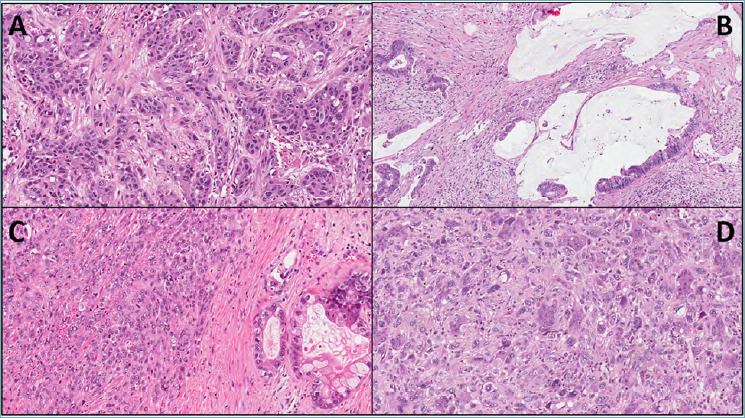
Representative images of the most relevant pancreatic ductal adenocarcinoma variants. (A) Adenosquamous carcinoma (original magnification 20X); (B) colloid carcinoma (original magnification 20X); (C) undifferentiated carcinoma (original magnification 20X); (D) undifferentiated carcinoma with osteoclast-like giant cells (original magnification 20X).
Adenosquamous carcinoma is composed of significant proportions with both ductal and squamous (at least 30%) differentiation 16,30. The squamous component can also be highlighted with immunohistochemistry for p63/p40 34. From a molecular point of view, this variant typically harbors KRAS, TP53 and UPF1 mutations 37,38. The prognosis is very poor 39.
Colloid carcinoma is characterized by the presence of large extracellular stromal mucin pools with suspended tumor cells composing at least 80% of tumor mass 16. This variant usually originates from intestinal-type IPMN 27,28. Immunohistochemical markers of colloid carcinoma reflect its intestinal profile, with positivity for MUC2, CK20 and CDX2 16. From a molecular point of view, colloid carcinoma are enriched of GNAS mutations (up to 60% of cases) and microsatellite instability 40,41. In pancreatic cancer, this alteration can be investigated with immunohistochemistry for the mismatch repair protein MLH1, PMS2, MSH2 and MSH6. In cases of doubtful results, MSI-based polymerase chain reaction or next generation sequencing should be performed 42.
Medullary carcinoma is a poorly differentiated carcinoma with limited gland formation, a pushing border, a syncytial growth and several tumor-infiltrating lymphocytes 41,43. This variant is usually associated with microsatellite instability, but a recent study highlighted that it can also arise in a hypermutated, non-microsatellite related genetic context, in association with POLE mutation 41-44.
Poorly cohesive/signet ring cell carcinoma is composed of at least 80% of individual poorly cohesive cells, often with intracellular mucin vacuoles peripherally displacing the nuclei 45.
Hepatoid carcinoma is an extremely rare neoplasm, defined as a carcinoma in which at least 50% of cells display histological and immunohistochemical evidence of hepatocellular differentiation 16,30. They are composed of large, polygonal cells resembling those of hepatocellular carcinoma. Alpha-fetoprotein, Hep-par1, CD10 and arginase are useful immunohistochemical markers to support such diagnosis, although the main diagnostic criterion remains morphology 16.
Rhabdoid carcinoma is a malignant neoplasm composed of large cells with rhabdoid features; it frequently harbors KRAS mutations/amplification, and in the case of KRAS wild-type, a typical SMARCB1 (INI1) immunohistochemical loss has been reported at the nuclear level 16,45.
Undifferentiated carcinoma is a malignant epithelial neoplasm in which the majority of tumor mass does not show any definitive direction of differentiation16. Different from conventional PDAC, undifferentiated carcinomas are hypercellular tumors. They can be stained with cytokeratin (CKAE1/3, CK8/18) and express an immunohistochemical profile associated with an activated epithelial-mesenchymal transition (expression of vimentin, Twist1 and Snai2, and E-Cadherin loss) 16,46,47.
The undifferentiated carcinoma with osteoclast-like giant cells variant (UCOGC) is composed by three cell types: spindle and/or pleomorphic cells, the real neoplastic cells, mononuclear histiocytes and osteoclast-like giant cells 16,46-48. Osteoclast-like giant cells can show over 20 nuclei each and do not have a malignant behavior. This variant shows a genetic profile very similar to conventional PDAC, and seems enriched in SERPINA3 mutations 49. Its unique immunologic microenvironment is dominated by the presence of tumor-stimulating histiocytes CD163-positive 50. In cases with the absence of an associated PDAC component, UCOGC prognosis may be very favorable with prolonged/long-term survivals 48-50.
IMMUNOHISTOCHEMISTRY AND MOLECULAR PATHOLOGY
An unequivocal immunohistochemical panel that can be used to discriminate PDAC from other extrapancreatic mucin-producing adenocarcinomas does not exist. However, some markers may be of help in supporting a PDAC diagnosis. First of all, PDACs express the same keratins as the normal pancreatic duct epithelium, such as keratins 7, 8, 18 and 19 16,30; indeed, the highest sensibility and specificity is reached by the 8-18 cocktail. Keratin 20, a typical intestinal-epithelial marker, is not expressed by PDAC cells, with the exception of infiltrating tumors arising from intestinal-type IPMN 51. Among mucins, PDAC cells are usually stained with IHC for MUC1, MUC4 and MUC5AC, but not MUC2, which has a staining pattern very similar to Keratin 20 52,53.
PDACs are usually negative for pancreatic exocrine enzymes such as trypsin, chymotrypsin and lipase, and for the acinar-related marker Bcl-10, as well as for neuroendocrine markers, including chromogranin A, synaptophysin, CD56 and CD200 16,30,49,54. Regarding “immune-molecular” staining, the DPC4 protein is lost in up to 55% of PDACs, and the p53 protein is expressed in most cases 16,30,49,55. These two IHC markers may be very useful for the differential diagnosis between infiltrating vs. reactive glands.
Regarding molecular pathology, the most important alterations that are considered as the main genetic drivers of PDAC are somatic mutations affecting four key genes: the oncogene KRAS and the tumor suppressors CDKN2A, TP53 and SMAD4 56,57. KRAS is the most common mutated gene in PDAC (up to 90-92% of cases); typical mutations occur in codons 12, 13 and 61 56-59. Microsatellite instability is a genetic alteration that can occur in up to 2% of PDAC; however, it is more common in colloid and medullary variant than in conventional PDAC, where it probably represents a percentage < 1% of all cases 41.
DIFFERENTIAL DIAGNOSIS
The most important differential diagnoses for conventional PDAC are summarized in Table II. The first to be considered is represented by chronic pancreatitis 30,60. From radiologic and macroscopic points of view, chronic pancreatitis may share several features with PDAC. It is important to underline that chronic pancreatitis with alcoholic or obstructive etiology usually involves the pancreas more widely than a neoplastic process, with a more rubbery and with a more gritty consistency of the parenchyma than in PDAC. From a microscopic point of view, the most important aspects to support the distinction between chronic pancreatitis and PDAC are certainly represented by the presence of vascular and neural invasion, and lymph node metastasis. Notably, the fibrosis of chronic pancreatitis may mimic the desmoplastic reaction of PDAC, and the degree of cell atypia should not be used as the most important criterion to rule out chronic pancreatitis, where the protracted inflammation may generate reactive cell alterations.
Table II.
Most relevant differential diagnoses for pancreatic ductal adenocarcinoma (PDAC), highlighting the histological aspect against PDAC diagnosis.
| PDAC versus: | Useful features versus PDAC |
|---|---|
| Chronic pancreatitis | Ductal lithiasis, dense inflammatory infiltration, no clear signs of infiltrating tumor (e.g.: nodal metastasis). |
| Autoimmune pancreatitis | Marked inflammation with abundant plasma cells concentrated around pancreatic ducts, obliterative venulitis, cellular fibro-inflammatory stroma with a storiform appearance An increased numbers of IgG4 plasma cells. |
| Reactive glands | Location of glands (the presence of “naked” glands in fat is very suggestive for PDAC), absence of mitotic figures, absence of stromal desmoplastic reaction. |
| Precursor lesions | The presence of a possible infiltrating component, which lacks in non-infiltrating precursor lesions, should be excluded through an extensive sampling. |
Autoimmune pancreatitis is another potential mimicker of PDAC, since it can present as a discrete, tumor-like lesion of the pancreas 61-67. The histological hallmarks of autoimmune pancreatitis are represented by a dense inflammation centered around pancreatic ducts, a cellular fibro-inflammatory stroma with a storiform appearance and a diffuse obliterative venulitis 61-67. A further potentially helpful analysis may include an immunohistochemical evaluation of plasma cells and of their IgG4+ sub-population, which is typically increased above all in type 1 autoimmune pancreatitis 64-67.
Another important differential diagnosis that can be encountered during routine diagnostic activity is represented by reactive glands. From a microscopic point of view, the most helpful findings in distinguishing PDAC from reactive glands are represented by the location and the architecture of glands, in addition to the cytological aspects 16,30. The presence of “naked” glands in fat is a histological hallmark of PDAC, but attention must be paid to the fact that the adipose tissue may represent the result of adipose involution of normal pancreatic parenchyma rather than the true peri-pancreatic adipose tissue. In this case, residual neuroendocrine islets should be documented in fat tissue. Other features, that can support PDAC diagnosis are the presence of mitotic figures, necrotic luminal debris and stromal desmoplastic reaction.
The suggested immunohistochemical analysis to support a PDAC diagnosis in cases of doubtful histology include P53 and DPC4. P53 aberrant staining patterns, which are strictly correlated with TP53 mutations, are represented by a complete loss of immunostaining or by a diffuse nuclear staining in at least 60-70% of tumor cells 49,68. DPC4 aberrant staining pattern, which is strictly associated with SMAD4 mutations, is represented by loss of DPC4 nuclear expression 69.
Rarely, PDAC can exhibit a cystic appearance, thus the differential diagnoses include in such cases different types of cystic lesions. The cystic appearance may represent the macroscopic phenotype of a microscopic epiphenomenon (e.g.: PDAC intraductal colonization of a retention cyst or of a congenital cyst).
Acinar neoplasms
DEFINITION AND TERMINOLOGY
Although the acinar component constitutes the vast majority of the pancreatic parenchyma, neoplasms showing acinar cell differentiation are relatively rare. They include acinar cell carcinoma, along with its mixed subtypes (mixed acinar-ductal carcinoma, mixed acinar-neuroendocrine carcinoma, mixed acinar-neuroendocrine-ductal carcinoma), and pancreatoblastoma 16. In addition to these malignant neoplasms, the pancreas may undergo the so-called “acinar cystic transformation”, previously known as acinar cell cystadenoma, a non-neoplastic cystic lesion lined by acinar and ductal non-atypical cells, with no evidence of recurrence or malignant transformation.
ACINAR CELL CARCINOMA
Clinical and gross features
Acinar cell carcinomas (ACC) are rare neoplasms, accounting for only 1-2% of all pancreatic neoplasms in adults. The median age at ACC diagnosis is 60 years; however, it may also rarely affect children. Although ACC is predominantly located in the pancreatic head, jaudice is a rare symptom. Some patients may develop a lipase hypersecretion syndrome. The ACC patient prognosis is poor, with a 5-year survival rate of 25%.
Grossly, ACC are large, well-circumscribed and solid mass, with a homogeneous, fleshy cut surface 70-73. Necrotic or hemorrhagic areas may be present. In rare instances, the so-called “acinar cell cystadenocarcinomas”, gross appearance is entirely cystic.
Microscopic description with diagnostic hallmarks
Histologically, ACC is a highly cellular tumor, with scarce stroma. Tumor cells show granular eosinophilic, PAS-diastase-positive cytoplasm and relatively uniform nuclei with a characteristic single prominent eosinophilic nucleolus 16,70-72. Several architectural patterns (acinar, glandular, trabecular and solid), as well as the intraductal growth pattern have been described. The intraductal growth pattern is generally associated with a better prognosis. A representative image of an acinar cell carcinoma is provided in Figure 4A.
Figure 4.
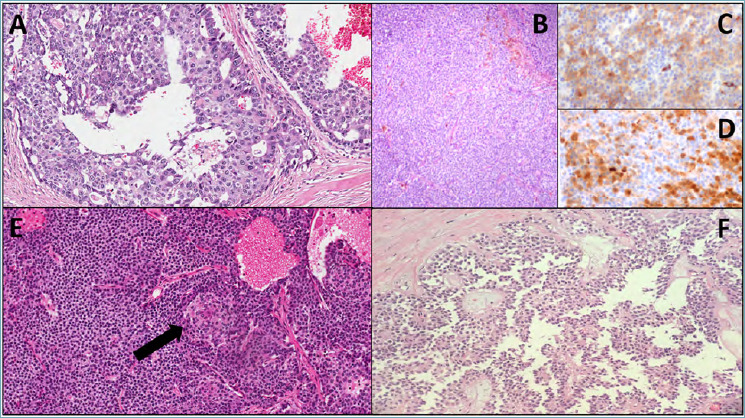
(A) Representative microscopic image of an acinar cell carcinoma, with aspects of intraductal growth (original magnification 20X); (B,C,D) Representative images of a mixed neuroendocrine-acinar neoplasm: B: hematoxylin-eosin staining (original magnification 10X), C: immunohistochemistry for synaptophysin (original magnification 20X), D: immunohistochemistry for trypsin (original magnification 20X); (E) representative histological image of a pancreatoblastoma, including a squamous nest, indicated with a black arrow (original magnification 20X); (F) representative microscopic image of a solid-pseudopapillary neoplasm (original magnification 10X).
Immunohistochemistry and molecular pathology
Immunohistochemistry is of pivotal importance to confirm the acinar cell differentiation. Trypsin, chymotrypsin and BCL-10 (clone 331.3, recognizing the COOH-terminal portion of carboxil ester lypase) are the most sensitive and specific immunohistochemical markers recommended for diagnosis. Pancreatic ductal markers, such as cytokeratins 7 and 19, as well as hepatocellular markers, such as HepPar-1, glypican 3, and alphafetoprotein, may be expressed by ACC 16,70-72.
Alterations in the Wnt/β-catenin pathway have been frequently found, often due to APC promoter hypermethylation 74. Microsatellite instability has been detected in about 10% of cases, while an ACC subset harbors potentially targetable gene fusions involving BRAF or RAF1 42,75.
Differential diagnosis
The main differential diagnoses include: pancreatoblastoma, pancreatic neuroendocrine neoplasm, solid pseudopapillary neoplasm, as well as medullary and hepatoid variants of pancreatic ductal adenocarcinoma (Tab. III).
Table III.
Histologic and immunohistochemical features helpful in the differential diagnosis of acinar and solid-pseudopapillary neoplasms
| Tumor type/subtype | Prominent nucleoli | Architectural patterns | Squamoid nests | Necrosis | Stroma | Acinar cell marker expression | Neuroendocrine marker expression | Important markers for diagnosis |
|---|---|---|---|---|---|---|---|---|
| Acinar cell carcinoma | Yes | Acinar, glandular, trabecular, solid | No | Frequent | Fibrous, scarce | Yes | No/focal, >30% in mixed |
Bcl10, trypsin |
| Pancreatoblastoma | Yes | Acinar, trabecular, solid | Yes | Possible | Fibrous, often hypercellular | Yes | Yes, often focal | Bcl10, trypsin; EMA-CK5-P63 (SN) |
| Pancreatic NET | Rare | Nesting, trabecular, glandular, solid | No | Very rare | Highly vascular, hyalinized | No | Yes, diffuse and strong | Chromogranin, Synaptophysin, Ki67 |
| NEC/large cell | Frequent | Nesting/trabecular, occasional rosettes | No | Frequent | Desmoplastic-type | No | Yes | Synaptophysin, TP53 |
| NEC/small cell | No | Diffuse sheets | No | Frequent | Desmoplastic-type | No | Yes | Synaptophysin, TP53, Rb |
| Medullary carcinoma | Yes | Solid, syncytial | No | Possible | Lymphocyte-rich | No | No | MMR proteins |
| Hepatoid carcinoma | Yes | Trabecular, glandular, solid | No | Possible | Scarce, occasionally lymphocyte-rich | No | Rare | Hep-par1, Arginase-1 |
| SPN | No | Solid, pseudopapillary | No | Possible | Fibrovascular, hyalinized | No | No/focal | β-catenin (nuclear), CD10, Progesteron receptor, LEF1, Vimentin, CD200 |
Abbreviations: NEC: neuroendocrine carcinoma; NET: neuroendocrine tumor; SN: squamoid nests; SPN: solid pseudopapillary neoplasm; MMR: mismatch repair.
TNM stage is the most important prognostic factor for ACC; they are staged with the same TNM staging system adopted for pancreatic ductal adenocarcinoma.
MIXED ACINAR CARCINOMAS
Mixed carcinomas (mixed acinar-ductal carcinoma, mixed acinar-neuroendocrine carcinoma, mixed acinar-neuroendocrine-ductal carcinoma) are defined as carcinomas composed of two or three different components, each constituting at least 30% of tumor volume 16.
Mixed acinar-neuroendocrine carcinomas account for about 20% of ACC (representative images are provided in Fig. 4B, C, D) Most acinar-neuroendocrine carcinomas do not display two morphologically distinct components, as the neuroendocrine differentiation is only recognized by immunohistochemistry. Such mixed acinar-neuroendocrine carcinomas do not fit the diagnosis of mixed neuroendocrine-non-neuroendocrine neoplasm (MiNEN), and should be regarded as a subtype of ACC. Indeed, their prognosis is similar to conventional ACC 72. However, rare true pancreatic MiNENs composed of separate acinar and neuroendocrine components have been reported 76. In such cases, the neuroendocrine component should be graded and reported in the final pathology report.
Mixed acinar-ductal carcinomas have either mucin deposits or a separate component strongly resembling a ductal adenocarcinoma, in addition to an acinar component. Mixed acinar-neuroendocrine-ductal carcinomas have a mixed composite morphology, with an immunohistochemical profile supporting the three lines of differentiation. Mixed acinar-ductal or acinar-neuroendocrine-ductal carcinomas usually have a poor prognosis.
PANCREATOBLASTOMA
Pancreatoblastoma is a rare malignant neoplasm with potential multiple lines of differentiation 16. Acinar cell differentiation is usually prominent. The median patient age at diagnosis is 3-4 years; however, cases in adults have been described. Pancreatoblastoma may be associated with Beckwith-Wiedenn syndrome and familial adenomatous polyposis syndrome (FAP), type 1.
Grossly, they are usually large, solid tumors, with soft yellowish lobules surrounded by fibrous bands on cut surface. Some cases may have a cystic appearance.
Histologically, the neoplasm shows a lobulated architecture, with highly cellular lobules separated by fibrous hypercellular septa. Most tumor cells are morphologically similar to those of ACC and most of them express acinar cell markers. The presence of a variable number of squamoid nests, composed of epitheliod-to-splindle cells showing squamous differentiation, is the histologic hallmark of the neoplasm and is crucial to establish correct diagnosis. A representative histologic image is provided in Figure 4E. Neoplastic cells within squamous nests may show nuclear clearing and abnormal nuclear or cytoplasmic positivity for β-catenin; CD200 may be also positive in the case of nuclear β-catenin staining 53,77,78.
Pancreatoblastomas may also express general markers of neuroendocrine differentiation (including CD200) and AFP. Molecular features of pancreatoblastoma are loss of 11p and alteration in Wnt/β-catenin pathway 79. Pancreatoblastomas may have ad indolent behavior, but the presence of metastasis and of a non-operable disease represent adverse prognostic factors.
Solid pseudopapillary neoplasms
DEFINITION AND TERMINOLOGY
Solid pseudopapillary neoplasm (SPN) of the pancreas is a low grade malignant epithelial tumor with uncertain cellular differentiation, first described by VK Frantz in 1959 80. It is a rare neoplasm, representing 0.9-2.7% of all pancreatic exocrine tumors 81; nonetheless, it accounts for 30% of all pancreatic neoplasms in patients younger than 40 years of age 82. SPNs were previously called “tumors” and considered to be benign or borderline lesions. They are now defined as malignant due to their demonstrated possibility to metastasize 83,84.
CLINICAL AND GROSS FEATURES
The vast majority of cases (90%) occur in adolescent girls and in young women (mean age 28 years). Cases involving male patients are very rare and tend to occur 5-10 years later in life with a more aggressive behavior 85,86. SPN is often an incidental finding in patients undergoing physical examination or imaging for other indications. Up to two-thirds of cases present with mass symptoms such as abdominal pain, discomfort, dyspepsia, nausea, vomiting or manifestations related to intratumoral hemorrhage. A small but significant percentage of patients present with acute hemoperitoneum 83. Tumor markers are generally normal, and there is no known association with genetic or paraneoplastic endocrine syndromes16. Metastases occur very rarely, mainly in the peritoneum and liver. The diagnosis is confirmed by imaging studies (ultrasound, MRI, CT); SPNs appear as well-demarcated neoplasms with both solid and cystic components. Calcifications are often seen, as well as fluid-debris levels 87,88. The long-term prognosis of SPNs after surgical resection is generally excellent.
SPNs may occur anywhere in the pancreas, although a slight preference for the body and tail region has been reported 89. Direct extension to surrounding organs, such as duodenum, spleen or the portal tract is rare but documented 16. SPNs tend to be solitary and well demarcated lesions, sometimes well-encapsulated, with a mean diameter around 10 cm (range: 0.5-25 cm). On cut sections, they typically show a mixture of solid and cystic areas. Solid areas have a characteristic yellow-light brown color and soft consistency, with macroscopically visible pseudopapillae; on the other hand, cystic areas are often filled with hemorrhagic and necrotic debris and may show calcification. Smaller lesions tend to be entirely solid, while other lesions may be completely cystic.
MICROSCOPIC DESCRIPTION WITH DIAGNOSTIC HALLMARKS
The microscopic features of SPN recapitulate its macroscopic appearance, with a mixture of solid, pseudopapillary and cystic-hemorrhagic areas. A representative histological image is provided in Figure 4F.
Solid areas are composed of loosely cohesive monomorphic polygonal cells admixed with capillary-sized blood vessels. In pseudopapillary areas, there is partial detachment of the neoplastic cells; the remaining elements are left to surround the blood vessels, therefore forming structures resembling papillae. The neoplastic cells are characterized by eosinophilic cytoplasm and uniform round-oval nuclei with granular chromatin, lacking a prominent nucleolus. Small PAS-Diastase positive hyaline globules are often found within the cytoplasm of the neoplastic cells and contain alpha-1 antitrypsin granules. Mitotic figures are absent or rare. Multinucleated atypical giant cells and nuclear pleomorphism are sometimes present, especially in older patients, and are considered to be degenerative changes rather than signs of malignancy 90. Foamy macrophages and cholesterol crystals are other common degenerative features typical of SPNs.
Foci of high-grade malignant transformation with high mitotic index may be present, and are associated with an extremely aggressive behavior 16. Despite its well-demarcated macroscopic appearance, SPNs may show infiltrative borders, with tumor cells surrounded by non-neoplastic pancreas without a desmoplastic reaction. The presence of infiltrative borders and capsular invasion are associated with local reoccurrence 91.
Although true tumor necrosis is rare, infarction is not uncommon, and can involve the lesion almost entirely. Pools of red blood cells, known as “blood lakes”, are typically present at the periphery of the lesion and should be distinguished from vascular invasion if tumor cells are present within them 83. The stroma around the neoplastic cells is usually scant and barely visible; when abundant, it may appear myxoid or hyaline. Calcifications are sometimes seen in the capsule.
Metastatic lesions tend to have the same morphologic features of the primary tumor; however, a higher degree of pleomorphism and mitotic activity may be present.
IMMUNOHISTOCHEMISTRY AND MOLECULAR PATHOLOGY
Over 90% of SPNs show nuclear/cytoplasmic expression of β-catenin, a finding which is often accompanied by loss of membranous expression of E-cadherin. The combination of these two markers is considered useful in the diagnosis of SPNs 92. Tumor cells are frequently positive for vimentin, CD56, neuron-specific enolase (NSE), alpha-1 antitrypsin, CD99. CD117 (c-kit) is expressed in up to 50% of cases, in absence of KIT mutations 93. Synaptophysin may be focally positive, while chromogranin A, trypsin, CEA and BCL-10 are consistently negative.
The key molecular feature of SPNs is the presence of somatic point mutations in exon 3 of the CTNNB1 gene, which encodes β-catenin. Such alterations are present in almost all cases and lead to defective phosphorylation and degradation of the β-catenin protein, which accumulates in the cytoplasm and nucleus of the neoplastic cells 84. Mutated β-catenin loses its function as an adhesion molecule, an event that could probably explain the poor cohesion of neoplastic cells. Recent evidences suggested that SPNs with malignant behavior harbor more often inactivating mutations of epigenetic regulators (KDM6A, TET1, BAP1) associated with metastatic disease 94.
Mutations in genes typically found in infiltrating ductal adenocarcinoma, such as KRAS, CDKN2A and SMAD4 have not been reported in SPNs; less than 5% of cases harbor TP53 mutations 83,95,96.
DIFFERENTIAL DIAGNOSIS
The main differential diagnoses are reported in Table III.
In case of diffuse cystic degeneration, SPNs may be radiologically and macroscopically confused with pancreatic pseudocysts. Clinical findings are important in distinguishing these two entities, since pseudocysts arise more commonly in men with a history of chronic pancreatitis, whereas SPNs typically occur in young women with no history of chronic disease. Microscopically, pseudocysts are characterized by the absence of an epithelial lining and of the classic neoplastic SPN cells.
Another important differential diagnosis for SPNs, above all in the case of solid appearance, is represented by well-differentiated neuroendocrine neoplasms. In this context, after a careful histologic examination, immunohistochemistry may be of great importance for completing this challenging distinction. Although SPNs and neuroendocrine neoplasm may share the positive expression for some markers, such as synaptophysin and CD200 54, at the same time SPNs have a distinct IHC profile, including the positivity for β-catenin (aberrant nuclear pattern), progesterone-receptor, CD10, vimentin and are constantly negative for chromogranin A (excluding a well-differentiated neuroendocrine neoplasm) and BCL-10 (excluding an acinar cell carcinoma).
The final pathology report for pancreatic malignant/exocrine tumors
The final pathology report for malignant/exocrine tumors of the pancreas should include some important points to both support the diagnosis and to permit an adequate oncologic staging.
Accordingly to the current TNM staging system, the most important information for resectable PDAC is represented by tumor size and number of metastatic lymph nodes 21. Furthermore, the status of all resection margins should be reported.
For tumors of pancreatic head, resection margins include: the pancreatic neck margin, the biliary margin, the retroperitoneal margin (posterior lamina) and the intestinal margins (one gastric and one intestinal in the case of Whipple procedure). Lymph nodes should be divided differentiating them into intestinal (duodenal), peri-gastric (Whipple procedure), pancreatic-duodenal (dividing them in anterior and posterior may be helpful, although it is not required by TNM staging system), peri-choloedocic and superior mesenteric artery lymph nodes (in the retroperitoneal margin). Other useful parameters to be reported are represented by vascular invasion, perineural invasion and adipose tissue infiltration. For PDAC, the grading of the tumor and the contemporary presence of dysplastic modifications of non-neoplastic ducts (e.g. PanIN, that supports the pancreatic primitiveness of the tumor) should be reported.
For tumors of the body-tail, the status of pancreatic transection margin must be reported. If tumors invade the anterior/posterior surfaces, this aspect should be mentioned in the final pathology report. Lymph nodes should be divided differentiating them into peri-pancreatic nodes (ideally identifying postero-superior nodes, which are classically located very closely to splenic vessels, and inferior nodes, although this distinction is not taken into account by TNM staging system) and the lymph nodes of splenic hilus. As for tumors affecting the pancreatic head, other useful parameters to be reported are represented by vascular invasion, perineural invasion and adipose tissue infiltration. For PDAC, in addition, grading of the tumor and the contemporary presence of dysplastic modifications of non-neoplastic ducts (e.g. PanIN, that supports the pancreatic primitiveness of the tumor) should be reported.
Figures and tables
References
- 1.Brierley JD, Gospodarowicz MK, Wittekind C. TNM Classification of Malignant Tumours. Oxfor: John Wiley & Sons, 2016. p. 274. [Google Scholar]
- 2.Neoptolemos JP, Stocken DD, Dunn JA, et al. Influence of resection margins on survival for patients with pancreatic cancer treated by adjuvant chemoradiation and/or chemotherapy in the ESPAC-1 randomized controlled trial. Ann Surg 2001;234:758-68. https://doi.org/10.1097/00000658-200112000-00007 10.1097/00000658-200112000-00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang B, Lee G, Qadan M, et al. Revision of pancreatic neck margins based on intraoperative frozen section analysis is associated with improved survival in patients undergoing pancreatectomy for ductal adenocarcinoma. Ann Surg 2019. December 5. https://doi.org/10.1097/SLA.0000000000003503. 10.1097/SLA.0000000000003503 Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 4.Lad NL, Squires MH, Maithel SK, et al. Is it time to stop checking frozen section neck margins during pancreaticoduodenectomy? Ann Surg Oncol 2013;20:3626-33. https://doi.org/10.1245/s10434-013-3080-9 10.1245/s10434-013-3080-9 [DOI] [PubMed] [Google Scholar]
- 5.Verbeke CS, Leitch D, Menon KV, et al. Redefining the R1 resection in pancreatic cancer. Br J Surg 2006;93:1232-7. https://doi.org/10.1002/bjs.5397 10.1002/bjs.5397 [DOI] [PubMed] [Google Scholar]
- 6.Lüttges J, Zamboni G, Klöppel G. Recommendation for the examination of pancreaticoduodenectomy specimens removed from patients with carcinoma of the exocrine pancreas. A proposal for a standardized pathological staging of pancreaticoduodenectomy specimens including a checklist. Dig Surg 1999;16:291-6. https://doi.org/10.1159/000018738 10.1159/000018738 [DOI] [PubMed] [Google Scholar]
- 7.Takahashi D, Kojima M, Sugimoto M, et al. Pathologic evaluation of surgical margins in pancreatic cancer specimens using color coding with tissue marking dyes. Pancreas 2018;47:830-6. https://doi.org/10.1097/MPA.0000000000001106 10.1097/MPA.0000000000001106 [DOI] [PubMed] [Google Scholar]
- 8.Verbeke CS, Gladhaug IP. Dissection of pancreatic resection specimens. Surg Pathol Clin 2016;9:523-38. https://doi.org/10.1016/j.path.2016.05.001 10.1016/j.path.2016.05.001 [DOI] [PubMed] [Google Scholar]
- 9.Grillo F, Ferro J, Vanoli A, et al. Comparison of pathology sampling protocols for pancreatoduodenectomy specimens. Virchows Arch 2020;476:735-44. https://doi.org/10.1007/s00428-019-02687-6 10.1007/s00428-019-02687-6 [DOI] [PubMed] [Google Scholar]
- 10.Adsay NV, Basturk O, Saka B, et al. Whipple made simple for surgical pathologists: orientation, dissection, and sampling of pancreaticoduodenectomy specimens for a more practical and accurate evaluation of pancreatic, distal common bile duct, and ampullary tumors. Am J Surg Pathol 2014;38:480-93. https://doi.org/10.1097/PAS.0000000000000165 10.1097/PAS.0000000000000165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adsay V, Mino-Kenudson M, Furukawa T, et al. Pathologic evaluation and reporting of intraductal papillary mucinous neoplasms of the pancreas and other tumoral intraepithelial neoplasms of pancreatobiliary tract: recommendations of Verona Consensus Meeting. Ann Surg 2016;263:162-77. https://doi.org/10.1097/SLA.0000000000001173 10.1097/SLA.0000000000001173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Verbeke C, Löhr M, Karlsson JS, Del Chiaro M. Pathology reporting of pancreatic cancer following neoadjuvant therapy: challenges and uncertainties. Cancer Treat Rev 2015;41:17-26. https://doi.org/10.1016/j.ctrv.2014.11.002 10.1016/j.ctrv.2014.11.002 [DOI] [PubMed] [Google Scholar]
- 13.Soer E, Brosens L, van de Vijver M, et al. Dilemmas for the pathologist in the oncologic assessment of pancreatoduodenectomy specimens: an overview of different grossing approaches and the relevance of the histopathological characteristics in the oncologic assessment of pancreatoduodenectomy specimens. Virchows Arch 2018;472:533-43. https://doi.org/10.1007/s00428-018-2321-5 10.1007/s00428-018-2321-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Campbell F, Smith RA, Whelan P, et al. Classification of R1 resections for pancreatic cancer: the prognostic relevance of tumour involvement within 1 mm of a resection margin. Histopathology 2009;55:277-83. https://doi.org/10.1111/j.1365-2559.2009.03376.x 10.1111/j.1365-2559.2009.03376.x [DOI] [PubMed] [Google Scholar]
- 15.Verbeke C, H äberle L, Lenggenhager D, et al. Pathology assessment of pancreatic cancer following neoadjuvant treatment: time to move on. Pancreatology 2018;S1424-3903(18)30077-2. https://doi.org/ 10.1016/j.pan.2018.04.010 10.1016/j.pan.2018.04.010 [DOI] [PubMed] [Google Scholar]
- 16.WHO Classification of Tumours Editorial Board. WHO Classification of Tumours. 5th ed. Lyon: IARC press; 2019. [Google Scholar]
- 17.Luchini C, Pea A, Yu J, et al. Pancreatic cancer arising in the remnant pancreas is not always a relapse of the preceding primary. Mod Pathol 2019;32:659-65. https://doi.org/10.1038/s41379-018-0183-7 10.1038/s41379-018-0183-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.He J, Ahuja N, Makary MA, et al. 2564 resected periampullary adenocarcinomas at a single institution: trends over three decades. HPB (Oxford) 2014;16:83-90. https://doi.org/10.1111/hpb.12078 10.1111/hpb.12078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amin MB, Edge S, Greene F, et al. : AJCC Cancer Staging Manual. 8th ed. Springer International Publishing; 2017. [Google Scholar]
- 20.Riva G, Pea A, Pilati C, et al. Histo-molecular oncogenesis of pancreatic cancer: From precancerous lesions to invasive ductal adenocarcinoma. World J Gastrointest Oncol 2018;10:317-27. https://doi.org/10.4251/wjgo.v10.i10.317 10.4251/wjgo.v10.i10.317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zamboni G, Hirabayashi K, Castelli P, Lennon AM. Precancerous lesions of the pancreas. Best Pract Res Clin Gastroenterol 2013;27:299-322. https://doi.org/10.1016/j.bpg.2013.04.001 10.1016/j.bpg.2013.04.001 [DOI] [PubMed] [Google Scholar]
- 22.Meyers N, Gérard C, Lemaigre FP, Jacquemin P. Differential impact of the ERBB receptors EGFR and ERBB2 on the initiation of precursor lesions of pancreatic ductal adenocarcinoma. Sci Rep 2020;10:5241. Published 2020 Mar 23. https://doi.org/10.1038/s41598-020-62106-8. 10.1038/s41598-020-62106-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bazzichetto C, Conciatori F, Luchini C, et al. From Genetic alterations to tumor microenvironment: The Ariadne’s String in Pancreatic Cancer. Cells 2020;9:309. Published 2020 Jan 28. https://doi.org/10.3390/cells9020309 10.3390/cells9020309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Basturk O, Hong SM, Wood LD, et al. A revised classification system and recommendations from the Baltimore Consensus meeting for neoplastic precursor lesions in the pancreas. Am J Surg Pathol 2015;39:1730-41. https://doi.org/10.1097/PAS.0000000000000533 10.1097/PAS.0000000000000533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sereni E, Luchini C, Salvia R, et al. Molecular and clinical patterns of local progression in the pancreatic remnant following resection of pancreatic intraductal papillary mucinous neoplasm (IPMN). Chin Clin Oncol 2019;8:21. https://doi.org/ 10.21037/cco.2019.04.03 10.21037/cco.2019.04.03 [DOI] [PubMed] [Google Scholar]
- 26.Pea A, Yu J, Rezaee N, et al. Targeted DNA Sequencing Reveals Patterns of Local Progression in the Pancreatic Remnant Following Resection of Intraductal Papillary Mucinous Neoplasm (IPMN) of the Pancreas. Ann Surg 2017;266:133-41. https://doi.org/10.1097/SLA.0000000000001817 10.1097/SLA.0000000000001817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Felsenstein M, Noë M, Masica DL, et al. IPMNs with co-occurring invasive cancers: neighbours but not always relatives. Gut 2018;67:1652-62. https://doi.org/10.1136/gutjnl-2017-315062 10.1136/gutjnl-2017-315062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scarpa A, Real FX, Luchini C. Genetic unrelatedness of co-occurring pancreatic adenocarcinomas and IPMNs challenges current views of clinical management. Gut 2018;67:1561-3. https://doi.org/10.1136/gutjnl-2018-316151 10.1136/gutjnl-2018-316151 [DOI] [PubMed] [Google Scholar]
- 29.Lupinacci RM, Goloudina A, Buhard O, et al. Prevalence of microsatellite instability in intraductal papillary mucinous neoplasms of the pancreas. Gastroenterology 2018;154:1061-5. https://doi.org/10.1053/j.gastro.2017.11.009 10.1053/j.gastro.2017.11.009 [DOI] [PubMed] [Google Scholar]
- 30.Luchini C, Capelli P, Scarpa A. Pancreatic ductal adenocarcinoma and its variants. Surg Pathol Clin 2016;9:547-60. https://doi.org/10.1016/j.path.2016.05.003 10.1016/j.path.2016.05.003 [DOI] [PubMed] [Google Scholar]
- 31.Veronese N, Nottegar A, Pea A, et al. Prognostic impact and implications of extracapsular lymph node involvement in colorectal cancer: a systematic review with meta-analysis. Ann Oncol 2016;27:42-8. https://doi.org/10.1093/annonc/mdv494 10.1093/annonc/mdv494 [DOI] [PubMed] [Google Scholar]
- 32.Veronese N, Fassan M, Wood LD, et al. Extranodal extension of nodal metastases is a poor prognostic indicator in gastric cancer: a systematic review and meta-analysis. J Gastrointest Surg 2016;20:1692-8. https://doi.org/10.1007/s11605-016-3199-7 10.1007/s11605-016-3199-7 [DOI] [PubMed] [Google Scholar]
- 33.Luchini C, Veronese N, Pea A, et al. Extranodal extension in N1-adenocarcinoma of the pancreas and papilla of Vater: a systematic review and meta-analysis of its prognostic significance. Eur J Gastroenterol Hepatol 2016;28:205-9. [DOI] [PubMed] [Google Scholar]
- 34.Karamitopoulou E, Wartenberg M, Zlobec I, et al. Tumour budding in pancreatic cancer revisited: validation of the ITBCC scoring system. Histopathology 2018;73:137-46. [DOI] [PubMed] [Google Scholar]
- 35.Lawlor RT, Veronese N, Nottegar A, et al. Prognostic role of high-grade tumor budding in pancreatic ductal adenocarcinoma: a systematic review and meta-analysis with a focus on epithelial to mesenchymal transition. Cancers (Basel) 2019;11:113. Published 2019 Jan 19. https://doi.org/10.3390/cancers11010113 10.3390/cancers11010113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hong SM, Jung D, Kiemen A, et al. Three-dimensional visualization of cleared human pancreas cancer reveals that sustained epithelial-to-mesenchymal transition is not required for venous invasion. Mod Pathol 2020;33:639-47. https://doi.org/10.1038/s41379-019-0409-3 10.1038/s41379-019-0409-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Basturk O, Khanani F, Sarkar F, et al. DeltaNp63 expression in pancreas and pancreatic neoplasia. Mod Pathol 2005;18:1193-8. https://doi.org/10.1038/modpathol.3800401 10.1038/modpathol.3800401 [DOI] [PubMed] [Google Scholar]
- 38.Liu C, Karam R, Zhou Y, et al. The UPF1 RNA surveillance gene is commonly mutated in pancreatic adenosquamous carcinoma. Nat Med 2014;20:596-8. https://doi.org/10.1038/nm.3548 10.1038/nm.3548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Boecker J, Feyerabend B, Tiemann K, et al. Adenosquamous carcinoma of the pancreas comprise a heterogeneous group of tumors with the worst outcome: a clinicopathological analysis of 25 cases identified in 562 pancreatic carcinomas resected with curative intent. Pancreas 2020;49:683-91. https://doi.org/10.1097/MPA.0000000000001548 10.1097/MPA.0000000000001548 [DOI] [PubMed] [Google Scholar]
- 40.Amato E, Molin MD, Mafficini A, et al. Targeted next-generation sequencing of cancer genes dissects the molecular profiles of intraductal papillary neoplasms of the pancreas. J Pathol 2014;233:217-27. https://doi.org/10.1002/path.4344 10.1002/path.4344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Luchini C, Brosens LAA, Wood LD, et al. Comprehensive characterisation of pancreatic ductal adenocarcinoma with microsatellite instability: histology, molecular pathology and clinical implications [published online ahead of print, 2020 Apr 29]. Gut 2020;gutjnl-2020-320726. https://doi.org/10.1136/gutjnl-2020-320726 10.1136/gutjnl-2020-320726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Luchini C, Bibeau F, Ligtenberg MJL, et al. ESMO recommendations on microsatellite instability testing for immunotherapy in cancer, and its relationship with PD-1/PD-L1 expression and tumour mutational burden: a systematic review-based approach. Ann Oncol 2019;30:1232-43. https://doi.org/10.1093/annonc/mdz116 10.1093/annonc/mdz116 [DOI] [PubMed] [Google Scholar]
- 43.Wilentz RE, Goggins M, Redston M, et al. Genetic, immunohistochemical, and clinical features of medullary carcinoma of the pancreas: A newly described and characterized entity. Am J Pathol 2000;156:1641-51. https://doi.org/10.1016/S0002-9440(10)65035-3 10.1016/S0002-9440(10)65035-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kryklyva V, ter Linden E, Kroeze LI, et al. Medullary pancreatic carcinoma due to somatic POLE mutation: a distinctive pancreatic carcinoma with marked long-term survival. Pancreas 2020;49:999-1003. https://doi.org/ 10.1097/MPA.0000000000001588 10.1097/MPA.0000000000001588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Agaimy A, Haller F, Frohnauer J, et al. Pancreatic undifferentiated rhabdoid carcinoma: KRAS alterations and SMARCB1 expression status define two subtypes. Mod Pathol 2015;28:248-60. https://doi.org/10.1038/modpathol.2014.100 10.1038/modpathol.2014.100 [DOI] [PubMed] [Google Scholar]
- 46.Ishida K, Yamashita R, Osakabe M, et al. Expression of epithelial-mesenchymal transition proteins in pancreatic anaplastic (undifferentiated) carcinoma. Pancreas 2019;48:36-42. https://doi.org/10.1097/MPA.0000000000001199 10.1097/MPA.0000000000001199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mattiolo P, Fiadone G, Paolino G, et al. Epithelial-mesenchymal transition in undifferentiated carcinoma of the pancreas with and without osteoclast-like giant cells. Virchows Arch 2020. July 13. https://doi.org/ 10.1007/s00428-020-02889-3. Online ahead of print. 10.1007/s00428-020-02889-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Muraki T, Reid MD, Basturk O, et al. Undifferentiated carcinoma with osteoclastic giant cells of the pancreas: clinicopathologic analysis of 38 cases highlights a more protracted clinical course than currently appreciated. Am J Surg Pathol 2016;40:1203-16. https://doi.org/10.1097/PAS.0000000000000689 10.1097/PAS.0000000000000689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Luchini C, Pea A, Lionheart G, et al. Pancreatic undifferentiated carcinoma with osteoclast-like giant cells is genetically similar to, but clinically distinct from, conventional ductal adenocarcinoma. J Pathol 2017;243:148-54. https://doi.org/10.1002/path.4941 10.1002/path.4941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Luchini C, Cros J, Pea A, et al. PD-1, PD-L1, and CD163 in pancreatic undifferentiated carcinoma with osteoclast-like giant cells: expression patterns and clinical implications. Hum Pathol 2018;81:157-65. https://doi.org/10.1016/j.humpath.2018.07.006 10.1016/j.humpath.2018.07.006 [DOI] [PubMed] [Google Scholar]
- 51.Moll R, Löwe A, Laufer J, Franke WW. Cytokeratin 20 in human carcinomas. A new histodiagnostic marker detected by monoclonal antibodies. Am J Pathol 1992;140:427-47. [PMC free article] [PubMed] [Google Scholar]
- 52.Nagata K, Horinouchi M, Saitou M, et al. Mucin expression profile in pancreatic cancer and the precursor lesions. J Hepatobiliary Pancreat Surg 2007;14:243-54. https://doi.org/10.1007/s00534-006-1169-2 10.1007/s00534-006-1169-2 [DOI] [PubMed] [Google Scholar]
- 53.Terada T, Ohta T, Sasaki M, et al. Expression of muc apomucins in normal pancreas and pancreatic tumours. J Pathol 1996;180:160-5. [DOI] [PubMed] [Google Scholar]
- 54.Lawlor RT, Daprà V, Girolami I, et al. CD200 expression is a feature of solid pseudopapillary neoplasms of the pancreas. Virchows Arch 2019;474:105-9. https://doi.org/10.1007/s00428-018-2437-7 10.1007/s00428-018-2437-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Xu JZ, Wang WQ, Zhang WH, et al. The Loss of SMAD4/DPC4 expression associated with a strongly activated hedgehog signaling pathway predicts poor prognosis in resected pancreatic cancer. J Cancer 2019;10:4123-31. Published 2019 Jul 10. https://doi.org/10.7150/jca.30883 10.7150/jca.30883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Waddell N, Pajic M, Patch AM, et al. Whole genomes redefine the mutational landscape of pancreatic cancer. Nature 2015;518(7540):495-501. https://doi.org/10.1038/nature14169 10.1038/nature14169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bailey P, Chang DK, Nones K, et al. Genomic analyses identify molecular subtypes of pancreatic cancer. Nature 2016;531(7592):47-52. https://doi.org/10.1038/nature16965 10.1038/nature16965 [DOI] [PubMed] [Google Scholar]
- 58.Almoguera C, Shibata D, Forrester K, et al. Most human carcinomas of the exocrine pancreas contain mutant c-K-ras genes. Cell 1988;53:549-54. https://doi.org/10.1016/0092-8674(88)90571-5 10.1016/0092-8674(88)90571-5 [DOI] [PubMed] [Google Scholar]
- 59.Singhi AD, George B, Greenbowe JR, et al. Real-time targeted genome profile analysis of pancreatic ductal adenocarcinomas identifies genetic alterations that might be targeted with existing drugs or used as biomarkers. Gastroenterology 2019;156:2242-53.e4. https://doi.org/10.1053/j.gastro.2019.02.037 10.1053/j.gastro.2019.02.037 [DOI] [PubMed] [Google Scholar]
- 60.Adsay NV, Bandyopadhyay S, Basturk O, et al. Chronic pancreatitis or pancreatic ductal adenocarcinoma? Semin Diagn Pathol 2004;21:268-76. https://doi.org/10.1053/j.semdp.2005.08.002 10.1053/j.semdp.2005.08.002 [DOI] [PubMed] [Google Scholar]
- 61.Zhang L, Chari S, Smyrk TC, et al. Autoimmune pancreatitis (AIP) type 1 and type 2: an international consensus study on histopathologic diagnostic criteria. Pancreas 2011;40:1172-9. https://doi.org/10.1097/MPA.0b013e318233bec5 10.1097/MPA.0b013e318233bec5 [DOI] [PubMed] [Google Scholar]
- 62.Zamboni G, Lüttges J, Capelli P, et al. Histopathological features of diagnostic and clinical relevance in autoimmune pancreatitis: a study on 53 resection specimens and 9 biopsy specimens. Virchows Arch 2004;445:552-63. https://doi.org/10.1007/s00428-004-1140-z 10.1007/s00428-004-1140-z [DOI] [PubMed] [Google Scholar]
- 63.De Marchi G, Paiella S, Luchini C, et al. Very high serum levels of CA 19-9 in autoimmune pancreatitis: Report of four cases and brief review of literature. J Dig Dis 2016;17:697-702. https://doi.org/10.1111/1751-2980.12403 10.1111/1751-2980.12403 [DOI] [PubMed] [Google Scholar]
- 64.Detlefsen S, Zamboni G, Frulloni L, et al. Clinical features and relapse rates after surgery in type 1 autoimmune pancreatitis differ from type 2: a study of 114 surgically treated European patients. Pancreatology 2012;12:276-83. https://doi.org/10.1016/j.pan.2012.03.055 10.1016/j.pan.2012.03.055 [DOI] [PubMed] [Google Scholar]
- 65.Zhang L, Smyrk TC. Autoimmune pancreatitis and IgG4-related systemic diseases. Int J Clin Exp Pathol 2010;3:491-504. Published 2010 May 25. [PMC free article] [PubMed] [Google Scholar]
- 66.Zhang L, Notohara K, Levy MJ, et al. IgG4-positive plasma cell infiltration in the diagnosis of autoimmune pancreatitis. Mod Pathol 2007;20:23-8. https://doi.org/10.1038/modpathol.3800689 10.1038/modpathol.3800689 [DOI] [PubMed] [Google Scholar]
- 67.Esposito I, Hruban RH, Verbeke C, et al. Guidelines on the histopathology of chronic pancreatitis. Recommendations from the working group for the international consensus guidelines for chronic pancreatitis in collaboration with the International Association of Pancreatology, the American Pancreatic Association, the Japan Pancreas Society, and the European Pancreatic Club. Pancreatology 2020;20:586-93. https://doi.org/10.1016/j.pan.2020.04.009 10.1016/j.pan.2020.04.009 [DOI] [PubMed] [Google Scholar]
- 68.Yemelyanova A, Vang R, Kshirsagar M, et al. Immunohistochemical staining patterns of p53 can serve as a surrogate marker for TP53 mutations in ovarian carcinoma: an immunohistochemical and nucleotide sequencing analysis. Mod Pathol 2011;24:1248-53. https://doi.org/10.1038/modpathol.2011.85 10.1038/modpathol.2011.85 [DOI] [PubMed] [Google Scholar]
- 69.Ritterhouse LL, Wu EY, Kim WG, et al. Loss of SMAD4 protein expression in gastrointestinal and extra-gastrointestinal carcinomas. Histopathology 2019;75:546-51. https://doi.org/10.1111/his.13894 10.1111/his.13894 [DOI] [PubMed] [Google Scholar]
- 70.Klimstra DS, Adsay V. Acinar neoplasms of the pancreas-A summary of 25 years of research. Semin Diagn Pathol 2016;33:307-18. https://doi.org/10.1053/j.semdp.2016.05.009 10.1053/j.semdp.2016.05.009 [DOI] [PubMed] [Google Scholar]
- 71.Klimstra DS, Heffess CS, Oertel JE, et al. Acinar cell carcinoma of the pancreas. A clinicopathologic study of 28 cases. Am J Surg Pathol 1992;16:815-37. https://doi.org/10.1097/00000478-199209000-00001 10.1097/00000478-199209000-00001 [DOI] [PubMed] [Google Scholar]
- 72.La Rosa S, Adsay V, Albarello L, et al. Clinicopathologic study of 62 acinar cell carcinomas of the pancreas: insights into the morphology and immunophenotype and search for prognostic markers. Am J Surg Pathol 2012;36:1782-95. https://doi.org/10.1097/PAS.0b013e318263209d 10.1097/PAS.0b013e318263209d [DOI] [PubMed] [Google Scholar]
- 73.La Rosa S, Sessa F, Capella C. Acinar cell carcinoma of the pancreas: overview of clinicopathologic features and insights into the molecular pathology. Front Med (Lausanne) 2015;2:41. Published 2015 Jun 15. https://doi.org/10.3389/fmed.2015.00041 10.3389/fmed.2015.00041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Furlan D, Sahnane N, Bernasconi B, et al. APC alterations are frequently involved in the pathogenesis of acinar cell carcinoma of the pancreas, mainly through gene loss and promoter hypermethylation. Virchows Arch 2014;464:553-64. https://doi.org/10.1007/s00428-014-1562-1 10.1007/s00428-014-1562-1 [DOI] [PubMed] [Google Scholar]
- 75.Chmielecki J, Hutchinson KE, Frampton GM, et al. Comprehensive genomic profiling of pancreatic acinar cell carcinomas identifies recurrent RAF fusions and frequent inactivation of DNA repair genes. [published correction appears in Cancer Discov 2015 Mar;5(3):332]. Cancer Discov 2014;4:1398-1405. https://doi.org/10.1158/2159-8290.CD-14-0617 10.1158/2159-8290.CD-14-0617 [DOI] [PubMed] [Google Scholar]
- 76.Klimstra DS, Rosai J, Heffess CS. Mixed acinar-endocrine carcinomas of the pancreas. Am J Surg Pathol 1994;18:765-78. https://doi.org/10.1097/00000478-199408000-00002 10.1097/00000478-199408000-00002 [DOI] [PubMed] [Google Scholar]
- 77.Ohike N, Morohoshi T. Exocrine pancreatic neoplasms of nonductal origin: acinar cell carcinoma, pancreatoblastoma, and solid-pseudopapillary neoplasm. Surg Pathol Clin 2011;4:579-88. https://doi.org/10.1016/j.path.2011.03.001 10.1016/j.path.2011.03.001 [DOI] [PubMed] [Google Scholar]
- 78.Tanaka Y, Kato K, Notohara K, et al. Significance of aberrant (cytoplasmic/nuclear) expression of beta-catenin in pancreatoblastoma. J Pathol 2003;199:185-90. https://doi.org/10.1002/path.1262 10.1002/path.1262 [DOI] [PubMed] [Google Scholar]
- 79.Wood LD, Klimstra DS. Pathology and genetics of pancreatic neoplasms with acinar differentiation. Semin Diagn Pathol 2014;31:491-7. https://doi.org/10.1053/j.semdp.2014.08.003 10.1053/j.semdp.2014.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kneeland Frantz V. Atlas of tumor pathology, Section VII, Fascicles 27 and 28. Tumors of the Pancreas. Washington, D.C.: Armed Forces Institute of Pathology; 1959. [Google Scholar]
- 81.Kosmahl M, Pauser U, Peters K, et al. Cystic neoplasms of the pancreas and tumor-like lesions with cystic features: a review of 418 cases and a classification proposal. Virchows Arch 2004;445:168-78. https://doi.org/10.1007/s00428-004-1043-z 10.1007/s00428-004-1043-z [DOI] [PubMed] [Google Scholar]
- 82.Konukiewitz B, Enosawa T, Klöppel G. Glucagon expression in cystic pancreatic neuroendocrine neoplasms: an immunohistochemical analysis. Virchows Arch 2011;458:47-53. https://doi.org/10.1007/s00428-010-0985-6 10.1007/s00428-010-0985-6 [DOI] [PubMed] [Google Scholar]
- 83.Hruban RH, Pitman MB, Klimstra DS. Tumors of the pancreas. American Registry of Pathology in collaboration with the Armed Forces Institute of Pathology 2007. [Google Scholar]
- 84.Abraham SC, Klimstra DS, Wilentz RE, et al. Solid-pseudopapillary tumors of the pancreas are genetically distinct from pancreatic ductal adenocarcinomas and almost always harbor beta-catenin mutations. Am J Pathol 2002;160:1361-9. https://doi.org/10.1016/s0002-9440(10)62563-1 10.1016/s0002-9440(10)62563-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Machado MC, Machado MA, Bacchella T, et al. Solid pseudopapillary neoplasm of the pancreas: distinct patterns of onset, diagnosis, and prognosis for male versus female patients. Surgery 2008;143:29-34. https://doi.org/10.1016/j.surg.2007.07.030 10.1016/j.surg.2007.07.030 [DOI] [PubMed] [Google Scholar]
- 86.Klöppel G, Morohoshi T, John HD, et al. Solid and cystic acinar cell tumour of the pancreas. A tumour in young women with favourable prognosis. Virchows Arch A Pathol Anat Histol 1981;392:171-83. [DOI] [PubMed] [Google Scholar]
- 87.Dong PR, Lu DS, Degregario F, et al. Solid and papillary neoplasm of the pancreas: radiological-pathological study of five cases and review of the literature. Clin Radiol 1996;51(10):702-5. https://doi.org/10.1016/s0009-9260(96)80242-x 10.1016/s0009-9260(96)80242-x [DOI] [PubMed] [Google Scholar]
- 88.Buetow PC, Buck JL, Pantongrag-Brown L, et al. Solid and papillary epithelial neoplasm of the pancreas: imaging-pathologic correlation on 56 cases. Radiology 1996;199:707-11. https://doi.org/10.1148/radiology.199.3.8637992 10.1148/radiology.199.3.8637992 [DOI] [PubMed] [Google Scholar]
- 89.Kang CM, Choi SH, Kim SC, et al. Predicting recurrence of pancreatic solid pseudopapillary tumors after surgical resection: a multicenter analysis in Korea. Ann Surg. 2014;260:348-55. https://doi.org/10.1097/SLA.0000000000000583 10.1097/SLA.0000000000000583 [DOI] [PubMed] [Google Scholar]
- 90.Kim SA, Kim MS, Kim MS, et al. Pleomorphic solid pseudopapillary neoplasm of the pancreas: degenerative change rather than high-grade malignant potential. Hum Pathol 2014;45:166-74. https://doi.org/10.1016/j.humpath.2013.08.016 10.1016/j.humpath.2013.08.016 [DOI] [PubMed] [Google Scholar]
- 91.Marchegiani G, Andrianello S, Massignani M, et al. Solid pseudopapillary tumors of the pancreas: Specific pathological features predict the likelihood of postoperative recurrence. J Surg Oncol 2016;114:597-601. https://doi.org/10.1002/jso.24380 10.1002/jso.24380 [DOI] [PubMed] [Google Scholar]
- 92.Kim MJ, Jang SJ, Yu E. Loss of E-cadherin and cytoplasmic-nuclear expression of beta-catenin are the most useful immunoprofiles in the diagnosis of solid-pseudopapillary neoplasm of the pancreas. Hum Pathol 2008;39:251-8. https://doi.org/10.1016/j.humpath.2007.06.014 10.1016/j.humpath.2007.06.014 [DOI] [PubMed] [Google Scholar]
- 93.Cao D, Antonescu C, Wong G, et al. Positive immunohistochemical staining of KIT in solid-pseudopapillary neoplasms of the pancreas is not associated with KIT/PDGFRA mutations. Mod Pathol 2006;19:1157-63. https://doi.org/10.1038/modpathol.3800647 10.1038/modpathol.3800647 [DOI] [PubMed] [Google Scholar]
- 94.Amato E, Mafficini A, Hirabayashi K, et al. Molecular alterations associated with metastases of solid pseudopapillary neoplasms of the pancreas. J Pathol 2019;247:123-34. https://doi.org/10.1002/path.5180 10.1002/path.5180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bartsch D, Bastian D, Barth P, et al. K-ras oncogene mutations indicate malignancy in cystic tumors of the pancreas. Ann Surg 1998;228:79-86. https://doi.org/10.1097/00000658-199807000-00012 10.1097/00000658-199807000-00012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fléjou JF, Boulange B, Bernades P, et al. p53 protein expression and DNA ploidy in cystic tumors of the pancreas. Pancreas 1996;13:247-52. https://doi.org/10.1097/00006676-199610000-00006 10.1097/00006676-199610000-00006 [DOI] [PubMed] [Google Scholar]


