Abstract
Introduction
Rise of central cytokines resulting from infections produces neuronal changes. Covid-19 allows the study of depressive symptoms in sustained stress and its relationship with molecular mechanisms.
Objectives
To assess correlation between IL-6, IL-1β and TNF-α and depressive symptoms. Characterize the depressive symptoms present.
Methods
Observational study. Patients admitted for Covid-19 older than 60 years with a interleukin determination were included. The Yesavage Geriatric Depression Scale was used, associating each item with a neurotransmitter.
Results
27 patients included. We did not find correlation between IL-6 levels and the GDS scale score (rho = 0.204; 95% CI −0.192 to 0.543); with IL-1β levels (rho = −0.126; 95% CI −0.490 to 0.276); nor of TNF-α (rho = −0.033; 95% CI −0.416 to 0.360). 3 patients (11.1%) presented score compatible with depressive disorder. It was associated with a deficiency of Noradrenaline and Serotonin.
Conclusions
We found no correlation between the levels of IL-6, IL-1β, and TNF-α with the GDS score. Depressive symptomatology is similar to vascular depressions.
Keywords: Depression, IL-6, Covid-19, Vascular, IL-1β, TNF-α
Abstract
Introducción
El incremento de citocinas centrales resultante de infecciones produce cambios neuronales. La Covid-19 permite estudiar los síntomas depresivos en un estrés sostenido y su relación con mecanismos moleculares.
Objetivos
Valorar la correlación entre niveles de IL-6, IL-1β y TNF-α y sintomatología depresiva. Caracterizar los cuadros depresivos presentes.
Métodos
Estudio observacional. Se incluyeron pacientes ingresados por Covid-19 mayores de 60 años con una determinación de interleucinas. Se utilizó la Escala de depresión geriátrica de Yesavage, asociándose cada ítem con un neurotransmisor.
Resultados
27 pacientes incluidos. No encontramos correlación entre los niveles de IL-6 y la puntuación de la escala GDS (rho = 0,204; IC95% −0.192 a 0.543); con los niveles de IL-1β (rho = −0,126; IC95% −0.490 a 0.276); ni de TNF-α (rho = −0,033; IC95% −0.416 a 0.360). 3 pacientes (11,1%) presentaron una puntuación compatible con cuadro depresivo. Se asoció a déficit de Noradrenalina y Serotonina.
Conclusiones
No hallamos correlación entre los niveles de IL-6, IL-1β y TNF-α con la puntuación en la GDS. La sintomatología depresiva presenta características similares a las depresiones vasculares.
Palabras clave: Depresión, IL-6, Covid-19, Vascular, IL-1β, TNF-α
Introduction
Psychological stress or the stress caused by an infection activates toll-like receptors which, once the NF-kB transcription factor or NLRP3 inflammasome and other inflammatory cytokines have been activated, increase the levels of interleukin 1 beta (IL-1β) and interleukin 6 (IL-6), leading to general disease symptoms as well as symptoms characteristic of depression such as dysphoria and anhedonia.1
Increased IL-1β, IL-6 and TNF-α as a result of infections or stress leads to stimulation of the glutamatergic NMDA and α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors, as well as a decrease in the expression of neuronal GABA-A receptors, causing an increase in reversible excitability.2
The NF-kB pathway complex is present in a wide variety of cells such as lymphocytes and endothelial cells. Activation of the NF-kB pathway and subsequent production of cytokines may be related to the deterioration of endothelial cells. In vitro and animal depression models have shown that TNF-α modifies the endothelial cells of the blood-brain barrier by increasing permeability and reducing tight junction protein expression associated with extracellular spaces. The NF-Kb-IKK signalling pathway has been associated with the regulation of neuronal morphology, necessary and sufficient to induce anxiety- and depression-like behaviours in mice.3
Benros et al. conclude that the increased risk of suffering from a mood disorder after hospitalization for infections and autoimmune diseases was 62% (RRI, 1.62; 95% CI 1.60–1.64) and 45% (RRI, 1.45; 95% CI 1.39–1.52) respectively. When they had both, the risk increased further (RRI, 2.35; 95% CI 2.25–2.46).4
Covid-19 provides a model for studying depression in the context of sustained stress and its correlation with molecular mechanisms.
The main objective of this study is to assess the correlation between IL-6 levels and depressive symptoms. Secondary objectives were to assess the same correlation between depressive symptoms and IL-1β and TNF-α levels, as well to characterise psychopathologically the depressive symptoms present during hospitalization.
Material and methods
Observational study. Patients admitted for covid-19 were included. The study was approved by the Clinical Research Ethics Committee of the León and El Bierzo Health Areas on 17th April 2020 (case file 2062).
Inclusion criteria:
-
1
Over 60 years of age admitted to hospital for covid-19 in whom determination of IL-6 is indicated.
-
2
Verbal informed consent.
Exclusion criteria:
-
-
Inability to complete clinical scales.
Verbal informed consent was chosen because it does not change the clinical intervention and because eliminating the need to use writing tools reduces the risk of contagion.
Laboratory and sociodemographic data were obtained from the medical records of the patients that were included.
The Yesavage Geriatric Depression Scale (GDS)5 was used for the evaluation of depressive symptoms (study variable) because it is easy to apply and has a study population-adapted profile.
The dichotomous structure of the GDS allows, in a hypothetical way, to correlate each item with a depressive symptom and, in turn, with the theoretical regulatory neurotransmitter (Table 1 ). A consensus was reached between 3 psychiatrists with more than 10 years of experience for this correlation. Although there may be discrepancies on its utility and accuracy, it allows for an approach that views depressive symptomatology as a continuum with normality, from a non-dualistic theoretical model, considering psychopathology as a symptom of a systemic disease.
Table 1.
Correlation of the questions of the Yesavage scale with psychopathology and associated neurotransmitters.
| Symptom | Neurotransmitter | |
|---|---|---|
| Are you basically satisfied with your life? | Hopelessness | SER |
| Have you given up many of your activities and interests? | Anergy | NA |
| Do you feel that your life is empty? | Hopelessness | SER |
| Are you often bored? | Anhedonia | DA |
| Are you hopeful for the future? | Hopelessness | SER |
| Are you troubled by thoughts you cannot get out of your head? | Rumination | SER |
| Are you often in good spirits? | General mood | SER |
| Are you afraid that something bad is happening to you? | Anxiety | NA |
| Do you feel happy most of the time? | Anhedonia | DA |
| Do you often feel helpless? | Loneliness | SER |
| Are you often restless and uneasy? | Restlessness | NA |
| Do you prefer to stay at home, rather than going out and doing new things? | Apathy | NA |
| Are you frequently worried about the future? | Rumination | SER |
| Do you feel you have more problems with memory than most? | Concentration | DA |
| Do you think it is wonderful to be alive now? | Anhedonia | DA |
| Do you often feel discouraged and melancholic? | Sadness | SER |
| Do you feel pretty worthless the way you are now? | Self esteem | SER |
| Are you very worried about the past? | Rumination | SER |
| Do you find life very stimulating? | Anhedonia | DA |
| Is it difficult for you to start new projects? | Anergy | NA |
| Do you feel full of energy? | Anergy | NA |
| Do you feel that your situation is hopeless? | Hopelessness | SER |
| Do you think that most people are better off than you are? | Hopelessness | SER |
| Are you often worried about little things? | Rumination | SER |
| Do you often feel like crying? | Lability | SER |
| Do you have trouble concentrating? | Concentration | DA |
| Do you feel better in the morning when you wake up? | Melancholic pole | SER |
| Do you prefer to avoid social gatherings? | Social phobia | SER |
| Is it easy for you to make decisions? | Doubt | SER |
| Is your mind as sharp as it used to be? | Concentration | DA |
Data collection was carried out at the León University Healthcare Complex (CAULE) between 17th April and 7th May 2020, when it was interrupted because requests for IL-6 levels ceased. We do not know the reason for this cessation, although it coincides with the end of the most intense phase of the pandemic.
Spearman's rho test was used to estimate the correlations.
Results
The determination of IL-6 levels was requested in the case of 48 admitted patients over the age of 60; 3 of them did not have Covid-19, 5 were admitted to the ICU, 2 died, 4 had cognitive abnormalities and 7 had been discharged or transferred. Finally, 27 patients were included in the study. Patients were detected through the Immunology laboratory, which reported the IL-6 determinations requested, regardless of the reason.
The sociodemographic and laboratory variables are shown in Table 2 . The profile of the patient over 60 years of age, admitted to the ward for Covid-19 whose IL-6 levels are requested is a male (70.4%), from rural areas (51.9%), and interleukin levels are requested around the eighth day of admission.
Table 2.
Study variables score.
| N | Minimum | Maximum | Mean | Deviation | |
|---|---|---|---|---|---|
| Age | 27 | 60 | 86 | 68.70 | 8.384 |
| Days of admission | 27 | 2 | 30 | 8.59 | 6.829 |
| IL-6 | 27 | 0.00 | 491.00 | 55.5785 | 110.85174 |
| IL-1B | 26 | 0.00 | 16.00 | 1.3477 | 3.06463 |
| TNF-alpha | 26 | 0.0 | 22.5 | 1.315 | 4.3663 |
| PCR | 27 | 1.00 | 377.70 | 85.9037 | 108.87488 |
| Ferritin | 27 | 48 | 4.315 | 1,297.56 | 1,138.221 |
| D-dimer | 27 | 119 | 56.645 | 3,772.81 | 10,788.393 |
| Haemoglobin | 27 | 8.50 | 15.40 | 12.8519 | 1.67318 |
| Red blood cells | 27 | 2.96 | 5.30 | 4.2456 | 0.60749 |
| Platelets | 27 | 7 | 639 | 232.07 | 132.877 |
| INR | 27 | 0.90 | 1.32 | 1.1100 | 0.10392 |
| Fibrinogen | 27 | 294 | 1.082 | 616.22 | 212.516 |
| Leukocytes | 27 | 0.40 | 18.30 | 8.6259 | 4.60231 |
| Neutrophils | 27 | 0.09 | 17.02 | 7.2315 | 4.38565 |
| Lymphocytes | 27 | 250 | 2.280 | 782.22 | 483.054 |
| SatO2 | 27 | 90 | 98 | 93.89 | 2.242 |
| Temperature | 27 | 34.50 | 37.10 | 36.1222 | 0.59247 |
| Systolic BP | 27 | 94 | 165 | 124.15 | 21.025 |
| Diastolic BP | 27 | 47 | 96 | 77.96 | 11.657 |
| Heart rate | 27 | 53 | 106 | 79.26 | 14.725 |
| Total GDS | 27 | 0 | 26 | 6.48 | 5.395 |
We found a mean elevation of IL-6 levels, strongly influenced by extreme values (median 11 pg/mL). Increased levels of CRP, ferritin, d-dimer and heart rate, and decreased oxygen saturation and lymphocytes were observed. The rest of the parameters remained at normal levels.
Psychopathologically, 3 of the 27 patients (11.1%) had a score on the GDS scale compatible with the presence of a depressive disorder.
We found no correlation between IL-6 levels and the score obtained on the GDS scale (Spearman's rho = 0.204; 95% CI from −0.192 to 0.543). We also found no correlation between the GDS scale and IL-1β levels (Spearman's rho = −0.126; 95%CI from −0.490 to 0.276); nor with TNF-α levels (Spearman's rho = −0.033; 95%CI from −0.416 to 0.360).
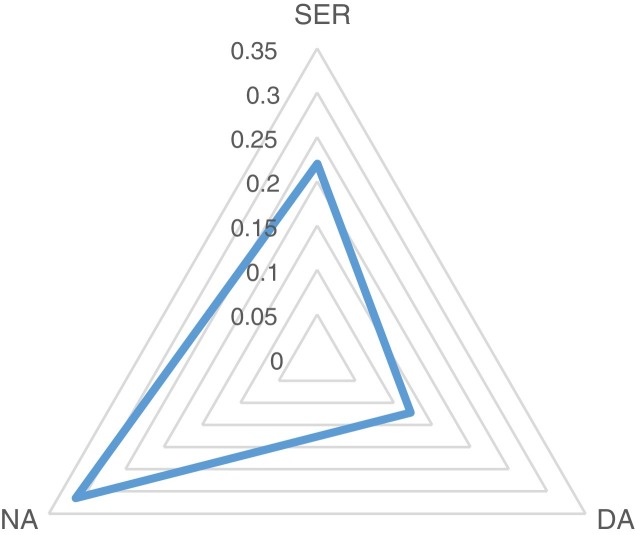
For the psychopathological characterization we performed a weighting between different neurotransmitters. According to Table 1, 17 items were assigned to serotonin, 6 to norepinephrine and 7 to dopamine. We divided the score obtained for each neurotransmitter by the number of items assigned. We found that the psychopathological condition shows symptoms associated with deficits in noradrenaline (mainly) and serotonin, and very little in dopamine. Fig. 1 shows the neurotransmitter abnormalities found.
Fig. 1.
Representation of the weighted values of different neurotransmitters (scale from 0 to 1). Serotonin: mean 0.22 ± 0.19; median 0.18. Noradrenaline: mean 0.31 ± 0.25; median 0.33. Dopamine: mean 0.12 ± 0.20; median 0.14.
Discussion
The sample was limited to patients admitted to hospital. Therefore, it cannot be extrapolated to the most severe conditions (patients admitted to the ICU have not been included), nor to mild conditions.
The scarcity of patients with GDS scale scores compatible with depressive symptoms stands out (only 3). Patients were in a situation of hospitalization for a little-known, potentially lethal disease, isolated and without visits. The mean stay at the time of assessment was higher than 8 days. We consider that the patients were subjected to a situation of intense stress, but the responses to the GDS scale hardly reflect the presence of depressive symptoms. It would be necessary to consider other factors with an effect on mood, such as the euphoric effect of corticosteroids or a direct effect of Covid-19 that could cause moria and even hyperthymia. As the prescribed treatment has not been collected and possible brain damage has not been examined, these factors cannot be determined, and research will need to be expanded in future studies.
The lack of correlation between interleukin levels and GDS scores could be influenced by the low sample size or because there is no correlation, although this would go against what is described in other conditions.6 The non-correlation would reinforce the claim that the disease or its treatment had an effect on mood.
We observe that the condition is characterized by a noradrenergic deficit, followed by a serotonergic deficit. This suggests that it shares characteristics with vascular depression.7 The fact that mood disorders in Covid-19 share a psychopathological profile with vascular depression is compatible with a process in which cardiovascular8, 9 and neurological disorders are evident.10 There was hardly any dopaminergic deficit-dependent symptomatology, which could be related to a euphoric effect of Covid-19 or its treatment.
Conclusions
There is no correlation between the levels of IL-6, IL-1β and TNF-α with the score obtained in the GDS in patients above 60 years of age with moderate Covid-19 symptoms.
Depressive symptoms in patients over 60 years of age with moderate Covid-19 symptoms shares characteristics with vascular depression, showing noradrenergic and serotonergic deficits.
Conflict of interests
None of the authors has a conflict of interest.
Footnotes
Please cite this article as: Serrano García A, Montánchez Mateo J, Franch Pato CM, Gómez Martínez R, García Vázquez P, González Rodríguez I. Relación entre los niveles de interleucina 6 y depresión en pacientes afectados por Covid-19. Med Clin (Barc). 2021;156:332–335.
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.medcle.2020.11.013.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Ramírez L.A., Pérez-Padilla E.A., García-Oscos F., Salgado H., Atzori M., Pineda J.C. Nueva teoría sobre la depresión: un equilibrio del ánimo entre el sistema nervioso y el inmunológico, con regulación de la serotonina-quinurenina y el eje hipotálamo-hipófiso-suprarrenal. Biomédica. 2018;38:437–450. doi: 10.7705/biomedica.v38i3.3688. [DOI] [PubMed] [Google Scholar]
- 2.Viviani B., Boraso M., Marchetti N., Marinovich M. Perspectives on neuroinflammation and excitotoxicity: a neurotoxic conspiracy? Neurotoxicology. 2014;43:10–20. doi: 10.1016/j.neuro.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 3.Ménard C., Hodes G.E., Russo S.J. Pathogenesis of depression: insights from human and rodent studies. Neuroscience. 2016;321:138–162. doi: 10.1016/j.neuroscience.2015.05.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benros M.E., Waltoft B.L., Nordentoft M., Ostergaard S.D., Eaton W.W., Krogh J., et al. Autoimmune diseases and severe infections as risk factors for mood disorders: a nationwide study. JAMA Psychiatry. 2013;70:812–820. doi: 10.1001/jamapsychiatry.2013.1111. [DOI] [PubMed] [Google Scholar]
- 5.Yesavage J.T., Rink T., Rose T., Aday M. In: Assessment in geriatric psychopharmacology. Crook T., Ferris S., Bartusleds R., editors. Mark Powley and Associates; New Canaan: 1983. Geriatric Depression Rating scale: comparison with self-report and psychiatric rating scales; pp. 153–167. [Google Scholar]
- 6.Sánchez J.M., Sánchez P.T., Peiró G., Sirera R., De Lamo M., Corbellas C., et al. Niveles séricos de il-6 y depresión en varones con cáncer de pulmón no microcítico avanzado. CM de Psicobioquimica. 2013;2:53–62. [Google Scholar]
- 7.Olivera-Pueyo J., Benabarre-Ciria S., Pelegrín-Valero C. Opciones Terapéuticas en depresiones vasculares. Psicogeriatría. 2008;0:35–41. [Google Scholar]
- 8.Guzik T.J., Mohiddin S.A., Dimarco A., Patel V., Savvatis K., Marelli-Berg F.M., et al. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. 2020;116:1666–1687. doi: 10.1093/cvr/cvaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castelnovo L., Capelli F., Tamburello A., Faggioli P.M., Mazzone A. Symmetric cutaneous vasculitis in COVID-19 pneumonia. J Eur Acad Dermatol Venereol. 2020;34:e362–e363. doi: 10.1111/jdv.16589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fotuhi M., Mian A., Meysami S., Raji C.A. Neurobiology of COVID-19. J Alzheimers Dis. 2020;76:3–19. doi: 10.3233/JAD-200581. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.