Abstract
Introduction:
Community health centers often screen for and address patients’ unmet social needs. This study examines the degree to which community health center patients report receiving social needs assistance and compares measures of access and quality between patients who received assistance versus similar patients who did not.
Methods:
A nationally representative sample of 4,699 nonelderly adults receiving care at community health centers from the 2014–2015 Health Resources and Services Administration Health Center Patient Survey was used, representing 12.6 million patients. The exposure—having “received social needs assistance”—was based on whether a patient received any community health center assistance accessing social programs (e.g., applying for government benefits) or basic needs (e.g., obtaining transportation, housing, food). Using logistic regression models with inverse probability of treatment weights, outcomes for patients who received social needs assistance with similar patients who did not were compared. Study outcomes, reported as absolute adjusted differences, included reporting a community health center as a usual source of care, reporting the emergency department as a usual source of care, perceived quality of care, and willingness to recommend the community health center to others. Data were analyzed in 2020.
Results:
Of the sample, 36% reported receiving social needs assistance, where the most common form of assistance was applying for government benefits. Relative to similar patients who did not receive social needs assistance, patients receiving assistance were significantly more likely to report a community health center as their usual source of care (adjusted difference=7.2 percentage points, 95% CI=2.2, 12.1) and to report perceived quality of care as “the best” (adjusted difference=11.1, 95% CI=5.4, 16.9). They were significantly less likely to report the emergency department as their usual source of care (adjusted difference= −4.2, 95% CI= −7.0, −1.3).
Conclusions:
As community health centers and other providers consider providing social needs assistance to patients, these results suggest that doing so may be associated with improved access to and quality of care.
INTRODUCTION
Lack of access to basic needs, such as stable housing or nutritious foods, can limit a patient’s ability to access care and negatively affect health outcomes.1-4 Patients with unmet social needs are twice as likely to use the emergency department (ED), twice as likely to have depression, and 1.5 times more likely to have high cholesterol.5 More than 90% of low-income people report having unmet social needs,6 and evidence suggests quality of care and health outcomes are often mediated by social risk factors, which are greater predictors of health outcomes than health care itself, accounting for one third of annual deaths.7
Community health centers (CHCs) deliver comprehensive, culturally competent, quality primary care services to >28 million low-income patients nationwide, irrespective of insurance coverage or ability to pay. CHC patients are often more socially complex and have worse health status than the general U.S. population.8-12 To receive federal funding, CHCs are required to provide comprehensive case management services, which include helping patients gain access to social services provided by federal, state, or local programs.13 CHCs are also more likely to assess unmet social needs relative to other sites of primary care.14,15 To do so, many CHCs integrate systematic processes to screen for unmet social needs16-19 and use screening results to refer or provide assistance in applying for social services.20
Although there is some evidence about the extent to which CHC patients are referred to social services, the types of social services provided, and to whom they are provided, less is known about the association between social needs assistance and quality and access to care.15,21,22 Recent evidence suggests that CHC patients report relatively high levels of social risk.22 Moreover, provision of enabling services—which include outreach, transportation, linguistic, and care coordination services—for CHC patients is associated with higher likelihoods of receiving preventive care, having an annual checkup, and better patient satisfaction; this is largely driven by care coordination services specifically.21,22 Other evidence suggests that on-site provision of social services at CHCs may also be associated with better performance on measures of healthcare quality; however, additional research on the association between receipt of social needs assistance and care continuity and perceived quality are needed.15
To fill this gap, using a nationally representative sample of CHC patients, this study builds on these findings by first examining the degree to which CHC patients report receiving social needs assistance and then comparing measures of access and perceived quality between patients who received assistance relative and similar patients who did not.
METHODS
Study Sample
Data from the 2014–2015 Health Center Patient Survey (HCPS), a cross-sectional survey of patients receiving care at CHCs funded by Health Resources and Services Administration’s Bureau of Primary Health Care, were used. Collected between September 2014 and April 2015, these are the only patient-level data to be collected post-Affordable Care Act (ACA) that are representative of all CHC patients across the U.S. Examples of survey domains include access to care, help received to access social programs, and satisfaction with care.
The HCPS is administered through the Health Resources and Services Administration and uses a 3-stage sampling design. The first-stage sampling units were CHCs, which were stratified by characteristics including demographics of the patient population, CHC size, geographic region, and rurality. The second-stage sampling units were sites within each CHC, and the third-stage sampling units were patients receiving care at the site. All surveyed patients had received face-to-face care at the CHC at least once in the past 12 months and were selected for in-person, 1-on-1 interviews when they registered with the CHC receptionist for a visit.
Measures
The outcomes for this study were as follows: (1) household enrollment in any social program (food stamps; Special Supplemental Nutrition Program for Women, Infants, and Children; Temporary Assistance for Needy Families; Section 8 Housing; or any other government assistance), (2) reporting a CHC as a usual source of care, (3) reporting the ED as a usual source of care, (4) having a routine checkup in the last year, (5) reporting perceived quality of care to be the “best possible” based on provider rating, and (6) willingness to recommend the CHC to family and friends.
The exposure was defined based on whether a patient received any CHC assistance (yes/no) with accessing social programs (e.g., applying for government benefits) or basic needs (e.g., transportation, housing, employment, obtaining food, and obtaining clothes). This group is referred to as having “received social needs assistance.” Survey questions and measure definitions are presented in Appendix Tables 1 and 2, available online. Appendix Figure 1, available online, shows the construction of the study sample, which included a final sample of 4,699 nonelderly adult CHC patients aged 18–64 years, representing 12.6 million CHC patients nationwide. About 341 respondents who reported not needing any of the services were excluded, and their characteristics were examined in a separate analysis. Although data were not available to examine why these respondents reported not needing any social services, potential reasons include having no perceived need for assistance or already being enrolled in social services and therefore not requiring CHC assistance.
Statistical Analysis
Descriptive statistics were generated to describe the percentage of the study sample who received each type of assistance.
To account for potential differences between patients who did versus did not receive social needs assistance, propensity scores were estimated using a logit model, where receipt of assistance was a binary outcome. The propensity score can be interpreted as the probability a patient received social needs assistance, given their observable sociodemographic, clinical, and state-level characteristics. Covariates for the propensity score model were selected if they were hypothesized to be a confounder or be associated with the outcome.23 Propensity scores were then used to calculate inverse probability of treatment weights (IPTWs), which served to balance on observable characteristics between the 2 groups, thus lessening the influence of selection bias. Building on previous work,21,24 the scores included 28 patient-level sociodemographic and clinical characteristics: age, gender, race/ethnicity, household income measured as a percentage of the federal poverty level, English proficiency, health insurance type (uninsured, public, or private), highest level of education attained, urban versus rural location, marital status, being born in the U.S., experiencing homelessness, sexual minority status, self-reported fair or poor health status, diagnosis of medical conditions (diabetes, hypertension, coronary heart disease, chronic obstructive pulmonary disease, angina, stroke, asthma, depression, generalized anxiety, or other mental health conditions [panic disorder, schizophrenia, or bipolar disorder]), patient type (e.g., general CHC patients, public housing, migrant and seasonal farm workers, or health care for the homeless), if they had visited this particular CHC for ≥5 years, and number of CHC visits in the last year. State-level covariates (e.g., Medicaid expansion status as of 2014) were included, as well as survey weights and sampling strata in the scores. To account for the complex survey design, the IPTWs were then multiplied by survey weights,25 and weights were normalized to a mean of 1. Covariate balance was assessed both before and after weighting by calculating standardized differences between those who received social needs assistance and those who did not. Standardized differences of ≥0.1 for a particular covariate suggest a meaningful imbalance between the 2 groups.26
Doubly robust logistic regression models with IPTWs were used to compare outcomes for patients who received social needs assistance with similar patients who did not, where the models directly adjusted for the covariates included in the propensity score model. SEs were clustered at the state level. Absolute adjusted differences were calculated using mean marginal effects. All analyses were conducted in 2020 using Stata, version 15.0.
RESULTS
Overall, 36% of the sample reported receiving any social needs assistance (Figure 1). The most common form of assistance was applying for government benefits (25.2%). Others reported receiving assistance with transportation (12.6%), obtaining food (5.5%), or finding employment (5.5%).
Figure 1. Proportion of health center patients receiving assistance to access social programs or basic needs, 2014–2015.
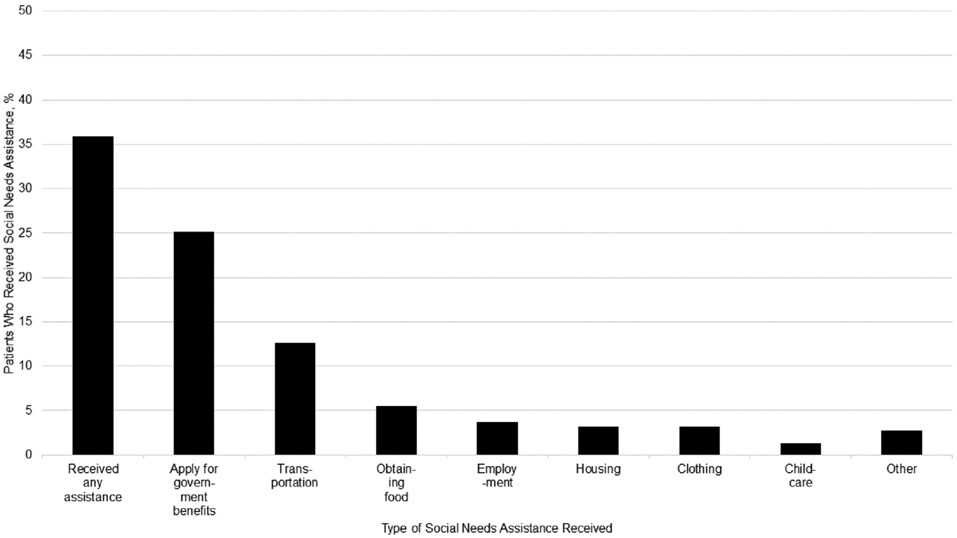
Notes: Unweighted sample consists of 2,109 patients, representing 4.5 million patients who reported receiving social needs assistance. Some patients reported assistance accessing multiple social programs or basic needs. Weighted percentages calculated using survey weights.
In Table 1, the sociodemographic, clinical, and state-level characteristics of those who received social needs assistance versus those who did not are compared. Before weighting, there were several important differences between the 2 groups: patients from racial/ethnic minority groups, with household incomes <100% of the federal poverty level, residing in urban locations, with publicly funded health insurance, experiencing homelessness, reporting fair or poor health, with mental health conditions, or residing in states that had expanded Medicaid eligibility were more likely to receive social needs assistance (standardized differences ≥0.1). After applying the IPTWs, differences were largely mitigated; however, there was some remaining imbalance by race, sexual minority status, and whether the patient resided in a rural location. Characteristics of patients who reported not needing social services are presented in Appendix Table 3, available online. Characteristics of the study sample, stratified by type of social needs assistance received (e.g., applying for government benefits, accessing basic needs) are presented in Appendix Table 4, available online.
Table 1.
Characteristics of CHC Patients by Receipt of Social Needs Assistance, 2014–2015
| Not IPTW weighted |
IPTW weighted |
|||||
|---|---|---|---|---|---|---|
| Characteristic | Received social needs assistance |
No social needs assistance received |
Standardized differences |
Received social needs assistance |
No social needs assistance received |
Standardized differences |
| Unweighted sample, n | 2,109 | 2,590 | — | 2,109 | 2,590 | — |
| Weighted population, n | 4,522,326 | 8,060,151 | — | 4,522,326 | 8,060,151 | — |
| Age, years | ||||||
| 18–34 | 37.4 | 38.6 | −0.025 | 38.9 | 38.8 | 0.004 |
| 35–44 | 21.1 | 21.8 | −0.019 | 22.5 | 21.0 | 0.035 |
| 45–54 | 24.3 | 21.6 | 0.066 | 22.3 | 21.9 | 0.009 |
| 55–64 | 17.2 | 18.0 | −0.020 | 16.3 | 18.3 | −0.054 |
| Race/ethnicity | ||||||
| White | 38.5 | 53.8 | −0.311 | 44.3 | 51.6 | −0.148 |
| Hispanic | 28.4 | 24.2 | 0.094 | 28.9 | 25.2 | 0.08 |
| Black | 24.9 | 15.9 | 0.224 | 20.9 | 16.6 | 0.111 |
| Asian | 3.1 | 1.4 | 0.114 | 1.8 | 2.2 | −0.026 |
| Other | 5.1 | 4.6 | 0.02 | 4.1 | 4.4 | −0.01 |
| Female | 67.7 | 64.7 | 0.063 | 46.7 | 47.6 | 0.054 |
| Income as % of FPL | ||||||
| ≤100% FPL | 65.0 | 55.2 | 0.203 | 61.3 | 57.8 | 0.071 |
| 101–138% FPL | 18.8 | 16.8 | 0.053 | 17.9 | 16.9 | 0.027 |
| 138–199% FPL | 9.0 | 13.0 | −0.127 | 10.2 | 11.5 | −0.040 |
| ≥200% FPL | 7.1 | 15.0 | −0.255 | 10.6 | 13.9 | −0.099 |
| Limited English proficiency | 30.7 | 25.0 | 0.127 | 29.1 | 26.6 | 0.056 |
| High school diploma or more | 61.9 | 65.6 | −0.077 | 62.8 | 63.7 | −0.020 |
| Rural residence | 36.5 | 56.1 | −0.401 | 37.6 | 53.9 | −0.331 |
| Insurance type | ||||||
| Uninsured | 31.2 | 37.3 | −0.127 | 34.6 | 35.7 | −0.02 |
| Public | 50.8 | 41.5 | 0.186 | 19.6 | 20.5 | −0.023 |
| Private | 17.3 | 20.9 | −0.092 | 45.8 | 43.8 | 0.041 |
| Other sociodemographic characteristics | ||||||
| Married | 23.8 | 28.2 | −0.102 | 24.9 | 28.3 | −0.076 |
| Non-U.S. born | 21.8 | 18.5 | 0.082 | 20.9 | 19.7 | 0.030 |
| Experiencing homelessness | 5.6 | 1.0 | 0.259 | 2.9 | 1.9 | 0.059 |
| Sexual minority (lesbian, gay, or bisexual) | 8.3 | 4.2 | 0.169 | 8.0 | 4.8 | 0.129 |
| Self-reported fair or poor health status | 46.7 | 39.3 | 0.149 | 45.3 | 40.5 | 0.098 |
| Diagnosis of medical conditions | ||||||
| Diabetes | 19.8 | 21.3 | −0.036 | 21.6 | 20.0 | 0.038 |
| Hypertension | 49.4 | 49.2 | 0.020 | 40.2 | 42.6 | −0.049 |
| Coronary heart disease | 2.1 | 2.2 | −0.006 | 1.3 | 2.2 | −0.071 |
| Chronic obstructive pulmonary disease | 8.4 | 7.3 | 0.040 | 7.4 | 7.4 | −0.002 |
| Angina | 2.2 | 2.5 | −0.019 | 2.1 | 2.4 | −0.016 |
| Stroke | 6.1 | 4.6 | 0.065 | 5.3 | 4.7 | 0.031 |
| Asthma | 17.2 | 16.2 | 0.028 | 13.6 | 16.6 | −0.083 |
| Depression | 19.0 | 14.3 | 0.126 | 17.6 | 14.8 | 0.075 |
| Generalized anxiety | 33.3 | 28.8 | 0.097 | 29.4 | 30.3 | −0.022 |
| Other mental health conditions | 27.3 | 20.3 | 0.165 | 23.4 | 21.9 | 0.036 |
| Limited activities of daily living | 26.6 | 21.4 | 0.122 | 22.8 | 23.4 | −0.015 |
| Patient type | ||||||
| Community health center | 86.0 | 92.8 | −0.223 | 90.1 | 90.0 | 0.004 |
| Public housing primary care | 1.9 | 0.9 | 0.084 | 1.7 | 1.0 | 0.055 |
| Migrant health center | 4.1 | 3.3 | 0.044 | 3.3 | 3.6 | −0.016 |
| Health care for the homeless | 8.0 | 3.0 | 0.221 | 4.9 | 5.4 | −0.021 |
| Care continuity | ||||||
| Has received care at CHC for 5 or more years | 45.8 | 34.9 | 0.222 | 38.4 | 37.1 | 0.026 |
| CHC visits in the last 12 months | ||||||
| 0 | 4.2 | 5.4 | −0.058 | 4.7 | 5.0 | −0.013 |
| 1–4 | 44.2 | 53.5 | −0.188 | 52.9 | 48.7 | 0.084 |
| 5 or more | 51.7 | 41.1 | 0.214 | 42.4 | 46.3 | −0.079 |
| Medicaid expansion state as of 2014 | 63.5 | 45.3 | 0.372 | 54.1 | 50.0 | 0.083 |
Note: Boldface indicates standardized difference greater than 0.1. Not IPTW-weighted estimates only applied survey weights. IPTW-weighted estimates use inverse probabilities from a logit propensity score model adjusting for covariates in this table. Standardized differences of means compare patients who received assistance accessing social programs or basic needs with those who did not.
CHC, community health center; FPL, federal poverty level; IPTW, inverse probability of treatment weights.
As presented in Table 2, relative to similar patients who did not receive social needs assistance, those who received social needs assistance were significantly more likely to report a CHC as their usual source of care (adjusted difference=7.2 percentage points, 95% CI=2.2, 12.1), more likely to report perceived quality of care as the “best possible” (adjusted difference=11.1 percentage points, 95% CI=5.4, 16.9), and more likely to definitely recommend the CHC to family and friends (adjusted difference=5.9 percentage points, 95% CI=1.0, 10.8). They were also significantly less likely to report the ED as their usual source of care (adjusted difference= −4.2 percentage points, 95% CI= −7.0, −1.3). There were no significant differences in having a checkup in the last year. Unweighted regression model estimates are in Appendix Table 5, available online.
Table 2.
Associations Between Receipt of CHC Social Assistance and Outcomes
| Variable | Unadjusted rates, % |
Adjusted differences | |
|---|---|---|---|
| Received social needs assistance |
Did not receive social needs assistance |
Difference (95% CI) | |
| Enrolled in social services | 72.6 | 61.3 | 4.8 (−1.2, 10.8) |
| Usual source – CHC | 84.3 | 78.6 | 7.2 (2.2, 12.1) |
| Usual source – ED | 4.4 | 6.5 | −4.2 (−7.0, −1.3) |
| Routine checkup in last year | 65.9 | 68.6 | −4.0 (−11.3, 3.3) |
| Perceived quality of care based on provider rating – best | 77.0 | 71.1 | 11.1 (5.4, 16.9) |
| Willingness to recommend | 87.5 | 84.3 | 5.9 (1.0, 10.8) |
Notes: Boldface indicates statistical significance (p<0.05). Authors defined enrolled in social programs outcome if respondent or someone in household received 1 of the following: food stamps, WIC, TANF, Section 8 Housing, or any other assistance from the government. Unadjusted rates apply survey weights only. Adjusted estimates use logistic regression; include inverse probability of treatment weights; and adjust for age, gender, race/ethnicity, household income measured as a percentage of the federal poverty level, English proficiency, health insurance type (uninsured, public, or private), highest level of education attained, urban versus rural location, marital status, being born in the U.S., experiencing homelessness, sexual minority status, self-reported fair or poor health status, diagnosis of select medical conditions (diabetes, hypertension, coronary heart disease, chronic obstructive pulmonary disease, angina, stroke, asthma, depression, generalized anxiety, or other mental health conditions [panic disorder, schizophrenia, or bipolar disorder]), patient type (e.g., general CHC patients, public housing, migrant and seasonal farm workers, or health care for the homeless), if they had visited this particular CHC for 5 years or more, number of CHC visits in the last year, and Medicaid expansion status as of 2014. Adjusted differences were calculated as mean marginal effects and are reported as absolute percentage point differences.
CHC, community health center; ED, emergency department; TANF, Temporary Assistance for Needy Families; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
DISCUSSION
To the authors’ knowledge, this is the first study to examine the association between receiving social needs assistance and access to and perceived quality of care. In a nationally representative sample of CHC patients, more than one third reported social needs assistance, which was associated with less self-reported use of ED as a usual source of care, increased use of a CHC as a usual source of care, higher perceived quality of providers, and higher satisfaction. These findings suggest that receiving social needs assistance is associated with patient trust and perceptions of quality, which may improve care continuity.
Recent evidence indicates that unmet social needs are associated with missed primary care appointments.27 Other work found that provision of enabling services at CHCs is associated with increased patient satisfaction, higher use of preventive services, and increased likelihood of having an annual checkup.21 This study builds on these findings; patients who received social needs assistance were significantly more likely to report that CHC as their usual source of care, thereby suggesting they were more likely to return to that CHC. As such, increasing the provision of comprehensive case management may assist in improving care continuity among CHC patients and potentially reduce unmet needs for primary care services. More so, given evidence that patients with unmet social needs, such as housing instability or food insecurity, have higher ED use,3,5 this study provides new evidence that receiving social needs assistance may potentially help to mitigate this.
Despite differences in patients’ self-reported usual sources of care, statistically significant differences in having a routine physical or checkup in the last 12 months based on receipt of social needs assistance were not observed, which warrants further exploration. Self-reported usual source of care reflects where a patient goes when care is needed, which may differ from actual utilization of care (e.g., having a routine checkup). Other possible explanations include potential discrepancies between self-reported usual source of care and actual usual source of care or the possibility that patients primarily sought care to address acute ailments.
Study findings also suggest that addressing the medical and social challenges that CHC patients face may impact their satisfaction with care and perceptions of care quality. Prior research suggests that patient satisfaction is largely driven by patient trust, which could be cultivated by extending patients’ relationships with the CHC beyond medical care. Moreover, satisfaction is closely associated with continuity of primary care, intentions to stay with a provider, and willingness to recommend a provider to others.28,29 As such, maximizing patient satisfaction and perceived quality may have important implications for continuity of care for CHC patients. Although some studies have suggested that there may be some reluctance from providers to screen for social needs, others suggest that screening for social needs and facilitating access to social services can improve the clinician–patient relationship.17,18,30,31 These findings support the latter hypothesis that receiving social needs assistance may build patient trust in the CHC and promote greater continuity of care.
Relative to other types of physician practices, CHCs are more likely to screen for unmet social needs.14 Many studies have examined the integration of tools (e.g., Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences [PRAPARE]; Health leads; Well Child Care, Evaluation, Community Resources, Advocacy, Referral, Education [WE CARE] survey instrument) that assess and document patients’ risks related to the social determinants of health into CHC electronic health record systems.32-36 Although this study’s findings suggest that there is an association between receiving social needs assistance and multiple outcomes, receiving assistance reflects the alignment of at least 3 events: social needs assistance was offered, the patient accepted assistance, and the patient remembered and reported these services. Although some patients may value receiving social needs assistance, there can be a discrepancy between patients screening positive for social risk factors and their interest in assistance.31,37 Several factors could prevent patients from accepting assistance, including lack of trust, fear of discrimination, perceived stigma related to receipt of government benefits or accepting help with basic needs, not perceiving that health care is the appropriate setting for social needs intervention, or receiving assistance elsewhere.37-39 Another possible interpretation of these findings is that having a consistent, high-quality, and trusted source of care may make CHC patients more likely to accept social needs assistance. More research is needed to fully understand the effects of social needs assistance on care delivery.
These results have several important implications. First, although all CHCs provide some level of assistance, CHC staffing and resource capacity may limit the extent to which they can do so. This study provides evidence to CHCs and the Health Resources and Services Administration about the value of investing in additional eligibility assistance and outreach staff. This is particularly important because, facing potential financial instability because of delayed extension of the federal Community Health Center Fund, many CHCs are considering eliminating or reducing assistance with social services. Although renewed in 2015 and 2018, these findings suggest the importance of extending (or making permanent) the Fund; without extended funding from Congress, critical services addressing the unmet health and social needs of low-income Americans may be cut.40,41
Second, other research has found that both Medicaid expansion and increased federal funding under the ACA increased capacity, expanded services provided, and improved quality of care delivered at CHCs.42-44 Many CHCs in both expansion and nonexpansion states reported increased improvements in the ability to coordinate care with social service providers (e.g., housing or Temporary Assistance for Needy Families).45,46 Given ongoing concerns around federal funding levels, any policies that decrease CHC revenue or roll back Medicaid eligibility (e.g., Supreme Court decision to repeal the ACA, Medicaid waivers that create barriers to enrollment47) may negatively affect CHC ability to connect patients to social services, which in turn may erode enrollment in social programs, and compromise access to and quality of care.
Finally, the coronavirus disease 2019 (COVID-19) pandemic has created new challenges and exacerbated financial strain on CHCs.48 Sharp declines in CHC revenue—driven by decreases in ambulatory visits and increases in COVID-19—related expenses—have led to elimination of services, support staff layoffs or furloughs, and nearly 2,000 temporary CHC site closures.49-52 As Americans face unprecedented unemployment rates, health insurance losses, food insecurity, and need for financial assistance, CHCs remain crucial in responding to COVID-19 and facilitating access to care.48,52,53 With increased demand and reduced capacity, many CHCs will likely be limited in their ability to provide social needs assistance. Although the Coronavirus Aid, Relief, and Economic Security Act provided $1.3 billion to support COVID-19 response efforts (e.g., buying testing materials) and maintaining CHC capacity, this amounts to <10% of annual CHC revenues, and there are concerns about the long-term viability of CHCs.49-52 Additional emergency funding to assist CHCs with revenue losses, payment reform (e.g., allowing Medicaid payments for nonmedical services), and stabilizing funding mechanisms for social services will be critical to facilitate CHCs’ ability to provide medical care and social needs assistance during the pandemic and to sustain their viability after.53
Limitations
First, although models adjusted for many patient-level and state-level characteristics, it was not possible to balance on unmeasured characteristics, and thus residual confounding may exist. In particular, although health status and burden of comorbid illness could influence CHC utilization or social needs assistance, the analysis was limited to the specific conditions that were collected in the HCPS. Although covariate balance for most covariates was achieved, some small differences between patients who received social needs assistance and those who did not remain after applying weights; to address this, the regression models directly adjusted for these covariates to minimize any residential confounding. Second, study data were limited to 2014–2015, although this remains the most recent HCPS and the only one following the ACA. Third, given that the survey was cross-sectional, it was not possible to estimate causality or examine temporality (e.g., how recently a patient received social needs assistance). Fourth, data are patient-reported and do not assess a patient’s perceived need for government benefits or basic needs. However, to examine the association between social needs assistance and the outcomes, patients who reported not needing any assistance were excluded. Fifth, the study may not capture the full extent of assistance provided (e.g., account for CHC patients who were already receiving services or who did not receive assistance from the CHC but were enrolled in social programs). Sixth, HCPS does not include visit-specific information (e.g., primary reason for visit), and thus the study could not contextualize characteristics of CHC visits where patients received social needs assistance. Finally, the results may not generalize outside CHCs.
CONCLUSIONS
Many providers are considering whether to provide social needs assistance to patients. Recent evidence suggests that on-site CHC provision of social services is associated with better performance on healthcare quality measures,15 and CHC patients receiving enabling services report a higher likelihood of receiving preventive services.21 This study builds on prior work, suggesting that among a nationally representative sample of nonelderly CHC patients, receipt of social needs assistance is associated with improved care continuity, higher perceived quality of care, and higher satisfaction with care.
Supplementary Material
ACKNOWLEDGMENTS
The interpretations and conclusions expressed in this article are those of the authors and do not constitute the positions or policies of the U.S. government, HHS, the Health Resources and Services Administration (HRSA), or the Department of the Veterans Affairs. We acknowledge HRSA in providing us with access to the restricted-use 2014 HRSA Health Center Patient Survey data.
Kevin H. Nguyen completed this work while supported by an Agency for Healthcare Research and Quality National Research Service Award Grant (Grant No. T32 HS000011-32) and the Robert Wood Johnson Foundation Health Policy Research Scholars program.
IRB approval was not needed. The Health Center Patient Survey is publicly available through HRSA, and a data use agreement was obtained from HRSA to use the Health Center Patient Survey with state identifiers for this study.
An earlier version of this work was presented at the AcademyHealth Virtual Annual Research Meeting on July 30, 2020.
No financial disclosures were reported by the authors of this paper.
Footnotes
SUPPLEMENTAL MATERIAL
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2020.08.030.
REFERENCES
- 1.Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129 (suppl 2):19–31. 10.1177/00333549141291S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Artiga S, Hinton E. Beyond health care: the role of social determinants in promoting health and health equity. Kaiser Family Foundation. https://www.kff.org/disparities-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/. Updated May 10, 2018. Accessed September 23, 2020. [Google Scholar]
- 3.Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21(1):71–77. 10.1111/j.1525-1497.2005.00278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cole MB, Nguyen KH. Unmet social needs among low-income adults in the United States: associations with health care access and quality. Health Serv Res. 2020;55(suppl 2):873–882. 10.1111/1475-6773.13555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berkowitz SA, Hulberg AC, Hong C, et al. Addressing basic resource needs to improve primary care quality: a community collaboration programme. BMJ Qual Saf. 2016;25(3):164–172. 10.1136/bmjqs-2015-004521. [DOI] [PubMed] [Google Scholar]
- 6.Kaiser Permanente Center for Health Research. Social needs survey–key findings. Oakland, CA: Kaiser Permanente. https://about.kaiser-permanente.org/content/dam/internet/kp/comms/import/uploads/2019/06/KP-Social-Needs-Survey-Key-Findings.pdf. Published June 2019. Accessed October 22, 2019. [Google Scholar]
- 7.Galea S, Tracy M, Hoggatt KJ, DiMaggio C, Karpati A. Estimated deaths attributable to social factors in the United States. Am J Public Health. 2011;101(8):1456–1465. 10.2105/AJPH.2010.300086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shin P, Alvarez C, Sharac J, et al. A profile of community health center patients: implications for policy. Oakland, CA: Kaiser Family Foundation. https://www.kff.org/report-section/a-profile-of-community-health-center-patients-health-status/. Published December 23, 2013. Accessed September 23, 2020. [Google Scholar]
- 9.Alvarez C, Lantz P, Sharac J, Shin P. Food insecurity, food assistance and health status in the U.S. community health center population. J Health Care Poor Underserved. 2015;26(1):82–91. 10.1353/hpu.2015.0006. [DOI] [PubMed] [Google Scholar]
- 10.Kaufman A, Powell W, Alfero C, et al. Health extension in New Mexico: an academic health center and the social determinants of disease. Ann Fam Med. 2010;8(1):73–81. 10.1370/afm.1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bruna S, Stone LC, Wilger S, Cantor J, Guzman C. The role of community health centers in assessing the social determinants of health for planning and policy: the example of frontier New Mexico. J Ambul Care Manage. 2014;37(3):258–268. 10.1097/JAC.0000000000000004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baggett TP, Berkowitz SA, Fung V, Gaeta JM. Prevalence of housing problems among community health center patients. JAMA. 2018;319(7):717–719. 10.1001/jama.2017.19869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Public Health Service Act, 42 U.S.C. § 254b. 2008.
- 14.Fraze TK, Brewster AL, Lewis VA, Beidler LB, Murray GF, Colla CH. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by U.S. physician practices and hospitals. JAMA Netw Open. 2019;2(9):e1911514. 10.1001/jamanetworkopen.2019.11514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kranz AM, Mahmud A, Agniel D, Damberg C, Timbie JW. Provision of social services and health care quality in U.S. community health centers, 2017. Am J Public Health. 2020;110(4):567–573. 10.2105/AJPH.2019.305519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Billioux A, Verlander K, Anthony S, Alley D. Standardized screening for health-related social needs in clinical settings: the accountable health communities screening tool. NAM Perspectives. May 30, 2017. 10.31478/201705b. [DOI] [Google Scholar]
- 17.Byhoff E, Cohen AJ, Hamati MC, Tatko J, Davis MM, Tipirneni R. Screening for social determinants of health in Michigan health centers. J Am Board Fam Med. 2017;30(4):418–427. 10.3122/jabfm.2017.04.170079. [DOI] [PubMed] [Google Scholar]
- 18.Tong ST, Liaw WR, Kashiri PL, et al. Clinician experiences with screening for social needs in primary care. J Am Board Fam Med. 2018;31(3):351–363. 10.3122/jabfm.2018.03.170419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Institute for Alternative Futures. Community health centers: leveraging the social determinants of health. Alexandria, VA: Institute for Alternative Futures. https://kresge.org/sites/default/files/IAF-CHCsLevera-gingSDH.pdf. Published March 2012. Accessed September 23, 2020. [Google Scholar]
- 20.Gottlieb LM, Hessler D, Long D, et al. Effects of social needs screening and in-person service navigation on child health: a randomized clinical trial. JAMA Pediatr. 2016;170(11):e162521. 10.1001/jamapediatrics.2016.2521. [DOI] [PubMed] [Google Scholar]
- 21.Yue D, Pourat N, Chen X, et al. Enabling services improve access to care, preventive services, and satisfaction among health center patients. Health Aff (Millwood). 2019;38(9):1468–1474. 10.1377/hlthaff.2018.05228. [DOI] [PubMed] [Google Scholar]
- 22.De Marchis E, Pantell M, Fichtenberg C, Gottlieb LM. Prevalence of patient-reported social risk factors and receipt of assistance in federally funded health centers. J Gen Intern Med. 2020;35(1):360–364. 10.1007/s11606-019-05393-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garrido MM, Kelley AS, Paris J, et al. Methods for constructing and assessing propensity scores. Health Serv Res. 2014;49(5):1701–1720. 10.1111/1475-6773.12182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cole MB, Trivedi AN, Wright B, Carey K. Health insurance coverage and access to care for community health center patients: evidence following the Affordable Care Act. J Gen Intern Med. 2018;33(9):1444–1446. 10.1007/s11606-018-4499-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ridgeway G, Kovalchik SA, Griffin BA, Kabeto MU. Propensity score analysis with survey weighted data. J Causal Inference. 2015;3(2):237–249. 10.1515/jci-2014-0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–3679. 10.1002/sim.6607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fiori KP, Heller CG, Rehm CD, et al. Unmet social needs and no-show visits in primary care in a U.S. northeastern urban health system, 2018–2019. Am J Public Health. 2020;110(suppl 2):S242–S250. 10.2105/AJPH.2020.305717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fan VS, Burman M, McDonell MB, Fihn SD. Continuity of care and other determinants of patient satisfaction with primary care. J Gen Intern Med. 2005;20(3):226–233. 10.1111/j.1525-1497.2005.40135.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Keating NL, Green DC, Kao AC, Gazmararian JA, Wu VY, Cleary PD. How are patients’ specific ambulatory care experiences related to trust, satisfaction, and considering changing physicians? J Gen Intern Med. 2002;17(1):29–39. 10.1046/j.1525-1497.2002.10209.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chhabra M, Sorrentino AE, Cusack M, Dichter ME, Montgomery AE, True G. Screening for housing instability: providers’ reflections on addressing a social determinant of health. J Gen Intern Med. 2019;34(7):1213–1219. 10.1007/s11606-019-04895-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hsu C, Cruz S, Placzek H, et al. Patient perspectives on addressing social needs in primary care using a screening and resource referral intervention. J Gen Intern Med. 2020;35(2):481–489. 10.1007/s11606-019-05397-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gottlieb L, Sandel M, Adler NE. Collecting and applying data on social determinants of health in health care settings. JAMA Intern Med. 2013;173(11):1017–1020. 10.1001/jamainternmed.2013.560. [DOI] [PubMed] [Google Scholar]
- 33.Gottlieb L, Tobey R, Singer J, Hessler D, Adler NE. Integrating social and medical data to improve population health: opportunities and barriers. Health Aff (Millwood). 2016;35(11):2116–2123. 10.1377/hlthaff.2016.0723. [DOI] [PubMed] [Google Scholar]
- 34.Gottlieb LM, Tirozzi KJ, Manchanda R, Burns AR, Sandel MT. Moving electronic medical records upstream: incorporating social determinants of health. Am J Prev Med. 2015;48(2):215–218. 10.1016/j.amepre.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 35.Garg A, Butz AM, Dworkin PH, Lewis RA, Thompson RE, Serwint JR. Improving the management of family psychosocial problems at low-income children’s well-child care visits: the WE CARE Project. Pediatrics. 2007;120(3):547–558. 10.1542/peds.2007-0398. [DOI] [PubMed] [Google Scholar]
- 36.Henrikson NB, Blasi PR, Dorsey CN, et al. Psychometric and pragmatic properties of social risk screening tools: a systematic review. Am J Prev Med. 2019;57(6 suppl 1):S13–S24. 10.1016/j.amepre.2019.07.012. [DOI] [PubMed] [Google Scholar]
- 37.De Marchis EH, Alderwick H, Gottlieb LM. Do patients want help addressing social risks? J Am Board Fam Med. 2020;33(2):170–175. 10.3122/jabfm.2020.02.190309. [DOI] [PubMed] [Google Scholar]
- 38.Alderwick H, Gottlieb LM. Meanings and misunderstandings: a social determinants of health lexicon for health care systems. Milbank Q. 2019;97(2):407–419. 10.1111/1468-0009.12390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gold R, Bunce A, Cowburn S, et al. Adoption of social determinants of health EHR tools by community health centers. Ann Fam Med. 2018;16(5):399–407. 10.1370/afm.2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kaiser Family Foundation. Data note: community health centers prepare for funding uncertainty. San Francisco, CA: Kaiser Family Foundation. http://files.kff.org/attachment/Data-Note-Community-Health-Centers-Prepare-for-Funding-Uncertainty. Published September 2019. Accessed September 23, 2020. [Google Scholar]
- 41.Rosenbaum S Will health centers go over the “funding cliff’? Milbank Q. 2015;93(1):32–35. 10.1111/1468-0009.12103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cole MB, Galárraga O, Wilson IB, Wright B, Trivedi AN. At federally funded health centers, Medicaid expansion was associated with improved quality of care. Health Aff (Millwood). 2017;36(1):40–48. 10.1377/hlthaff.2016.0804. [DOI] [PubMed] [Google Scholar]
- 43.Cole MB, Wright B, Wilson IB, Galárraga O, Trivedi AN. Medicaid expansion and community health centers: care quality and service use increased for rural patients. Health Aff (Millwood). 2018;37(6):900–907. 10.1377/hlthaff.2017.1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Han X, Luo Q, Ku L. Medicaid expansion and grant funding increases helped improve community health center capacity. Health Aff (Millwood). 2017;36(1):49–56. 10.1377/hlthaff.2016.0929. [DOI] [PubMed] [Google Scholar]
- 45.Paradise J, Rosenbaum S, Markus A, et al. Community health centers: recent growth and the role of the ACA. Kaiser Family Foundation. https://www.kff.org/medicaid/issue-brief/community-health-centers-recent-growth-and-the-role-of-the-aca/. Updated January 18, 2017. Accessed September 23, 2020. [Google Scholar]
- 46.Lewis C, Coleman A, Abrams MK, Doty MM. The role of Medicaid expansion in care delivery at community Health Centers. The Commonwealth Fund. https://www.commonwealthfund.org/publications/issue-briefs/2019/apr/role-medicaid-expansion-care-delivery-FQHCs. Updated April 4, 2019. Accessed September 23, 2020. [Google Scholar]
- 47.Medicaid waiver tracker: approved and pending section 1115 waivers by state. Kaiser Family Foundation. https://www.kff.org/medicaid/issue-brief/medicaid-waiver-tracker-approved-and-pending-section-1115-waivers-by-state. Updated September 1, 2020. Accessed September 23, 2020. [Google Scholar]
- 48.Johnson K, Goodnough A. Just when they’re needed most, clinics for the poor face drastic cutback. New York Times. April 4, 2020. https://www.nytimes.com/2020/04/04/us/coronavirus-community-clinics-seattle.html. Accessed September 23, 2020. [Google Scholar]
- 49.Corallo B, Tolbert J. Impact of coronavirus on community health centers. Kaiser Family Foundation. https://www.kff.org/coronavirus-covid-19/issue-brief/impact-of-coronavirus-on-community-health-centers/. Updated May 20, 2020. Accessed September 23, 2020. [Google Scholar]
- 50.Kim J-H, Desai E, Cole MB. How the rapid shift to telehealth leaves many community health centers behind during the COVID-19 pandemic. Health Affairs Blog. June 2, 2020. 10.1377/hblog20200529.449762. [DOI] [Google Scholar]
- 51.Kishore S, Hayden M. Community health centers and Covid-19—time for Congress to act. N Engl J Med. 2020;383(8):e54. 10.1056/NEJMp2020576. [DOI] [PubMed] [Google Scholar]
- 52.Wright B, Fraher E, Holder MG, Akiyama J, Toomey B. Will community health centers survive COVID-19? J Rural Health. In press. Online May 16, 2020. 10.1111/jrh.12473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Petchel S COVID-19 makes funding for health and social services integration even more crucial. Health Affairs Blog. April 14, 2020. 10.1377/hblog20200413.886531. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


