Abstract
Background
Measures exist to improve early recognition of, and response to deteriorating patients in hospital. Despite these, 7% of the deaths reported to the National Reporting and Learning System from acute hospitals in 2015 related to a failure to recognise or respond to deterioration. Interventions have been developed that allow patients and relatives to escalate patient deterioration to a critical care outreach team. However, there is not a strong evidence base for the clinical effectiveness of these interventions, or patients' ability to recognise deterioration.
Aims
The aims of this study were as follows. (a) To identify methods of involving patients in recognising deterioration in hospital, generated by health professionals. (b) To develop and evaluate an identified method of patient involvement in practice, and explore its feasibility and acceptability from the perspectives of patients.
Methods
The study used a mixed-methods design. A measure to capture patient-reported wellness during observation was developed (Patient Wellness Questionnaire) through focus group discussion with health professionals and patients, and piloted on inpatient wards.
Results
There was limited uptake where patients were asked to record ratings of their wellness using the Patient Wellness Questionnaire themselves. However, where the researcher asked patients about their wellness using the Patient Wellness Questionnaire and recorded their responses during observation, this was acceptable to most patients.
Conclusions
This study has developed a measure that can be used to routinely collect patient-reported wellness during observation in hospital and may potentially improve early detection of deterioration.
Keywords: acute care, clinical deterioration, communication, patient involvement, patient safety
Introduction
Clinical deterioration is marked by a prolonged period of clinical instability (National Confidential Enquiry into Patient Outcome and Death, 2005) and can occur at any time during a patient's illness, although patients are more vulnerable to deterioration following emergency admission to hospital, after surgery and during recovery from a critical illness (NHS Improvement, 2016). If clinical deterioration is not promptly responded to, this can result in a number of severe consequences for the patient including increased length of hospital stay, admission to the intensive care unit and increased morbidity and mortality (Johnston et al., 2015; Soar and Subbe, 2012; Stelfox et al., 2014). Measures exist to improve early recognition of, and appropriate response to, the deteriorating patient, for example the use of early warning scoring systems and the establishment of Critical Care Outreach Teams (CCOT) (Jonsson et al., 2011).
Early warning scores (EWS) are based on routine measurement of patients' physiological vital signs (Royal College of Physicians, 2012). If a patient's EWS is outside the expected range, this indicates the patient may be deteriorating and can prompt health professionals to escalate patient care by alerting a CCOT (Royal College of Physicians, 2012). CCOT typically consist of staff with critical-care skills who provide timely treatment on the ward to support the deteriorating patient (Alam et al., 2014). However, evidence for the efficacy of these systems at reducing in-hospital mortality among other serious adverse events is equivocal (Patel et al., 2011, De Meester et al., 2013). Some patients who are deteriorating continue to go unrecognised and appropriate, timely action is not always taken. Of the deaths and serious incidents reported to the National Reporting and Learning System from acute hospitals in 2015, 7% related to a failure to recognise or respond to deterioration (NHS Improvement, 2016).
Increasingly, patients are encouraged to become more active partners in their healthcare, and their involvement is promoted as a means of improving patient safety (Lawton and Armitage, 2012). Detecting clinical deterioration and escalating care is one area where patients and relatives could be involved to improve safety (Albutt et al., 2016; Gill, Leslie and Marshall. 2016). Patients and relatives may intuitively sense that a patient is deteriorating (Roland, 2015). There have been instances where relatives have recognised signs that the patient is deteriorating before health professionals. Despite raising their concerns, staff did not respond appropriately to escalate the patient's care, resulting in the unexpected death of the patient (King, 2010; Raymond et al., 2009).
These high-profile cases have led increasing numbers of healthcare organisations to invest in patient- and relative-led escalation services that invite patients and relatives to escalate clinical deterioration by activating a CCOT if they feel a patient is deteriorating, and the ward team has not responded appropriately (Chen et al., 2012). A systematic review of studies exploring the implementation and evaluation of patient- and relative-led escalation interventions revealed that it was unclear whether introducing the service reduced preventable deterioration and improved patient outcomes (Albutt et al., 2016) These interventions do not consider the extent to which patients and relatives can detect clinical deterioration, and little is known about their ability to recognise signs of the patient's deteriorating condition (Albutt et al., 2016).
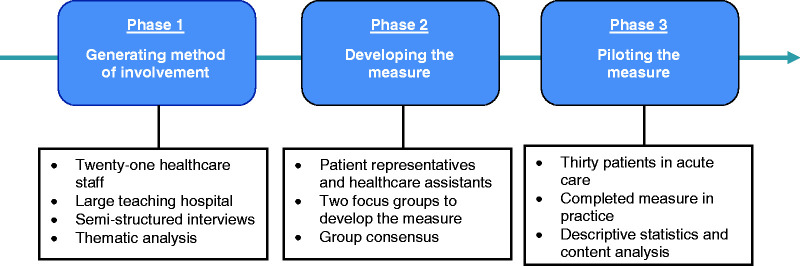
This study aimed to develop and evaluate the feasibility of an approach to involving patients and relatives in the detection of clinical deterioration in hospital. Development and evaluation of the feasibility of the approach was carried out in three phases: (1) generating methods of potential patient and relative involvement in recognising deterioration; (2) developing a measure to capture patient-reported wellness; (3) piloting the measure (see Figure 1 for a flow diagram of study phases). A mixed-methods design was used whereby qualitative methods were employed during phases 1 and 2, and quantitative methods were employed during phase 3. Using a mixed-methods approach can be useful when conducting research in an applied health setting to explore complex issues (O'Cathain et al., 2007), as was the case in the current study. The qualitative component allowed healthcare staff perspectives to be explored and content for the Patient Wellness Questionnaire (PWQ) versions to be generated. The quantitative component allowed feasibility of the PWQ and variability of patient responses to be explored. The study data were integrated using a convergent design (Fetters et al., 2013) and this is outlined in the discussion.
Figure 1.
Flow diagram of study phases.
Ethical approval for this study was granted by University of Leeds Faculty Research Ethics Committee (Reference: 15-0043) and NHS Health Research Authority North West Research Ethics Committee (Reference: 16/NW/0472). All participants provided informed consent to participate. Consent forms and research data were stored separately and securely. Only members of the research team had access to research data. All identifiers and names were removed so that transcripts and patient data (patient wellness ratings) were anonymised.
Phase 1: Generating methods of potential patient and relative involvement in recognising deterioration
Aims
This preliminary work aimed to gain healthcare staff perspectives on whether patients and relatives can provide useful information to aid staff in the management of deteriorating patients, the types of information patients and relatives could provide and how they might be involved to improve early detection of deterioration.
Method
EQUATOR guidance
Good Reporting of a Mixed Method Study (GRAMMS; O'Cathain et al., 2008) was used as EQUATOR guidance (See supplementary file A for EQUATOR checklist).
Participants and setting
The study was conducted at a large teaching hospital in the North of England. Healthcare staff caring for adult patients were eligible to participate. A purposive sampling strategy was used to recruit participants across specialities to include those working on base wards who recognise clinical deterioration and escalate patient care, and those working in Intensive Care who respond to identified patients who are deteriorating. A purposive sampling strategy allowed us to identify and select individuals who were especially knowledgeable about, and had diverse experience with, deteriorating patients (Cresswell and Plano Clark, 2011). See Table 1 for participant professions and specialities.
Table 1.
Profession and speciality of participants in phase 1.
| Profession | Speciality/current rotation |
|---|---|
| Healthcare assistant | Cardiology |
| Student nurse | Cardiology |
| Matron | Elderly medicine |
| Registrar | Elderly medicine |
| Matron | General surgery (Acute care) |
| Student nurse | General surgery (Acute care) |
| Healthcare assistant | General surgery (Urology and Vascular) |
| Consultant | Intensive Care |
| Consultant | Intensive Care |
| Anaesthetist | Intensive Care |
| Junior doctor (F2) | Intensive Care |
| Ward sister | Intensive Care |
| Staff nurse | Intensive Care |
| Critical care outreach nurse | Intensive Care |
| Registrar | Maternity |
| Midwife | Maternity |
| Consultant | Nephrology |
| Junior doctor (F1) | Nephrology |
| Junior doctor (F1) | Nephrology |
| Junior doctor (F2) | Nephrology |
| Junior doctor (F2) | Nephrology |
Procedure
Potential participants were approached and given verbal and written information about the study. A semi-structured interview schedule was developed through consultation with a multi-disciplinary expert group including experienced health-services researchers, research nurses and clinicians, namely the (Yorkshire Quality and Safety Research Group). Interviews took place in a quiet space on the ward and were audio-recorded and transcribed verbatim by the researcher. Interview length ranged from 5 to 27 minutes, with an average of 13 minutes. Data collection was complete once thematic saturation was reached when no new codes were created as a result of three additional interviews, as suggested by Bowen (2008).
Data analysis
Thematic analysis was conducted using an inductive, semantic approach in line with guidance from Braun and Clarke (2006). Meaningful units of text that addressed the research questions were identified, and text relating to similar ideas were grouped together into categories that formed provisional codes. The data set was then reviewed to confirm each code had a suitable name, definition and units of text to support it. Second coders (RL, JOH) independently coded 20% of the total number of transcripts to reduce subjectivity in the analysis and test inter-rater reliability. Discrepancies were resolved through discussion until consensus was reached. Once a definitive set of codes had been established, these were organised into provisional key themes and quotations that represented these themes were identified.
Results
Some 21 healthcare staff participated in semi-structured interviews. Four main themes were identified: (1) Knowing the patient; (2) Patients viewed as experts in themselves; (3) Relatives can be a help or hindrance; (4) Facilitators of patients and relative involvement in practice.
Theme 1: Knowing the patient
Participants talked about the importance of knowing the patient to be better able to recognise subjective changes in their wellness that may indicate deteriorating health. Undoubtedly, patients know themselves, and their close relatives may spend time with them in their day-to-day life outside of hospital, and while they are in hospital. Subsequently, patients, and to some extent relatives, have personal information about the patient and have developed knowledge about their normal health and wellbeing, enhancing their ability to identify subjective indictors of deterioration. Participants described ways in which patients and relatives could subjectively identify that the patient was becoming more unwell. These included changes in signs and symptoms, and the patients' physical appearance, capabilities and behaviour. Compared to objective indicators, taking account of patients' subjective experiences of the illness may give health professionals a more organic insight into their progress or decline:
A person is not a set of numbers. So all of your numbers may sit within the norm but it's about how you feel, you know, and those numbers are never going to tell me how you feel. Only you can do that (Matron 2).
Theme 2: Patients viewed as experts in themselves
In terms of the potential role for patients in aiding early detection of deterioration, participants felt that patients’ views on changes in their health and wellness were credible. Patients were perceived as being experts in their own bodies, with an awareness of their baseline wellness: ‘I think patients know their own bodies. They know whether they are feeling okay and this is what they are always like or whether actually they are really feeling not great’ (Registrar 1).
While what patients say about their health and wellness was viewed as valuable, participants highlighted circumstances that should be acknowledged when considering the role of patients in managing patient deterioration. The majority of participants stated that patients must have a certain level of capacity to make judgements about their wellness, and to express these to staff. Patients who are unconscious, have cognitive impairments or are disorientated cannot effectively communicate with health professionals, and thus cannot have a role in managing their deteriorating condition.
Theme 3: Relatives can be a help or hindrance
Participants discussed the extent to which relatives can make accurate judgements about changes in patient wellness. When a relative is concerned about the wellness of a family member, this can be predictive of genuine patient deterioration: ‘We see patients who have been clearly deteriorating for a number of days, and you speak to the family and they’ve been trying to raise concerns all that time, so you suspect there's a missed opportunity there’ (Consultant 1). Factors that can limit the accuracy of relatives’ judgements about patient wellness and result in relatives interfering with the work of health professionals were also considered.
Relatives may misjudge the seriousness of signs and symptoms because they lack medical training and clinical knowledge. Delirium was proposed as an example of this:
One day the patient may be completely compos mentis and be okay, they're sick, they've got a reason why they're in hospital, but that's actually on the mend and their delirium is settled one day. And the next day because of the nature of the delirium, they're completely trying to climb out of bed, they are completely confused, wandersome, at risk of falling and can't hold a conversation with their relative and so relatives obviously take that to mean they're really sick again but actually that's the nature of delirium (Registrar 2).
Some participants felt that health professionals do not respect the views of relatives as much as they should. On this topic, one participant said:
So I think the whole area of this research [greater involvement for patients and relatives in recognising deterioration] in theory is going to have an attraction but in practice it could be difficult because of staffing, and there's cultural stuff there as well. I don't feel we're as nice to relatives as we should be. We don't respect relatives as much as we should. They hold the key often in history and information and we don't seem to want to get it because we don't respect them enough (Consultant 2).
To ensure relatives are informed and feel that their concerns have been addressed, this may require extensive and continuous communication from health professionals. Respect between health professionals and relatives may be eroded as health professionals may not have the resources to communicate with patients and relatives, and ensure they feel listened to.
Theme 4: Facilitators of patients (and relative) involvement in practice
Participants stated that patients and relatives may contribute towards the management of deteriorating patients where there is gradual deterioration that may precede a serious adverse event. However, at the point of acute deterioration, the utility of patient and relative input was questioned:
It depends on the acuteness of the deterioration of the person. If it's a gradual deterioration then yeah, in the initial stages where the patient is deteriorating, I think that's fine. But then personally I think we need to, it's better that relatives have been removed from that immediate area so you can actually care for the individual, treat the individual and then bring the family back in to it to answer the questions (Ward sister 1).
Some participants proposed that patients and relatives could become more involved in managing patient deterioration if they were vigilant to signs and symptoms that indicate someone's condition is worsening. This could be achieved through educating patients and relatives about objective and subjective signs and symptoms:
I think they [patients and relatives] could be provided with information in terms of what we [health professionals] need to know, what they can do to help us help them if you catch my drift. If we provide them with ‘this is what temperature you’d normally feel like day to day, you wouldn't feel cold’ (Student nurse 2).
Nevertheless, there were mixed views on educating patients: ‘I don't think it would be appropriate for us to teach family members about NEWS charts so it would come down to their feeling that things are just not quite right’ (Consultant 2).
There was greater consensus that routinely prompting patients for their perspectives on their condition would be an acceptable method of engaging them in recognising deterioration. It was suggested that patients could be prompted during clinical observations:
I think if it became integrated in to care when you're doing physical observations, and ‘How do you feel?’ ‘Do you still … ’ ‘Do you feel well?’ Any sort of phrased question that can prompt a response in that way to explain how they're feeling in their self I think is useful (Midwife 1).
Some participants were uncertain, and had differing views about the prompts health professionals should use to elicit patients' views on changes in their wellness, particularly whether they should be prompted for information about general improvement or decline in wellness, or about changes in specific signs and symptoms.
Phase 2: Developing a measure to capture patient-reported wellness
Aims
Based on the information gathered from health professionals about engaging patients in recognising deterioration during phase 1, in phase 2 we aimed to identify suitable questions for healthcare staff to ask patients during clinical observations to prompt them for their views on changes in their wellness. We were unable to identify any previous measure that serves to capture patients' perceptions of changes in their wellness while in hospital.
Method
Participants
Two focus groups were held: one with three healthcare assistants (who predominantly conduct clinical observations), and the other with five patient representatives. Focus group durations were 54 minutes and 1 hour 4 minutes, respectively. It is recognised that three healthcare assistants are a small number of people for a focus group. It was difficult for healthcare assistants to be released from clinical duties to participate, a challenge reported elsewhere in the literature (Tausch and Menold, 2016). However, it was vital to gain healthcare assistant perspectives and establish group consensus, therefore the researchers chose to proceed with a small focus group for pragmatic reasons. Healthcare assistants and patient representatives were chosen as they represent the views of patients and people caring for them, two populations that the measure will be developed for use with.
Procedure
During the focus groups, potential question and response options that could be used to measure patient views on changes in patient wellness were presented and discussed. The potential question and response options were created based on findings from interviews in phase 1, and questions used in the self-reported health literature (Benyamini, 2003; Frankenberg and Jones, 2004; Idler and Benyamini, 1997) (see Supplementary File B for the potential question and response options). In the focus group with patient representatives, participants imagined that they were a patient in hospital and the nurse was asking them about changes in their wellness using the question options a few times a day during their stay. In this context, participants discussed what they felt each question was asking them, how difficult the question was to answer, how appropriate the question was and how willing they would be to answer it. In the focus group with healthcare staff, they discussed the same points but from the perspectives of their patients, for example, whether they thought patients would be willing to answer the question options. The focus groups were audio-recorded and transcribed verbatim.
Results
Based on discussions during the focus groups, three versions of a measure were developed to capture patient perspectives on changes in their wellness (referred to as PWQ). The questionnaire versions use different wording and response options to ask patients to give a rating of their current wellness, how their wellness has changed from an earlier time point or whether they are worried about changes in their wellness (see Table 2 for PWQ versions).
Table 2.
Patient Wellness Questionnaire versions.
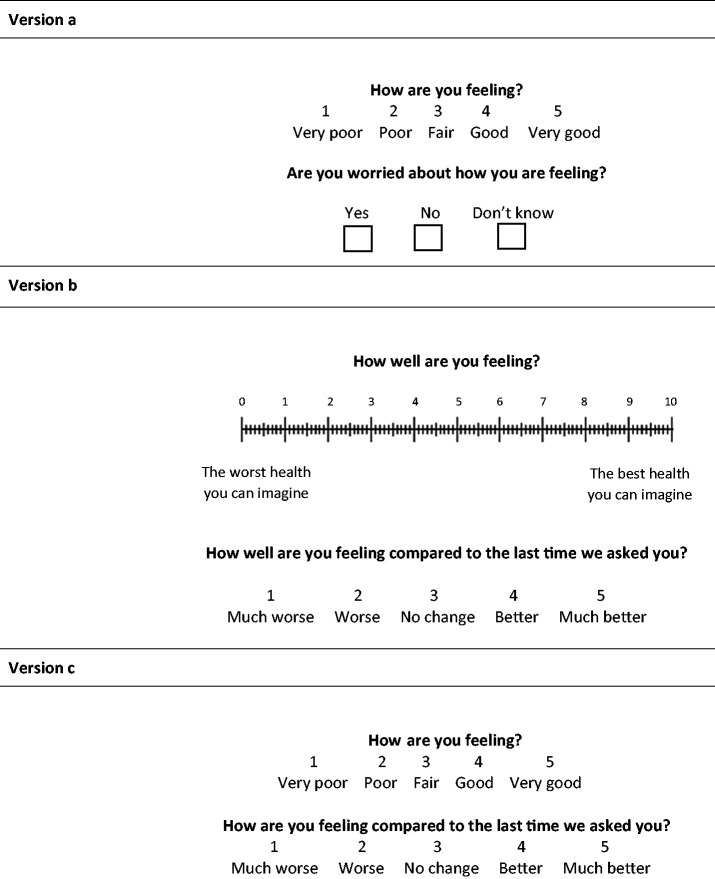
|
Phase 3: Piloting the measure
Aims
During the final phase, we piloted the PWQ versions that were developed during phase 2 with patients receiving care on in-patient wards. Versions A and C of the PWQ used a five-point scale and Version B of the questionnaire had a 10-point scale. Patients choose one option from the scale to measure their feelings about their wellness. The pilot study aimed to address the following primary research questions from the perspectives of patients:
What is the feasibility and acceptability of asking patients to rate their wellness during clinical observations, and of recording their responses?
Is there a version of the PWQ that is most appropriate to prompt patients for their views on their wellness during observation?
Appropriateness of PWQ versions was determined by patients' views of how understandable the questions were, how comfortable they were answering the questions, and the variability over time in their responses. In relation to the last point, to aid recognition of deterioration, it is important that there is variation within individual patient's ratings of their wellness where the patient is reporting a perceived improvement or decline in wellness. Therefore, we were keen to ensure the piloted measure could detect variations in wellness.
Method
Participants and setting
The pilot study was conducted on three wards at a hospital in Northern England. The wards were purposively sampled based on cardiac arrest call audit data. Number of cardiac arrest calls was used to indicate the prevalence of unrecognised patient deterioration on wards, to highlight wards that might benefit most from an intervention to improve early recognition of deterioration. Clinical deterioration preceding a cardiac arrest can be unpreventable, but it was felt that cardiac arrest call audit data was the most appropriate proxy measure for unrecognised patient deterioration (Frost et al., 2015; Green et al., 2018). Three wards with the highest numbers of cardiac arrest calls of all inpatient wards in the hospital (excluding paediatrics and cardiology) in 2014–2015 were selected. The number of cardiac arrest calls recorded on the sampled medical and surgical wards in 2014–2015 were 23 and 15, and 11. The proposed sample size was 30 patient participants in line with recommendations regarding sample sizes for pilot studies (Browne, 1995; Whitehead et al., 2016). Eligibility criteria for patient participants included the following: patients must be receiving care on one of the sampled wards, be over the age of 18 years old, have capacity to give informed consent as judged by a senior nurse, and predicted to be in hospital for at least three more days by nursing staff to ensure sufficient patient wellness ratings could be collected.
Procedure
Through discussion with the nurse in charge, patients who had capacity to give informed consent were identified and approached by a member of nursing staff. Potential participants were then approached by the researcher at their bedside at convenient times to fit around planned treatment or care. The study was introduced to potential participants and information sheets were provided. If willing to participate, the researcher collected written informed consent.
Patients participated in the study for up to seven days (based on average length of hospital stay for all causes) (NHS Confederation, 2016). If patient participants were discharged from hospital before seven days then they only participated in the study until they were discharged. In the first part of the study period, participants were given booklets containing repeated sets of patient wellness questions. Participants were asked to record their answers to one set of patient wellness questions in their booklet after each clinical observation, along with the time and date. Healthcare assistants were asked to prompt patients to complete the patient wellness questions while they carried out the clinical observation. Where patient wellness ratings were recorded by participants themselves, this method is referred to as participant recorded patient wellness ratings.
In the second part of the study period, the researcher attended daytime clinical observations, asking patients for their patient wellness ratings and recording these. Where patient wellness ratings were recorded by the researcher, this method is referred to as researcher recorded patient wellness ratings. Patient participants were then asked to give feedback about the whether the questions were easy to understand, appropriate, and suitable to answer during clinical observation. Participants were also asked in greater detail about the nature of perceived changes in their wellness (see Supplementary File C for feedback questions).
Data analysis
Data analysis was conducted using the statistical software SPSS. To analyse variability in participants' patient wellness ratings, these were first converted into Z scores. Versions A and C of the PWQ used a five-point scale and Version B of the questionnaire had a 10-point scale. As such, responses to Versions A and C were on a different normal distribution to Version B. Z scores enable us to compare scores that are from different normal distributions. Descriptive statistics, including the ranges, means (Ms) and standard deviations (SDs) of ratings were calculated. Analysis was conducted to establish variability in participant's patient wellness ratings over all study days and individual study days, and based on ward type (medical or surgical), gender, ethnicity and age. The analysis of patients' feedback responses focused on manifest content: the visible, countable content of the text, as opposed to the underlying meaning of the text (Kondracki et al., 2002). The researcher searched for occurrences of similar words or content between participants' feedback responses and counted the number of participants that gave the same response to a feedback question.
Results
Of the 59 patients approached to participate in the study, 30 were recruited, one withdrew because they felt too unwell and 29 declined participation. Participants' reasons for declining participation were: feeling too unwell (n = 9), feeling too tired (n = 5), not wanting to give informed consent (n = 2), expecting visitors (n = 1), no reason given (n = 12). On one of the sampled wards, participants were asked to record their own patient wellness ratings after clinical observations. The low number of patient wellness ratings recorded when asking participants to record their wellness ratings themselves suggested it was necessary to use a different approach to collect the data. Therefore, on the remaining two wards, the researcher attended clinical observations and recorded participants' wellness ratings. See Table 3 for characteristics of the patients recruited from the sampled wards.
Table 3.
Summary of patient characteristics.
| Ward 1 (n = 8) | Ward 2 (n = 7) | Ward 3 (n = 15) | |
|---|---|---|---|
| Patient characteristics | n | n | n |
| Age | |||
| ≥60 years old | 5 | 2 | 7 |
| ≤60 years old | 3 | 5 | 8 |
| Gender | |||
| Male | 8 | 5 | 9 |
| Female | 0 | 2 | 6 |
| Ethnicity | |||
| White British | 7 | 6 | 14 |
| Asian Bangladeshi | 1 | 0 | 0 |
| Asian Pakistani | 0 | 1 | 1 |
Characteristics of patient wellness ratings
Participant recorded patient wellness ratings
Eight participants were asked to record their answers to Version A of the PWQ after each clinical observation, and M = 0.01 (SD = 0.57, range: −0.82–0.75, Mdn = 0.1). Analysis revealed there was variation in patient wellness ratings in both age groups. There was greater variation in patient wellness ratings given by younger patients aged 60 or over (M = −0.17, SD = 0.82, range: −0.82–0.75, Mdn = −0.46) compared to patients 60 or over (M = 0.19, SD = 0.18, range: 0.05–0.40, Mdn = 0.14), and younger patients reported poorer wellness than older patients. Although this was a mixed gender ward, all participants in the sample using this method were males. Female patients approached to participate in the study declined. The mean percentage of patient wellness ratings recorded by patient participants out of the total number of opportunities was low, at 14%.
Researcher recorded patient wellness ratings
The characteristics of patient wellness ratings are discussed where the researcher attended observations to ask 22 participants Version B or Version C of the PWQ and record their wellness ratings. In terms of the questionnaire versions, there was variation in patient wellness ratings in response to Version B (M = 0.58, SD = 0.49, range: 0.01–1.36, Mdn = 0.44) and Version C (M = −0.27, SD = 0.28, range: −0.78–0.34, Mdn = −0.32) of the PWQ. Table 4 outlines the variation in patient wellness ratings on individual and all study days.
Table 4.
Variation in patient wellness ratings by study day.
| Day | M | SD | Min | Max | Mdn |
|---|---|---|---|---|---|
| All days | 0.01 | 0.54 | −0.78 | 1.36 | −0.12 |
| Day 1 | 0.11 | 0.86 | −0.87 | 2.79 | −0.13 |
| Day 2 | 0.05 | 0.55 | −0.87 | 1.3 | 0.03 |
| Day 3 | −0.15 | 0.72 | −1.73 | 0.72 | 0.03 |
There was variation in patient wellness ratings across the three questionnaire versions for age, gender and ward type. In terms of age, there was greater variation in patient wellness ratings given by older patients aged 60 or over (M = −0.01, SD = 0.51, range: −0.42–1.12, Mdn = −0.32) compared to patients 60 or younger (M = −0.09, SD = 0.43, range: −0.78–0.6, Mdn = −0.12). Patient wellness ratings reported by male participants (M = 0.09, SD = 0.6, range: −0.78–1.36, Mdn = −0.02) had greater variability than those reported by females (M = −0.14, SD = 0.39, range: −0.64–0.44, Mdn = −0.23). Participants receiving care on medical wards (M = 0.58, SD = 0.49, range: 0.01–1.36, Mdn = 0.44) reported greater variability in patient wellness ratings compared to those on surgical wards (M = −0.27, SD = 0.28, range: −0.78–0.34, Mdn = −0.32). The full range of response options on a five-point scale was used by participants to rate their wellness when they were asked versions A and C of the PWQ. Version B of the questionnaire had a 10-point scale for participants to rate how well they were feeling, and participants did not use the full range of response options to rate their wellness. Patients reported the poorest wellness in response to Version C (M = −0.27) of the questionnaire, followed by Version A (M = 0.01) and then Version B (M = 0.58). The mean percentage of patient wellness ratings recorded by the researcher out of the total number of opportunities was 95%.
Qualitative content analysis
Feedback responses were collected from 17 patient participants. Participants were asked Version A, B, or C of the PWQ during clinical observation (Version A, n = 7; Version B, n = 7; Version C, n = 16). Participants were asked to rate on a five-point scale (strongly agree to strongly disagree) their agreement with the following statements in relation to the PWQ version they were asked while participating in the study: ‘I understood what the questions were asking me’ and ‘I was comfortable answering the questions’. Table 5 details the frequencies of participants’ responses.
Table 5.
Frequency of patient participants' responses to feedback questions.
| Patient wellness questionnaire version | Feedback question | Participant response |
|||||
|---|---|---|---|---|---|---|---|
| Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | N | ||
| Version A | I understood what the questions were asking me | 4 | 1 | 0 | 0 | 0 | 5 |
| I was comfortable answering the questions | 4 | 1 | 0 | 0 | 0 | 5 | |
| Version B | I understood what the questions were asking me | 6 | 0 | 0 | 0 | 0 | 6 |
| I was comfortable answering the questions | 6 | 0 | 0 | 0 | 0 | 6 | |
| Version C | I understood what the questions were asking me | 6 | 0 | 0 | 0 | 0 | 6 |
| I was comfortable answering the questions | 6 | 0 | 0 | 0 | 0 | 6 | |
A number of patient participants elaborated on their understanding of what the patient wellness questions were asking them about. Response topics and frequencies are organised into a categorisation matrix and presented in Table 6.
Table 6.
Categorization matrix exploring the content validity of patient wellness questions.
| Feedback question | My general wellbeing | My mental health | Progress in my health | Adequacy of my treatment | n of patient respondents |
|---|---|---|---|---|---|
| What do you think the patient wellness questions are asking you about? | 6 | 3 | 4 | 2 | 15 |
Patients' feedback regarding the feasibility and acceptability of the measure are displayed as word frequency counts in Table 7.
Table 7.
Word frequency counts for patients' responses to feedback questions.
| Feedback question | Yes | No | Don't know | n of patient respondents |
|---|---|---|---|---|
| Was it acceptable be asked the patient wellness questions as frequent as every observation? | 15 | 2 | 0 | 17 |
| Will your answers to the patient wellness questions help staff recognise if you're getting more unwell? | 10 | 4 | 3 | 17 |
| During your stay in hospital, were you aware of any changes in your health or wellness? | 11 | 2 | 1 | 14 |
| Were you concerned about the changes in your health or wellness? | 5 | 5 | 1 | 11 |
The majority of patient participants felt that it was acceptable to be asked patient wellness questions as frequently as every observation. Although, one participant felt it would be more appropriate to answer the questions once at the end of each day. They talked about their ability to give accurate answers to patient wellness questions, where being in pain made it difficult to think clearly about their wellness. Patients' perspectives on the utility of the measure were largely positive. A small proportion were doubtful that health professionals would look at their ratings of their wellness because; health professionals lack time to consider what patients say about how they're feeling, recording patients' views on their wellness creates further paperwork, health professionals may not be responsive to new interventions, and health professionals are sufficiently trained to recognise deterioration without input from patients.
Discussion
This study aimed to develop and evaluate the feasibility and acceptability of a measure to record patient-reported wellness during routine observation from a patient perspective to potentially improve early detection of clinical deterioration in hospital. Asking patients to record their answers to the PWQ after each observation was not a feasible method to routinely collect data about patients' views on change in their wellness. This is reflected in the low percentage of patient wellness ratings recorded using the method. Subsequently, the researcher attended daytime patient observations for each patient participant, asking for their wellness ratings and recording these. This data collection method is not sustainable in practice, but it was first important to ensure sufficient data were collected to answer the research questions. Using this method, it was found that patients are willing and able to give information about changes in their wellness during routine observations. Inviting healthcare assistants and nurses who conduct clinical observations to ask patients about their wellness and record their responses, along with objective vital sign measures, may be a sustainable approach to routinely collecting this information from patients and warrants further investigation.
Using a mixed-methods approach provided a better understanding of the involvement of patients in recognising clinical deterioration in hospital than using either qualitative or quantitative methods alone. Qualitative analysis suggested that health professionals believe there is a role for patients in recognising clinical deterioration and routinely recording patient-reported wellness during observation may be appropriate. Quantitative analysis allowed the researchers to understand whether patients can recognise variations in their wellness that may indicate genuine deterioration, and the acceptability of using the Patient Wellness Questionnaire to capture patient-reported wellness.
Relevance to clinical practice
Encouraging ward staff to genuinely engage with patients is vital to improve detection of acute illness (Rainey et al., 2015). Routinising conversations that elicit communication about changes in patient wellness may also encourage more open dialogue between ward staff and patients. Indeed, the current study identified that routinely asking patients about changes in their wellness uncovered concerns patients had that related to communication failure with health professionals, for instance requests for pain relief that had not been acted on by staff. This finding is consistent with a systematic review of studies exploring patient and relative led escalation systems (Albutt et al., 2016). Communication failure between health professionals, patients and relatives was cited in all studies as a reason why patients and relatives activated a Critical Care Outreach Team. Often, the types of communication failure reported were unrelated to a patient's deteriorating clinical condition. Yet, escalating non-life-threatening concerns to a team with critical care skills may not be the most appropriate or cost-effective method to address these issues (Albutt et al., 2016). Prompting patients for their views on changes in their wellness during routine observation also uncovers non-life-threatening patient concerns, and encouraging ward staff to address these concerns during routine care may be a more appropriate approach.
This study found that all three versions of the PWQ were well received by patients and the ratings patients gave about their wellness in response to the three versions of the PWQ varied overtime. Finding variability in patients' ratings of their wellness adds to our limited understanding of their ability to recognise changes in their health and suggests that patients can subjectively perceive changes in their wellness overtime. It is not yet known whether patient-reported changes in wellness are associated with objective, clinical measures of patient health, such as the EWS, to signal deterioration in their condition.
Future research should seek to understand the extent to which patients can recognise genuine deterioration in their condition, and the clinical effectiveness of routinely recording patient-reported wellness. Routinely recorded patient-reported wellness has the potential to be a data stream that could be combined with EWS and laboratory tests to aid identification of deterioration. Including routinely recorded patient-reported wellness in predictive algorithms used to identify deteriorating patients will allow researchers to explore whether the algorithms are enhanced when patient-reported wellness is also considered.
Limitations
The findings reported here are based on data collected from patients receiving care on a small number of acute care wards within one hospital in the North of England. As such, the findings of these studies may not be generalisable to healthcare systems in other countries. Furthermore, it should be noted that the patient sample were predominantly British males, despite the sampled wards being mixed gender wards. Again, this may limit the generalisability of the findings to patients of different ethnicities. Nevertheless, patients were recruited from both medical and surgical wards and thus the conclusions drawn are relevant to both types of acute ward. Transforming qualitative data into quantitative data using content analysis may have resulted in loss of detail in the original data collected during phase 3 of the study. However, it was appropriate to use content analysis because the researchers aimed to gather a quantitative description of patients' feedback regarding the acceptability of being asked the PWQ during routine observation.
Patients who participated in phase 3 of the study were mostly well and shortly to be down streamed or discharged from hospital. It was not possible to recruit more unwell patients whose conditions may be more likely to deteriorate because they were not well enough to follow the process of gaining informed consent. Nursing staff often asked patients how they were feeling as part of usual care and these more unwell patients may have had the capacity to answer questions about how they are feeling during routine observation in the study but could not participate without giving informed consent. Therefore, it was not possible to include all patients in the study who may have had capacity to answer a version of the PWQ.
Conclusions
In the current study, we have developed a measure that can be used to routinely collect patient-reported wellness during observation in hospital. It will now be important to identify approaches to collecting patient wellness ratings during routine observation using the PWQ that are sustainable in practice, and to explore whether changes in patient-reported wellness are indicative of genuine patient deterioration.
Key points for policy, practice and/or research
In this study, a measure to capture patient-reported wellness during routine observation in hospital was developed to potentially contribute towards improved early detection of patient deterioration.
Inviting healthcare assistants and nurses who conduct clinical observations to ask patients about their wellness and record their responses, along with objective vital sign measures, may be a sustainable approach to routinely collecting this information from patients.
The findings provide greater understanding about the ability of patients to recognise clinical deterioration in their condition in hospital.
Supplemental Material
Supplemental material, JRN867744 Supplemental Material1 for Involving patients in recognising clinical deterioration in hospital using the Patient Wellness Questionnaire: A mixed-methods study by Abigail Albutt, Jane O'Hara, Mark Conner and Rebecca Lawton in Journal of Research in Nursing
Supplemental material, JRN867744 Supplemental Material2 for Involving patients in recognising clinical deterioration in hospital using the Patient Wellness Questionnaire: A mixed-methods study by Abigail Albutt, Jane O'Hara, Mark Conner and Rebecca Lawton in Journal of Research in Nursing
Supplemental material, JRN867744 Supplemental Material3 for Involving patients in recognising clinical deterioration in hospital using the Patient Wellness Questionnaire: A mixed-methods study by Abigail Albutt, Jane O'Hara, Mark Conner and Rebecca Lawton in Journal of Research in Nursing
Acknowledgements
We would like to thank the patients and healthcare staff who took part in the study for giving their time. The research was supported by the National Institute for Health Research (NIHR) Yorkshire and Humber Patient Safety Translational Research Centre (NIHR YH PSTRC). The views expressed in this article are those of the author(s) and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care.
Biography
Abigail Albutt graduated from the University of Manchester in 2013 with a BSc (Hons) in Psychology, and from the University of Leeds in 2014 with an MSc in Psychological Approaches to Health. She completed her PhD with the Bradford Institute for Health Research and the University of Leeds in 2018. Abi’s PhD explored the feasibility and clinical effectiveness of involving patients in recognising clinical deterioration in hospital by routinely recording patient‐reported wellness during observation. Abi currently works as a Research Fellow in the recently funded NIHR Yorkshire and Humber Patient Safety Translational Research Centre within the Patient Involvement in Patient Safety theme.
Jane O'Hara is an Associate Professor in Patient Safety and Improvement Science, and Deputy Director of the YQSR Group. She completed a PhD in Organisational and Health Psychology at the University of Nottingham. Jane's experience centres on large-scale applied research, feasibility and randomised controlled trials, and evaluation of improvement/implementation projects. Since 2014 Jane has held a joint post between the Leeds Institute of Medical Education (LIME) at the University of Leeds and the Bradford Institute of Health Research. At LIME, Jane has a role in ensuring that the teaching of patient safety and quality improvement within the medical curriculum remains up-to-date and evidence-based. Jane has received funding from the NIHR, The Health Foundation, Health Education England and the charitable sector. Jane is leading a theme in the NIHR Yorkshire and Humber Patient Safety Translational Research Centre on the involvement of patients in patient safety and quality.
Mark Conner is an applied social psychologist who joined the University of Leeds in August 1990. He became Professor of Applied Social Psychology in August 2005. Professor Conner has a BSc in Psychology from the University of Lancaster and a PhD in Psychology from the University of Birmingham.
Rebecca Lawton is Professor in Psychology of Healthcare at the University of Leeds. Since 2009 Rebecca has held a joint post at Bradford Institute for Health Research, Bradford Teaching NHS Hospitals Foundation Trust where she leads the YQSR Group. Rebecca is Director of the NIHR Yorkshire and Humber Patient Safety Translational Research Centre, funded by the NIHR. Rebecca graduated from University of Nottingham with a BA in Psychology in 1991. In 1994 Rebecca was awarded a PhD from the University of Manchester, the culmination of an ESRC (Case) studentship working with Professor James Reason and investigating the role of procedural violations in railway accidents. Rebecca stayed at Manchester, working as a Research Fellow on two research projects. In 1999 Rebecca took up a post at the University of Leeds as a lecturer and was later promoted to Senior Lecturer in Health Psychology, before her promotion to Professor in 2012. Rebecca has attracted research funding from the NIHR, ESRC, MRC, The Health Foundation, British Academy and Bupa Foundation and has published over 180 peer reviewed articles.
Contributor Information
Abigail Albutt, Research Fellow, Yorkshire Quality and Safety Research Group, Bradford Institute for Health Research, Bradford Royal Infirmary, Bradford, UK.
Jane O'Hara, Associate Professor in Patient Safety and Improvement Science, Yorkshire Quality and Safety Research Group, Bradford Institute for Health Research, Bradford Royal Infirmary, Bradford, UK; Leeds Institute for Medical Education, University of Leeds, UK.
Mark Conner, Professor of Applied Social Psychology, School of Psychology, University of Leeds, UK.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethics
Ethical approvals for this study were obtained from University of Leeds Faculty Research Ethics Committee (Reference: 15-0043) and NHS Health Research Authority North West Research Ethics Committee (Reference: 16/NW/0472).
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was conducted as part of a PhD studentship funded by University of Leeds 110 Anniversary Scholarships.
References
- Alam N, Hobbelink EL, van Tienhoven AJ, et al. (2014) The impact of the use of Early Warning Score (EWS) on patient outcomes: A systematic review. Resuscitation 85: 587–594. [DOI] [PubMed] [Google Scholar]
- Albutt A, O'Hara J, Conner M, et al. (2016) Is there a role for patients and their relatives in escalating clinical deterioration in hospital? A systematic review. Health Expect. Epub ahead of print, 26 October 2016. DOI:10.1111/hex.12496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benyamini Y. (2003) Gender differences in the self-rated health-mortality association: Is it poor self-rated health that predicts mortality or excellent self-rated health that predicts survival?. Gerontologist 43(3): 396–405. [DOI] [PubMed] [Google Scholar]
- Bowen GA. (2008) Naturalistic inquiry and the saturation concept: A research note. Qualitative Research 8(1): 137–152. [Google Scholar]
- Braun V, Clarke V. (2006) Using thematic analysis in psychology. Qualitative Research in Psychology 3(2): 77–101. [Google Scholar]
- Browne RH. (1995) On the use of a pilot sample for sample size determination. Statistics in Medicine 14: 1933–1940. [DOI] [PubMed] [Google Scholar]
- Chen JG, Kemper AR, Odetola F, et al. (2012) Prevalence, characteristics, and opinions of pediatric rapid response teams in the United States. Hospital Paediatrics 2(3): 133–140. [DOI] [PubMed] [Google Scholar]
- Cresswell JW, Plano Clark VL. (2011) Designing and Conducting Mixed Method Research, 2nd ed. Thousand Oaks, CA: SAGE. [Google Scholar]
- De Meester K, Das T, Hellemans K, et al. (2013) Impact of a standardized nurse observation protocol including MEWS after Intensive Care Unit discharge. Resuscitation 84: 184–188. [DOI] [PubMed] [Google Scholar]
- Fetters MD, Curry LA and Creswell JW (2013) Achieving Integration in Mixed Methods Designs–Principles and Practices. Health Services Research 48(6): 2134–2156. [DOI] [PMC free article] [PubMed]
- Frankenberg E, Jones NR. (2004) Self-rated health and mortality: Does the relationship extend to a low income setting?. Journal of Health and Social Behavior 45(4): 441–452. [DOI] [PubMed] [Google Scholar]
- Frost SA, Chapman A, Aneman A, et al. (2015) Hospital outcomes associated with introduction of a two-tiered response to the deteriorating patient. Critical Care Resuscitation 17(2): 77–82. [PubMed] [Google Scholar]
- Gill FJ, Leslie GD, Marshall AM. (2016) The impact of implementation of family initiated escalation of care for the deteriorating patient in hospital: A systematic review. Worldviews Evidence Based Nursing 13(4): 303–313. [DOI] [PubMed] [Google Scholar]
- Green M, Lander H, Snyder A. (2018) Comparison of the Between the Flags calling criteria to the MEWS, NEWS and the electronic Cardiac Arrest Risk Triage (eCART) score for the identification of deteriorating ward patients. Resuscitation 123: 86–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. (1997) Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior 38(1): 21–37. [PubMed] [Google Scholar]
- Johnston MJ, Arora S, King D, et al. (2015) A systematic review to identify the factors that affect failure to rescue and escalation of care in surgery. Surgery 157(4): 752–763. [DOI] [PubMed] [Google Scholar]
- Jonsson T, Jonsdottir H, Moller AD, et al. (2011) Nursing documentation prior to emergency admissions to the intensive care unit. Nursing in Critical Care 16: 164–169. [DOI] [PubMed] [Google Scholar]
- King S. (2010) Josie's Story: A mother's inspiring crusade to make medical care safer, New York, NY: Grove Press. [Google Scholar]
- Kondracki NL, Wellman NS, Amundson DR. (2002) Content analysis: Review of methods and their applications in nutrition education. Journal of Nutrition Education and Behavior 34(4): 224–230. [DOI] [PubMed] [Google Scholar]
- Lawton R and Armitage G (2012) The role of the patient in clinical safety. Available at: http://www.health.org.uk/sites/default/files/TheRoleOfThePatientInClinicalSafety.pdf (accessed 23 March 2017).
- National Confidential Enquiry into Patient Outcome and Death (2005) An Acute Problem? Available at: http://www.ncepod.org.uk/2005report/introduction.html (accessed 15 Feb 2017).
- NHS Confederation (2016) Key statistics on the NHS. Available at: http://www.nhsconfed.org/resources/key-statistics-on-the-nhs (accessed 20 April 2017).
- NHS Improvement (2016) The Adult Patient Who is Deteriorating: Sharing learning from literature, incident reports and root cause analysis investigations. Available at: https://improvement.nhs.uk/documents/176/Deterioration_in_adults_report_7july.pdf (accessed 21 Sept 2018).
- O'Cathain A, Murphy E, Nicholl J. (2007) Why, and how, mixed methods research is undertaken in health services research in England: A mixed methods study. BMC Health Services Research 7: 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Cathain A, Murphy E, Nicholl J. (2008) The quality of mixed methods studies in health services research. Journal of Health Services Research and Policy 13(2): 92–98. [DOI] [PubMed] [Google Scholar]
- Patel MS, Jones MA, Jiggins M, et al. (2011) Does the use of a track and trigger warning system reduce mortality in trauma patients?. Injury 42: 1455–1459. [DOI] [PubMed] [Google Scholar]
- Rainey H, Ehrich K, Mackintosh N, et al. (2015) The role of patients and their relatives in ‘speaking up’ about their own safety-a qualitative study of acute illness. Health Expectations 18: 392–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raymond J, Kyzer B, Copper T, et al. (2009) South Carolina patient safety legislation: The impact of the Lewis Blackman Hospital Patient Safety Act on a large teaching hospital. Journal of the South Carolina Medical Association 105(1): 12–15. [PubMed] [Google Scholar]
- Roland D. (2015) But I told you she was ill! The role of families in preventing avoidable harm in children. BMJ Quality Safety 24: 186–187. [DOI] [PubMed] [Google Scholar]
- Royal College of Physicians (2012) National Early Warning Score (NEWS). Standardising the assessment of acute-illness severity in the NHS. Available at: file:///H:/MyDocuments/Downloads/National%20Early%20Warning%20Score%20(NEWS)%20-%20Standardising%20the%20assessment%20of%20acute-illness%20severity%20in%20the%20NHS_0%20(2).pdf (accessed 1 April 2019).
- Soar J, Subbe CP. (2012) Identifying the patient at risk of deterioration, intensive care unit admission or cardiac arrest: Stop predicting, start preventing. Critical Care Medicine 40: 2243–2244. [DOI] [PubMed] [Google Scholar]
- Stelfox HT, Bagshaw SM, Gao S. (2014) Characteristics and outcomes for hospitalized patients with recurrent clinical deterioration and repeat medical emergency team activation. Critical Care Medicine 42: 1601–1609. [DOI] [PubMed] [Google Scholar]
- Tausch AP, Menold N. (2016) Methodological aspects of focus groups in health research. Global Qualitative Nursing Research 3 DOI: 10.1177/2333393616630466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead AL, Julious SA, Cooper C, et al. (2016) Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Statistical Methods in Medical Research 25(3): 1057–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, JRN867744 Supplemental Material1 for Involving patients in recognising clinical deterioration in hospital using the Patient Wellness Questionnaire: A mixed-methods study by Abigail Albutt, Jane O'Hara, Mark Conner and Rebecca Lawton in Journal of Research in Nursing
Supplemental material, JRN867744 Supplemental Material2 for Involving patients in recognising clinical deterioration in hospital using the Patient Wellness Questionnaire: A mixed-methods study by Abigail Albutt, Jane O'Hara, Mark Conner and Rebecca Lawton in Journal of Research in Nursing
Supplemental material, JRN867744 Supplemental Material3 for Involving patients in recognising clinical deterioration in hospital using the Patient Wellness Questionnaire: A mixed-methods study by Abigail Albutt, Jane O'Hara, Mark Conner and Rebecca Lawton in Journal of Research in Nursing