Abstract
Background
Isolation precautions in patients with multi-drug-resistant bacteria and other communicable infectious agents can be associated with adverse effects. Patients’ perspectives of isolation suggest that the imposed environment and procedures create barriers to their physical, social and emotional needs.
Aims
The purpose of this paper is to review the literature to uncover any reliable evidence supporting the assertion that stigma is a significant characteristic of the experience of source isolation in healthcare settings.
Methods
The methodological framework of Arksey and O’Malley was applied to this review. A total of 14 papers identified from 189 abstracts screened were included in the review.
Results
The research reviewed suggests a clear association between stigmatisation and isolation in which stigma does have a direct negative effect on patients placed in hospital isolation. None of the studies found evidence to the contrary.
Conclusions
The implications of this literature review for policy-makers and healthcare professionals suggest that when isolation or other forms of constraint are implemented and in use, patients must be provided with strengthened forms of support, including social and emotional support, and given access to healthcare of optimal quality to prevent the associated adverse effects of isolation as much as possible.
Keywords: barrier nursing, literature review, source isolation, stigma, stigmatization
Introduction
Despite huge strides in the control of Clostridium difficile and methicillin-resistant Staphylococcus aureus (MRSA), the risk of healthcare-associated infections continues to have an impact on both acute and community care settings and their reduction is embedded within national targets for National Health Service (NHS) healthcare providers. Infection control is integral to patient care and assists in reducing morbidity and mortality (Curran, 2001). Source isolation, or barrier nursing, is one way in which nursing staff can contribute to controlling the spread of transmissible infection within the hospital setting.
The utilisation of single room isolation standard precautions, in addition, where necessary, to transmission-based precautions (TBPs), is a cornerstone of hospital infection prevention control (IPC) practice and procedure, and is implemented for patients known or suspected to be infected or colonised with pathogens spread by air, droplet or contact routes (Garner, 1996). (These precautions have provided an alternative to placing any number of patients in infectious disease hospitals.) Although a seemingly simple notion, in practice source isolation is complex and a number of challenges are involved in implementing IPC precautions. Caring for isolated patients may vary depending on the structure of the organisation, available resources and the changing epidemiology of healthcare-associated infections, and involves healthcare workers – and on occasions patients and visitors – conforming to strict protocols concerning, for example, adherence to the requirements of source isolation, the correct use of personal protective equipment (PPE), performing appropriate hand hygiene and the cleaning of equipment and the environment. In addition, all of these elements must be implemented without compromising patient safety.
This paper offers a critical review of the literature regarding the association between source isolation and stigmatisation, so as to inform the improved nursing and healthcare of patients placed in hospital isolation.
Historical and policy context
The notion of ‘isolation’ in infectious diseases refers to the possibility of separating infected people (or those suspected to be infected) from the wider population, and has historically been used to control and prevent the spread of infectious diseases. During times of epidemics, isolation has been directed to many numbers of patients, which has lasted until the individual has been cured or considered non-contagious. Anthropologists trace ‘quarantine’ as far back as the Old Testament purity laws (Armstrong, 1993), and prior to the availability of effective therapy for mycobacterial disease the practice of isolating was used in forms such as leper colonies and tuberculosis sanatoriums. From the late 1870s, forms of isolation developed from isolation huts to isolation hospitals in the 1940s and through to isolation in general hospitals from the 1960s onwards. Beginning in the 1960s, isolation was employed for longer durations within hospitals, initially for the protective isolation of severely immunocompromised patients and later to prevent cross-transmission from patients with multiple drug-resistant bacterial organisms, most principally MRSA (Garner, 1996). With medical advancements, the trend has been towards isolating infection rather than isolating people. This has distanced public health from the dark side of the history of isolation and quarantine, in which the poor and immigrants were most often targeted unfairly (Edelson, 2003).
Defining isolation
As mentioned previously, isolation practices have evolved over the past century, becoming more and more focused on the known routes of transmission of infection in healthcare facilities (i.e. airborne, droplet and contact). In the UK, there has been a move away from dedicated isolation facilities towards isolation in single rooms on general wards. For infections that are spread via airborne, droplet or contact, and most importantly the latter, those organisms that are considered to be epidemiologically significant (i.e. multiple antibiotic-resistant bacteria), placing the patient in single room isolation is considered to be an important component of TBPs (Siegal et al., 2007). TBPs are used in addition to standard precautions to prevent the spread of infectious diseases and epidemiologically important organisms such as MRSA, Clostridium difficile and norovirus. These precautions encompass patient placement, the use of PPE, hand hygiene, the appropriate management of linen and waste, decontamination of equipment and the environment, as well as the prevention of occupational exposure to infectious diseases/pathogens via, for example, available immunisations. The physical barrier of a single room is further thought to act as a psychological cue or reminder to the healthcare worker to perform the correct procedures that make up the practice of isolation (Prieto and Macleod Clark, 2005). Even though there is a lack of robust evidence for the effectiveness of isolation in preventing the spread of organisms spread by the contact route (Aboelela et al., 2006), the practice is based on a sound theoretical rationale and is widely accepted.
Conceptualising stigma
At present, isolation practices and procedures follow a medical approach at the expense of the psychological and social contexts. Isolation procedures favour strict isolation and additional forms of restrictions, without understanding the social outcomes of these practices. Research suggests that the impact of such restrictions can lead to feelings of loneliness, social exclusion and stigmatisation that may impact on the quality of care and prolong patient recovery.
Erving Goffman’s Stigma: Notes on the Management of Spoiled Identity transformed both scholarly and broader public understanding of the ways in which stigma impacts on wellbeing, social relations and community cohesion. Goffman observes that ‘stigma’ is a complex phenomenon that has come to refer to an ‘attribute that is deeply discrediting’ and that reduces the bearer ‘from a whole and usual person to a tainted, discounted one’ (Goffman, 1963: 3).
In the 50 or so years since Stigma was initially published, alternative or elaborated definitions have varied considerably. Weiss and colleagues (2006: 280) describe stigma as a ‘social process, experienced or anticipated, characterised by exclusion, rejection, blame or devaluation that result from experience, perception or reasonable anticipation of an adverse social judgement about a person or a group’. Stafford and Scott (1986: 80) proposed that stigma ‘is a characteristic of persons that is contrary to a norm of a special unit’, where a ‘norm’ is defined as a ‘shared belief that a person ought to behave in a certain way at a certain time’ (Stafford and Scott, 1986: 81). Stigma is thus greatly influenced by situation and context. Crocker and colleagues (1998: 505) suggest that ‘stigmatised individuals possess (or are believed to possess) some attribute, or characteristic, that conveys a social identity that is devalued in a particular social context’. Jones et al. (1984), in an especially influential definition, draw on the observation of Goffman (1963: 4) that stigma can be viewed as a relationship between an ‘attribute and a stereotype’ to produce a definition of stigma as a ‘mark’ (attribute) that links a person to undesirable characteristics (stereotypes). For Link and Phelan (2001) stigma is defined as the co-occurrence of labelling, stereotyping, separation, status loss and discrimination in a context in which power is exercised. As such, stigmatisation involves a multiplicity of outcomes that both disadvantages the stigmatised and is a major source of stress in their lives, including loss of status, structural discrimination and consequences that appear unrelated to the stereotype.
Methods
This review drew on the five-stage methodological framework suggested by Arksey and O’Malley (2007). These five stages are identification of research questions, identification of relevant studies, study selection, charting the data, and collating, summarising and evaluating the results of the scoping review. The research questions identified are as follows:
What is the research supporting and evidencing contemporary source isolation practices and procedures in healthcare isolation settings?
What are the psychological, emotional and social impacts of being placed in source isolation in healthcare isolation settings?
To what extent is stigma experienced by patients placed in source isolation in healthcare isolation settings?
Utilising the framework of Arksey and O’Malley (2007) enabled an examination of the extent, range and nature of research activity relating to source isolation, the identification of gaps in the existing literature, and provided rigour and transparency in terms of the methods adopted, allowing replication and validity of the review findings. The credibility and reflexive nature of this framework, together with its wider recognition, were the reasons for its application. The framework used to critically appraise the quality of included studies was that of Greenhalgh (2010).
Electronic searches were undertaken on ASSIA and Medline databases for research that had collected data about some aspect of source isolation and stigma. The review was limited primarily to English-language studies in the health arena but not to any particular nation state. The search terms used were ‘isolation’, ‘source isolation’, ‘stigma’, ‘stigmatisation’, ‘health’ and ‘healthcare’. The abstracts of potentially relevant citations were examined to determine the relevance of the original research. Full texts of all relevant articles were then obtained. In addition, bibliographies and secondary references of obtained articles were examined for additional studies. Policy documentation and reports were further searched for online.
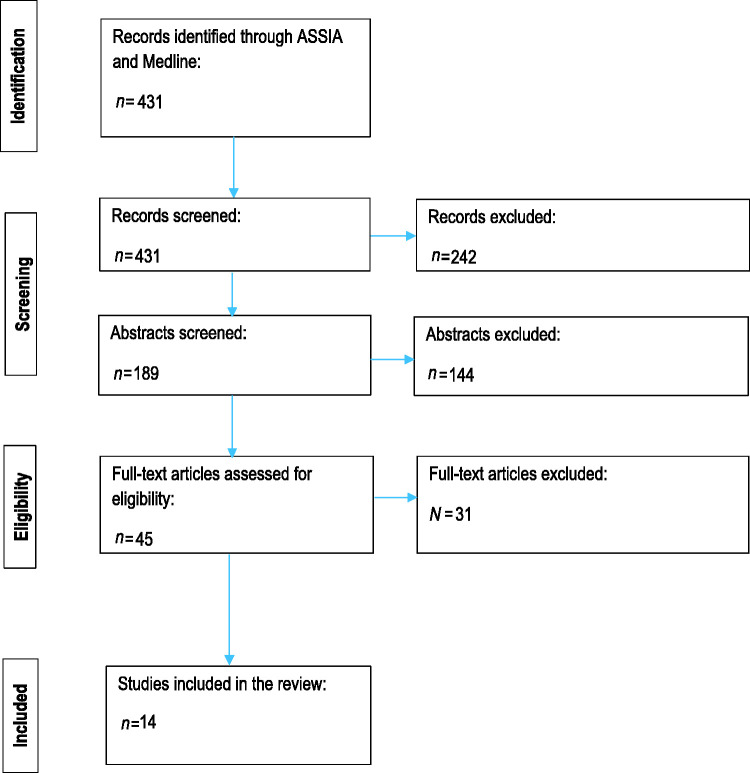
Figure 1.
Flow diagram of literature screening.
The eligibility criteria for inclusion of articles in this review were research that was original and published between 1990 and 2017 that related to aspects of source isolation and stigma. The review process is described in figure 1. Of the 431 papers identified on screening, 386 did not meet the inclusion criteria and 45 full articles were retrieved. Of these, 14 original papers were identified as addressing the identified research questions and are included in this review. The characteristics of included papers are outlined in Table 1.
Relating isolation and stigma in healthcare settings
The inevitability of isolation is to experience segregation from wider hospitalised patients and limited opportunities for socialisation. Social restrictions placed on people in isolation, including reduced contact with other patients, limited visiting, less interaction with hospital staff and disruption of routine, can lead to feelings of loneliness, abandonment, social isolation and stigmatisation (Cookson, 1997; Davies and Rees, 2000; Knowles, 1993; Lindberg et al., 2009; MacKelliag, 1987; Madeo, 2001, 2003; Mayho, 1999; Oldman, 1998; Rees et al., 2000; Rump et al., 2017; Ward, 2000). In turn, these feelings may lead to depression and induce further psychological impacts, including anxiety and rapid mood changes, that may prolong patient recovery (Davies and Rees, 2000; Gammon, 1998; Kennedy and Hamilton, 1997; Knowles, 1993; Lindberg et al., 2009; Rees et al., 2000).
Identified themes
Following the identification of the review research questions and relevant studies, the selected studies were charted, analysed and synthesised, and emerging themes were identified and discussed. From this analysis, three primary themes emerged:
isolation and social exclusion;
isolation and mental ill health;
isolation, PPE and patient satisfaction.
Theme 1: Isolation and social exclusion
Notions of social exclusion and of experiencing a lack of control emerged as main themes from the studies reviewed. In the research of Newton et al. (2001) patients did not perceive themselves as having any form of control over the course of their infection and stay in isolation, which the authors suggest was due to an absence of patients’ clear understanding of the MRSA infection and the purposes and practices of isolation and barrier nursing. Madeo (2001) sought to offer an understanding of the experience of seven MRSA-positive isolated patients in hospital. Patients’ responses are described under four main themes that emerged from the author’s data: understanding and the impact on visitors, isolation – whether viewed as a hotel or prison, treatment and stigma. While patients valued the privacy and quietness at night offered by single rooms, they missed the company and companionship of other patients during daytime hours. The 14 MRSA patients spoken with by Criddle and Potter (2006), who held negative views regarding isolation, talked in terms of feeling like a ‘leper’ when describing their emotions regarding stigmatisation. Lindberg et al. (2009) explored patient experiences and understandings of MRSA colonisation. In their research, 13 MRSA ‘sufferers’ were interviewed and expressed feelings of ‘uncertainty’, ‘distaste’ and of ‘being unclean’. Participants voiced these feelings through metaphors such as ‘having the plague’, of being a ‘plague victim’, and talked about understanding how it would feel to be HIV positive. For Lindberg and colleagues (2009), the ‘striking result’ of their study was participants’ experiences of social isolation and limitations of daily life. Rump et al. (2017: 273) relate the experiences of MRSA carriers to ‘a feeling of being left alone in the dark’.
Table 1.
Characteristics of included studies.
| Publication details | Principal study objective | Study design | Summary of findings |
|---|---|---|---|
| Andersson et al., 2010, Sweden | To ascertain and describe the patients’ knowledge, perceptions and experiences of being MRSA positive | Qualitative: Semi-structured interviews with 15 patients (8 women and 7 men) with MRSA-infected wounds | Living with MRSA can be extremely stressful for the patients. Knowledge and empathy from staff involved in their care is crucial to optimise patients’ experiences. Staff education to meet patients’ demand for information and prevent contamination is essential. |
| Barratt et al., 2010, New Zealand | To explore the lived experience of hospitalised patients in MRSA isolation in an acute care hospital in New Zealand and the meaning of those experiences for patients | Qualitative: Interpretative phenomenology utilising semi-structured interviews Participants: 10 adult patients with MRSA infection and under isolation precautions for more than 3 days | Source isolation for MRSA influences the quality of care and in particular the opportunity for emotional support. |
| Cassidy, 2006, Ireland | To illuminate issues central to general student nurses’ experiences of caring for isolated patients within the hospital environment, which may assist facilitators of learning to prepare students for caring roles | Qualitative: Hermeneutic phenomenology utilising unstructured open-ended interviews Participants: 8 students in the second year of the 3-year undergraduate programme in general nursing | The imposed physical, psychological, social and emotional barriers of isolation dramatically alter the caring experience. Balancing the care of isolated patients in order to meet their individual needs while preventing the spread of infection has significance for students. Applying infection control theory to the care of patients in source isolation is vital for students’ personal and professional development. Perceptions of supernumerary status influence students’ experiences of caring for these patients. |
| Clavelle et al., 2013, USA | To increase understanding of patient perceptions of the nursing professional image, appearance and identification to inform implementation of professional clinical attire | Quantitative: 350 randomly selected inpatients were surveyed using the professional image and patient preferences survey prior to a revision of the dress code for nursing | Organisations should assess patient perceptions before implementation of a dress code for nursing. |
| Criddle and Potter, 2006, UK | To research the phenomenon of being colonised with MRSA from the patient’s perspective | Qualitative: Phenomenological study utilising semi-structured interviews Participants: 14 patients post discharge from hospital | Providing good quality and reassuring information appropriate to the patient and their current condition is key to improving understanding. Recommendations for practice include enhanced training for healthcare workers on how to address sensitively the patient’s information needs and reduce unnecessary confusion and distress. |
| Knowles, 1993, UK | To explore the experience of source isolation from the perspectives of nurses and patients | Qualitative: In-depth interviews Participants: 8 patients and their nurses from different inpatient hospital wards | Patients feel isolated, bored, lonely, abandoned and stigmatised. Some patients value their privacy and solitude. Issues around control and communication. Nurses accurately perceived the responses of patients. |
| Lindberg et al., 2009, Sweden | To explore individuals’ experiences and understandings of methicillin-resistant Staphylococcus aureus (MRSA) colonisation | Qualitative: Open-ended semi-structured interviews. Participants: 13 people carrying MRSA (9 women and 4 men) | Participants experienced fears and limitations in everyday life and expressed a need to protect others from contagion. They experienced encounters with, and information from, healthcare workers differently: some were content, whereas others were discontented. The described fears, limitations and inadequate professional–patient relationship generated unacceptable distress for MRSA-colonised persons. |
| Madeo, 2001, UK | To understand the experience of MRSA isolation from the perspective of patients | Qualitative: Phenomenological approach utilising in-depth interviews. Participants: 7 patients (3 women and 4 men). All had MRSA for at least 2 weeks and were nursed in isolation | Issues of stigma, environment, communication and access. Healthcare staff need to be made aware of how patients feel when they are isolated with MRSA so that strategies can be implemented to make their stay in hospital as pleasant as possible. Effective communication, including information on treatment, unrestricted visiting and staff being accessible to patients and visitors, will improve the quality of care delivered and make the patient’s stay a more pleasurable one. |
| Mayho, 1999, UK | To describe the experience of being placed in source isolation | Qualitative: Autobiographical case study. Author placed in source isolation for pulmonary tuberculosis | Issues of regressive behaviour, anger, boredom, as well as loss of control and independence. |
| Mehrotra et al., 2013, USA | To determine the association between contact precautions and patient satisfaction | Prospective cohort study of inpatients, evaluated at admission and on hospital days 3, 7 and 14 (until discharge). At each point, patients underwent a standardised interview. After discharge, the standardised interview and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey were administered by telephone Participants: 528 medical or surgical patients not admitted to intensive care | Patients under contact precautions were more likely to perceive problems with their care, especially poor coordination of care and lack of respect for patient preferences. |
| Newton et al., 2001, UK | To document the perceptions of patients infected with MRSA together with their experience of source isolation | Qualitative: Semi-structured interviews: 19 participants who had been infected with MRSA and placed in source isolation | Patients infected with MRSA appear to understand little regarding their condition or the necessity for barrier nursing and source isolation. |
| Rump et al., 2017, the Netherlands | To identify and quantify the occurrence of MRSA-associated stigma, and to explore its association with mental health in a country with an MRSA ‘search and destroy’ policy | Quantitative: Questionnaire among 57 Dutch MRSA carriers (people who carry MRSA without signs of MRSA infection) at two hospitals and two regional health services in the Netherlands. Stigma was measured with an adjusted version of the Berger HIV Stigma Scale. Mental health was measured with the 5-item RAND Mental Health Inquiry | A significant proportion of MRSA carriers reported stigma due to MRSA. Stigma was associated with poor mental health. |
| Sadala, 1999, Brazil | To understand the meanings given to the caring of patients’ isolation wards by nursing students, focusing particularly on aspects of communication and interpersonal relationships | Qualitative: Phenomenological approach utilising interviews Participants: 18 third-year students from two different schools of nursing at public universities of São Paulo, Brazil. The students were performing nursing practice on isolation wards | Students describe difficulties and anxieties, as well as their willingness to take care of isolated patients, resulting in the overcoming of obstacles and in contacting and becoming involved when taking care of patients. |
| Ward, 2000, UK | To identify the ways in which healthcare professionals can prevent or reduce the negative emotional effects experienced by patients placed in hospital isolation | Mixed methods: 21 patients being nursed in isolation completed questionnaires. Qualitative interviews with 5 patients with negative experiences of isolation | Recommendations made from research include the provision of written and individualised information, improved communication from medical staff, provision of a common room and better facilities to relieve patient boredom. |
MRSA: methicillin-resistant Staphylococcus aureus.
Cassidy (2006) explored the meaning of isolation for second-year student nurses attached to caring for infectious patients in source isolation within the hospital setting. Student nurses demonstrated considerable empathy and understanding of the physical, social and psychological effects of source isolation. Participants commented that patients in isolation must feel ‘socially isolated’ and may even feel like ‘aliens’. The work of Cassidy (2006) and Criddle and Potter (2006) is consistent with research by Andersson et al. (2010), Barratt et al. (2010) and Newton et al. (2001), and is coherent with Madeo (2001), who identified social isolation and stigma as significant experiences of MRSA patients. In Madeo's study, patients associated having MRSA with being unclean; the isolation diagnosis sign on their room door symbolised their uncleanliness, thus reaffirming their sense of stigma.
Criddle and Potter (2006) talk of the commencement of isolation as being a significant event for patients in terms of exclusion, particularly when patients are moved with little or no notice or explanation. This estrangement from others is further complicated by fear of being a ‘risk to others’ in terms of passing on the infection, whether this be actual or perceived. A number of studies in this literature review highlight patients’ expressed fear of bacteria and colonisation-induced psychological strain, including anxiety, with regard to behaving correctly and ‘protecting others’ from the contagion (Andersson et al., 2010; Criddle and Potter, 2006; Lindberg et al., 2009; Ward, 2000). In the study by Lindberg et al. (2009) participants feared reactions from others in terms of disassociation, and spoke of feelings of guilt and shame in relation to partners and for having infected family members. Participants who were parents felt further guilt if their child contracted MRSA, even though the direction of contagion remained unconfirmed. In similar ways, participants in the study by Andersson et al. (2010) expressed feelings of being a threat to their environment, in part due to their ‘dirtiness’, and described the fear of infecting someone else as being traumatic and causing anxiety. The notion of isolation as a means of protecting others may further result in less contact with hospital staff and visitors, thus further intensifying feelings and emotions of social isolation for the patient (Ward, 2000).
Theme 2: Isolation and mental ill health
In a recent study, Rump et al. (2017) sought to identify the occurrence of MRSA-associated stigma and to explore its association with mental health. Their research involved a cross-sectional questionnaire that was administered to 57 MRSA carriers (people who carry MRSA without MRSA infection) at two hospitals in two regional health services in the Netherlands; a country which, according to the authors, employs an MRSA policy of ‘search and destroy’. The research by Rump et al. (2016) found signs of poor mental health among 33% of MRSA carriers. Their study suggests that a substantial proportion of MRSA carriers experience signs of stigma: 32% of MRSA carriers reported stigma; of these, 14% reported ‘clear stigma’ and 42% reported ‘suggestive for stigma’. Rump and colleagues (2016) noted that while isolation of MRSA patients may be proportionate to the overall aim of reducing risk, at the same time it is perceived as stigmatising by the affected person. In their study exploring the ‘lived experience’ of patients in MRSA isolation in an acute care hospital in New Zealand, Barratt and colleagues (2010: 55) argued that stigmatisation is a distinguishing characterisation involved in the identity of ‘(B)eing MRSA positive’. Stigmatisation for MRSA carriers further involves stigmatising situations in interactions with hospital staff, which are reflective of barriers at institutional levels (Rump et al., 2017).
Theme 3: Isolation, PPE and patient satisfaction
Perceptions of social isolation and stigma associated with isolation may be aggravated by inconsistent implementation practices and the use of PPE when treating the patient, which can add an additional barrier to effective communication. Difficulty and dissatisfaction over being unable to distinguish a nurse from other forms of healthcare workers is well documented (Clavelle et al., 2013; Mehrotra et al., 2013), and while patients appear to understand the importance of PPE, the reasons behind maintaining isolation practices and the significance of controlling the spread of infection, the literature suggests that the use of PPE increases fear and stigmatises the patient. Participants in the study of Barratt et al. (2010) spoke of being left feeling ‘infectious’ or ‘contagious’ due to the use of gowns and gloves worn by the hospital staff caring for them. Madeo (2001) describes patients feeling ‘unclean’ or ‘dirty’ when touched by staff wearing aprons. Mayho (1999) described how the use of masks in isolation prevented him from seeing the facial features of hospital staff and thus he never saw a smile throughout his inpatient stay. This is supported by Knowles (1993), who stated there is dissatisfaction among isolated patients regarding masks as it prevents facial expressions being seen. Moreover, concerns regarding personal risks of acquiring infection sometimes create obstacles between nursing staff and patients, and between student nurses and patients (Cassidy, 2006). Sadala (1999) described the ways in which symbols and objects of isolation such as PPE acquire meanings that represent keeping a distance and thereby reducing anxiety for nursing staff. A number of studies included in this literature review highlight inconsistencies in the use of PPE by staff, which patients claim to find troubling, confusing and stigmatising, and to be a physical barrier to contact time, effective communication and even quality of care in that it provides an additional process that needs to be performed prior to entering patients’ rooms, thus increasing the anxiety and stresses of isolation (Barratt et al., 2010; Criddle and Potter, 2006; Knowles, 1993; Newton et al., 2001).
Discussion
Isolation has long been employed to control the spread of infectious diseases. Nursing patients in isolation is influenced by the setting in which such nursing care is provided. Caring experiences and patient–healthcare staff relationships are dramatically altered by the uniqueness of imposed physical, social and emotional barriers. The purpose of this paper has been to discuss and analyse the state of knowledge related to the experience of stigma and stigmatisation within source isolation in healthcare settings. In doing so, isolation has been positioned within its historical context.
Stigma is a powerful phenomenon with far-ranging effects on its targets, and is hugely shaped by situation and context in that it resides not in the person but in a social context. Stigma, signalling relations of shame, contributes to the hidden burden of illness for patients in hospital isolation settings and influences the effectiveness of case finding and treatment, which are major interests of IPC. A number of studies reviewed exemplify the ways in which stigma thwarts, undermines or exacerbates a number of processes, is closely associated with depression, and may induce further psychological impacts including anxiety, stress, fear, distrust in others and rapid mood changes, leading to adverse health outcomes for isolated patients. The stigmatisation of isolation involves exclusion, labelling, negative stereotyping and loss of status for the isolated patient. Each of these stigma-induced processes mediates the relationship between stigma and the prolonging of recovery for the patient placed in hospital isolation. While each of these terms is often referred to loosely and is used interchangeably within the literature reviewed, this paper argues that stigma is a broader and more inclusive concept than any one of these individual processes.
This literature review suggests that the experience of isolation can involve the construction of a social identity that is devalued (Crocker et al., 1998), in that the isolated patient possesses (or is believed to possess) an attribute that marks them as being different from hospital patients more widely. The studies of Barratt et al. (2010), Cassidy (2006), Criddle and Potter (2006), Lindberg et al. (2009) and Madeo (2001) are particularly powerful in this, with patients either feeling or being referred to as lepers or aliens, of having the plague, and of being unclean or dirty. In stigmatisation, these ‘marks’ may be visible or invisible and become associated with ‘discrediting dispositions’ – negative evaluations and stereotypes (Jones et al., 1984). These stereotypes and evaluations are widely shared and well known among members of a culture (Crocker et al., 1998), and become the basis for excluding or avoiding members of the stereotyped category. This literature review has shown the ways in which – for patients placed in isolation – it is not only their separation from wider hospital patients that marks and signifies their difference, but that the visible symbols and objects of isolation intensify their social exclusion and loss of status and exercise a devaluation in their social identity in the eyes of others.
A number of papers in this review utilised qualitative methodologies to investigate the impact of isolation on patients and included only small numbers of research participants. Thus, generalisation is limited by the specific populations studied, without a theoretical perspective. While this perhaps is not too surprising, isolation enquiry related to stigma would benefit from employing mixed research methodologies and greater attention to research design details. Deeper understanding regarding the meaning and impact of stigma could be strengthened by a mixed-methods approach that develops a redefining of health-related stigma. Developing understandings drawing on theoretical perspectives is particularly important in relation to stigma, especially when health professionals have substantial interests in recognising and diminishing the impact of stigma as both a feature and a cause of any number of health problems. Goffman's (1963) conceptualisation of stigma has guided a wide range of social science research studies, and his work has been pivotal in the development of practical initiatives designed to combat the impact of social stigma. Such initiatives include programmes designed to reduce the social stigma of conditions such as HIV and AIDS and in the area of mental health and disability, as well as sexual orientation and gender identity. Further research that investigates potential utilisations of stigma and stigmatisation theories relating to patient isolation, nursing practice and patient care in healthcare isolation settings is thus much warranted. In so doing, it is critical that such research rethinks the notion so that it may better guide public health research, policy and practice.
Implications for nursing and nursing practices
This review of the literature draws attention to the complexities involved in nursing patients in source isolation and suggests a clear need for isolation practices and procedures to consider the psychological, emotional and social impacts of being placed in source isolation in healthcare isolation settings. Stigma is considerable in the patient experience of being placed in source isolation. This has been known for a number of years and has never been fully addressed. Nursing staff and other healthcare workers need enhanced training in becoming aware of this, and in looking for ways to improve the experience of isolation and contact precautions of patients placed in source isolation. Nursing staff need to better prepare patients for source isolation in providing timely adequate information and in offering support for improving the patient’s self-control of the situation. This is especially true for those patients expected to experience long periods of isolation, thus making them more vulnerable to the negative effects and stigmatisation of isolation. Nursing staff should encourage social interaction, frequent contact between staff and patients, and visiting to reduce feelings of social exclusion for patients placed in isolation in healthcare settings. Ensuring patients do not feel they receive less direct nursing care and medical attention is important in challenging the stigmatising experience of source isolation. This has implications for understanding the adherence of patients to IPC procedures.
Limitations
This literature review offers an insight and critique of the field of knowledge in nursing related to source isolation, stigma and stigmatisation. The review is limited by the phrases used for searching, the databases accessed, the frame and method of searching for literature, and time constraints. Searching additional databases or using additional search phrases may have identified more publications. The criteria that the article be written or available in the English language may further have led to omissions of studies published in other languages, particularly as the studies that were screened and included were international.
Conclusions
Stigma is becoming a priority interest of public health. This comprehensive review of the literature was conducted to examine the state of current knowledge regarding stigma and stigmatisation in healthcare isolation settings. This paper reveals stigma to be significant in the experience of source isolation for hospital patients. Published reflection and primary research regarding stigma and hospital isolation is emerging, albeit slowly and the evidence is not extensive. Much of this literature explores stigma as a glimpse of a wider picture of adverse outcomes relating to isolation, thus its full power and significance remain somewhat obscured and subsequently little progress has been made. To our knowledge, this is the first paper to examine most specifically the relationship between stigma, stigmatisation and source isolation.
This literature review highlights the complexities involved in nursing patients in source isolation in healthcare settings. Present guidelines for isolating patients with infectious diseases appear to be influenced heavily by historical, clinical experiences. Isolation or other forms of constraints have a serious impact on a patient’s health, welfare and liberty. Stigma exerts a pervasive impact on the health and wellbeing of people placed in hospital isolation. Simply knowing that patients in isolation experience stigma and a loss of control, which impacts adversely on the suffering and hidden burden of illness, is not enough on its own. There is a further need to uncover the ways in which they are linked and why there is such a relationship, and to identify ways of ensuring that, for patients in isolation, stresses, uncertainties and the stigma of the isolation experience are not intensified by nursing interventions but are reduced to promote effective coping strategies for patients. The implications of this literature review for policy-makers and healthcare professionals suggest that when isolation or other forms of constraint are implemented and in use, patients must be provided with strengthened forms of support, including social and emotional support, and given access to healthcare of optimal quality to prevent adverse effects of the restrictions as much as possible. Implications for researchers are indisputably evident: stigma is considerable in the patient experience of being placed in source isolation – more high quality studies are needed to address this.
Key points for policy, practice and/or research
Stigma is becoming a priority interest of public health.
Stigma exerts a pervasive impact on the health and wellbeing of patients placed in source isolation in hospital settings.
There is a need to uncover the ways in which the experience of stigma and source isolation are linked, in order to identify ways of ensuring that the stresses, uncertainties and stigma of the isolation experience are not intensified by nursing interventions, but are reduced to promote effective coping strategies for patients.
It is necessary for policy-makers and healthcare professionals to acknowledge that when source isolation or other forms of constraint are implemented and in use, patients must be provided with strengthened forms of support, including social and emotional support, and given access to healthcare of optimal quality to prevent adverse effects of the restrictions as much as possible.
Biography
John Gammon is currently the Deputy Head of the College of Human and Health Sciences at Swansea University. He has significant experience in higher education, with subject expertise in infection prevention and control, healthcare management and research. His research interests include infection control practice, isolation strategies and behavioural compliance within a clinical context.
Julian Hunt is a Research Officer at Swansea University. He is a Sociologist with particular interest in ethnographic and participatory research methods. He has previously worked on a number of health and mental health studies, including the Welsh Assembly Government’s Sustainable Health Action Research Programme (SHARP) – an action research initiative that focused on health inequalities and community health development. He has combined this with a keen interest in historical sociology and the impact of class and place upon social, cultural and economic life.
Charles Musselwhite is Associate Professor in Gerontology at the Centre for Innovative Ageing (CIA), Swansea University and heads up the group’s environments and ageing research strand. He is operational director of the Centre for Ageing and Dementia Research (CADR), an initiative to develop and enhance research, policy and practice for older people across Wales. He completed his PhD at the Transportation Research Group, University of Southampton in 2004 and has worked at Bournemouth University (2003–2006), then the University of the West of England in the pioneering Centre for Transport and Society (2006–2013). His research has involved several invited international and national presentations at conferences and invited presentations to the House of Commons and House of Lords. He makes frequent appearances on radio and television across the world and is keen to engage his research with the public.
Contributor Information
John Gammon, Deputy Head of College, Innovation, Engagement and Organisational Development, Swansea University, UK.
Julian Hunt, Research Officer, College of Human and Health Sciences, Swansea University, UK.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethics
Ethical approval was not needed to undertake this literature review.
Funding
The author(s) received no financial support for the research, authorship and/or publication of this article.
References
- Aboelela SW, et al. (2006) Effectiveness of barrier precautions and surveillance cultures to control transmission of multidrug-resistant organisms: A systematic review of the literature. American Journal of Infection Control 30(7): 40–43. [DOI] [PubMed] [Google Scholar]
- Andersson H, Lindholm C, Fossum B. (2010) MRSA – Global threat and personal disaster: Patients’ experiences. International Nursing Review 58(1): 47–53. [DOI] [PubMed] [Google Scholar]
- Arksey H, O’Malley L. (2007) Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology 8(1): 19–32. [Google Scholar]
- Armstrong D. (1993) Public health, spaces and the fabrication of identity. Sociology 27(3): 393–410. [Google Scholar]
- Barratt R, Shaban R, Moyle W. (2010) Behind barriers: Patients’ perceptions of source isolation for methicillin-resistant Staphylococcus aureus (MRSA). Australian Journal of Advanced Nursing 28(2): 53–59. [Google Scholar]
- Cassidy I. (2006) Student nurses' experiences if caring for infectious patients in source isolation. A hermeneutic phenomenological study. Journal of Clinical Nursing 15(10): 1247–1256. [DOI] [PubMed] [Google Scholar]
- Clavelle J, Goodwin M, Tivis L. (2013) Nursing professional attire: Probing patient preferences to uniform implementation. Journal of Nursing Administration 43(3): 172–177. [DOI] [PubMed] [Google Scholar]
- Cookson B. (1997) How to resist. Health Service Journal 30: 9–11. [PubMed] [Google Scholar]
- Criddle P, Potter J. (2006) Exploring patients’ views on colonization with of Methicillin-resistant Staphylococcus aureus. British Journal of Infection Control 7(2): 24–28. [Google Scholar]
- Crocker J, Major B, Steele C. (1998) Social stigma. In: Gilbert DT, Fiske ST. (eds) The Handbook of Social Psychology, Boston, MA: McGraw-Hill. [Google Scholar]
- Curran E. (2001) Reducing the risk of healthcare acquired infection. Nursing Standard 16(1): 45–52. [DOI] [PubMed] [Google Scholar]
- Davies H, Rees J. (2000) Psychological effects of isolation nursing. (1): Mood disturbance. Nursing Standard 14(28): 35–38. [DOI] [PubMed] [Google Scholar]
- Edelson PJ. (2003) Quarantine and social equity. The Journal of the American Medical Association 290(21): 2874. [DOI] [PubMed] [Google Scholar]
- Gammon J. (1998) Analysis of the stressful effects of hospitalisation and source isolation on coping and psychological constructs. International Journal of Nursing Practice 4(2): 84–96. [DOI] [PubMed] [Google Scholar]
- Garner JS. (1996) Guideline for isolation precautions in hospitals. American Journal of Infection Control 24(1): 24–52. [DOI] [PubMed] [Google Scholar]
- Goffman E. (1963) Stigma: Notes on the Management of Spoiled Identity, Englewood Cliffs, NJ: Prentice Hall. [Google Scholar]
- Greenhalgh T. (2010) How to Read a Paper: The Basics of Evidence-based Medicine, 4th edn. Oxford: Wiley-Blackwell. [Google Scholar]
- Jones E, et al. (1984) Social Stigma: The Psychology of Marked Relationships, New York: Freeman. [Google Scholar]
- Kennedy P, Hamilton LR. (1997) Psychological impact of the management of methicillin-resistant Staphylococcus aureus (MRSA) in patients with spinal cord injury. Spinal Cord 35(9): 617–619. [DOI] [PubMed] [Google Scholar]
- Knowles H. (1993) The experience of infectious patients in isolation. Nursing Times 89(30): 53–56. [PubMed] [Google Scholar]
- Lindberg M, et al. (2009) Suffering from methicillin-resistant Staphylococcus aureus: Experiences and understandings of colonization. Journal of Hospital Infection 73: 271–277. [DOI] [PubMed] [Google Scholar]
- Link BG, Phelan JC. (2001) Conceptualizing stigma. Annual Review of Sociology 27(6): 363–385. [Google Scholar]
- MacKellaig JM. (1987) A study of the psychological effects of intensive care with particular emphasis on patients in isolation. Intensive Care Nursing 2(4): 176–185. [DOI] [PubMed] [Google Scholar]
- Madeo M. (2001) Understanding the MRSA experience. Nursing Times 97(30): 36–37. [PubMed] [Google Scholar]
- Madeo M. (2003) The psychological impact of isolation. Nursing Times 99(7): 7. [PubMed] [Google Scholar]
- Mayho P. (1999) Barrier grief. Nursing Times 95(31): 24–25. [PubMed] [Google Scholar]
- Mehrotra P, et al. (2013) Effects of contact precautions on patient perception of care and satisfaction: A prospective cohort study. Infection Control and Hospital Epidemiology 34(10): 1087–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton JT, Constable D, Senior V. (2001) Patients' perceptions of methicillin-resistant Staphylococcus aureus and source isolation: A qualitative analysis of source-isolated patients. Journal of Hospital Infection 48(4): 275–280. [DOI] [PubMed] [Google Scholar]
- Oldman T. (1998) Isolated cases. Nursing Times 94(11): 67–70. [PubMed] [Google Scholar]
- Prieto J, Macleod Clark J. (2005) Contact precautions for Clostridium difficile and methicillin-resistant Staphylococcus aureus: Assessing the impact of a supportive intervention to improve practice. Journal of Research in Nursing 10(5): 511–526. [Google Scholar]
- Rees J, Davies H, Birchall C. (2000) Psychological effects of source isolation. (2): Patient satisfaction. Nursing Standard 14(29): 32–36. [DOI] [PubMed] [Google Scholar]
- Rump B, et al. (2017) Signs of stigma and poor mental health among carriers of MRSA. Journal of Hospital Infection 95(3): 268–274. [DOI] [PubMed] [Google Scholar]
- Sadala M. (1999) Taking care as a relationship: A phenomenological view. Journal of Advanced Nursing 30(4): 808–817. [DOI] [PubMed] [Google Scholar]
- Siegal J, et al. (2007) Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings (2007). Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/hicpac/pdf/isolation/isolation2007.pdf (accessed 8 April 2019).
- Stafford MC, Scott RR. (1986) Stigma, deviance and social control. In: Ainlay SC, Becker G, Coleman LM. (eds) The Dilemma of Difference, New York: Plenum. [Google Scholar]
- Ward D. (2000) Infection control: Reducing the psychological effects of isolation. British Journal of Nursing 9(3): 162–170. [DOI] [PubMed] [Google Scholar]
- Weiss MG, Ramakrishna J, Somma D. (2006) Health-related stigma: Rethinking concepts and interventions. Psychology, Health and Medicine 11(3): 277–287. [DOI] [PubMed] [Google Scholar]