Abstract
Background
Many reasons for missed appointments are given by people who inject drugs and it is suggested that one solution cannot solve this complex issue (Poll et al., 2017). Increasingly, nurses and other health professionals are expected to actively involve patients and service users in developing innovative, effective and accessible services. This project used co-production as the approach to address this challenge.
Aims
This paper describes how a co-production method was used to develop accessible nurse-led hepatitis C virus services for people who inject drugs.
Methods
Using research evidence from a study conducted by the lead author as a starting point, a series of co-production workshops were run using creative co-design methods to identify the barriers to engagement with clinics. Potential solutions were then co-produced.
Results
The solutions included myth-busting posters, peer-support, a mobile clinic van and the offer of incentives and enablers (travel costs or a reward for attendance).
Conclusions
The service-development project illustrates how, with the right methods, it is possible to successfully engage with hard-to-access groups to co-produce innovative solutions for an important clinical challenge.
Keywords: case study, co-production, evidence-based practice, innovation and improvement, knowledge mobilisation, service-development, substance use and misuse
Introduction
In the recent document, Leading Change, Adding Value: A framework for nursing, midwifery and care staff (NHS England, 2016), commitment five states that nurses should be at the forefront of ‘facilitating the involvement of individuals and their carers in co-designing and providing care services’ (p. 32). This sits alongside the Nursing and Midwifery Council (NMC) code (section 2.1). This requires nurses and midwives to ‘work in partnership with people to make sure you deliver care effectively’ (p. 4) (NMC, 2015). These obligations are clearly worthwhile, but the documents do not elaborate on how to achieve them or how to overcome the considerable challenges in doing so. This paper presents a service-development case study to show a successful approach in achieving partnership working with a group that is traditionally seen as hard to access.
Background
Hepatitis C
The starting point for this project was research evidence from a doctoral study being translated into interventions to improve attendance at nurse-led hepatitis C virus (HCV) outreach clinics sited in drug treatment services. Nurses play a critical role in the management of hepatitis C, including screening people at risk of infection; giving a diagnosis; undertaking an initial patient assessment including arranging blood tests and scans; and supporting patients on treatment. This work is undertaken in a variety of settings, including drug misuse services and prisons.
HCV is a blood-borne virus that infects liver cells. Thus, if patients with HCV do not engage with clinics and receive curative treatment, they are at risk of developing advanced liver disease (cirrhosis), hepatocellular carcinoma and death (Pawlotsky et al., 2018). In England, approximately 160,000 people are chronically infected with HCV, with approximately half of this figure remaining undiagnosed (Costella, 2018). Those at greatest risk of infection are people who inject drugs (PWIDs) who have shared drug-injecting paraphernalia such as needles, syringes, spoons and filters (contaminated with HCV) with others. Some people may have only injected drugs such as heroin, amphetamines and crack cocaine on a couple of occasions while experimenting in their younger years. Other people may have injected these drugs for many years and be known to drug services. The latter group of PWIDs are largely male; aged between 30 and 60 years; in receipt of state benefits; experience other co-morbidity including depression, lung disease and poor venous circulation; have been in contact with the criminal justice system and experienced periods of homelessness (Harris et al., 2012). Despite curative treatment (which is now more effective, of shorter duration and better tolerated with few side effects), many PWIDs do not engage with services to be given treatment.
The project described here was preceded by a qualitative research study conducted by one of the authors (RP), who is a Nurse Consultant in Viral Hepatitis and lead for HCV outreach clinics for PWIDs. His study identified barriers and facilitators to attending such outreach clinics for PWIDs infected with HCV (Poll et al., 2017). Numerous reasons were uncovered that explained why patients did not attend (DNA). These included the financial cost and practical difficulties of getting to the clinic; a drug-using lifestyle and having other priorities to meet above addressing their HCV infection; and myths about the health effects of HCV infection and treatment. Thus, the findings of the study revealed that the issue of DNA was complex and no single intervention is likely to work for everyone.
Co-production
Co-production is a slippery concept and if it is not clearly defined, there is a danger its meaning is diluted and its potential to transform services is reduced. At the same time, a definition that is too narrow can stifle creativity and decrease innovation (Social Care Institute for Excellence, 2013).
Co-production is a broadly used term and has various definitions and applications. In the context of this project we define co-production as a meaningful engagement of all stakeholders in the design of new services or knowledge (Social Care Institute for Excellence, 2013)
We will address three contexts in turn:
1. Co-production in research and implementation.
There are research methods that are described as participatory, such as action research, which can be described as co-productive. They are in contrast to the more transactional approaches to involving people as ‘subjects’ or research. They share the recognition that those participants have their own knowledge to contribute. There is also a narrative of Patient and Public Involvement (PPI) in research. The United Kingdom (UK) National Institute of Health Research’s INVOLVE (2019) definition of PPI describes:
working with research funders to prioritise research;
offering advice as members of a project steering group;
commenting on and developing research materials;
undertaking interviews with research participants.
We deliberately do not describe this project activity as PPI as none of the above describe co-productive relationships.
Co-production has developed as a method of knowledge mobilisation in response to the growing evidence on the shortcomings of traditional approaches to getting research evidence into practice. Such traditional methods are referred to in the literature as ‘mode 1’ knowledge mobilisation. This describes the situation where knowledge is created in ‘academic institutions’ then packaged up and translated to non-academic stakeholders, where the professor, in their office writing papers, hopes they are of use to their intended audience. Instead, co-production embraces ‘mode 2’ knowledge mobilisation. This is where knowledge is generated in the context of its use (Gibbons, 1994), ensuring the research is relevant to the end users and informed by them.
2. Health service design.
The need for and practice of co-production in health services has been discussed for several years now in relation to service improvement (Cottam and Leadbeater, 2004). This was seen as the chance to draw on the theory and practice of professionals not usually associated with healthcare. The early work in this area was undertaken by Bate and Robert (2006) and became experience-based co-design. This approach used theory and practice from design as a means to scaffold the contribution of both staff and patients in creating new services. In this project we choose to focus on the generation of new services as a pragmatic process, which is achieved through sharing knowledge from those who both receive and deliver services. The rationale is that service users know not only what does work, but also what does not work, in context. Additionally, no individual can ‘see’ the whole service or appreciate what it is like to both deliver and receive said service, so again multiple viewpoints are needed, including those making the journey though services.
3. Person-centred care.
Co-production aligns closely with the person-centred care agenda (Batalden et al., 2016) and was seen as a good fit for the self-management agenda around recovery. Co-production in healthcare delivery can take the form of shared decision making through to the implementation of person-centred healthcare as described by McCormack and McCance (2006). We did not specifically consider person centredness in this project; however, we recognise that through the co-production of services often a more person-centred service is the natural outcome (Wolstenholme et al., 2017).
Successful co-production has been described as challenging (Greenhalgh et al., 2016) and there remains a lack of guidance about how to do it well. In this case the Nurse Consultant leading this project recognised the potential of co-production and sought expertise by working in partnership with the UK National Institute for Health Research (NIHR) Collaborations for Leadership in Applied Health Research and Care (CLAHRC) Translating Knowledge into Action (TK2A) theme.
The TK2A theme has expertise in the use of co-production in knowledge mobilisation over the past 10 years (Cooke et al., 2016b). They have a particular focus on techniques drawn from design and the creative arts, as these methods encourage and support the successful engagement of stakeholders in co-production (Langley et al., 2018).
The methods of co-production that were used in this project actively involved stakeholders, patients and service users. Co-production was used to ensure all stakeholders:
played a critical part in identifying barriers and solutions to engagement with the clinic;
perceived the project to be a priority with a clear shared goal(s);
developed a keen interest in learning via collaboration; and
found the experience of working together to implement research evidence to be positive.
The primary aim of the project was to devise interventions to improve access to the nurse-led hepatitis C clinic; this sits within the health service design concept of co-production.
Methods
Study setting
This project was undertaken by an HCV service based in a large teaching hospital in the North of England. The service is led by a medical consultant, with a multidisciplinary team comprising of a Nurse Consultant (RP), junior doctors, specialist nurses and a psychologist, social worker and dietician. A weekly morning hospital clinic is run for new and follow-up HCV patients and the Nurse Consultant sees most of the former (four of the six available appointment slots), whereas doctors see the remaining patients. All new patients are offered a telephone appointment reminder and a same-day liver scan (where contact is made) on the day of the appointment. On other days of the week the specialist nurses run hospital clinics for patients on treatment. In addition, the Nurse Consultant runs a weekly HCV outreach clinic in the drug misuse clinic near the city centre and offers four to six appointments on alternate mornings and afternoons. In the outreach clinic, clients of the drug service are offered a discussion about their HCV infection and treatment. Following this, and with the client’s consent, an appointment is arranged with the hospital clinic for a new patient assessment and treatment.
Recruitment
A concise and clearly written information sheet about the project was developed. The project lead’s contact details were added for further information. This information was circulated to approximately 12 third-sector organisations. Representatives from each were invited to participate. Also, the project lead telephoned some participants from his earlier research study and invited them to participate. The Hep C Trust (a national charity) also took part. The service users were given a £20 high street voucher in recognition of the time they offered the project and their travel expenses were reimbursed. The workshops were aligned to phases of the ‘Better Services by Design’ approach (User Centred Healthcare Design, 2015), which has four phases: discover, define, develop and deliver. Methods were drawn from service design and user-centred healthcare design practice.
Study cohort
The study participants comprised of 12 service users who were current or former patients of the hospital HCV clinic and 10 stakeholders representing seven different agencies. The patients all had a history of injecting drug use and some had successfully completed HCV treatment. The service users were male and female and all spoke English. After the first workshop two service users dropped out, one due to deteriorating mental health and the other for an unknown reason. Not all the stakeholders were able to participate in every workshop due to work commitments.
Workshops
Two co-production workshops were held in a neutral venue that was easily accessible for participants using public transport where required.
Workshop 1
The first workshop started with a game of Taboo® as a way of gently introducing participants to each other, to help their minds think creatively and to demonstrate the value a range of different perspectives can bring to a given topic. The workshop moved on to identifying the reasons for missed clinic appointments in two separate groups – service users and stakeholders. The groups were separated for this initial process to allow trust and openness in the process to be established. All subsequent activities were collaborative. Each group was invited to share and record their experiences and knowledge of non-attendance by developing ‘personas’. These are profiles of potential service users including age, occupation, where they lived, their interests and what their needs were and brings together lots of information about similar people into one fictional character (Stickdorn and Schneider, 2012).
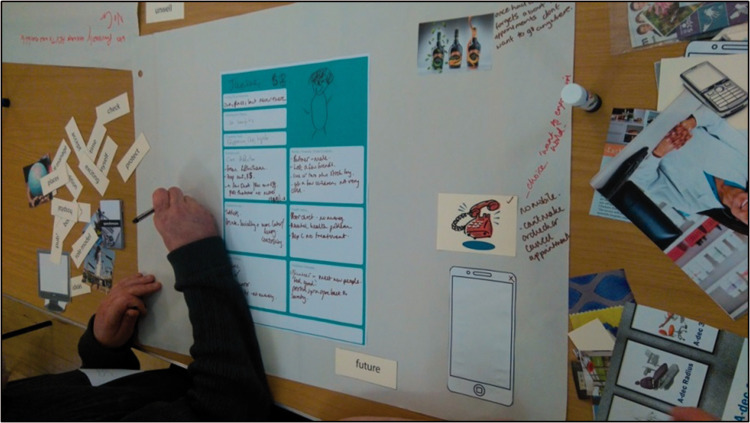
Three outline personas (see example in Figure 1) were provided as a starting point from which to personalise their characters, adding their own details to bring the characters to life (see Figure 2). In addition to using coloured pens, the participants used pictures from magazines and printed cards to complete their personas to enable everyone to contribute regardless as to concerns about ‘not being creative’ or literate.
Figure 1.
Example of persona outline.
HCV: hepatitis C virus; JSA: Jobseeker’s Allowance.
Figure 2.
Developing personas.
The latter part of the first workshop was used for participants to come together and explain their personas to the whole group. This provided an opportunity for others to clarify the details of each persona and begin to identify key themes for missed appointments (see Table 1).
Table 1.
Key themes for missed appointments.
| • Support | • Money |
| • Money | • Place |
| • Information | • Time |
| • Addiction | • Mental health |
| • Transport | • Physical health |
These themes were developed by writing the persona in the centre of a large sheet of paper and asking the groups to consider what might be the barriers or facilitators for their persona to attend the HCV clinic. Again, there was a wide range of visual materials and inspiration to support and promote the groups to identify themes.
The final list of themes was generated during the workshop with a review by the project team of all the materials produced to check nothing had been missed after the workshop. These key themes were similar to the previous research evidence (Poll et al., 2017) and reinforced the complexity of the problem of non-attendance of HCV clinics. Thus, it was likely that a number of interventions would be required to help solve the problem and these interventions would need to be novel, if not innovative. This ideation work was the focus of the second workshop.
Workshop 2
The second workshop began with a warm-up activity, challenging small mixed groups of participants to come up with ‘as many uses for’ a typical household object as possible. Unusual responses were encouraged and constraints introduced to shift the focus of idea generation and encourage new ideas. This approach facilitated joint creative thinking in a safe environment before the creative endeavour was directed at the ‘real’ question.
The next activity was to create a visual outline of the existing referral pathway to the hospital HCV clinic for all the participants. Participants were then split into their two groups again – service users and stakeholders. In these groups, the participants were invited to review their personas (from workshop 1), focusing on the difficulties or barriers they faced in attending the clinic and consider solutions for them. Each group was facilitated by a designer, who used visual methods to capture then explore possible solutions with the participants. Within this process participants were asked to use blue-sky thinking to imagine a service without considering constraints. Different framing techniques were used to help facilitate this, for example, ‘how might a large supermarket chain achieve this’, ‘imagine that you can’t use any written communication to deliver the service’. The framing techniques helped participants, particularly professionals, who (understandably) struggled to see beyond the constraints of their current service provision. Framing has been cited as a good way to explore complex and wicked problems of which non-attendance is a good example (Bowen et al., 2010).
All possible solutions were then shared with the whole group, which enabled discussion and some clarification of the ideas/service proposals put forward. In addition to some novel and innovative service changes, the participants recommended the value of clear and accurate information about HCV such as dispelling myths about care and treatment. The key suggested interventions to improve access to the clinic for PWIDs are summarised in Table 2.
Table 2.
Interventions to improve access.
| Theme | Interventions | |
|---|---|---|
| Incentives | Rewards | Money or gift for attending: tea, coffee, sandwich, cash |
| Enablers | Bus pass/ taxi to allow attendance; mobile phones to engage with service | |
| Take the service to the users: the hep C bus, mobile clinic | ||
| Information | Peer support | Buddy system, paid volunteers |
| Visual communication | Scare-stories posters, discussion prompt cards, information packs | |
| Environment | Environment redesign | |
The workshop outcomes suggested the offer of incentives in the form of money, gifts, refreshments, a bus pass, taxi or mobile phone might improve access to the clinic. Service changes in the form of a different approach to outreach were proposed. They also identified there was a set of ‘scare stories’, information based on previous versions of treatment for HCV, which were potentiated within the drug using community, and that professionals did not necessarily feel able to consistently provide a counter narrative. The possibility of peer support was also suggested. Finally, there was a wide-ranging discussion on the physical environment of one of the key locations of HCV outreach. It was outside the scope of the project to address this within the workshop and this was communicated to participants to ensure transparency.
Workshop 3
In this shorter workshop the service users and stakeholders were invited to contribute to the development of the draft video scripts for both the mobile clinic van and the buddy service, and scare-stories/myths posters.
Finally, a celebration event was held where the final outputs were shared and service users were able to share them with wider stakeholders, local and regional commissioners, and representatives from public health.
Results
The co-production workshops identified four interventions (excluding redesign of the ‘Environment’) that are presented in this section. Two interventions were incentives (Rewards and Enablers). The other two were information (Peer Support and Visual Communication). The project had to be responsive to the emergent ideas and so a range of methods to ‘evaluate’ and test these ideas were developed in collaboration with the project team and workshop participants. These evaluation approaches are also described below.
Incentives: Rewards and enablers
Many participants recognised there were practical reasons that individuals might not be able to get to their appointments. Finance and motivation were two recurrent issues for all the personas developed. The responses to this was two-fold, first to reward attendance and second to arrange transport to enable the individual to attend their appointment. A 3-month project to determine the acceptability and feasibility of offering a reward and an enabler to newly referred patients with a history of drug use. These patients were allocated one of the following if they booked and attended an appointment:
return taxi (enabler) for their appointments;
a £10.00 voucher (reward) for each appointment attended; or
a return taxi and a £10.00 voucher (enabler and reward).
During the project all eligible patients were sent a letter to book a new appointment with the HCV clinic, outlining their allocation of a taxi, voucher or both if they booked and attended an appointment. These were allocated in order of receipt of the referral and not randomly. The HCV clinic routinely runs a weekly telephone reminder service for all new patients booked into the clinic the following week. If the patient attended their appointment the voucher was given after their blood tests and a return taxi arranged where indicated. If a patient attended a further appointment with a health professional or for a scan, within the duration of the project, they were given the same reward or enabler. As well as numerical attendance data, some limited qualitative feedback was collected from the patients (not reported here). After 3 months the project was evaluated. The results suggested it was both feasible to run an incentive scheme and acceptable to patients. Also, despite the small numbers, the change in attendance rates was encouraging.
Service changes
The second initiative suggested by the workshop participants was an ‘enabler’. This was in the form of a mobile clinic van staffed by the hospital specialist team that would provide screening, care and treatment for HCV. The van would be fully equipped and people would not have to attend the hospital for blood tests, scans or treatment. It would stop at various locations throughout the city so people could attend without facing problems due to travel or transport. Also, the van would allow clients motivated not to use drugs to avoid having to attend a hepatitis outreach clinic in a drug treatment service and meet people and behaviours linked to drug use. This proposed change to the way the service is delivered would be a huge undertaking and was considered to be a long-term concept. In the short term it was agreed to produce a short animation and a commentary outlining the benefits of a mobile clinic for one of the personas developed in the workshops. The video can be accessed from the link https://youtu.be/DWCF6j2oygs.
Information: Peer support and visual communication
In keeping with the literature for HCV and other conditions such as substance misuse and HIV, the use of buddies or ‘peer support’ was suggested by the participants as a strategy that may help improve engagement with the clinic (Kulik and Shah, 2016; Simoni et al., 2009). The buddies will have first-hand experience of treatment for HCV and know what is involved; undertaken training for the role and gained a nationally recognised qualification(s); and receive payment for their service. It was anticipated the buddy would accompany the service user to appointments, provide support and advice and signpost the service user to other agencies where needed. Again, similar to the mobile van proposal, this initiative was a long-term aspiration with the concept captured on a short video, which be accessed from https://youtu.be/LmDwnTZEexs.
From a ‘visual communication’ perspective, posters and postcards have been devised from the scare stories identified by the workshop participants about HCV including myths about treatment. These posters were developed alongside the workshop activity, with an iterative approach to gathering the questions, getting responses from the key health professionals and then translating those responses back into lay language. The posters and postcards comprise of a concise statement frequently made about HCV and ask whether it is true or false. On the reverse side, the correct response is given with a brief explanation to support the answer. The posters can be accessed from the https://drive.google.com/file/d/0B7Zq0J4mkDqeRVd4aHVoanJqdG8/view, with copies available for other areas to add their own logo and contact information.
In summary, the workshops enabled the production of four proposed interventions to improve access with the HCV clinic. The testing of the offer of an incentive (voucher) and enabler (taxi) showed an improvement in attendance particularly by using the incentives, and warrants further research. A video illustrating the use of a mobile clinic van has been well received, with interest from other services and commissioners. A pilot service using a van for delivery is being planned. Similarly, a video illustrating the use of peers was produced and a peer co-ordinator has now been employed to build a team of peers. Fourthly, postcards and posters dispelling the myths of HCV and treatment were produced and have been displayed in services locally with requests for their use made by other services across the country.
Discussion
This project shows it is possible to engage a group of service users who are typically hard to access to participate in a project, for example, trying to recruit and gain the experiences of service users who do not attend clinic appointments to be offered curative treatment, let alone participate in a service improvement project. Their participation was achieved in a number of ways. Service users were reimbursed for their time and their travel expenses were paid. It could be argued this conveys to service users that their time and participation is important and on a par with stakeholders who are salaried. The workshops were hosted in a neutral venue, away from clinical and support services. The way the workshops were run and using independent facilitators with no hidden agendas appeared to be successful. For example, each workshop started with a warm-up activity that was non-threatening and designed to help people think creatively. Also, the use of personas and other creative methods enabled people to share their experiences within small groups, rather than individuals simply being asked to disclose personal information in a larger group.
The workshops produced a number of interventions rather than one single intervention. This was in response to the complex and nuanced problem of overcoming DNA in HCV outreach services. Each of the four proposals to emerge from the project will be briefly considered in the light of existing literature and policy.
The initial feasibility and acceptability testing of giving a voucher (incentive) and transport in a taxi (enabler) to improve clinic attendance showed some encouraging results. The National Institute for Health and Care Excellence (NICE) supports the use of incentives, termed contingency management, for people with substance misuse problems where there is some evidence of their effectiveness (NICE, 2007). Also, the use of financial incentives in the form of shopping vouchers has been shown to increase low breastfeeding rates (<40%) in Derbyshire and Yorkshire (Relton et al., 2018). In the UK there does not appear to be any published research about the use of incentives and enablers to improve engagement with HCV clinics. However, some UK research and service improvement work has and is being undertaken using incentives in the form of vouchers (monetary, supermarket) and protein drinks to increase HCV testing and treatment uptake in pharmacies, needle-exchange and drug services (Elsharkawy et al., 2013; Verma and Leeman, 2018). Meanwhile, in a single-centre randomised control trial study in the United States of America with 59 HCV patients randomised to either fixed or lottery-based financial incentives to reinforce clinic attendance and medication adherence, all 31 (100%) assigned to the lottery arm and 24 out of 28 (86%) assigned to the fixed-incentive arm completed a 12-week course of treatment (Wohl et al., 2017). Overall, 92% of scheduled visits were attended. Thus, there appears to be evidence supporting the need for a study investigating the offer of a voucher and taxi to improve attendance at hospital HCV clinics. Such a study would need to include some form of economic analysis to assess the potential cost implications of using incentives and enablers.
The suggestion of a mobile clinic van to improve access to HCV services and increase uptake of treatment appears to be an innovative idea in this field, with HCV services previously running outreach clinics in drug-misuse clinics, general-practitioner (GP) surgeries (providing clinics for the homeless) or health centres and prisons instead. These outreach clinics in drug services and GP practices have been shown to improve attendance rates from 50% (in hospital) to 70–75% (in outreach clinics) (Budd, 2018; Elsharkawy et al., 2013). However, it could be argued that a mobile clinic van offers the flexibility of delivering a clinic in locations not well served by mainstream services and is an alternative for people unable to get to and/or who dislike attending their GP or drug service. For example, an HCV bus with a mobile clinic room has recently started to visit homeless hostels to improve access to care and treatment to a population previously unserved (Agarwal, 2018). Further, some GP practices or other similar settings may be unable to host an outreach clinic due to a shortage of accommodation, addressed by the van. Mobile vans have been employed to deliver other nurse-led services, for example blood-borne virus testing and health screening such as for tuberculosis (University College London NHS Foundation Trust, 2018). This way of delivering services supports the proposal of nurses also delivering HCV treatment (and not just screening) in a van that offers a one-stop shop for people who find it hard to access mainstream services.
The stakeholders and service users suggested a peer support scheme would improve access to HCV clinics and increase uptake of treatment. This type of intervention has been used in other fields notably substance misuse, mental health and HIV (MIND, 2018; Tracy and Wallace, 2016). Similarly, the more established roles of care navigators and health trainers have been employed within the NHS to work with people who are deemed to have complex care needs in the fields of mental health and older people (Simms, 2016; Leveaux et al., 2012). These roles were developed to help people stay well and to avoid repeated admissions to hospital and entail providing health advice; signposting people to other services; care management; and co-ordination of input from multiple agencies. It is anticipated that an HCV peer supporter could use their experience and knowledge of HCV infection and treatment to facilitate a person to engage with a clinic. A peer would meet with the person (with their consent) to offer advice and support and accompany them to the clinic.
Finally, it was suggested that the myth-busting posters might help people with HCV engage with clinics. Many people with HCV may rely on information about the infection and its treatment from their drug-using acquaintances and can be misinformed. Also, the field of HCV infection and particularly its treatment has advanced considerably over the years. New direct-acting, antiviral tablets are given over several weeks with few side effects and high cure rates (NICE, 2015, 2018). It is important that new and correct information is made available to people with HCV infection. Although the posters have been made available as widely as possible, it is recognised that some people who are not in contact with services will not see them and will need to be provided with information through other means such as outreach workers.
The project provides further evidence and a response to two points from the literature; first, that co-production is hard and second that nurses should be at the forefront of facilitating the involvement of individuals and their carers in co-designing and providing care services. Using a creative co-productive approach allowed genuine and authentic involvement of stakeholders in redesigning services. Second, using the described approach helped to overcome the challenges identified in doing co-production, namely power differences (Greenhalgh et al., 2016; Kothari and Wathen, 2017), time (Kothari and Wathen, 2017; Rycroft-Malone et al., 2016), trust (Greenhalgh et al., 2016) and language (Cooke et al., 2016a).
Conclusion
Using co-production and creative methods allowed those who usually do not have a voice in the design of services to contribute, thus developing contextually sensitive solutions that are more likely to work for hard-to-access groups and those services trying to access them. Sometimes the most obvious solutions from the healthcare professional perspective (outreach clinic) is not the best solution for the service users and their broader context, as participants did not want to identify with treatment for substance abuse. Visual methods and a solution-based approach deliver outputs that commissioners and other health services find easier and more compelling to work with than traditional report-based outputs of projects, and there is a sense of legitimacy from the co-production methods. Co-production methods attend to a solution-based approach allowing people’s involvement to be recognised and validated by the project outputs.
Key points for policy, practice and/or research
This project and its outcomes offer some implications for nursing practice, which include:
A candidate method for nurses to transform high-quality evidence, which highlights a clinical problem, into solutions that are grounded in patient’s experience and context.
Generate further research questions that are grounded in a desire to improve service delivery and benefit patients.
Biography
Daniel Wolstenholme was the programme manager of the NIHR CLAHRC Yorkshire and Humber and managed the Translating Knowledge into Action Theme. He is an NMC-registered Adult Nurse who has worked in health services research for the last 12 years as part of the NIHR CLAHRC Yorkshire and Humber. Dan's research interest is in knowledge mobilisation, specifically creative co-production, or how using creative methods we can get people to work together to deliver meaningful, successful change.
Ray Poll has been Nurse Consultant for Viral Hepatitis at Sheffield Teaching Hospitals NHS Foundation Trust since 2002. He is responsible for the strategic development and management of nurse-led clinics in hospital and a drug-treatment service (for clients infected with hepatitis C). The latter was the setting for his doctoral study completed in 2014, investigating the reasons for clients’ missed appointments. His research interests include exploring ways to make services more accessible to patients. He is nurse member of the National Strategy Group for Viral Hepatitis. Ray has published in a variety of nursing and medical journals and a chapter for a research-based public health book.
Angela Tod is a Professor of Older People and Care in the School of Nursing and Midwifery at the University of Sheffield. Her nursing background is in cardiology and cardiac rehabilitation. Angela has many years of experience conducting and applying research into healthcare, as well as posts focusing on research capacity building in nurses, midwives and allied health professionals. Her research has mainly focused on care for adults and older people. Her particular research focus is in patient experience studies, especially in areas of public health, health inequalities and health care access. Angela’s methodological expertise lies in qualitative research, in standalone and mixed-method studies.
Contributor Information
Daniel Wolstenholme, Director, Centre for Quality Improvement and Clinical Audit, Royal College of Obstetricians and Gynaecologists, United Kingdom.
Ray Poll, Nurse Consultant for Viral Hepatitis, Sheffield Teaching Hospitals, NHS Foundation Trust Sheffield, United Kingdom.
Declaration of conflicting interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The authors authored the article within the scope of employment for their employer, Sheffield Teaching Hospitals NHS Foundation Trust.
Ethics
This project was approved through clinical governance as a service improvement project by Sheffield Teaching Hospitals NHS Foundation Trust. Ethical principles were adhered to and informed consent was obtained from all participants.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The research was funded by the NIHR CLAHRC Yorkshire and Humber. The views expressed are those of the author(s), and not necessarily those of the NIHR or the Department of Health and Social Care (http://clahrc-yh.nihr.ac.uk).
ORCID iD
Daniel Wolstenholme https://orcid.org/0000-0003-1507-6043
References
- Agarwal K (2018) Transforming hepatitis C treatment from cure to elimination. Available at: https://www.kingshealthpartners.org/latest/1884-transforming-hepatitis-c-treatment-from-cure-to-elimination (accessed 18 August 2019).
- Batalden M, Batalden P, Margolis P, et al. (2016) Co-production of healthcare service. BMJ Quality and Safety 25(7): 509–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bate P, Robert G. (2006) Experience-based design: From redesigning the system around the patient to co-designing services with the patient. Quality & Safety In Health Care 15(5): 307–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Dearden A, Wright P, et al. (2010) Participatory healthcare service design and innovation. In: ACM International Conference Proceeding Series, 2010.
- Cooke J, Langley J, Wolstenholme D, et al. (2016. a) “Seeing” the difference: The importance of visibility and action as a mark of “authenticity” in co-production. International Journal of Health Policy Management 5: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooke J, Langley J, Wolstenholme D, et al. (2016. b) ‘Seeing’ the difference: The importance of visibility and action as a mark of ‘authenticity’ in co-production: Comment on ‘collaboration and co-production of knowledge in healthcare: opportunities and challenges’. International Journal of Health Policy and Management 6(6): 345–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costella A (2018) Hepatitis C in England 2018 report. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/693917/HCV_in_England_2018.pdf (accessed 12 March 2019).
- Cottam H and Leadbeater C (2004) RED Paper 01 Health: Co-creating Services. Available at: http://www.designcouncil.info/RED/health/REDPaper01.pdf (accessed 25 October 2011).
- Elsharkawy AM, Miller C, Hearn A, et al. (2013) Improving access to treatment for patients with chronic hepatitis C through outreach. Frontline Gastroenterology 4(2): BMJ Publishing Group: 125–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons M (1994) The New Production of Knowledge: The Dynamics of Science and Research in Contemporary Societies. Sage. Available at: https://uk.sagepub.com/en-gb/eur/the-new-production-of-knowledge/book204307 (accessed 19 June 2017).
- Greenhalgh T, Jackson C, Shaw S, et al. (2016) Achieving research impact through co-creation in community-based health services: Literature review and case study. Milbank Quarterly 94(2): 392–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- INVOLVE (2019) Frequently asked questions | INVOLVE. Available at: https://www.invo.org.uk/frequently-asked-questions/ (accessed 15 November 2019).
- Kothari A, Wathen CN. (2017) Integrated knowledge translation: Digging deeper, moving forward. Journal of Epidemiology and Community Health 71(6): 619–623. [DOI] [PubMed] [Google Scholar]
- Kulik W, Shah A. (2016) Role of peer support workers in improving patient experience in Tower Hamlets Specialist Addiction Unit. BMJ Quality Improvement Reports 5(1): BMJ Open Quality: u205967.w2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langley J, Wolstenholme D, Cooke J. (2018) ‘Collective making’ as knowledge mobilisation: The contribution of participatory design in the co-creation of knowledge in healthcare. BMC Health Services Research 18(1): 585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack B, McCance T V. (2006) Development of a framework for person-centred nursing. Journal of Advanced Nursing 56(5): 472–479. [DOI] [PubMed] [Google Scholar]
- MIND (2018) Peer support | Mind, the mental health charity - help for mental health problems. Available at: https://www.mind.org.uk/information-support/drugs-and-treatments/peer-support/#.XIgQ0y10fOR (accessed 12 March 2019).
- NHS England (2016) Leading Change, Adding Value: A framework for nursing, midwifery and care staff. Available at: https://www.england.nhs.uk/wp-content/uploads/2016/05/nursing-framework.pdf (accessed 30 July 2018).
- NICE (2007) Appendix C: Contingency management – key elements in the delivery of a programme | Drug misuse in over 16s: Psychosocial interventions | Guidance. Available at: https://www.nice.org.uk/guidance/cg51/chapter/Appendix-C-Contingency-management-key-elements-in-the-delivery-of-a-programme (accessed 12 March 2019).
- NICE (2015) Overview | Ledipasvir–sofosbuvir for treating chronic hepatitis C | Guidance. Available at: https://www.nice.org.uk/guidance/ta363 (accessed 12 March 2019).
- NICE (2018) Overview | Glecaprevir–pibrentasvir for treating chronic hepatitis C | Guidance. Available at: https://www.nice.org.uk/guidance/ta499 (accessed 12 March 2019).
- NMC (2015) The Code Standards of conduct, performance and ethics for nurses and midwives. London: NMC Available at: http://www.nmc-uk.org/.
- Pawlotsky JM, Negro F, Aghemo A, et al. (2018) EASL Recommendations on Treatment of Hepatitis C 2018 J Hepatol 69: 461–511. [DOI] [PubMed]
- Poll R, Allmark P, Tod AM. (2017) Reasons for missed appointments with a hepatitis C outreach clinic: A qualitative study. International Journal of Drug Policy 39: 130–137. [DOI] [PubMed] [Google Scholar]
- Rycroft-Malone J, Burton CR, Bucknall T, et al. (2016) Collaboration and co-production of knowledge in healthcare: Opportunities and challenges. International Journal of Health Policy Management 5(54): 221–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Huh D, Frick PA, et al. (2009) Peer support and pager messaging to promote antiretroviral modifying therapy in Seattle: A randomized controlled trial. Journal of Acquired Immune Deficiency Syndromes (1999) 52(4): 465–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Social Care institute for Excellence (2013) Co-production in social care: What it is and how to do it: What is co-production. Available at: https://www.scie.org.uk/publications/guides/guide51/what-is-co-production/index.asp (accessed 6 July 2018).
- Stickdorn M and Schneider J (2012) This Is Service Design Thinking: Basics, Tools, Cases. Wiley. Available at: http://books.google.co.uk/books?id=vmzJkQEACAAJ (accessed 6 July 2018).
- Tracy K and Wallace SP (2016) Benefits of peer support groups in the treatment of addiction. Substance Abuse and Rehabilitation 7: 143–154.. [DOI] [PMC free article] [PubMed]
- University College London NHS Foundation Trust (2018) Find & Treat service. Available at: https://www.uclh.nhs.uk/OurServices/ServiceA-Z/HTD/Pages/MXU.aspx (accessed 12 March 2019).
- User Centred Healthcare Design (2015) Better Services by Design. Available at: http://www.bsbd.org.uk/ (accessed 6 July 2018).
- Verma S and Leeman D (2018) HCV testing in NSP (Needle and Syringe Provision) Community Pharmacies Pilot (Phase 1) Report and Findings. Available at: http://apps.who.int/iris/bit- (accessed 12 March 2019).
- Wohl DA, Allmon AG, Evon D, et al. (2017) Financial Incentives for Adherence to Hepatitis C Virus Clinical Care and Treatment: A Randomized Trial of Two Strategies. Open Forum Infectious Diseases 4(2). Oxford: Oxford University Press. [DOI] [PMC free article] [PubMed]
- Wolstenholme D, Ross H, Cobb M, et al. (2017) Participatory design facilitates person centred nursing in service improvement with older people: A secondary directed content analysis. Journal of Clinical Nursing 26: 1217–1225. [DOI] [PMC free article] [PubMed] [Google Scholar]