Abstract
Abdominal wall blocks provide considerable analgesia for relieving post-operative pain. Although they have been performed generally for post-operative pain management, abdominal wall blocks can be used as the principal anaesthesia method in certain cases. In this study, the case of a 47-year-old male patient who underwent surgical excisional biopsy for 2 vague intramuscular mass lesions (was within the rectus abdominis muscle and the other was within the transversus abdominis muscle) was presented. Ultrasonography (USG)-guided oblique subcostal transversus abdominis plane block in combination with USG-guided rectus sheath block was performed successfully as anaesthesia for the abdominal wall surgery. The intervention was performed fully under regional anaesthesia without any need for deep sedation or general anaesthesia.
Keywords: Abdominal wall, oblique subcostal transversus abdominis plane block, pain management, rectus sheath block, regional anaesthesia
Introduction
Surgical excisional biopsy of superficial mass lesions is usually performed as an outpatient procedure in the office setting using a local anaesthetic. However, sedation or general anaesthesia or regional nerve blocks are needed in some non-compliant patients or for the interventions of lesions located in deep tissues. The use of peripheral regional anaesthetic techniques has been shown to be effective for post-operative pain management. In addition, it has been recommended to consider the use of surgical site-specific regional analgesic techniques as part of multi-modal analgesia (1).
In this study, ultrasonography (USG)-guided oblique subcostal transversus abdominis plane (TAP) block in combination with USG-guided rectus sheath (RS) block has been presented as the principal anaesthesia technique for abdominal wall surgery.
Case Presentation
A 47-year-old male patient (182 cm, 85 kg) with the American Society for Anesthesiologists score of II was admitted to the hospital because of fast-growing palpable swellings and pain on the abdominal wall. Physical examination and USG revealed 2 vague intramuscular mass lesions; 1 was present within the rectus abdominis muscle (2×3 cm2), and 1 was present within the transversus abdominis muscle (3×5 cm2). The patient underwent diagnostic excisional biopsy of the 2 mass lesions under local infiltration anaesthesia. However, the intervention could not be finished owing to severe pain because of inadequacy of local anaesthesia for the surgical procedure. Thereafter, the patient was scheduled for surgery in the operating room with the plan of deep sedation or general anaesthesia. In the operating room, after obtaining the consent from the patient, USG-guided oblique subcostal TAP block in combination with RS block was performed as anaesthesia for the abdominal wall surgery. Furthermore, 15 minutes after block administration, the sensory blockade to pinprick sufficiently covered the surgical area. The intervention was performed entirely under regional anaesthesia without any need for further sedative administration (except for 2 mg midazolam used for premedication) or general anaesthesia.
Abdominal wall blocks
Abdominal wall blocks were performed after routine monitoring of electrocardiogram, non-invasive blood pressure and oxygen saturation. After premedication with 2 mg midazolam, USG-guided (6–18 MHz linear probe, Esaote® MyLabSeven, Italy) oblique subcostal TAP block and RS block were performed using an in-plane technique with 21-G 50-mm and 100-mm insulated stimulator needles (SonoPlex STIM®, Pajunk®, Germany). Full aseptic precautions were maintained during the procedure.
Posterior rectus sheath block
Posterior RS block was performed for the excision of the first intramuscular mass that was present within the substance of the rectus abdominis muscle. USG scout scanning was performed above the level of the umbilicus (below the xiphoid) starting from the medial and proceeding to the lateral abdominal wall. The linea alba, rectus muscle, mass lesion within the substance of rectus muscle, peritoneal cavity, linea semilunaris, external abdominal oblique, internal abdominal oblique and transversus abdominis muscles were visualised (Figure 1). After scout scanning and identifying the landmarks for the block, the linear USG probe was placed at a level below the xiphoid (above the mass lesion). Using the in-line approach, the block needle was inserted with a lateral to medial trajectory. The needle was then advanced through the subcutaneous tissues, the anterior rectus sheath, into the rectus muscle. Once the needle tip approached the posterior aspect of the muscle, care was taken not to advance it too deep owing to the very close proximity of the peritoneum. The target site for needle tip placement was superficial to the posterior rectus sheath. After verifying the correct placement of the needle by a test injection, 15 mL of a local anaesthetic (0.5% bupivacaine) was injected, and the spread of the local anaesthetic opening the compartment was seen (Figure 2). After the block, the local anaesthetic covering the posterior aspect of the rectus muscle was confirmed with a post-block USG scan along the rectus muscle.
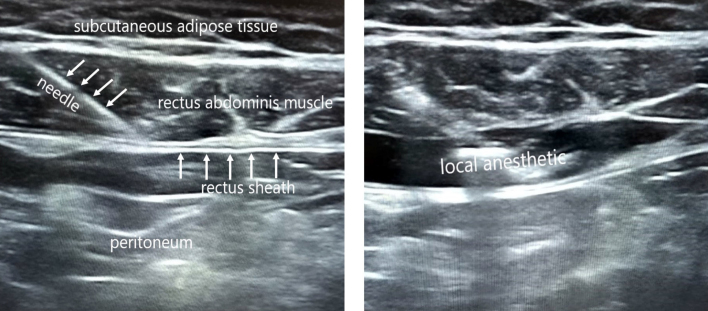
Figure 1.
Sonogram of the anterior abdominal wall (arrows indicating the mass lesion within the rectus abdominis muscle)
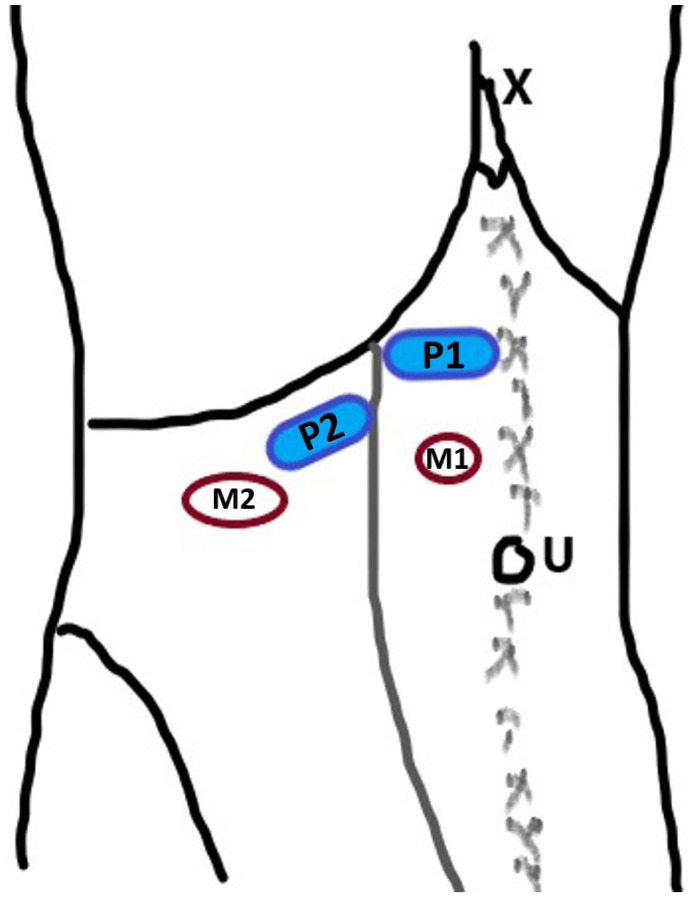
Figure 2.
Sonogram of the rectus sheath block
Left: Labelled sonogram showing the advancing needle; Right: Hydrodissection of the posterior aspect of the rectus abdominis muscle from posterior rectus sheath
Oblique subcostal transversus abdominis plane block
Oblique subcostal TAP block was performed for the excision of the second intramuscular mass lesion that was present within the transversus abdominis muscle. USG scout scanning was performed with the USG probe placed obliquely on the upper abdominal wall starting from the medial to lateral abdominal wall along the costal margin. The linea alba, rectus muscle, peritoneal cavity, linea semilunaris, external abdominal oblique, internal abdominal oblique and transversus abdominis muscles and the mass lesion within the transversus abdominis muscle were visualised. The planned block site was matched with the second surgical incision. After identifying the landmarks for the block (rectus abdominis muscle and underlying hypoechoic transversus abdominis muscle), the block needle was inserted in-plane from the medial to lateral abdominal wall. The needle was then advanced through the subcutaneous adipose tissue and the rectus abdominis muscle and entered the plane between the rectus abdominis and transversus abdominis muscles. After verifying the correct placement of the needle by a test injection, 15 mL of a local anaesthetic (0.5% bupivacaine) was injected, and hydrodissection of the subcostal plane was seen. After the block, the local anaesthetic spread between the rectus abdominis and transversus abdominis, and it spread laterally between the internal abdominal oblique and transversus abdominis muscles, which was confirmed with a post-block USG scan along the subcostal line.
Discussion
USG-guided oblique subcostal TAP block was described by Hebbard et al. (2) for post-operative analgesia, especially for upper abdominal surgeries. Thereafter, it was used successfully as an analgesic technique in abdominal surgeries and chronic pain management (3–5). Recently, TAP block was reported as a principal regional anaesthesia technique in minimally invasive abdominal surgeries (6, 7). Subcostal oblique TAP block aims to provide analgesia for upper abdominal incision as high as the T8 level. Although oblique subcostal TAP block provides analgesia for somatic pain in almost the entire anterior abdominal wall, it may be inadequate for the incisions close to the xiphoid or the midline of the abdomen. In this study, subcostal oblique TAP block was performed successfully as the anaesthetic technique for the second subcostal surgical site (Figure 3).
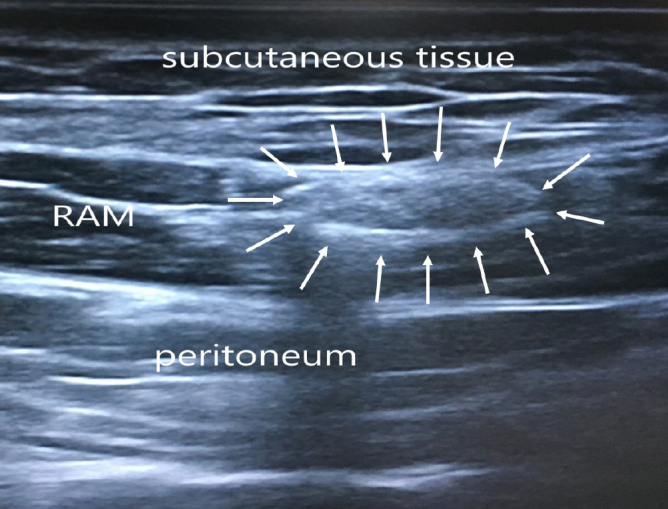
Figure 3.
Diagram showing the scan positions for the blocks
U: Umbilicus; X: Xiphoid process; P1: Probe position for rectus sheath block; P2: Probe position for oblique subcostal transversus abdominis plane block; M1: Location of the first mass lesion within the rectus abdominis muscle; M2: Location of the second mass lesion within the transversus abdominis muscle
USG-guided RS block is generally used for analgesia for vertical midline or paramedian surgical incisions. Posterior RS block provides its analgesic effect on the middle portion of the abdominal wall from the xiphoid to the symphysis pubis by targeting the ventral rami of the 7th to 12th intercostal nerves (8). In several surgical procedures requiring midline skin incisions, RS block was shown to reduce systemic analgesic requirements when performed in addition to general anaesthesia (9). Recently, it was reported that RS block (in combination with sedation) was performed successfully for surgical anaesthesia in a patient undergoing diverting colostomy (10). In this study, RS block was performed successfully for the anaesthetic technique of the first surgical site (the paramedian incision made just below the level of the xiphoid).
Conclusion
This case highlights that abdominal wall blocks can be effectively used as the principal anaesthesia technique in certain cases.
Main Points:
The subcostal transversus abdominis plane block provides adequate analgesia for upper abdominal surgery.
The rectus sheath block provides analgesia on the middle portion of the abdominal wall from the xiphoid to the symphysis pubis.
Abdominal wall blocks are generally used as a part of multimodal analgesia. They can also be used effectively as the principal anaesthesia technique in certain cases.
Acknowledgements
I would like to thank to Dr. Gonca Yıldız for her assistance with the surgery.
Footnotes
Informed consent: Written informed consent was obtained from the patient who participated in this case.
Peer-review: Externally peer-reviewed.
Conflict of Interest: The author have no conflicts of interest to declare.
Financial Disclosure: The author declared that this study has received no financial support.
References
- 1.Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, et al. Management of Postoperative Pain: A Clinical Practice Guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17:131–57. doi: 10.1016/j.jpain.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 2.Hebbard PD, Barrington MJ, Vasey C. Ultrasound-guided continuous oblique subcostal transversus abdominis plane blockade: description of anatomy and clinical technique. Reg Anesth Pain Med. 2010;35:436–51. doi: 10.1097/AAP.0b013e3181e66702. [DOI] [PubMed] [Google Scholar]
- 3.Altıparmak B, Korkmaz Toker M, Uysal AI, Kuşçu Y, Gümüş Demirbilek S. Ultrasound-guided erector spinae plane block versus oblique subcostal transversus abdominis plane block for postoperative analgesia of adult patients undergoing laparoscopic cholecystectomy: Randomized, controlled trial. J Clin Anesth. 2019;57:31–6. doi: 10.1016/j.jclinane.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 4.Tulgar S, Kapakli MS, Kose HC, Senturk O, Selvi O, Serifsoy TE, et al. Evaluation of Ultrasound-Guided Erector Spinae Plane Block and Oblique Subcostal Transversus Abdominis Plane Block in Laparoscopic Cholecystectomy: Randomized, Controlled, Prospective Study. Anesth Essays Res. 2019;13:50–6. doi: 10.4103/aer.AER_194_18. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 5.Kale A, Aytuluk HG, Cam I, Basol G, Sunnetci B. Selective Spinal Nerve Block in Ilioinguinal, Iliohypogastric and Genitofemoral Neuralgia. Turk Neurosurg. 2019;29:530–7. doi: 10.5137/1019-5149.JTN.23990-18.1. [DOI] [PubMed] [Google Scholar]
- 6.Yamamoto H, Shido A, Sakura S, Saito Y. Monitored anesthesia care based on ultrasound-guided subcostal transversus abdominis plane block for continuous ambulatory peritoneal dialysis catheter surgery: case series. J Anesth. 2016;30:156–60. doi: 10.1007/s00540-015-2074-0. [DOI] [PubMed] [Google Scholar]
- 7.Li Z, Tang XH, Li Q, Zhang WJ, Tao T, Zhu T. Ultrasound-Guided Oblique Sub-Costal Transversus Abdominis Plane Block as the Principal Anesthesia Technique in Peritoneal Dialysis Catheter Implantation and Plasma Ropivacaine Concentration Evaluation in ESRD Patients: A Prospective, Randomized, Double-Blinded, Controlled Trial. Perit Dial Int. 2018;38:192–9. doi: 10.3747/pdi.2017.00222. [DOI] [PubMed] [Google Scholar]
- 8.Osaka Y, Kashiwagi M, Nagatsuka Y, Oosaku M, Hirose C. Ultrasound-guided rectus sheath block for upper abdominal surgery. Masui. 2010;59:1039–41. [PubMed] [Google Scholar]
- 9.Karaarslan E, Topal A, Avci O, Tuncer Uzun S. Research on the efficacy of the rectus sheath block method. Agri. 2018;30:183–8. doi: 10.5505/agri.2018.86619. [DOI] [PubMed] [Google Scholar]
- 10.Duggan EW, Vadlamudi R, Spektor B, Sharifpour M. Abdominal Surgery with Bilateral Rectus Sheath Block: A Case Report. A A Pract. 2019;13:278–80. doi: 10.1213/XAA.0000000000001055. [DOI] [PubMed] [Google Scholar]