Abstract
BACKGROUND
Hypoxaemia is frequently seen during flexible bronchoscopies that are done with a nasal approach under the traditional sedation with propofol. This study investigated the potential benefits of supraglottic jet oxygenation and ventilation (SJOV) using the Wei nasal jet tube (WNJ) in reducing hypoxaemia in patients undergoing bronchoscopy under moderate to deep intravenous sedation using a propofol, lidocaine and remifentanil cocktail.
OBJECTIVES
Our primary objective was to evaluate the efficacy and complications of SJOV via the WNJ during flexible bronchoscopy under moderate to heavy sedation with propofol and remifentanil.
DESIGN
A randomised controlled clinical trial.
SETTING
The 180th Hospital of People's Liberation Army, Quanzhou, China, from 1 June to 1 November 2019.
PATIENTS
A total of 280 patients aged ≥18 years with American Society of Anesthesiologists’ physical status 1 to 3 undergoing flexible bronchoscopy were studied.
INTERVENTIONS
Patients were assigned randomly into one of two groups, a nasal cannula oxygenation (NCO) group (n = 140) using a nasal cannula to deliver oxygen (4 l min−1) or the SJOV group (n = 140) using a WNJ connected to a manual jet ventilator to provide SJOV at a driving pressure of 103 kPa, respiratory rate 20 min−1, FiO2 1.0 and inspiratory:expiratory (I:E) ratio 1:2.
MAIN OUTCOME MEASURES
The primary outcome was an incidence of desaturation (defined as SpO2 < 90%) during the procedure. Other adverse events related to the sedation or SJOV were also recorded.
RESULTS
Compared with the NCO group, the incidence of desaturation in the SJOV group was lower (NCO 37.0% vs. SJOV 13.1%) (P < 0.001). Patients in the SJOV group had a higher incidence of a dry mouth at 1 min (13.1% vs. 1.5%, P < 0.001) than at 30 min (1.5% vs. 0%, P = 0.159) or at 24 h (0% vs. 0%). There was no significant difference between the groups in respect of sore throat, subcutaneous emphysema or nasal bleeding.
CONCLUSIONS
SJOV via a WNJ during flexible bronchoscopy under moderate to deep sedation with propofol and remifentanil significantly reduces the incidence of desaturation when compared with regular oxygen supplementation via a nasal cannula. Patients in the SJOV group had an increased incidence of transient dry mouth.
TRIAL REGISTRATION
Registered at www.chictr.org.cn (ChiCTR1900023514).
Introduction
Flexible bronchoscopy has been used in both diagnostic and therapeutic applications in treating lung diseases.1 Without sedation, patients often find the procedure extremely uncomfortable, experiencing difficulty with breathing, coughing, pain, fear, anxiety and airway irritation. With adequate sedation (or general anaesthesia), patients have better tolerance of the procedure, with reductions in coughing, fear and complications.2,3 Amanda et al.4 suggested that sedation should be recommended for all patients undergoing bronchoscopy procedures except where contraindications exist. The use of a mixture of propofol 0.5 mg/kg and remifentanil 0.5 μg/kg has been reported to produce a high satisfaction score with patients and bronchoscopists because of its short recovery time, but also has a high incidence of hypoxaemia.5 Hypoxaemia is usually caused by suppression of ventilation due to controlled sedation and the bronchoscopy, which produces both obstruction and stimulation of the airway.
Studies have shown that 82.5% of patients undergoing this procedure experience hypoxaemia if not supplied with supplemental oxygen.6 The procedure is complicated and fraught with difficulty because the anaesthesiologist and bronchoscopist share the same airway.7 If hypoxaemia occurs (as defined as SpO2 < 90%), the procedure should be stopped until the hypoxaemia is corrected. Supplemental oxygen can be very helpful in reducing hypoxaemia during flexible bronchoscopy,8–11 but there is still a risk of hypoxaemia due to insufficient ventilation because the flexible bronchoscope occupies part of the airway and stimulates the bronchus, leading to dyspnoea or apnoea. Additionally, depression due to sedative drugs or anaesthetics can lead to insufficient ventilation. Hypoxaemia has been reported to occur in 40% of sedated bronchoscopy patients.12 High-flow nasal oxygen (HFNO) has been proposed to prevent hypoxaemia during bronchoscopy, but has not shown any significant advantage over standard oxygen flow at 10 l min−1.8 Furthermore, studies have indicated that HFNO results in the accumulation CO2 because of insufficient ventilation.13,14
Supraglottic jet oxygenation and ventilation (SJOV) is established by placing a jet catheter through the nasal cavity, and has been used effectively in both oxygenation and ventilation15 as well as in difficult airway management and colonoscopy.16–20 The Wei nasal jet tube (WNJ; Well Lead Medical Company, Guangzhou, China) has two channels built inside its wall, one for jet oxygenation and ventilation delivered supraglottically and the other for monitoring the end-tidal partial pressure of CO2 (Fig. 1). SJOV with the WNJ has been used effectively in upper gastrointestinal endoscopy in patients under sedation with propofol.21,22 It has also been used in fibreoptic bronchoscopic intubation of paralysed patients with a difficult airway,23 without severe complications such as barotrauma or severe nose bleeding.21–23 Therefore, we proposed that using SJOV with the WNJ may be appropriate for reducing hypoxaemia during flexible bronchoscopy under moderate to heavy sedation with a combination of propofol, lidocaine and remifentanil.
Fig. 1.
Components for flexible bronchoscopy using the Wei nasal jet tube
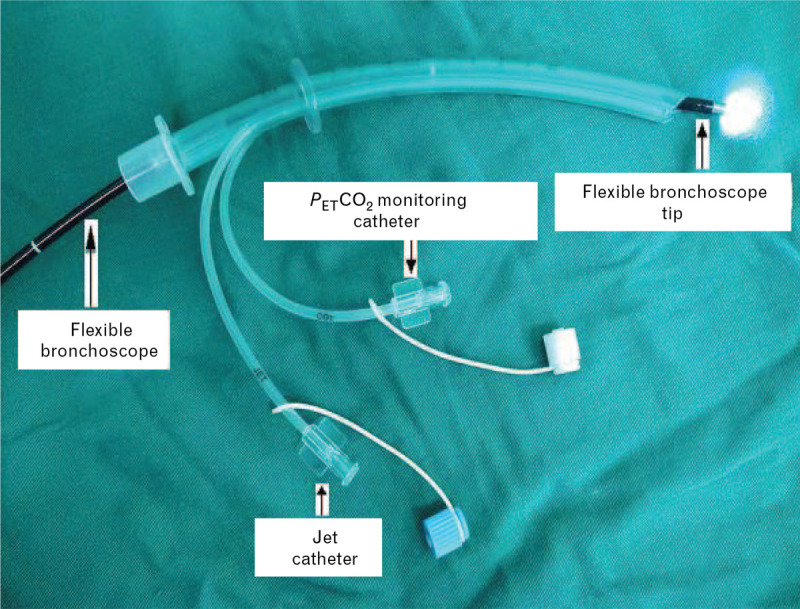
PETCO2, end-tidal partial pressure of carbon dioxide.
Our study aim was to evaluate the efficacy and complications of SJOV via the WNJ during flexible bronchoscopy under moderate to heavy sedation. We hypothesised that using SJOV via the WNJ would result in a lower incidence of hypoxaemia than procedures performed with only supplemental oxygen delivered by a nasal cannula in patients under sedation with a combination of propofol, lidocaine and remifentanil during flexible bronchoscopy.
Methods
This randomised controlled clinical trial was approved (2019–33) by the Medical Ethics Committee of the 180th Hospital of People's Liberation Army, Quanzhou, China, on 27 May 2019. The study was registered at www.chictr.org.cn (ChiCTR1900023514). The study was conducted in accordance with the Declaration of Helsinki, as all the authors had access to the study data and reviewed and approved the final manuscript. All investigators, including nurses and anaesthesiologists, participated in the standardised training for the use of SJOV, including the mechanism of action, indications and contraindications for its use in upper airway flexible bronchoscopy, and the precautions for and management of predicted adverse events. Written informed consent was obtained from all participating patients.
Patients aged ≥18 years with American Society of Anesthesiologists’ (ASA) physical status of 1–3 undergoing flexible bronchoscopy from 1 June to 1 November 2019 were studied. Patients with the following conditions were excluded: pre-operative resting pulse oxygen saturation on room air <90%, obstructive sleep apnoea [OSA; STOP-BANG (Snoring, Tiredness, Observed apnoea, blood Pressure, Body mass index, Age, Neck circumference and Gender) ≥3],24 intolerance of or allergic to the study drug, history of nasopharyngeal surgery, nasal malformation, nasal tissue hyperplasia, bleeding diseases or pregnancy. Patients were allocated randomly to one of two groups according to computer-generated randomisation results: nasal cannula supplement oxygen group (NCO group) or SJOV via the WNJ (SJOV group). Randomisation was undertaken using opaque sealed envelopes which were selected randomly before induction of anaesthesia.
Patients fasted pre-operatively for at least 8 h and were premedicated with i.v. midazolam 0.02 mg kg−1 in the preparation room. Patients received standard monitoring, including heart rate, electrocardiogram, noninvasive arterial pressure and oxygen saturation with pulse oximetry (SpO2). Patients were premedicated to receive nebulisation of 2% lidocaine using a nebulisation device.
Patients were pre-oxygenated for 3 min via a facemask with an oxygen flow rate of 10 l min−1 immediately preceding sedation. The patients were then treated with boluses of a propofol/lidocaine cocktail (propofol 200 mg + lidocaine 40 mg) with 0.5 mg kg−1 of propofol and 0.5 μg kg−1 of remifentanil i.v.5 This was followed by a continuous infusion of remifentanil 0.075 μg kg−1 min−1 at the discretion of the anaesthesiologist. The depth of sedation was assessed to achieve a moderate to deep sedation level using the modified observer's assessment of alertness/sedation (MOAA/S)25 score of 2 or 3 (5, responds readily to name spoken in normal tone; 4, lethargic and responds to name spoken in normal tone; 3, responds only after name is called loudly, repeatedly or both; 2, responds only after mild prodding or shaking; 1, responds only after painful trapezius squeeze; 0, does not respond to painful trapezius squeeze). Patients were administered additional boluses of propofol (10 or 20 mg) when MOAA/S was >3.
In the NCO group, patients received supplemental oxygen (4 l min−1) via a nasal cannula in one nostril; the other was used for the flexible bronchoscope.
In the SJOV group, a well-lubricated WNJ was inserted into one nostril. The inserted depth was the distance from the tip of the nose to the earlobe on one side. We would try the other nostril if the insertion into one nostril failed twice. If WNJ insertion into the second nostril also failed twice, the patient was excluded from the study. A flexible bronchoscope was placed through the lumen of the WNJ as a conduit after the WNJ had been inserted successfully into the nostril. SJOV was subsequently established using a manual jet ventilator (Well Lead Medical Company, Guangzhou, China) connected to the proximal end of a built-in jet catheter on the WNJ (Fig. 2) with the following working parameters: driving pressure 103 kPa, respiratory rate 20 min−1, inspiratory:expiratory (I:E) ratio 1:2 and gas source 100% oxygen. Positioning of the WNJ was adjusted and verified during SJOV based on optimal chest expansion. If obvious chest rising did not occur, an up-and-down manoeuvre was performed to change the depth of the insertion, or the WNJ was rotated slightly. The anaesthesiologist titrated the propofol and remifentanil infusions to maintain moderate to deep sedation with propofol.
Fig. 2.
Illustration of a well lubricated Wei nasal jet tube inserted into the left nostril with supraglottic jet oxygenation and ventilation during flexible bronchoscopy
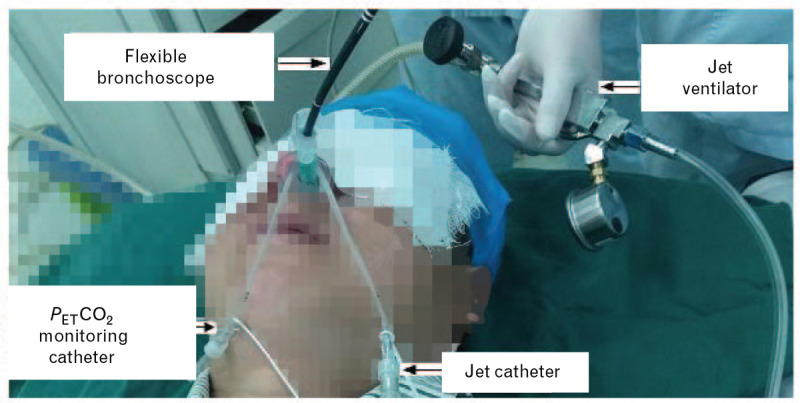
PETCO2, end-tidal partial pressure of carbon dioxide.
Fig. 3.
CONSORT flow diagram
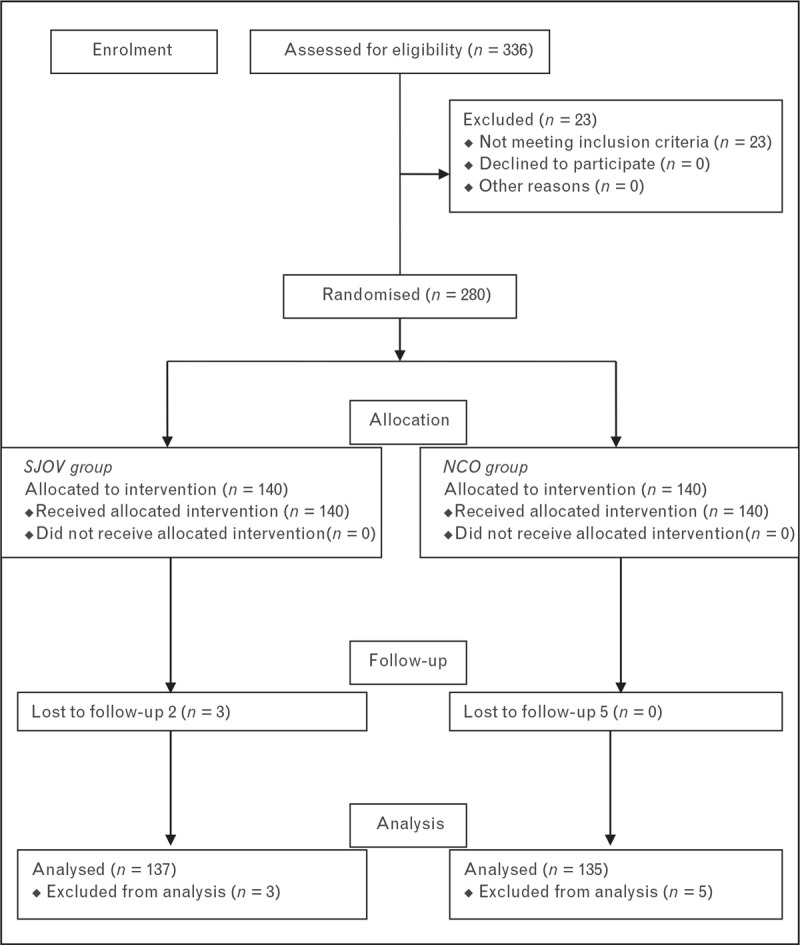
NCO group, nasal cannula supplement oxygen group; SJOV group, supraglottic jet oxygenation and ventilation group.
A satisfaction score using a numerical rating scale (NRS; 0, very dissatisfied; 10, very satisfied) was obtained from the bronchoscopist at the end of the procedure, and from the patients before leaving the bronchoscopy room.
Outcomes were collected by a separate investigator using the World Society of Intravenous Anaesthesia (SIVA) adverse sedation event reporting tool.26 The primary outcome was desaturation, which was defined as SpO2 < 90% during the procedure. Hypoxaemia was described as follows: subclinical respiratory depression (SpO2 90–95%); oxygen desaturation (SpO2 75–89% for ≤60 s); or severe oxygen desaturation (SpO2 < 75% at any time or <90% for >60 s).
The secondary outcomes included other adverse events related to the sedation according to the World SIVA adverse sedation event reporting tool, which included the following:
-
(1)
Minimal risk: nausea/retching, muscle rigidity, myoclonus, hypersalivation, paradoxical response, agitation during recovery, prolonged recovery.
-
(2)
Minor risk: airway obstruction, failed sedation, allergic reaction without anaphylaxis, bradycardia, tachycardia, hypotension, hypertension, seizure.
-
(3)
Sentinel risk: cardiovascular collapse/shock, cardiac arrest/absent pulse.
-
(4)
Adverse events related to SJOV at 1 and 30 min after the procedure, including pneumothorax, subcutaneous emphysema, nose bleeding.
The procedure time, total propofol dose, and bronchoscopist and patient satisfaction scores were recorded. Patients with no adverse events related to SJOV at 30 min after the procedure were followed up by telephone 24 h after the procedure.
When hypoxaemia occurred, it was treated using the following sequence in the NCO group: verbal and tactile stimulation; increasing the oxygen delivery to 10 l min−1; jaw thrust; removing bronchoscope and mask ventilation; tracheal intubation for mechanical ventilation. In the SJOV group, the following sequence was used: verbal and tactile stimulation; increasing the driving pressure to 172 kPa; jaw thrust; removing bronchoscope and mask ventilation; tracheal intubation for mechanical ventilation.
When other adverse events related to the sedation occurred, the interventions were performed to treat the adverse events according to step 3 in the World SIVA adverse sedation event reporting tools. Nose bleeding at 1 min was treated with vasoconstriction by the anaesthesiologist using ephedrine in the nasal cavity. Nasopharyngeal doctors treated the nose bleeding if it happened 30 min after surgery.
Pass (version 11.0, NCSS, LLC, Kaysville, Utah, USA) software was used for sample size calculation. The incidence of hypoxaemia has been reported to be up to 30% during bronchoscopy for patients who were sedated with propofol and remifentanil.5 Assuming that the SJOV via the WNJ would achieve a reduction from 30 to 15% for the incidence of hypoxaemia, we calculated a sample of 121 patients in each group (α = 0.05, power = 0.8). If the attrition rate was set at 15%, a total of 280 patients (140 in each group) would be required.
Data are presented as number (%), or as mean ± SD. The Student's t-test was used to analyse age, height, weight, BMI, baseline SpO2, SpO2 before sedation, the procedure time, propofol dose, patient satisfaction and bronchoscopist satisfaction. The χ2 test was used to analyse sex, ASA physical status, Mallampati class, co-morbidities, procedures and adverse events. P values of < 0.05 were considered statistically significant. Analysis was performed using SPSS version 13.0 (SPSS, Chicago, IL, USA).
Results
Between 1 June and 1 November 2019, 280 patients who underwent flexible bronchoscopy were allocated randomly to one of two groups (the SJOV group or the NCO group). Three patients in the SJOV group and five patients in the NCO group were excluded from analysis in the study because of an inability to follow up due to incorrect phone numbers (Fig. 1). There was no serious morbidity, such as barotrauma (e.g. abnormal gastric distension or pneumothorax) or death.
There were no significant differences between the NCO and SJOV groups in terms of age, sex, body mass index, American Society of Anesthesiologists’ physical status grading, Mallampati class, baseline SpO2, SpO2 before sedation, co-morbidities and type of procedure (Table 1).
Table 1.
Patient characteristics
| Characteristic | NCO group (n = 135) | SJOV group (n = 137) |
| Age, years | 53.4 ± 13.6 | 51.7 ± 13.8 |
| Male sex | 104 (77.0) | 106 (77.3) |
| Height, cm | 165.8 ± 7.0 | 165.7 ± 7.6 |
| Weight, kg | 57.9 ± 9.5 | 58.3 ± 10.3 |
| BMI, kg m−2 | 21.0 ± 2.8 | 21.1 ± 3.1 |
| ASA physical status, 1/2/3 | 29/84/22 | 34/89/14 |
| Mallampati class, 1/2/3/4 | 86/41/6/2 | 80/42/10/5 |
| Baseline SpO2, % | 96.0 ± 1.9 | 96.5 ± 1.6 |
| SpO2 before sedation, % | 99.9 ± 0.30 | 99.9 ± 0.25 |
| Comorbidities | ||
| Hypertension | 41 (30.3) | 46 (33.6) |
| Ischaemic heart disease | 27 (20.0) | 30 (21.9) |
| COPD | 31 (23.0) | 27 (19.7) |
| Asthma | 2 (1.5) | 2 (1.5) |
| Lung malignancy | 36 (26.7) | 39 (28.5) |
| Two or more comorbidities | 28 (20.7) | 27 (19.7) |
| Procedures | ||
| Inspection only | 59 (43.7) | 61 (44.5) |
| Inspection + BAL | 18 (13.3) | 15 (10.9) |
| Inspection + BW | 11 (8.1) | 15 (10.9) |
| Inspection + BB | 47 (34.8) | 46 (33.6) |
Values are mean ± SD or number (%).
ASA, American Society of Anesthesiologists; BAL, broncho-alveolar lavage; BB, bronchial biopsy; BMI, body mass index; BW, bronchial washing; COPD, chronic obstructive pulmonary disease; NCO group, nasal cannula supplemental oxygen group; SJOV group, supraglottic jet oxygenation and ventilation group; SpO2, peripheral oxygen saturation.
The procedure time was shorter in the SJOV group than in the NCO group (12.7 ± 6.2 vs. 15.9 ± 8.9 min, P = 0.001). The bronchoscopists were more satisfied with the sedation procedure in the SJOV group than in the NCO group (9.4 ± 0.8 vs. 9.0 ± 1.2, P = 0.001). However, there were no significant differences in patient satisfaction and propofol dose between groups (Table 2).
Table 2.
Procedure data, propofol dosage and satisfaction
| Characteristic | NCO group (n = 135) | SJOV group (n = 137) | P value |
| Procedure time, min | 15.9 ± 8.9 | 12.7 ± 6.2 | 0.001 |
| Propofol dose, mg | 79.7 ± 23.5 | 75.8 ± 22.3 | 0.135 |
| Patient satisfaction score | 8.0 ± 0.8 | 8.0 ± 0.8 | 0.097 |
| Bronchoscopist satisfaction score | 9.0 ± 1.2 | 9.4 ± 0.8 | 0.000 |
Values are mean ± SD.
NCO group, nasal cannula supplement oxygen group; SJOV group, supraglottic jet oxygenation and ventilation group.
The incidence of desaturation in the SJOV group was lower than in the NCO group (37% vs. 13.1%, P < 0.001). The incidences of subclinical respiratory depression, oxygen desaturation and severe oxygen desaturation were significantly lower in the SJOV group than in the NCO group (P < 0.01). There were no cases of severe oxygen desaturation in the SJOV group, and five in the NCO group (P = 0.023).
In the SJOV group, two patients (1.5%) required an increase in the driving pressure and eight patients (5.8%) required jaw thrust to correct desaturation, which was significantly less than the 14 patients (10.4%) and 19 patients (14.1%), respectively, in the NCO group. Two patients (1.5%) required mask ventilation to correct hypoxaemia in the NCO group, but none in the SJOV group. There was no difference between the two groups in terms of stimulation requirement (Table 3).
Table 3.
Incidence of hypoxaemia and need for airway assistance
| Characteristic | NCO group (n = 135) | SJOV group (n = 137) | P value |
| Hypoxaemia | 50 (37.0) | 18 (13.1) | 0.001 |
| Subclinical respiratory depression | 32 (23.7) | 15 (10.9) | 0.005 |
| Hypoxaemia | 13 (9.6) | 3 (2.2) | 0.009 |
| Severe hypoxaemia | 5 (3.7) | 0 (0) | 0.023 |
| Need for airway assistance | 50 (37.0) | 18 (13.1) | 0.000 |
| Stimulation | 15 (11.1) | 8 (5.8) | 0.118 |
| Increasing oxygen delivery | 14 (10.4) | 0.002 | |
| Increasing driving pressure | 2 (1.5) | ||
| Jaw thrust | 19 (14.1) | 8 (5.8) | 0.023 |
| Mask ventilation | 2 (1.5) | 0 (0) | 0.156 |
Values are number of patients (% of group total).
NCO group, nasal cannula supplement oxygen group; SJOV group, supraglottic jet oxygenation and ventilation group.
In all, 24 (17.8%) patients had minimal risk and 11 (8.1%) patients had minor risk in the NCO group compared with similar numbers of 23 (16.8%) and 12 (8.8%), respectively, in the SJOV group. No patient had sentinel risk in either group (Table 4).
Table 4.
Other adverse events related to the sedation
| Adverse event | NCO group (n = 135) | SJOV group (n = 137) | P |
| Minimal risk | 24 (17.8) | 23 (16.8) | 0.829 |
| Nausea/retching | 10 (7.4) | 8 (5.8) | 0.603 |
| Muscle rigidity, myoclonus | 0 (0) | 0 (0) | – |
| Hypersalivation | 13 (9.6) | 14 (10.2) | 0.871 |
| Paradoxical response | 1 (0.7) | 0 (0) | 0.313 |
| Agitation during recovery | 0 (0) | 1 (0.7) | 0.320 |
| Prolonged recovery | 0 (0) | 0 (0) | – |
| Minor risk | 11 (8.1) | 12 (8.8) | 0.856 |
| Airway obstruction | 0 (0) | 0 (0) | – |
| Failed sedation | 0 (0) | 0 (0) | – |
| Allergic reaction without anaphylaxis | 0 (0) | 0 (0) | – |
| Bradycardia | 0 (0) | 1 (0.7) | 0.320 |
| Tachycardia | 6 (4.4) | 4 (2.9) | 0.504 |
| Hypotension | 3 (2.2) | 5 (3.6) | 0.486 |
| Hypertension | 2 (1.5) | 2 (1.5) | 0.988 |
| Seizure | 0 (0) | (0) | – |
| Sentinel risk | 0 (0) | 0 (0) | – |
| Cardiovascular collapse/shock | 0 (0) | (0) | — |
| Cardiac arrest/absent pulse | 0 (0) | (0) | — |
Values are number (% of group total).
NCO group, nasal cannula supplement oxygen group; SJOV group, supraglottic jet oxygenation and ventilation group.
One minute after waking up, 18 (13.1%) patients in the SJOV group had a dry mouth, which was significantly higher than the two (1.5%) in the NCO group. There were no significant differences in sore throat or nasal bleeding between the groups. No patients had severe barotrauma such as subcutaneous emphysema in either group.
Thirty minutes after waking up, dry mouth was significantly lower in the SJOV group than at 1 min and there was none in the NCO group. Nasal bleeding stopped naturally, without the need for medical or surgical treatment. However, the number of patients with sore throat had increased in both groups but there was no difference between the groups.
At 24 h after the procedure, dry mouth had disappeared in the SJOV group, without any medical interventions. Sore throat was also relieved, although not completely (Table 5).
Table 5.
Adverse events related to oxygen delivery system
| Adverse event | NCO group (n = 135) | SJOV group (n = 137) | P |
| 1 min after procedure | 24 (17.8) | 40 (29.2) | 0.026 |
| sore throat | 3 (2.2) | 6 (4.4) | 0.320 |
| subcutaneous emphysema | 0 (0) | 0 (0) | – |
| nasal bleeding | 19 (14.1) | 16 (11.7) | 0.555 |
| dry mouth | 2 (1.5) | 18 (13.1) | 0.001 |
| 30 min after procedure | 12 (8.9) | 20 (14.6) | 0.132 |
| sore throat | 12 (8.9) | 18 (13.1) | 0.246 |
| subcutaneous emphysema | 0 (0) | 0 (0) | – |
| nasal bleeding | 0 (0) | 0 (0) | – |
| dry mouth | 0 (0) | 2 (1.5) | 0.159 |
| 24 h after procedure | 1 (0.7) | 2 (1.5) | 0.570 |
| sore throat | 1 (0.7) | 2 (1.5) | 0.570 |
| dry mouth | 0 (0) | 0 (0) | – |
Values are number (% of group total).
NCO group, nasal cannula supplement oxygen group; SJOV group, supraglottic jet oxygenation and ventilation group.
Discussion
Our study shows that the SJOV is a novel and efficient method to decrease the incidence of desaturation in patients receiving flexible bronchoscopy under moderate to deep sedation in comparison with the commonly used oxygen supply via a regular nasal cannula. There were some minor and tolerable adverse events related to SJOV but no severe complications such as barotrauma in any patient.
Studies have shown that OSA is associated with a high risk of traffic accidents and cardiovascular disease.27–29 The STOP-BANG questionnaire is a concise and convenient screening tool for pre-operative OSA and has a high sensitivity in detecting OSA.24 Chung et al. reported that patients with a STOP-BANG score of 0 to 2 can be classified as low risk for moderate to severe OSA.30 Consequently, OSA patients (STOP-BANG ≥ 3) were excluded in this study for the safety of patients. The present study indicates that SJOV is feasible and effective in reducing the incidence of hypoxaemia during flexible bronchoscopy under moderate to deep sedation. The incidence of hypoxaemia was 37% when nasal cannula supplemental oxygen was used, which was reduced to 13% with SJOV. The procedure was seldom interrupted in the SJOV group. Previous studies have suggested that SJOV was effective in maintaining oxygenation/ventilation in obese patients under sedation or general anaesthesia in various types of difficult airway management.16–19 In the process of flexible bronchoscopy, jet pulses can be injected into the trachea and lung around the flexible bronchoscope, even after it passes the vocal cords, thus maintaining adequate oxygenation and ventilation. However, nasal cannula supplemental oxygen has a much lower efficiency in maintaining oxygenation and ventilation in patients with severe respiratory depression or apnoea under heavy sedation, especially when a flexible bronchoscope is already in the airway, due to the lack of forward injecting power.
Capnography should be used in all patients undergoing procedural sedation by facilitating early detection of ventilation problems,31,32 which may give earlier indications of respiratory suppression or apnoea than pulse oximetry. The end-tidal partial pressure of carbon dioxide (PETCO2) monitoring catheter built inside the wall of the WNJ is extremely important, and opens inside the inner lumen of the WNJ at the middle position. The intermittent powerful jet pulses are able to reduce CO2 washout and CO2 dilution33 from the jet flow, and provide acute measurement of PETCO2, as demonstrated by previous studies.23,34–36 Respiratory depression or apnoea can be detected effectively, while simultaneously monitoring the effectiveness of SJOV during moderate-to-deep sedation. Additional airway assistance may be provided to prevent the occurrence of hypoxaemia and accumulation of CO2 during SJOV.
The adverse events related to SJOV were considered when beginning the study. Barotrauma is a severe adverse event in the process of jet ventilation. Duggan et al.37 reported that during transtracheal jet ventilation (TTJV), there was a high incidence of barotrauma, up to 30%. Barotrauma can occur when jet ventilation is used in a closed tissue cavity.38 Significantly different from TTJV, which has the jet pulse initiated below the vocal cords, SJOV has jet pulses generated above the vocal cords, securing a patent upper airway because of nose and mouth opening and minimising the risks of barotrauma.
The incidence of dry mouth was higher after SJOV because oxygenation without humidification was used in the manual jet ventilator. Studies indicate that breathing dry air for a long time interrupts the tracheal secretion of mucus and may result in acute damage and inflammation.17 However, the presence of a dry mouth was transient. The presence of sore throat increased after 30 min in both groups, possibly because of the termination of the analgesic effects of lidocaine and remifentanil. This indicates that the sore throat was due mainly to the stimulation of the throat caused by flexible bronchoscopy rather than jet ventilation.
Another potential risk of inserting the WNJ or flexible bronchoscope into a nostril is that of nasal bleeding.21,22,39 Nasal bleeding occurred in both groups, but there was no significant difference between groups at the end of the procedure. All nasal bleeding stopped after 30 min.
The study had the following limitations. First, the study is a single-blinded protocol; the investigator was not blinded, which might produce bias in this study. Second, the depth of sedation using the OAA/S was a subjective estimation, and any additional boluses of propofol might add deviation. Bispectral index score (BIS) monitoring could potentially eliminate this deviation. Studies40,41 have indicated that moderate sedation during flexible fibreoptic bronchoscopy using BIS monitoring can be used safely by non-anaesthesiologists with propofol but have not reduced hypoxaemic events.
In summary, during moderate to deep sedation with propofol and remifentanil for flexible bronchoscopy, SJOV via the WNJ can reduce the incidence of desaturation and can increase bronchoscopist satisfaction, compared with the commonly used supplemental oxygen via a nasal cannula. Transient and mild adverse events related to the SJOV are dry mouth and sore throat, but without serious complications such as barotrauma.
Acknowledgements relating to this article
Assistance with the study: we thank Rachel Mund for English wording, grammar review and editing.
Financial support and sponsorship: none.
Conflicts of interest: Huafeng Wei is the inventor of the WNJ used in this study and is a consultant to the Well Lead Medical Company, China. The other authors have no conflicts of interest.
Presentation: an abstract summarising this study was presented at the World Airway Management Meeting (WAMM2019) in 2019 in Amsterdam, the Netherlands.
Footnotes
Published online 25 November 2020
References
- 1.American Thoracic Society. Flexible bronchoscopy. Am J Respir Crit Care Med 2015; 191:7–8. [Google Scholar]
- 2.Maguire GP, Rubinfeld AR, Trembath PW, et al. Patients prefer sedation for fibreoptic bronchoscopy. Respirology 1998; 3:81–85. [DOI] [PubMed] [Google Scholar]
- 3.Putinati S, Ballerin L, Corbetta L, et al. Patient satisfaction with conscious sedation for bronchoscopy. Chest 1999; 115:1437–1440. [DOI] [PubMed] [Google Scholar]
- 4.McCambridge AJ, Boesch RP, Mullon JJ. Sedation in bronchoscopy: a review. Clin Chest Med 2018; 39:65–77. [DOI] [PubMed] [Google Scholar]
- 5.Ryu JH, Lee SW, Lee J, et al. Randomized double-blind study of remifentanil and dexmedetomidine for flexible bronchoscopy. Br J Anaesth 2012; 108:503–511. [DOI] [PubMed] [Google Scholar]
- 6.Fruchter O, Tirosh M, Carmi U, et al. Prospective randomized trial of bispectral index monitoring of sedation depth during flexible bronchoscopy. Respiration 2014; 87:388–393. [DOI] [PubMed] [Google Scholar]
- 7.Lin H, Chen W, Yao W, et al. Clinical application of the modified laryngeal mask airway for endobronchial ultrasound-guided transbronchial needle aspiration biopsy. Zhonghua Yi Xue Za Zhi 2014; 94:651–654. [PubMed] [Google Scholar]
- 8.Douglas N, Ng I, Nazeem, et al. A randomized controlled trial comparing high-flow nasal oxygen with standard management for conscious during bronchoscopy. Anaesthesia 2018; 73:169–176. [DOI] [PubMed] [Google Scholar]
- 9.Yserbyt J, De Maeyer N, Dooms C, et al. The feasibility of tracheal oxygen supplementation during flexible bronchoscopy. Respiration 2016; 92:48–52. [DOI] [PubMed] [Google Scholar]
- 10.Christopher KL, Schwartz MD. Transtracheal oxygen therapy. Chest 2011; 139:435–440. [DOI] [PubMed] [Google Scholar]
- 11.Kampelmacher MJ, Deenstra M, van Kesteren RG, et al. Transtracheal oxygen therapy: an effective and safe alternative to nasal oxygen administration. Eur Respir J 1997; 10:828–833. [PubMed] [Google Scholar]
- 12.Lo Y-L, Lin T-Y, Fang Y-F, et al. Feasibility of bispectral index-guided propofol infusion for flexible bronchoscopy sedation: a randomized controlled trial. PLoS One 2011; 6:e27769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rajan S, Joseph N, Tosh P, et al. Effectiveness of transnasal humidified rapid insufflation ventilatory exchange versus traditional preoxygenation followed by apnoeic oxygenation in delaying desaturation during apnoea: a preliminary study. Indian J Anaesth 2018; 62:202–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gustafsson IM, Lodenius Å, Tunelli J, et al. Apnoeic oxygenation in adults under general anaesthesia using Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE) – a physiological study. Br J Anaesth 2017; 118:610–617. [DOI] [PubMed] [Google Scholar]
- 15.Wei H. A new tracheal tube and methods to facilitate ventilation and placement in emergency airway management. Resuscitation 2006; 70:438–444. [DOI] [PubMed] [Google Scholar]
- 16.Dziewit JA, Wei H. Supraglottic jet ventilation assists intubation in a Marfan's syndrome patient with a difficult airway. J Clin Anesth 2011; 23:407–409. [DOI] [PubMed] [Google Scholar]
- 17.Li Q, Xie P, Zha B, et al. Supraglottic jet oxygenation and ventilation saved a patient with ‘cannot intubate and cannot ventilate’ emergency difficult airway. J Anesth 2017; 31:144–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peng J, Ye J, Zhao Y, et al. Supraglottic jet ventilation in difficult airway management. J Emerg Med 2012; 43:382–390. [DOI] [PubMed] [Google Scholar]
- 19.Levitt C, Wei H. Supraglottic pulsatile jet oxygenation and ventilation during deep propofol sedation for upper gastrointestinal endoscopy in a morbidly obese patient. J Clin Anesth 2014; 26:157–159. [DOI] [PubMed] [Google Scholar]
- 20.Yang ZY, Meng Q, Xu YH, et al. Supraglottic jet oxygenation and ventilation during colonoscopy under monitored anesthesia care: a controlled randomized clinical trial. Eur Rev Med Pharmacol Sci 2016; 20:1168–1173. [PubMed] [Google Scholar]
- 21.Qin Y, Li LZ, Zhang XQ, et al. Supraglottic jet oxygenation and ventilation enhances oxygenation during upper gastrointestinal endoscopy in patients sedated with propofol: a randomized multicentre clinical trial. Br J Anaesth 2017; 119:158–166. [DOI] [PubMed] [Google Scholar]
- 22.Shao LJ, Liu SH, Liu FK, et al. Comparison of two supplement oxygen methods during gastroscopy with intravenous propofol anesthesia in obese patients: study protocol for a randomized controlled trial. Trials 2018; 19:602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu C, Wei J, Cen Q, et al. Supraglottic jet oxygenation and ventilation-assisted fibre-optic bronchoscope intubation in patients with difficult airways. Intern Emerg Med 2017; 12:667–673. [DOI] [PubMed] [Google Scholar]
- 24.Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology 2008; 108:812–821. [DOI] [PubMed] [Google Scholar]
- 25.Chernik DA, Gillings D, Laine H, et al. Validity and reliability of the Observer's Assessment of Alertness/Sedation Scale: study with intravenous midazolam. J Clin Psychopharmacol 1990; 10:244–251. [PubMed] [Google Scholar]
- 26.Mason KP, Green SM, Piacevoli Q. Adverse event reporting tool to standardize the reporting and tracking of adverse events during procedural sedation: a consensus document from the World SIVA International Sedation Task Force. Br J Anaesth 2012; 108:13–20. [DOI] [PubMed] [Google Scholar]
- 27.Turkington PM, Sircar M, Allgar V, et al. Relationship between obstructive sleep apnoea, driving simulator performance, and risk of road traffic accidents. Thorax 2001; 56:800–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shahar E, Whitney CW, Redline S, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the sleep heart health study. Am J Respir Crit Care Med 2001; 163:19–25. [DOI] [PubMed] [Google Scholar]
- 29.Petrini F, Di Giacinto I, Cataldo R, et al. Perioperative and periprocedural airway management and respiratory safety for the obese patient: 2016 SIAARTI Consensus. Minerva Anestesiol 2016; 82:1314–1335. [PubMed] [Google Scholar]
- 30.Chung F, Abdullah HR, Liao P, et al. A practical approach to screen for obstructive sleep apnea. Chest 2016; 149:631–638. [DOI] [PubMed] [Google Scholar]
- 31.Hinkelbein J, Lamperti M, Akeson J, et al. European Society of Anaesthesiology and European Board of Anaesthesiology guidelines for procedural sedation and analgesia in adults. Eur J Anaesthesiol 2018; 35:6–24. [DOI] [PubMed] [Google Scholar]
- 32.Conway A, Douglas C, Sutherland JR. A systematic review of capnography for sedation. Anaesthesia 2016; 71:450–454. [DOI] [PubMed] [Google Scholar]
- 33.Sorbello M, Pulvirenti GS, Pluchino D, et al. State of the art in airway management during g.i. endoscopy: the missing pieces. Dig Dis Sci 2017; 62:1385–1387. [DOI] [PubMed] [Google Scholar]
- 34.Gupta S. Supraglottic jet oxygenation and ventilation - a novel ventilation technique. Indian J Anaesth 2020; 64:11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liang H, Hou Y, Sun L, et al. Supraglottic jet oxygenation and ventilation for obese patients under intravenous anesthesia during hysteroscopy: a randomized controlled clinical trial. BMC Anesthesiol 2019; 19:151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liang H, Hou Y, Wei H, et al. Supraglottic jet oxygenation and ventilation assisted fiberoptic intubation in a paralyzed patient with morbid obesity and obstructive sleep apnea: a case report. BMC Anesthesiol 2019; 19:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Duggan LV, Ballantyne Scott B, Law JA, et al. Transtracheal jet ventilation in the ’can’t intubate can’t oxygenate’ emergency: a systematic review. Br J Anaesth 2016; 117: Suppl 1: i28–i38. [DOI] [PubMed] [Google Scholar]
- 38.Craft TM, Chambers PH, Ward ME, et al. Two cases of barotraumas associated with transtracheal jet ventilation. Br J Anaesth 1990; 64:524–527. [DOI] [PubMed] [Google Scholar]
- 39.Mehta AC, Dweik RA. Nasal versus oral insertion of the bronchoscope: advantages and disadvantages. J Bronchol 1996; 3:224–228. [Google Scholar]
- 40.Clark G, Licker M, Younossian AB, et al. Titrated sedation with propofol or midazolam for flexible bronchoscopy: a randomized trial. Eur Respir J 2009; 34:1277–1283. [DOI] [PubMed] [Google Scholar]
- 41.Lo YL, Lin TY, Fang YF, et al. Feasibility of bispectral index-guided propofol infusion for flexible bronchoscopy sedation: a randomized controlled trial. PloS One 2011; 6:e27769. [DOI] [PMC free article] [PubMed] [Google Scholar]


