Abstract
Healthcare waste comprises the waste generated by healthcare facilities, medical laboratories and biomedical research facilities. Improper treatment of this waste poses serious risks of disease transmission to waste pickers, waste workers, health workers, patients, and the community in general through exposure to infectious agents. Poor management of the waste emits harmful and deleterious contaminants into society. However, contamination of highly contagious agents such as the COVID-19 virus has created enormous instability in healthcare waste handling and subsequent recycling because of the volume of the waste generated and its contagious nature. Several countries have adopted safety measures to combat this contamination and manage healthcare waste; however, these measures are insufficient and vary depending on the context of the country. In addition, the WHO has set out guidelines for management of healthcare waste. These guidelines are helping to manage the highly contagious healthcare waste resulting from the current pandemic. Proper healthcare waste management may add value by reducing the spread of the COVID-19 virus and increasing the recyclability of materials instead of sending them to landfill. Disinfecting and sorting out healthcare waste facilitates sustainable management and allows their utilization for valuable purposes. This review discusses the different healthcare solid waste management strategies practiced in different countries, the challenges faced during this management, and the possible solutions for overcoming these challenges. It also provides useful insights into healthcare solid waste management scenarios during the COVID-19 pandemic and a possible way forward.
Keywords: Healthcare solid waste, COVID-19, Healthcare waste management, Challenges, Solutions
Graphical abstract
1. Introduction
After radiation waste, healthcare waste is considered the second most hazardous waste globally. It includes various forms of waste, both hazardous and non-hazardous, such as sharps, human body parts, blood, chemical waste, pharmaceutical waste, and medical devices (Rodriguez-Morales, 2013). All of this waste is produced mainly by hospitals, primary care facilities, laboratories, mortuaries, autopsy centers, laboratories, blood banks, nursing homes, and other medical locations (Pepin et al., 2014). It is generated during diagnosis, treatment, immunization of humans or animals, research, or the production or testing of biologicals. If not properly handled, it can have devastating effects on human health (Johannessen et al., 2000). During any infectious disease outbreak, the waste generated from healthcare facilities increases exponentially; as a result, special care must be taken by management in order to avoid troubling impacts (Ramteke and Sahu, 2020).
The outbreak of coronavirus disease 2019 (COVID-19) has arisen from the SARS-CoV-2 virus, which causes an acute respiratory disease (Mol and Caldas, 2020; WHO, 2019; WHO, 2020b); it was first reported in Wuhan, China (Wang et al., 2020) in December 2019. It has been acknowledged as a Public Health Emergency of International Concern (PHEIC) (Wilder-Smith and Osman, 2020), and the virus has spread to almost all countries across the globe. The pandemic continues to be a significant public health threat worldwide. The rapid increase in the number of COVID-19 infected patients and the highly transmissible nature of the disease have led to a high number of hospitalizations. Thus, the generation of healthcare solid waste has rapidly increased. Additionally, the increase in the amount of personal protective equipment (PPE) used during the COVID-19 pandemic, compared to normal circumstances, has further contributed towards the increase in healthcare solid waste (Haji et al., 2020; Wei and Manyu, 2020; WHO, 2020b). Thus, it has become necessary to increase the handling capacity for healthcare waste (WHO, 2020b), since improper management of the waste may cause further spread of the virus.
Worldwide, at least 5.2 million people, including 4 million children, die each year from diseases originating from unmanaged medical waste (Star, 2020). Considering the global transmission of COVID-19, excessive biomedical waste has become a new major threat to public health as well as to the environment during this pandemic. Exposure to waste can easily infect waste management workers; thus, the necessary protective gear must be worn by these workers as well as by other front line workers, i.e. doctors and nurses (ISWA-Jordan, 2020). The solid waste (i.e. sharps, PPE, and pathological waste) generated by COVID-19 positive patients and the doctors and nurses who treat them should be considered infectious waste. The situation necessitates installation of appropriate collection mechanisms for infectious waste, with trained workers using special containers (marked, lined, and sharp-safe boxes), and subsequent in situ treatment prior to any movement (WHO, 2020b). According to Ilyas et al. (2020) and ISWA-Lebanon (2020), techniques such as using disinfectant and storing the waste for nine days have been employed in order to disinfect waste (Ilyas et al., 2020; ISWA-Lebanon, 2020); this could reduce the risk of further infection from COVID-19. The solid waste generated from the waiting areas of healthcare facilities should be considered non-hazardous waste and kept in prescribed bags or containers, sealed before movement, and disposed of properly by waste management workers. Alternative technologies, i.e. autoclaves and incinerators with high temperature burners, have been used for managing healthcare solid waste in a sustainable way (WHO, 2020b). During this pandemic, different countries have adopted different measures for handling healthcare solid waste, while the WHO has formulated special guidelines to manage it.
However, there is no single document that contains all the management strategies for healthcare waste adopted by different countries during the COVID-19 outbreak. Therefore, this review investigates the healthcare solid waste management strategies and practices in different countries, along with the WHO guidelines. The review also makes an attempt to explore the challenges in managing COVID-19-related healthcare solid waste in these countries. In addition, the review addresses possible solutions for dealing with this waste in the fast-evolving situation of the COVID-19 pandemic.
2. Methods used to conduct the mini-review
In order to accomplish the objective of this review, we searched the literatures in the scholar sites including Scopus and Web of Science. The search keywords are ‘healthcare waste’, ‘COVID-19’, ‘pandemic’, ‘novel corona’, ‘SARS-CoV-2’, ‘types of healthcare waste’, and ‘healthcare waste management’. Obtained literatures were further screened with respect to the languages and only articles in English language were selected for this review. Finally, the selected articles were analyzed in relation to the selected key words.
3. Composition of healthcare waste
Generally, the waste generated from healthcare facilities, research centers, and laboratories relating to medical procedures is considered healthcare waste. Approximately 75–90% of healthcare solid waste is similar to waste produced in households, and is thus categorized as ‘non-hazardous’ or ‘general healthcare’ waste. In reality, this waste is generated from the administrative, kitchen, and housekeeping functions of medical and healthcare facilities. The remaining 10–25% of waste is designated ‘hazardous waste’, which poses serious environmental and health risks (Yves Chartier et al., 2014). It has been observed that the composition of healthcare solid waste during the COVID-19 pandemic is more or less similar to that produced in normal circumstances, except for the generation of a huge quantity of plastics/micro-plastics. However, the pandemic has seen the generation of a vastly increased quantity of waste (Singh et al., 2020a). As observed during normal circumstances, the composition of healthcare solid waste is very important, as this dictates its ability to be recycled and sustainably managed, which is vital during the current pandemic.
3.1. Hazardous healthcare waste
3.1.1. Chemical waste
Chemicals are omnipresent in healthcare facilities. As major consumers of chemicals, the chemical waste these facilities generate can have deleterious impacts on health and the environment. This type of waste accounts for about 3% of waste originating from healthcare activities (Ilyas et al., 2020). Waste that contains chemical substances, i.e. laboratory reagents, film developing reagents, expired/unused disinfectants, solvents, and waste containing heavy metals (batteries, broken thermometers, blood-pressure gauges, etc.) is considered chemical healthcare waste (Yves Chartier et al., 2014). Due to serious health concerns, a growing number of hospitals have substituted some of their most hazardous substances with safer alternatives and adopted careful management strategies. However, there are plenty of facilities in both developing and developed countries that still use these toxic chemicals and have poor chemical waste management strategies.
3.1.2. Infectious waste
Waste that contains infective pathogens, resulting in disease incidence and progression, is defined as infectious healthcare waste; it comprises materials contaminated with blood and body fluids, human excreta, laboratory cultures, and microbiological products (Askarian et al., 2010; Yves Chartier et al., 2014). PPE, i.e. boots, long-sleeved gowns, heavy-duty gloves, masks, goggles, and face shields are also considered infectious waste, and waste generated from these materials has increased by a substantial amount during the COVID-19 pandemic (WHO, 2020b). Therefore, there is a tremendous challenge in managing this type of waste during the pandemic (Rowan and Laffey, 2021).
3.1.3. Pathological waste
Pathological waste is typically a smaller portion, part, or slice of any tissue, organ, or body part, taken from surgical or microbiological specimens from animal or human bodies (Yves Chartier et al., 2014). This type of waste originates from tissues or samples of tissues that are inspected and/or examined in a laboratory to diagnose or study abnormality or diseased tissues. In essence, this type of waste is similar to infectious waste, and careful handling is required to manage it during the current pandemic. It can spread infection in a similar fashion to infectious waste because of the presence of infective viral particles in the tissue samples (WHO, 2020b).
3.1.4. Radioactive waste
Radioactive waste is a by-product of various nuclear technologies used in healthcare facilities, including nuclear medicine, radiotherapy, and reagents for research. This waste contains radioactive substances, i.e. unused liquids from radiotherapy or laboratory research. Radioactive contaminated glassware, packages/absorbent paper, urine, and excreta from patients treated or tested with unsealed radionuclides also constitute radioactive waste (Yves Chartier et al., 2014). Exposure to radioactive elements can cause serious health problems and also poses a risk to the environment if not managed properly. The outbreak of the COVID-19 pandemic has compromised the containment of radioactive waste, and special measures need to be put in place to manage this toxic waste so that its exposure to humans and the environment can be minimized.
3.1.5. Sharps waste
Sharps waste is another type of healthcare solid waste; it is composed of used ‘sharps’ including used or unused hypodermic, intravenous, or other needles, auto-disable syringes, syringes with attached needles, infusion sets, scalpels, pipettes, knives, blades, and broken glasses (Askarian et al., 2010; Kalogiannidou et al., 2018; Mato and Kassenga, 1997; Yves Chartier et al., 2014). Generated sharps healthcare waste should be treated with extra care and properly managed during the COVID-19 pandemic (WHO, 2020b), as it has been found that SARS-CoV-2 can survive on different surfaces for a certain period. Waste workers could be easily infected by sharps contaminated with the virus, and this could increase community transmission.
3.1.6. Pharmaceutical waste
Pharmaceutical waste can be generated from many activities and locations in healthcare facilities, i.e. pharmacies, distribution centers, and hospitals. Expired and contaminated pharmaceutical products are considered pharmaceutical waste (Yves Chartier et al., 2014). Used biological products for therapy and transdermal patches, and contaminated pharmaceuticals including vaccines, are also listed as pharmaceutical waste (Malsparo, 2020). The amount of pharmaceutical waste has increased substantially during the COVID-19 pandemic due to the increased number of hospital admissions. Waste workers who collect this type of waste from pharmacies, distribution centers, and hospitals can easily be infected with SARS-CoV-2 if they come into contact with COVID-19 patients and virally contaminated pharmaceutical waste during its collection from designated treatment units.
3.2. Non-hazardous healthcare waste
Used plastic water bottles, office paper, magazines, newspapers, food waste, and food packaging are considered non-hazardous healthcare solid waste (Askarian et al., 2010; Kalogiannidou et al., 2018) if not contained alongside hazardous waste. Non-hazardous waste is comparable to domestic waste and can be recycled for sustainable waste management. It is probable that both asymptomatic and symptomatic COVID-19 patents generate a huge amount of non-hazardous SARS-CoV-2 contaminated healthcare waste during their daily actions in healthcare facilities, which poses a serious risk of community transmission.
3.3. Other waste
The test kits and waste generated from different diagnostic methods for COVID-19 are another additional type of healthcare waste that has been generated in substantial amounts during the COVID-19 outbreak, as global transmission and prevalence have necessitated the detection of infections to aid with appropriate social distancing and quarantine measures. The use of rapid test kits for identifying an infected person produces additional waste in the waste stream, as each kit is used only once. There is always a chance that this waste could be contaminated with SARS-CoV-2 and contribute to further spread if not managed properly.
4. Persistence rate of COVID-19 virus and its possible transmission through healthcare solid waste
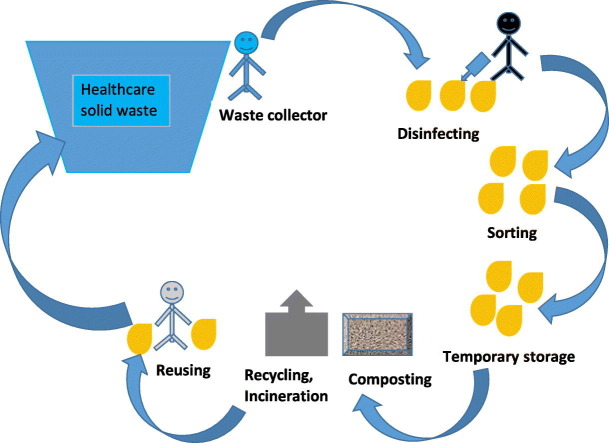
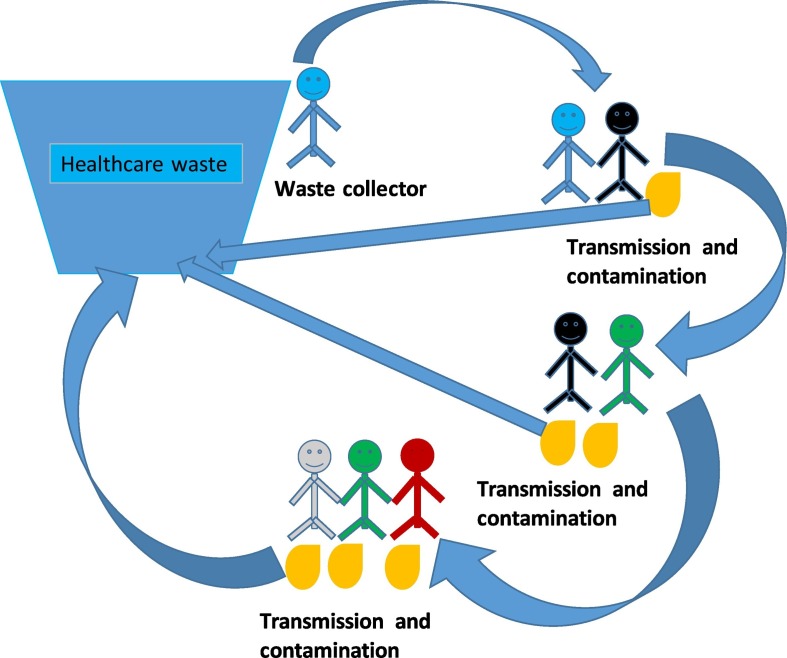
The transmission of COVID-19 virus occurs through sneezing, coughing, contact with touched objects, and physical contact (ISWA-Netherlands, 2020). Information about the survival period of the COVID-19 virus on different substrates is very important for formulating appropriate management practices and measures for dealing with healthcare solid waste. The survival period of SARS-CoV-2 varies from a few hours to a few days, based on the substrate type and the environmental conditions. The survival periods of the COVID-19 virus following aerosolization on copper, cardboard, plastic, and stainless steel are 3 h, 4 h, 24 h, and 2–3 days respectively (van Doremalen et al., 2020). Other researchers have reported that the virus can also survive on inanimate surfaces, i.e. metal, glass, or plastic, for a period of 9 days (Kampf et al., 2020). It can persist in dechlorinated tap water and hospital waste water at 20 °C for 2 days (Wang et al., 2005). The longer survival period of this novel COVID-19 virus poses an increased risk of community transmission. Improper management of solid waste generated from healthcare facilities can increase the spread of the COVID-19 virus (Nzediegwu and Chang, 2020; Ramteke and Sahu, 2020; Sharma et al., 2020; Yang et al., 2020). Waste pickers are directly exposed to contaminated waste and are susceptible to infection as a result. Thus, they can unintentionally transmit the virus within their community. The transmission pathway of this novel virus is presented in Fig. 1 .
Fig. 1.
Transmission of COVID-19 virus through healthcare waste.
5. Waste management strategies during the COVID-19 pandemic
A healthcare waste management strategy refers to a facility's program for managing generated waste for disposal. It usually addresses: (1) compliance with regulations; (2) responsibilities of staff members; (3) definitions/classification of healthcare waste; (4) specific procedures for handling healthcare waste; and (5) training of related workers. Different countries have adopted different strategies in response to the management of the huge and infectious amount of waste produced during the COVID-19 pandemic.
In response to the pandemic, healthcare waste management strategies should include several additional measures in order to ensure appropriate containment for avoiding infection. Different countries have adopted the best possible management approaches based on their capacity, resources, and commitment (Singh et al., 2020b; Zand and Heir, 2020c). Different organizations have offered guidelines for managing healthcare waste in a way that follows safety measurements and is sustainable (WHO, 2020a). According to the guidelines provided by various member states of the European Union (EU), healthcare solid waste generated during the COVID-19 pandemic is considered infectious waste, and the capacity to manage this waste should be increased. There should be suitable facilities for temporary storage of the waste if there are any issues relating to incineration or disposal capacity. The waste should be stored in sealed containers located in protected areas that only authorized personnel are allowed to enter. Disinfectant should be used on outer and inner surfaces in order to avoid possible transmission of the virus. All workers working in the area should follow proper safety measures (Cremonesi et al., 2020; Waste-Mangement, 2020).
During the COVID-19 epidemic in Hubei, China, infected healthcare solid waste has been segregated and packed by waste handling employees in hospitals. They disinfect the waste using 0.5% chlorine solution and pack it in double bags prior to placing it in temporary healthcare storage within the hospitals. The method of disposal of healthcare waste depends on the particular hospital and its waste management facilities. Sterilization by autoclave or irradiation has been used before disposing of the segment of waste in a licensed landfill. In some hospitals, incineration on-site or in a special remote area has been used to dispose of the healthcare waste. Mobile incineration or autoclave systems have been provided to support the extra healthcare waste generated during the outbreak. Cement kilns and other industrial furnaces have been considered as alternative facilities for disposing of healthcare waste. Additional healthcare waste has been temporarily stored in selected areas that has been secured and isolated. Only designated vehicles have been used for transporting healthcare solid waste, and data have been recorded properly. Load areas have been locked, disinfected, and separated from drivers in order to avoid risk of infection (ADB, 2020).
As per the guidelines of the CDC (Centers for Disease Control and Prevention), in the United States of America (USA), healthcare waste generated by COVID-19 patients is considered the same as waste generated by other patients. Thus, the waste has been treated as regular healthcare waste and does not require any additional special treatment (Commendatore, 2020).
The Philippines has made a special amendment for handling healthcare waste during the COVID-19 pandemic. There are special registered transporters and treatment, storage, and disposal (TSD) facilities for handling healthcare waste and disposing of it on the island of Luzon. There is a special permit in place to collect pathological and infectious healthcare waste for smooth handling. Each registered transporter is required to pass through a special checkpoint, and to provide the following online documents: an official request letter; a transporter and TSD registration certificate; a transport management plan; a transportation route; a schedule; and an agreement between the healthcare waste generator, the transporter, and the treatment workers. Each vehicle used for transporting the waste has the following special markings: name and ID of transport; placard; waste class; and waste number. These are readable from 15 m' distance from the vehicle. The registered transporter is required to submit a compliance and completion report of transportation, attested by a representative from the healthcare and TSD department (EMB, 2020).
In Jordan, healthcare waste management during the current pandemic has been carried out following three main principles: reduction of unnecessary healthcare waste; isolation of regular waste from hazardous waste; and proper treatment in order to reduce risks to health workers and society. Personnel dealing with COVID-19 contaminated healthcare waste are required to use PPE, i.e. ultra-filtered masks (Nano) and fluid protective long-sleeved clothes, along with a cap, shoes, elastic leather gloves, protective glasses, and a full-face protector. The respective authorities closely supervise the work in order to ensure that local rules and regulations, i.e. new guidelines for cleaning and disinfection around COVID-19, are followed strictly. Waste originating from COVID-19 patients is rapidly disposed of on a daily basis. Temporary and permanent storage areas, containers, and healthcare waste bags are sanitized to prevent the spread of the virus (ISWA-Jordan, 2020).
In all adopted strategies, healthcare waste is required to be managed on a frequent basis during the pandemic. The waste needs to be collected, separated, and stored with special identification labels; it should then be treated, transported, and disposed of properly. Personal protection, disinfection, and training should be considered necessary for proper management of healthcare waste (UN, 2020). Waste from confirmed COVID-19 patients, i.e. infectious waste, sharps, and pathological waste should be collected with safety measures and kept in special bags with proper markings. Healthcare waste collectors should use PPE, i.e. boots, long-sleeved gowns, heavy-duty gloves, masks, goggles, and face shields, and they should wash their hands with sanitizer or disinfectant after disposing of the waste (WHO, 2020b).
Considering the above-mentioned examples, it is clear that strategies are not similar in all countries. As the COVID-19 pandemic has heightened and hospitals have become overburdened with COVID-19 patents, infected people have needed medical attention in households. There are no management strategies for healthcare waste generated from households. A unique management strategy is important in this situation, although the economic condition of a country influences its management of healthcare solid waste. Nevertheless, development of suitable management is crucial in the current situation. Recyclability and reduction of landfill should also be considered to aid sustainable management of healthcare solid waste during and after the COVID-19 pandemic.
6. Challenges
Healthcare solid waste is hazardous to health and the environment (Ansari et al., 2019; Rahman et al., 2020). Doctors and nurses have a higher risk of infection (Ferreira and Teixeira, 2010; ISWA-Jordan, 2020). Water is contaminated near landfills containing healthcare waste (Ramteke and Sahu, 2020; Ubuoh et al., 2019).
The COVID-19 pandemic has put tremendous pressure on existing waste management systems, which is exemplified by the increase of waste accumulation in Hubei province, China (Wei and Manyu, 2020). A COVID-19 patient can generate around 3.4 kg of healthcare waste per day (ADB, 2020). Thus, healthcare waste has gradually increased in quantity during the pandemic (Mingyu, 2020). In Hubei, healthcare waste has increased by 600% from 40 to 240 tons, which has overwhelmed the existing transport and disposal infrastructure. Other countries are facing similar challenges in terms of dealing with the huge amount of waste (ADB, 2020); this trend has been observed in France, Italy, and the Netherlands. Healthcare solid waste in France and the Netherlands has increased from 40% to 50% and 45% to 50%, respectively (Wei and Manyu, 2020). The trend has also been observed in India (Ramteke and Sahu, 2020) and Iran (Zand and Heir, 2020a, Zand and Heir, 2020b, Zand and Heir, 2020c). Used PPE and general waste, i.e. food and dining boxes and infusion bottles and bags used by nurses, have seen a tremendous increase in quantity during the COVID-19 pandemic (Wei and Manyu, 2020). In Europe, governments are facing challenges in retaining waste management staff, maintaining a safe environment for workers, handling household waste produced by patients at home, and creating space for extra waste produced by the pandemic (Waste-Mangement, 2020). Landfill containing healthcare solid waste generated during the pandemic can contaminate water. The cost of the healthcare sector has also increased during the pandemic.
7. Potential for healthcare solid waste management strategies
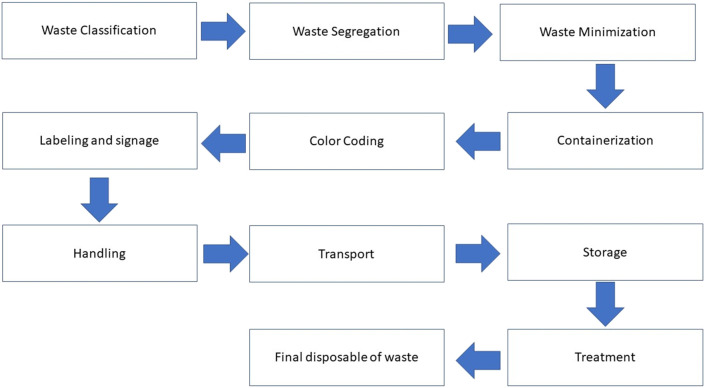
A good healthcare waste management system in a healthcare facility requires an assessment of the waste stream and existing environmental practices, evaluation of waste management options, development of waste management plans, and promulgation of institutional policies and guidelines that clearly define the roles and responsibilities of personnel. Establishment of waste management organization, allocation of staff, financial resources, implementation of plans, periodic training, monitoring, evaluation, and continuous improvement are also important for sustainably managing healthcare waste. The effective management of waste is solely dependent on good healthcare waste management organization and strategies. A waste management team or committee should be formed in order to develop and implement a waste management plan. In low-income areas, there should be an infection control committee, with one person responsible for healthcare waste management in healthcare facilities. It is important to review the strategy periodically, and all staff members involved in healthcare waste should be well aware of the processes and periodic changes (Bharsakade et al., 2021; Thakur, 2021). Overall, the optimization of healthcare resources may reduce waste generation (Rodríguez-Pardo et al., 2020). An effective management strategy for healthcare solid waste during the COVID-19 pandemic is proposed in Fig. 2 .
Fig. 2.
Overview of healthcare solid waste management during COVID-19 pandemic.
Though healthcare solid waste classifications differ between countries, most countries prefer the criteria set out by the WHO. Segregation plays an important role in efficient healthcare waste management (Omar et al., 2012). It covers the separation of different types of waste according to a classification at the point of origin. Therefore, if segregation of recyclable waste from other non-hazardous waste is carried out efficiently, it will minimize the waste significantly (Mosquera et al., 2014; Windfeld and Brooks, 2015). Segregation involves separation of waste into appropriate containers. To segregate infectious waste, clearly marked containers are used that distinguish the type and weight of the waste. Infectious waste is generally kept in plastic bags, plastic-lined cardboard boxes, or other leak-proof containers meeting specific performance standards following elimination of sharps and fluids. Color-coding is employed to identify different types of waste easily. In most countries, red or yellow bags are commonly used to contain infectious waste. General healthcare waste is placed in black or transparent bags. Infectious waste containers are labelled with the international biohazard symbol in a contrasting color. The primary containers, used for sharps disposal, are usually rigid, leak-proof, break-resistant, and puncture-resistant. To prevent leaks from primary containers during transport, secondary leak-proof containers are preferred. To improve segregation efficiency and minimize the incorrect use of containers, appropriate measures should be taken to determine the proper placement and labelling of these containers. It is usual practice to place general trash containers beside infectious waste containers in areas where both types of waste are generated; this leads to effective and better segregation. It is also good practice to use an appropriate number of waste containers. Posters with illustration schemes for proper segregation are sometimes affixed to walls in areas where multiple containers are located; these can serve as reminders to health workers about the purposes of using specific containers for specific waste.
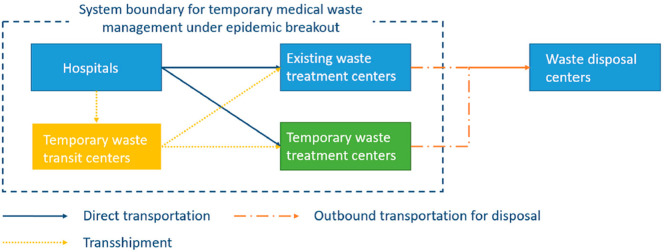
On the other hand, handling the increasing volume of healthcare solid waste and the increased spread of infection is the single biggest issue arising from the novel COVID-19 virus. Temporary healthcare waste treatment centers and temporary transportation facilities can help to manage the waste effectively and to avoid transmission during the COVID-19 pandemic (Fig. 3 ). Waste collected from hospitals and other healthcare centers can be transferred to temporary or existing treatment centers, either directly or through temporary transit centers. Following this, the treated waste can be transferred to waste disposal centers. Waste generation is unpredictable, as the number of infections is not stable (Yu et al., 2020). Therefore, temporary waste treatment and transit may help to manage healthcare solid waste effectively (Yu et al., 2020). The establishment of extra healthcare waste treatment capacity, along with alternative technologies, may help to handle the waste properly. These alternative technologies, i.e. autoclaves and burn incinerators with high temperatures, may help to handle waste during the pandemic (Ilyas et al., 2020; WHO, 2020b). SF-CO2 sterilization technology can help to reduce the risk of exposure to infectious healthcare waste (Hossain et al., 2011). Sterilwave, an ultra-compact technique, can also help to treat healthcare waste, as it kills the COVID-19 virus on-site effectively and thus avoids community transmission during the handling of healthcare waste. This technique can reduce the weight of the waste, and treated waste can even be managed as regular municipal waste (Bertin-medical-Waste, 2020). In addition, a mobile treatment system may help to handle the extra burden of managing healthcare waste during the pandemic.
Fig. 3.
The healthcare solid waste management system during COVID-19 (Yu et al., 2020).
The necessary PPE for handling healthcare waste comprises boots, a long-sleeved gown, heavy-duty gloves, a mask, and goggles or a face shield. It is essential that appropriate hand hygiene is maintained after removing waste. The PPE should be removed safely after the safe disposal of waste, and sanitizer should be used to disinfect the hands after disposing of the waste. Soiled PPE must be put in a sealed bag for safe cleaning either off-site or on-site. The cleaning agent is 10% lime slurry (WHO, 2020c). A summary of information about the techniques used for managing healthcare waste during the COVID-19 pandemic is presented in Table 1 .
Table 1.
An overview of measured strategies for healthcare waste treatment (Ilyas et al., 2020; Klemeš et al., 2020; Manupati et al., 2021; Nibudey and Vidya, 2020; WHO, 2020c).
| Taken measurements | Implications | Impacts |
|---|---|---|
| Safety | PPE and hand sanitizer for workers | Protects workers from being infected |
| Disinfectant | Disinfecting waste prior to sorting | Prevents workers from contracting the virus and spreading it to others |
| Storage | Temporary storage for 9 days | Helps to handle excess waste and prevent it from spreading the virus, which can persist for up to 9 days |
| Treating location | On-site treatment | Suitable for handling extra waste |
| Treating technique | Sterilwave (an ultra-compact mobile treatment system), autoclave, burn incinerator, SF-CO2 sterilization, microwave or radio-wave treatment | Kills the virus |
| Handling | Sorting waste and putting it in different bags based on type of waste | Easier to handle and dispose of |
| Social distancing | 1.5 m among workers and public during waste handling | Prevents infection and spread |
| Training | Using PPE and sanitization | Use of these will help protect from infection |
| Advertisement of guidelines | Social media and display in workplaces | People will become more aware of health measures |
Proper healthcare waste management may help to increase the proportion of recyclable waste (Moreira and Gunther, 2013). Recyclable material can be increased by autoclaving, which may help to reduce the volume of landfill waste during the COVID-19 pandemic (Zand and Heir, 2020a). An autoclave utilizes the basic principle of steam sterilization in which infectious items, such as virus and bacteria are exposed to direct steam at the required temperature and pressure for the defined time. Thus, autoclaving of healthcare solid waste can improve the efficiency of the recycling process as the process can effectively disinfect the contaminated waste. This recycling strategy can reduce the cost of essential safety materials for healthcare during the pandemic. On the other hand, use of disinfectant, such as sodium hypochlorite and alcohol, can inactivate the COVID-19 virus, which can survive for up to 9 days. Therefore, the use of disinfectants and 9-day storage of healthcare waste in an appropriate containment facility can reduce the spread of the virus among healthcare waste handling workers. Alternatively, the healthcare waste can also be used for energy generation. In this regard, pyrolysis and combustion can be used to produce value added products from healthcare waste during the pandemic. Some of the notable examples include incinerator ash from healthcare waste, which has been used in Portland cement (Rowan and Laffey, 2021; Sobiecka et al., 2014). In addition, organic waste can be used to make compost (Abylkhani et al., 2020) and other valuable products, e.g., bioenergy (Velvizhi et al., 2020). Considering all these options, utilizing healthcare waste for valuable purposes and a process of monetization during the pandemic can add definitive value to the circular economy.
8. Conclusions
The volume of healthcare waste is increasing tremendously due to the high infection rate of the novel COVID-19 virus. Virus-contaminated healthcare waste may infect workers in the waste management sector due to their direct exposure to waste and poor safety measures. Thus, the spread of the virus may increase gradually. The WHO has provided clear guidelines for managing healthcare waste during the pandemic. Different nations have taken different measures to manage healthcare waste properly. Effective safety measures and working strategies may allow for proper healthcare waste management without spreading the virus to others. Disinfecting waste, followed by proper segregation and on-site treatment of the waste, can also provide better and healthier healthcare waste management. To accommodate surplus healthcare waste, mobile treatment and temporary storage strategies may aid sustainable management of healthcare waste without further spreading the virus. Proper healthcare waste management can also help to recycle waste or convert it into valuable products, e.g. energy. Therefore, proper healthcare waste management can add value to national economies for sustainable development. In addition, it will help to reduce the spread of the COVID-19 virus.
Funding
None.
Ethical approval
Not required.
CRediT authorship contribution statement
Atanu Kumar Das: Conceptualization, Writing – original draft, Writing – review & editing, Visualization. Md. Nazrul Islam: Conceptualization, Writing – original draft, Writing – review & editing. Md. Morsaline Billah: Conceptualization, Writing – original draft, Writing – review & editing. Asim Sarker: Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
None.
Editor: Lotfi Aleya
References
- Abylkhani B., Guney M., Aiymbetov B., Yagofarova A., Sarbassov Y., Zorpas A.A., et al. Detailed municipal solid waste composition analysis for Nur-Sultan City, Kazakhstan with implications for sustainable waste management in Central Asia. Environ. Sci. Pollut. Res. 2020 doi: 10.1007/s11356-020-08431-x. [DOI] [PubMed] [Google Scholar]
- ADB. Managing Infectious Medical Waste during the COVID-19 Pandemic, https://www.adb.org/publications/managing-medical-waste-covid19, 2020.
- Ansari M., Ehrampoush M.H., Farzadkia M., Ahmadi E. Dynamic assessment of economic and environmental performance index and generation, composition, environmental and human health risks of hospital solid waste in developing countries; a state of the art of review. Environ. Int. 2019;132 doi: 10.1016/j.envint.2019.105073. [DOI] [PubMed] [Google Scholar]
- Askarian M., Heidarpoor P., Assadian O. A total quality management approach to healthcare waste management in Namazi hospital, Iran. Waste Manag. 2010;30:2321–2326. doi: 10.1016/j.wasman.2010.06.020. [DOI] [PubMed] [Google Scholar]
- Bertin-medical-Waste. China chooses the Sterilwave solution for on-site treatment of waste contaminated by the coronavirus, https://www.bertin-medical-waste.com/my-account/, 2020.
- Bharsakade RS, Acharya P, Ganapathy L, Tiwari MK. A lean approach to healthcare management using multi criteria decision making. OPSEARCH 2021.
- Commendatore C. Coronavirus Impacts Hit Solid Waste Managers, Generators, https://www.waste360.com/medical-waste/coronavirus-impacts-hit-solid-waste-managers-generators, 2020.
- Cremonesi P., Sartini M., Spagnolo A.M., Adriano G., Zsirai E., Patrone C., et al. Transformation of a ferry ship into a ship hospital for COVID-19 patients. Int. J. Environ. Res. Public Health. 2020;17:1–10. doi: 10.3390/ijerph17238976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EMB. Management of Infectious Healthcare Waste During Covid-19 Pandemic, https://emb.gov.ph/management-of-infectious-healthcare-waste-during-covid-19-pandemic/, 2020.
- Ferreira V., Teixeira M.R. Healthcare waste management practices and risk perceptions: findings from hospitals in the Algarve region, Portugal. Waste Manag. 2010;30:2657–2663. doi: 10.1016/j.wasman.2010.07.012. [DOI] [PubMed] [Google Scholar]
- Haji J.Y., Subramaniam A., Kumar P., Ramanathan K., Rajamani A. State of personal protective equipment practice in Indian intensive care units amidst COVID-19 pandemic: a Nationwide survey. Ind. J. Crit. Care Med. 2020;24:809–816. doi: 10.5005/jp-journals-10071-23550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hossain M.S., Santhanam A., Norulaini N.A.N., Omar A.K.M. Clinical solid waste management practices and its impact on human health and environment - a review. Waste Manag. 2011;31:754–766. doi: 10.1016/j.wasman.2010.11.008. [DOI] [PubMed] [Google Scholar]
- Ilyas S., Srivastava R.R., Kim H. Disinfection technology and strategies for COVID-19 hospital and bio-medical waste management. Sci. Total Environ. 2020;749 doi: 10.1016/j.scitotenv.2020.141652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ISWA-Jordan. Country Specific Waste Management Responses, COVID-19 Response International knowledge sharing on Waste Management, https://www.iswa.org/fileadmin/galleries/0001_COVID/Jordan_Solid_Waste_Handling_Manual_Coronavirus_crisis-ENG.pdf:https://www.iswa.org/iswa/covid-19/, 2020.
- ISWA-Lebanon. Country Specific Waste Management Responses, COVID-19 Response International knowledge sharing on Waste Management, https://www.iswa.org/fileadmin/user_upload/_temp_/MoE__Lebanon__-_COVID19_MSW_Management_General_Guidelines_April_23_2020.pdf:https://www.iswa.org/iswa/covid-19/, 2020.
- ISWA-Netherlands. Country Specific Waste Management Responses, COVID-19 Response International knowledge sharing on Waste Management, https://www.iswa.org/fileadmin/galleries/0001_COVID/Netherlands_Waste_Management_during_Covid19.pdf:https://www.iswa.org/iswa/covid-19/, 2020.
- Johannessen L., Dijkman M., Bartone C., Hanrahan D., Boyer M., Chandra C. World Bank; Washington DC: 2000. Health Care Waste Management Guidance Note. [Google Scholar]
- Kalogiannidou K., Nikolakopoulou E., Komilis D. Generation and composition of waste from medical histopathology laboratories. Waste Manag. 2018;79:435–442. doi: 10.1016/j.wasman.2018.08.012. [DOI] [PubMed] [Google Scholar]
- Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020;104:246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klemeš J.J., Fan Y.V., Tan R.R., Jiang P. Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew. Sust. Energ. Rev. 2020;127 doi: 10.1016/j.rser.2020.109883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malsparo. Pharmaceutical Waste Management, https://www.malsparo.com/pharm.htm, 2020.
- Manupati V.K., Ramkumar M., Baba V., Agarwal A. Selection of the best healthcare waste disposal techniques during and post COVID-19 pandemic era. J. Clean. Prod. 2021;281 doi: 10.1016/j.jclepro.2020.125175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mato R., Kassenga G.R. A study on problems of management of medical solid wastes in Dar es Salaam and their remedial measures. Resour. Conserv. Recycl. 1997;21:1–16. [Google Scholar]
- Mingyu Q. GmbH CIWMINPDGfIZG. 2020. China’s waste sector response to Covid-19. Tayuan Diplomatic Office Building 2–5, 14 Liangmahe South Rd, Chaoyang District, 100600 Beijing, PR China. [Google Scholar]
- Mol M.P.G., Caldas S. 2020. Can the Human Coronavirus Epidemic Also Spread through Solid Waste? Waste Management & Research. [DOI] [PubMed] [Google Scholar]
- Moreira A.M.M., Gunther W.M.R. Assessment of medical waste management at a primary health-care center in Sao Paulo, Brazil. Waste Manag. 2013;33:162–167. doi: 10.1016/j.wasman.2012.09.018. [DOI] [PubMed] [Google Scholar]
- Mosquera M., Andres-Prado M.J., Rodriguez-Caravaca G., Latasa P., Mosquera M.E.G. Evaluation of an education and training intervention to reduce health care waste in a tertiary hospital in Spain. Am. J. Infect. Control. 2014;42:894–897. doi: 10.1016/j.ajic.2014.04.013. [DOI] [PubMed] [Google Scholar]
- Nibudey A., Vidya Baliga S. Preparing hospitals in India for covid-19 pandemic. Int. J. Res. Pharm. Sci. 2020;11:333–341. [Google Scholar]
- Nzediegwu C., Chang S.X. Improper solid waste management increases potential for COVID-19 spread in developing countries. Resour. Conserv. Recycl. 2020;161 doi: 10.1016/j.resconrec.2020.104947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omar D, Nazli SN, Karuppannan SAL. Clinical waste management in district hospitals of Tumpat, Batu Pahat and Taiping. In: Abbas MY, editor. Aice-Bs 2012 Cairo. 68, 2012, pp. 134–145.
- Pepin J., Abou Chakra C.N., Pepin E., Nault V., Valiquette L. Evolution of the global burden of viral infections from unsafe medical injections, 2000-2010. PLoS One. 2014;9 doi: 10.1371/journal.pone.0099677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman M.M., Bodrud-Doza M., Griffiths M.D., Mamun M.A. Biomedical waste amid COVID-19: perspectives from Bangladesh. Lancet Glob. Health. 2020;8:E1262. doi: 10.1016/S2214-109X(20)30349-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramteke S., Sahu B. Novel coronavirus disease 2019 (COVID-19) pandemic: considerations for the biomedical waste sector in India. Case Studies in Chemical and Environmental Engineering. 2020;2:100029. doi: 10.1016/j.cscee.2020.100029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Morales A. Rijeka; InTech: 2013. Current Topics in Public Health. [Google Scholar]
- Rodríguez-Pardo J., Fuentes B., Alonso de Leciñana M., Campollo J., Calleja Castaño P., Carneado Ruiz J., et al. Acute stroke care during the COVID-19 pandemic. Ictus Madrid Program recommendations. Neurologia. 2020;35:258–263. doi: 10.1016/j.nrl.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowan N.J., Laffey J.G. Unlocking the surge in demand for personal and protective equipment (PPE) and improvised face coverings arising from coronavirus disease (COVID-19) pandemic – implications for efficacy, re-use and sustainable waste management. Sci. Total Environ. 2021;752:142259. doi: 10.1016/j.scitotenv.2020.142259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma H.B., Vanapalli K.R., Cheela V.R.S., Ranjan V.P., Jaglan A.K., Dubey B., et al. Challenges, opportunities, and innovations for effective solid waste management during and post COVID-19 pandemic. Resour. Conserv. Recycl. 2020;162 doi: 10.1016/j.resconrec.2020.105052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh N., Tang Y.Y., Ogunseitan O.A. Environmentally sustainable Management of Used Personal Protective Equipment. Environ. Sci. Technol. 2020;54:8500–8502. doi: 10.1021/acs.est.0c03022. [DOI] [PubMed] [Google Scholar]
- Singh N., Tang Y.Y., Zhang Z.T., Zheng C.M. COVID-19 waste management: effective and successful measures in Wuhan, China. Resour. Conserv. Recycl. 2020;163 doi: 10.1016/j.resconrec.2020.105071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobiecka E., Obraniak A., Antizar-Ladislao B. Influence of mixture ratio and pH to solidification/stabilization process of hospital solid waste incineration ash in Portland cement. Chemosphere. 2014;111:18–23. doi: 10.1016/j.chemosphere.2014.03.057. [DOI] [PubMed] [Google Scholar]
- Star TD. Poor medical waste management will increase infections. The Daily; Star: 2020. https://www.thedailystar.net/editorial/news/poor-medical-waste-management-will-increase-infections-1909561 [Google Scholar]
- Thakur V. Framework for PESTEL dimensions of sustainable healthcare waste management: Learnings from COVID-19 outbreak. J. Clean. Prod. 2021;287 doi: 10.1016/j.jclepro.2020.125562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ubuoh E.A., Ezenwa L.I., Ndukwu M.C., Emeka-Chris C.C. Assessment of cation chemistry of groundwater near hospital wastes dumpsites in Umuahia Nigeria using multivariate and analytical index approach. Environ. Technol. Innov. 2019;15 [Google Scholar]
- UN. Managing biomedical and healthcare waste during COVID-19, https://samoa.un.org/en/40100-managing-biomedical-and-healthcare-waste-during-covid-19, 2020.
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velvizhi G., Shanthakumar S., Das B., Pugazhendhi A., Priya T.S., Ashok B., et al. Biodegradable and non-biodegradable fraction of municipal solid waste for multifaceted applications through a closed loop integrated refinery platform: paving a path towards circular economy. Sci. Total Environ. 2020;731 doi: 10.1016/j.scitotenv.2020.138049. [DOI] [PubMed] [Google Scholar]
- Wang X.W., Li J.S., Jin M., Zhen B., Kong Q.X., Song N., et al. Study on the resistance of severe acute respiratory syndrome-associated coronavirus. J. Virol. Methods. 2005;126:171–177. doi: 10.1016/j.jviromet.2005.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waste-Mangement. Waste management in the context of the coronavirus crisis, https://ec.europa.eu/info/sites/info/files/waste_management_guidance_dg-env.pdf, 2020.
- Wei G, Manyu L. The Hidden Risks of Medical Waste and the COVID-19 Pandemic, https://www.waste360.com/medical-waste/hidden-risks-medical-waste-and-covid-19-pandemic, 2020.
- WHO. Water, sanitation, hygiene, and waste management for the COVID-19 virus, https://www.who.int/publications-detail/water-sanitation-hygiene-and-waste-management-for-covid-19, 2019.
- WHO. Interim guidance, Water, sanitation, hygiene, and waste management for SARS-CoV-2, the virus that causes COVID-19, https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC-WASH-2020.4, 2020a.
- WHO. Water, sanitation, hygiene, and waste management for the COVID-19 virus: interim guidance. World Health Organization, https://www.who.int/publications-detail/water-sanitation-hygiene-and-waste-management-for-covid-19, 2020b, pp. 9.
- WHO. Water, sanitation, hygiene, and waste management for the COVID-19 virus: interim guidance, https://www.who.int/publications-detail/water-sanitation-hygiene-and-waste-management-for-covid-19, 2020c.
- Windfeld E.S., Brooks M.S.L. Medical waste management - a review. J. Environ. Manag. 2015;163:98–108. doi: 10.1016/j.jenvman.2015.08.013. [DOI] [PubMed] [Google Scholar]
- Wilder-Smith A., Osman S. Public health emergencies of international concern: a historic overview. J. Tra. Med. 2020;27(8):1–13. doi: 10.1093/jtm/taaa227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang W., Cai C., Dai X.H. The potential exposure and transmission risk of SARS-CoV-2 through sludge treatment and disposal. Resour. Conserv. Recycl. 2020;162 doi: 10.1016/j.resconrec.2020.105043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu H., Sun X., Solvang W.D., Zhao X. Reverse logistics network Design for Effective Management of medical waste in epidemic outbreaks: insights from the coronavirus disease 2019 (COVID-19) outbreak in Wuhan (China) Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17051770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yves Chartier J.E., Pieper Ute, Prüss Annette, Rushbrook Philip, Stringer Ruth, Townend William, Wilburn Susan, Zghondi Raki. World Health Organization (WHO); 2014. Safe Management of Wastes from Health-care Activities. [Google Scholar]
- Zand A.D., Heir A.V. Emerging challenges in urban waste management in Tehran, Iran during the COVID-19 pandemic. Resour. Conserv. Recycl. 2020;162 doi: 10.1016/j.resconrec.2020.105051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zand A.D., Heir A.V. Environmental impacts of new Coronavirus outbreak in Iran with an emphasis on waste management sector. J. Mater. Cycles Waste Manag. 2020;23:240–247. doi: 10.1007/s10163-020-01123-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zand A.D., Heir A.V. Emanating challenges in urban and healthcare waste management in Isfahan, Iran after the outbreak of COVID-19. Environmental Technology. 2020;42(2):329–336. doi: 10.1080/09593330.2020.1866082. [DOI] [PubMed] [Google Scholar]