Abstract
The purpose of this study was to retrospectively assess patients treated with modular, non-cemented, tapered, fluted, distal fixation stems. We included patients with 24 months mínimum follow-up. Diagnosis that led to revisions were described. The radiographic analysis was made with preoperative, immediate postoperative and last control postoperative X-rays. Sixty-seven patients met inclusion criteria. We observed 59,7% (n=40) Osteointegration, 34,3% of Stable Fibrosis and 5,97% Unstable fibrosis. Stress Shielding was registered with 10,44% and Subsidence was observed in 34,3% of the patients. Modular, fluted, tapered, distal fixation stems have an excellent survival rates.
Keywords: Revision of total hip replacement, Arthroplasty, Joint replacement, Distal Fixation Stems
1. Introduction
In the past decade, primary hip arthroplasties have increased and consequently the number of revisions. In the U.S., between 1990 and 2002, revision rate for Total Hip Replacement (THR) was 17,5% and its expected that for 2026, it will be over 30%.1
When an orthopedic surgeon performs revisions of hip arthroplasties, they have to struggle with several problems like bone stock deficiency, implant removal and achieving a stable fixation to restore joint biomechanics. This are some of the reasons distal fixation stems were developed, due their ability to skip the proximal bone defect.2
Initially, they were non-modular, cylindrical, titanium stems, with good results and 10 years implant survival rate of 85–95%. However, persistent thigh pain and severe stress shielding was very frequent.3 When Wagner's non-modular, tapered, extensively porous-coated stems appeared, they seemed like a great solution. Due its geometry, they were able to improve axial and rotational stability, but it was observed high dislocation and subsidence rates.4,5
With the modular stems arrival, it was able to achieve and stable fixation and the possibility to adapt more easily femoral version, head-neck off-set and proper length for each patient.5 Jang et al., performed a retrospective study in 2015 where they analyzed 47 hip revisions, with Paprosky's type II, IIIA and IIIB defects, treated with modular, cementless, distal fixation stems and they reported high survival rate of 86% with a Harris Hip Score (HHS) improvement from 39,5 to 91,3.6
The purpose of this study was to assess patients treated with modular, non-cemented, tapered, fluted, distal fixation stems, focusing in their indications, clinical-radiological evolution and complications.
2. Method
Since 2008 to 2016, 137 hip revisions were performed. All surgeries were performed at a high volume center, by the same senior surgeon (FAL) with a postero-lateral approach.
We included in our study, adult patients that underwent revision of the femoral component and a modular, cementless, tapered and fluted, distal fixation stem was used instead, with a minimum follow up of 24 months.
First author collected data from medical records and radiographic registry of the center. Patients with multiple previous surgeries, rheumatoid arthritis, or previous biological treatments or chemotherapy were excluded.
Diagnosis that led to revisions is described on Table 1.
Table 1.
Nominal and percentage distribution of causal diagnosis for prosthetic femoral component revision.
| Diagnosis | Patients (n) | Percentage (%) |
|---|---|---|
| Mechanical loosening | 25 | 37,30 |
| Septic Loosening | 24 | 35,80 |
| Peri-prosthetic Fracture | 7 | 10,44 |
| No-union | 7 | 10,44 |
| Instability | 2 | 3 |
| Stem rupture | 2 | 3 |
Regarding loosening revisions, patients were groupd with Paprosky's7 method, detailed in Table 2.
Table 2.
Distribution according Paprosky classification about bone stock defects.
| Mechanical Loosening | I |
II |
IIIA |
IIIB |
IV |
|---|---|---|---|---|---|
| 0 | 5 | 12 | 7 | 1 | |
| Septic Loosening | 0 | 9 | 11 | 4 | 0 |
We documented 7 periprosthetical fractures and grouped them using Vancouver's classification.8 Four were B2, two B3 and one case B1. All cases, the fracture was due a fall of patient's own height.
Functional assessment was carried out comparing preoperative and postoperative HHS. We also recorded surgical, clinical and infectious complications.
Radiographic assessment was made with antero-posterior and lateral view comparing preoperative, immediate postoperative and last control X-rays.
We evaluated stems behavior with Engh's criteria, and we grouped three categories: Osteointegration, Stable Fibrosis and Unstable Fibrosis9
Stress Shielding was defined as the presence of osteolysis or bone loss in greater trochanter in most recent x-ray.10
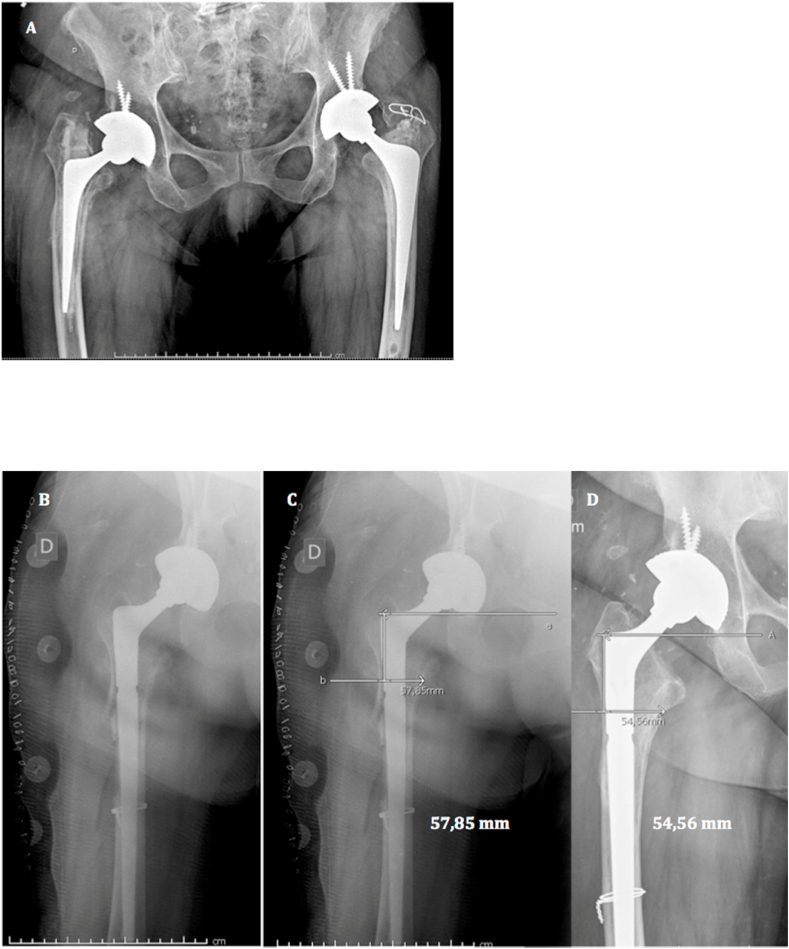
Stem subsidence was registered by measuring vertical migration, using as reference points, the distance from the shoulder of the femoral component to the lower edge of lesser trochanter. In those cases, where the lesser trochanter was absent, we used the first wire loop.10
All measurements were performed three times by two independent authors and the average was used. To decrease error from precision bias, we used Synapse Software ® (Medical system, Fujifilm, USA). To avoid magnification error on the images, we used as reference internal diameter of cephalic component.
Revision-free survival rate of the stem was calculated.
3. Results
Four patients were excluded for not complying the minimum follow up (two of those died before 24 months).
Sixty-seven patients met inclusion criteria, with 37 (55,2%) women and 30 (44,8%) men. Mean age was 66,5 years (22–88). Thirty-seven (55,2%) right hips were treated and 30(44,8%) left hips. We used Restoration, Stryker, NJ, USA ® in 42 (62,7%) patients and ZMR, Zimmer, Warsaw, USA ® 25 (37,3%) times.
Mean follow-up was 29,45 months (range 24–120). We observed statistically significant improvement of HHS from a mean of 37,6 ± 7,4 to 83,6 ± 8,3 (p<. 05).
Analyzing stems behavior, we found 59,7% (n = 40) Osteointegration, 34,3%(n = 23) Stable Fibrosis and 5,97%(n = 4) Unstable fibrosis. Stress Shielding was registered in seven (10,4%) patients.
Subsidence was observed in 34,3% (n = 23) of the patients. Mean migration value was 3,2 ± 2,5 mm (0,2–8,3). Eight (11,9%) of those had more than 5 mm of subsidence, but no symptoms were registered.
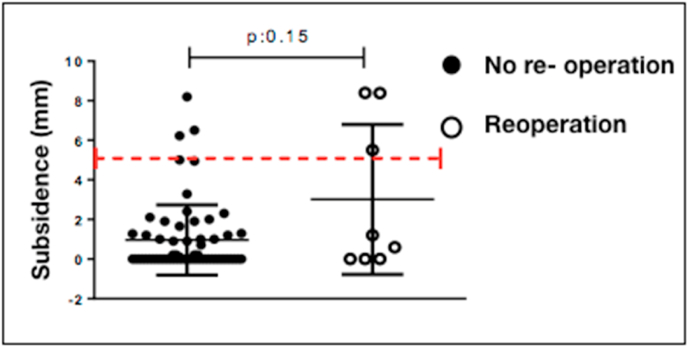
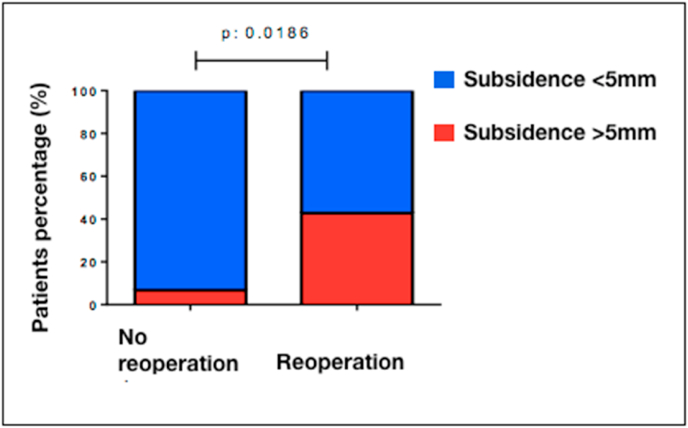
Although in absolute value, there were no statistically significant differences in millimeters of subsidence, in reoperated patients (3,01 ± 3,7 vs 0,96 ± 1,7; p = 0,15)(Fig. 1), we were able to observe a significant increase of percentage that required an additional procedure when subsidence was ≥5 m. (42,8% vs 6,7%)(Fig. 2).
Fig. 1.
Subsidence and reoperation. The dotted line points the limit of ≥5 mm. We observed there's no association between those patients who suffered subsidence over 5 mm and reoperation.
Fig. 2.
Picture showing the percentage difference from patients that required additional procedure with subsidence ≥ 5 mm on blue squares, and below 5 mm on red squares.
Complication rate was 11,94%. One patient evolved with steppage due to an External Popliteal-Sciatic nerve injury that was treated with electro-stimulation and orthesis achieving partial recovery.
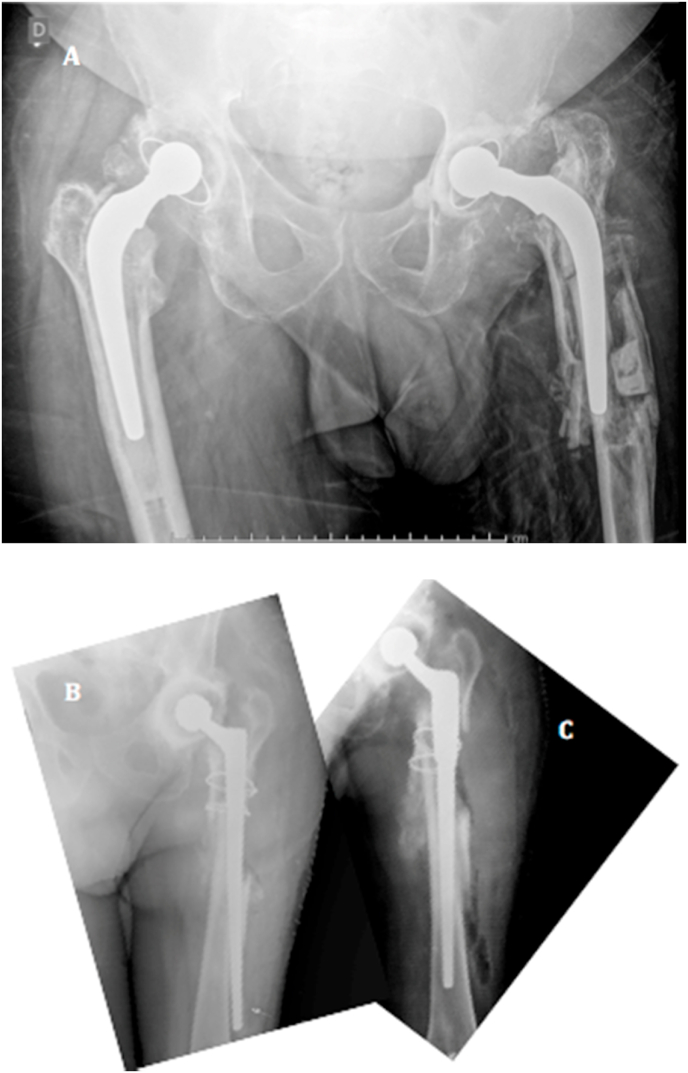
Seven patients (10,4%) required additional procedures. There were 2 cases of intraoperative fractures that required immediate surgical reduction to fix it.
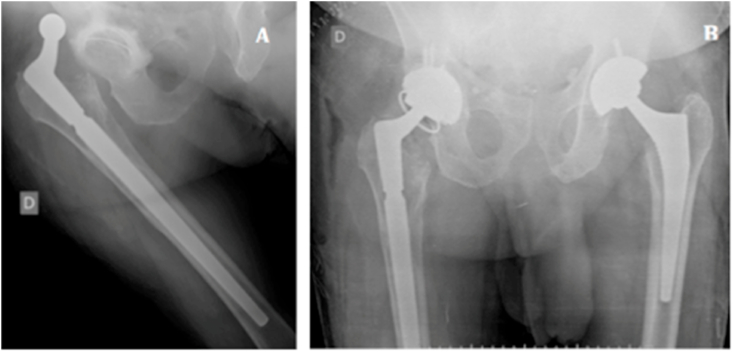
There were no symptoms after second procedure. Another patient suffered a fall of its own height and evolved with stem rupture. We decided to perform revision of the stem using a megaprosthesis. Three patients had dislocations that required open reduction. One of them had liner rupture, so we exchange the polyethylene insert and there was no need for further procedures. Another patient suffered recurrent dislocations, forcing us to use a more constrained system, with tripolar cup (Fig. 3).
Fig. 3.
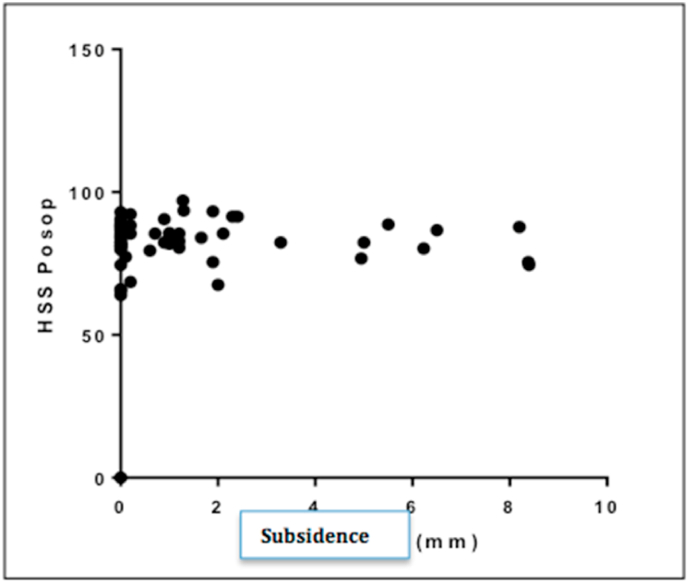
We can appreciate HHS values are in a consistent range despite values of subsidence.
There was one acute infection, treated with toilette and debridement plus exchange of mobile components. The involved microorganism was Aureus Staphylococcus methicillin-sensitive (ASMS).
Two years revision-free survival rate of the implant was 89,6%. If we discriminate causes attributable to the stem (2 intraoperative fracture and 1 stem rupture), this number increases to 95,5%.
There was no relationship between HHS and subsidence, observing and Spearson relation with r = 8,08 and a CI95% = −0,15 to 0,31; p = 0,47 (Fig. 4).
Fig. 4.
A) Dislocation of femoral stem with a cemented cup. B) Cup Exchange for a tripolar system.
We found there was no statistically significant difference If we separate patients according subsidence ≥ 5 mm and those who were below that number with HHS. (83,49 +- 6,9 VS 82,27 +- 5,7; p = 0,6).
4. Discussion
Revisions in hip arthroplasty represents a really complex procedure, where orthopedic surgeons must face multiple challenges like bone stock deficiencies, mainly at expense of the metaphysis, that makes harder to achieve a good stability with standard stems.11 Modular stems of distal fixation allows to overcome this obstacle, achieving good proximal filling of the femur with distal impaction. Also they have multiple options to adjust femoral off-set, version and if its necessary.12
The Swedish Registry proved that first cause of hip revisions is aseptic loosening, followed by infection and periprosthetic fracture.13 This is consistent with our study where we found that aseptic and infectious loosening represented 70% of the patients.
Several authors have suggested that proper fixation of the femoral component in Paprosky's I to IIIA defects could be achieved with the used of an extended porous-coated stem,14,15 while on IIIB and IV types, modular distal fixation stems would allow a fixation more stable with a smaller isthmus segment, thanks to their geometry.16 In 2014, Brown et al.17 analyzed 135 hip revisions with severe femoral defects and obtained excellent results. In our study, although we used distal fixation stems, author's opinion is that, they prefer long cemented stems with bone graft impaction (Ling technique) for patients with Paprosky's IV defects.18
We observed 7 periprosthetic fractures (4 B2, 2 B3 and one B1). One of the great advantages of Vancouver classification is that helps us to decide the proper treatment. Several authors19,20,21 endorse the use of cementless, tapered, fluted, distal fixation stems, because they can led us to achieve really good clinical and radiographic results. Recently, we published a paper of this types of fracture that showed a high success rates with this stems.22
In 1990, Charles A. Engh, 9) published an article about the biological behavior and stability of porous surface stems. Basically, he defined very clearly major and minor radiological signs that defined osteointegration of the stems, as well as the stability. It's so, that our institution published an article, with 22 patients who underwent 22 revisions, with proximal fixation and distal anchor, cementless stems for Paprosky's II and IIIA defects, and obtained 77,2% of osteointegration. In this analysis, we observed about 60% of bone integration and we believe that this percentage its because we included more severe defects (IIIB and IV).11
The design of this implants leads to a decrease of the load on the proximal femur; this causes a minor bone density (stress shielding).23 Our evaluation revealed seven (10,4%) patients in this situation.
There's no consensus in literature, that stem subsidence and loosening may be related.24,25 When the stem press fit isn't strong enough to support physiological loads, the stem achieves a secondary stability by subsidence into the femur. In 2008, Kang et al.26 analyzed 39 hip revisions treated with distal fixation stems (ZMR, Zimmer, Warsaw, USA ®) and they observed a mean subsidence of 4,4 mm and 5 cases with more than 5 mm of migration. In more recent study, the Revision Total Hip Arthroplasty Study Group27 described 61 hips treated with distal fixation stems, with an average subsidence of 3 mm, and of this patients, 5 (8,2%) presented migration above 10 mm. There was one case of reoperation because early mechanical failure of the stem. Our mean subsidence was 3,29 mm and we were unable to demonstrate an statistically significant relationship with revision surgery. (p = 0,15) (Fig. 5).
Fig. 5.
A. 76 year old female. Antero-posterior right hip X-ray. We can observe osteolysis and debonding around femoral stem of right hip. B. Immediate postoperative radiography. Conversion of standard to modular, distal fixation stems. We kept acetabular component because it was well fixed. C) Measure of the distance between the shoulder of the stem and the caudal edge of the lesser trochanter → 57,85 mm. D) 26 months later, you can see the distance decreases to 54,56 mm.
The total percentage of complications and the improvement on HHS is similar to other recent series on the literature (Table 3).
Table 3.
Studies comparison. We can see complications percentages and HHS values before surgery and after surgery.
| Studies | Complications (%) | Harris Hip Score | |
| Before surgery | After surgery | ||
| Neumann 2011 | 13,6 | 35,9 (20–65) | 94,3 (82–100) |
| Zunino 2016 | 25,3 | 37 (10–77) | 81 (33–96) |
| Rieger 2017 | 16,2 | – | 85,6 (31–100) |
| Our study 2019 | 11,9 | 37,6 (19–62) | 83,6 (41–97) |
There were two femur fractures with the distal tip of the stem that required open fixation immediately. This is why we recommend the use of C-arm routinely in complex femur revisions (Fig. 6).
Fig. 6.
A. Left hip Periprosthetic Fracture (Vancouver B3). We can observe that the fracture involves the stem area and poor bone stock. B. Fracture during surgery with the tip of the stem. C) Distal fixation stem reduction.
Authors like Van Houwelingen28 proved that modular, fluted, tapered, distal fixation stems achieves 5–10 years a mean of 90% implant survival. These values are consistent with more recent publications.29,30 Although our prosthetic survival rates involves a minor follow-up (mean of 30 months), we obtained similar results with current literature. We must continue follow-up in the future to be able to analyze more significant long-term results.
The strengths of this study is the number of patients that allows us o perform an statistical association of the results and the follow-up, that's enough to analyze the clinical and radiographic, short term, behavior of the stems.
The weaknesses are those of a retrospective study and the heterogeneity of the diagnosis treated with this implants.
5. Conclusion
Modular, fluted, tapered, distal fixation stems have excellent survival rates, with great clinical results when we must face Paprosky's type II and IIIA defects.
It remains as pending continue the follow-up of this group in the future.
Declaration of competing interest
None of the authors involved in this work received any benefit for this publication.
References
- 1.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg - Ser A. 2007;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Canella R.P., de Alencar P.G.C., Ganev G.G., de Vincenzi L.F. Revision total hip arthroplasty using a modular cementless distal fixation prosthesis: the Zmr® hip system. Clinical and radiographic analysis of 30 cases. Rev Bras Ortop. 2010;45(3):279–285. doi: 10.1016/S2255-4971(15)30369-4. https://linkinghub.elsevier.com/retrieve/pii/S2255497115303694 (English Ed [Internet] Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lachiewicz P.F., Soileau E.S. What is the survivorship of fully coated femoral components in revision hip arthroplasty? Clin Orthop Relat Res. 2014;473(2):549–554. doi: 10.1007/s11999-014-3689-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baktir A., Karaaslan F., Gencer K., Karaoğlu S. Femoral revision using the wagner sl revision stem: a single-surgeon experience featuring 11-19 years of follow-up. J Arthroplasty. 2015;30(5):827–834. doi: 10.1016/j.arth.2014.12.024. [Internet] Available from. [DOI] [PubMed] [Google Scholar]
- 5.Huang Y., Zhou Y., Shao H., Gu J. What is the difference between modular and nonmodular tapered fluted titanium stems in revision total hip arthroplasty. J Arthroplasty. 2017 doi: 10.1016/j.arth.2017.05.021. [Internet] Available from. [DOI] [PubMed] [Google Scholar]
- 6.Jang H.-G., Lee K.-J., Min B.-W., Ye H.-U., Lim K.-H. Mid-term results of revision total hip arthroplasty using modular cementless femoral stems. Hip pelvis. 2015;27(3):135–140. doi: 10.5371/hp.2015.27.3.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paprosky W.G., Perona P.G., Lawrence J.M. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994;9(1):33–44. doi: 10.1016/0883-5403(94)90135-x. [DOI] [PubMed] [Google Scholar]
- 8.Duncan C.P., Masri B.A. Fractures of the femur after hip replacement. 1995;25:293–304. [PubMed] [Google Scholar]
- 9.Engh C., Massin P., Suthers K. Roentgenographic assessment. Clin Orthop Relat Res. 1990;257:107–128. [PubMed] [Google Scholar]
- 10.Malchaul H., Kiirrholml J., Wang Y.X., Herbertsl P. Accuracy of migration analysis in hip arthroplasty. 1995;66(5) doi: 10.3109/17453679508995578. [DOI] [PubMed] [Google Scholar]
- 11.Garabano G., Pastrián D.S.M., Sel H. Revisiones de cadera en defectos óseos femorales Paprosky II y IIIA Utilización de prótesis no cementada. modular. 2016:115–121. [Google Scholar]
- 12.Sivananthan S., Lim C.T., Narkbunnam R., Sox-Harris A., Huddleston J.I., Goodman S.B. Revision hip arthroplasty using a modular, cementless femoral stem: intermediate-term follow-up. J Arthroplasty [Internet] 2017;32(4):1245–1249. doi: 10.1016/j.arth.2016.10.033. Available from. [DOI] [PubMed] [Google Scholar]
- 13.Of O. 2002. The Swedish Total Hip Replacement Register. [DOI] [PubMed] [Google Scholar]
- 14.Nadaud M.C., Griffin W.L., Fehring T.K. Cementless revision total hip arthroplasty without allograft in severe proximal. Femoral Defects. 2005;20(6):738–744. doi: 10.1016/j.arth.2004.12.053. [DOI] [PubMed] [Google Scholar]
- 15.Engh C.A., Ellis T.J., Koralewicz L.M., Mcauley J.P., Engh C.A. Extensively porous-coated femoral revision for severe femoral bone loss minimum 10-year. Follow-Up. 2002;17(8):955–960. doi: 10.1054/arth.2002.35794. [DOI] [PubMed] [Google Scholar]
- 16.Bedair H., Tetrault M., Choi H.R. A comparison of modular tapered versus modular cylindrical stems for complex femoral revisions. J Arthroplasty [Internet] 2013;28(8 SUPPL):71–73. doi: 10.1016/j.arth.2013.04.052. Available from. [DOI] [PubMed] [Google Scholar]
- 17.Brown N.M., Tetreault M., Cipriano C.A., Della Valle C.J., Paprosky W., Sporer S. Modular tapered implants for severe femoral bone loss in THA: reliable osseointegration but frequent complications. Clin Orthop Relat Res. 2014;473(2):555–560. doi: 10.1007/s11999-014-3811-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lopreite F, Garabano G, Pastrián DM. Utilización de tallos femorales largos cementados asociados a injerto óseo molido e impactado en revisiones de cadera. Rev Asoc Arg Ortop y Traumatol. 77:2–9.
- 19.Abdel M.P., Lewallen D.G., Berry D.J. Periprosthetic femur fractures treated with modular fluted. Tapered Stems. 2014:599–603. doi: 10.1007/s11999-013-2936-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pereira S., Allende B. 2016. Tratamiento de las fracturas periprotésicas de cadera de tipos B2 y B3 con tallos no cementados de fijación distal. 287–93. [Google Scholar]
- 21.Neumann D., Thaler C., Dorn U. 2012. Management of Vancouver B2 and B3 Femoral Periprosthetic Fractures Using a Modular Cementless Stem without Allografting; pp. 1045–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nazur G. Tratamiento de las fracturas periprotésicas de fémur Vancouver B2 y B3. 2012;77:252–259. [Google Scholar]
- 23.Bs D.W.H., Callaghan J.J., Liu S.S. Second-generation extensively porous-coated THA stems at minimum 10-year followup. 2009;2290–6 doi: 10.1007/s11999-009-0831-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zunino L.A.S., Núñez J., Mangupli M.M., Pioli I., Gómez D.J., Allende B.L. Revisión femoral con tallo cónico de fijación distal. Rev la Asoc Argentina Ortop y Traumatol. 2017;82(1):40–47. [Google Scholar]
- 25.Rieger B., Ilchmann T., Bolliger L., Stoffel K.K., Zwicky L., Clauss M. Mid-term results of revision total hip arthroplasty with an uncemented modular femoral component. HIP Int. 2018;28(1):84–89. doi: 10.5301/hipint.5000522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kang M.N., Huddleston J.I., Hwang K., Imrie S., Goodman S.B. Early outcome of a modular femoral component in revision total hip arthroplasty. J Arthroplasty. 2008;23(2):220–225. doi: 10.1016/j.arth.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 27.Total R., Arthroplasty H., Group S. A comparison of modular tapered versus modular cylindrical stems for complex femoral revisions. J Arthroplasty [Internet] 2013;28(8):71–73. doi: 10.1016/j.arth.2013.04.052. Available from. [DOI] [PubMed] [Google Scholar]
- 28.Houwelingen AP Van, Duncan C.P., Masri B.A., Greidanus N.V., Garbuz D.S. 2013. High Survival of Modular Tapered Stems for Proximal Femoral Bone Defects at 5 to 10 Years Followup; pp. 454–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Neumann D., Dueckelmann L., Thaler C., Dorn U. 2012. Revision Total Hip Arthroplasty Using a Cementless Tapered Revision Stem in Patients with a Mean Age of 82 Years; pp. 961–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rieger B., Illchman T., Bolliger L., Stoffer K., Zwicky L.C.M. Mid-term results of revision total hip arthroplasty with and uncement modular femoral component. 2018;28:84–89. doi: 10.5301/hipint.5000522. [DOI] [PMC free article] [PubMed] [Google Scholar]