Abstract
Charcot Neuroarthropathy (CN) of the ankle/hindfoot is a devastating condition that results in a loss of alignment, bony malleolar protrusions and frequently leads to ulceration, infection, and amputation. Major limb amputations in this patient population has a 5-year mortality rate approximating 39%–68%. The treatment goal for CN of the ankle/hindfoot is to provide stability with a plantigrade foot that is infection free, shoeable and allows independent weight bearing. The use of a circular frame external fixator is often required when treating patients with CN of the ankle/hindfoot because they often present late with deformity, soft tissue compromise and infection which are contraindications to primary internal fixation. These patients require urgent surgical attention to salvage the limb or risk amputation. In this narrative review article we will discuss the indications, management options, surgical technique, evidence and describe our experience in the use of circular frame external fixation in patients with ankle/hindfoot Charcot Neuroarthropathy.
Keywords: Charcot neuroarthropathy, Hindfoot, Ankle, Circular frame external fixator, Limb salvage
1. Introduction
Charcot neuroarthropathy (CN) is a progressive, non-infectious, destructive, inflammatory process of the foot and ankle and is a known complication of neuropathy. CN is associated with diabetes and usually occurs 10–15 years from diagnosis with current estimates of its prevalence ranging from 0.08% to as high as 13% for this population.1, 2, 3, 4, 5
CN destroys the bony architecture of the foot and ankle resulting in the devastating sequalae of deformity, pressure area formation, ulceration, infection, and amputation.3,5, 6, 7, 8 Once ulceration develops, the risk of infection and amputation rises twelve-fold.5 This greatly reduces overall quality of life and dramatically increases the morbidity and mortality for these patients (8). Approximately 40–60% of all amputations of the lower extremity are performed on patients with diabetes9 with the 5-year mortality rate for this population approximating 39%–68%.2
Unfortunately, patients with CN generally present late to an orthopaedic foot and ankle surgeon often with deformity, instability, tissue breakdown and/or osteomyelitis.10,11 Early recognition and intervention is imperative to prevent permanent deformity, ulceration, and amputation.7
The goal for patients with CN is limb salvage and quality of life. Most orthopaedic textbooks recommend nonoperative treatments for CN such as total contact casting and accommodative bracing however, most peer-reviewed clinical studies recommend early surgical correction of deformity. This is because accommodative bracing of deformity is often successful in limb salvage and infection resolution however is unsuccessful in improving the quality of life in affected individuals.8,12,13 Patients with a favorable outcome are defined as being ulcer and infection free at a minimum of 1 year, clinical stability at the surgical site, and ability to ambulate in the community with custom made shoes.8,12, 13, 14
The unstable or deformed CN ankle/hindfoot with or without ulceration is a major clinical challenge.7,10,11 CN at the ankle/hindfoot is progressive and often presents with a significant deformity and fragmentation of the talus and malleoli.2 Deformities associated with ankle/hindfoot are often multiplanar, resulting in sagittal, coronal and rotational malalignment and shortening due to collapse (15). The loss of alignment between the foot and ankle, and the protrusion of the medial or lateral malleoli, frequently leads to ulceration, osteomyelitis and major amputation4,13,16
2. Indications
The indication for surgical stabilization of the CN ankle/hindfoot is progressive deformity, dislocation and/or instability with risk of ulceration.1,6,13,17 Arthrodesis is the method of choice when surgically correcting CN deformities in this region. The choice of fixation largely depends on the presence of active infection, ulceration and bone quality.15
The use of circular frame external fixation (CFEF) in the setting of ankle/hindfoot CN is indicated in the following.
-
1.
Clinical and radiological nonplantigrade deformity, joint instability and pain with an open wound, active infection and/or osteomyelitis.13, 14, 17 Active infection is an contraindication to internal fixation18 (Figs. 1, Fig. 2)
-
2.
Severe bony deformity preventing large acute corrections that may compromise the soft tissue envelope. CFEF allows for gradual deformity corrections while maintaining the soft tissue envelope.
-
3.
Two stage deformity correction. CFEF is used to gradually correct the deformity while maintaining the soft tissue envelope in the first stage then the patient undergoes internal fixation in the second stage (Fig. 3).
-
4.
Revision CN Arthrodesis.2 Increased stability is gained from spanning the arthrodesis site with multiple levels of fixation, allowing for increased rigidity and support.
-
5.
Supplemental fixation to internal fixation.18 When internal fixation is tenuous due to bone stock, or if a periprosthetic fracture has occurred CFEF can be used to increase rigidity and support (Fig. 4).
-
6.
To allow weightbearing in patients who are unable to maintain non weight bearing after surgery (Fig. 4).
Figs. 1.
48 year old male with Charcot neuroarthropathy who sustained an ankle fracture then developed infection and osteomyelitis. a) b) X-rays demonstrating a vertical shear medial malleolus fracture. c) d) X-rays showing fixation with headless compression screws with circular frame external fixation to supplement the fixation while it unites. e) f) After the circular frame external fixator was removed the patient presented with dehiscence of the wound and osteomyelitis of the fracture site. CT scans shows evidence of infection with periosteal reaction. g) X-ray post debridement and placement of antibiotic cement spacer to control the infection. h) i) Circular frame external fixator used for definitive ankle fusion. j) k) weight bearing x-rays demonstrating fusion the ankle fusion in situ 2 years post injury.
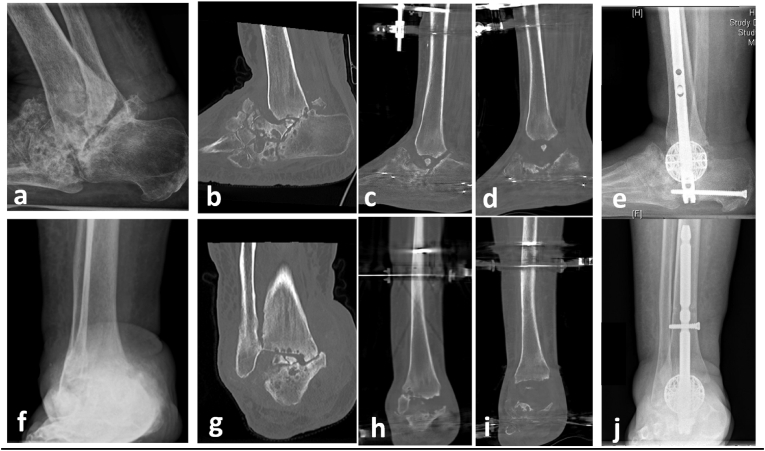
Fig. 2.
a-e) Xray and CT of a 60 year old male with hindfoot Charcot Neuroarthropathy with osteomyelitis. f-h) Xray and CT scan demonstrating circular frame external fixation in insitu for acute tibial-calcaneal fusion with use of intraosseous antibiotic bone substitute within the tibia and calcaneus. i) j) 12 weeks fluoroscopy post removal of circular frame external fixation demonstrating a tibial-calcaneal arthrodesis.
Fig. 3.
65 year old female with hindfoot Charcot Neuroarthropathy that underwent a 2 stage procedure for management. a) b) f) g) Preoperative Xray and CT demonstrating hindfoot Charcot neuropathy with almost complete loss of the talus and tibo-calcaneal abutment. c)h) CT scans with circular frame external fixation insitu prior to gradual distraction of the joint. d)i) CT scan with circular frame external fixation insitu after the gradual distraction of the joint was complete. The amount distracted was calculated with a hexapod program to plan for the space for the custom spherical spacer while maintaining the soft tissue envelope. e) j) X-rays demonstrating hindfoot nail and spherical spacer insitu to restore the height while stabilizing the hindfoot.
Figs. 4.
43 year old male with severe osteoporosis and neuropathy with a bi-malleolar ankle fracture. a) x ray demonstrating bimalleolar ankle fracture with evidence of previous midfoot Charcot correction and broken hardware. b) c) X-rays demonstrating acute hindfoot fusion with circular frame external fixation to supplement the internal fixation due to the poor bone stock and allow patient to weight bear earlier.
3. Management
The main treatment goal for CN of the ankle/hindfoot is to provide stability with a plantigrade foot that is shoeable, infection free and allow independent weight bearing. A functional, well aligned, stable ankle/hindfoot reduces the risk of ulcer formation, infection and ultimately prevents amputation while improving the patient’s overall quality of life.4,6,7,12,13,15,19, 20, 21, 22 The ability to ambulate in the community with commercially available diabetic footwear is a successful clinical outcome following operative reconstruction of CN deformity10
The basis of management of CN starts with a multidisciplinary team approach.23 These patients are often complex clinically with difficult social circumstances. In our unit these patients are reviewed by appropriate specialists such as Endocrinologists, Vascular surgeons, Plastic Surgeons, Anesthetists and Rehabilitation physicians preoperatively along with allied health services that include occupational therapist, social workers, podiatrists, physiotherapists, diabetic educators and dieticians.
Treatment of CN is demanding and challenges the surgeon’s skill and creativity. The historic treatment of CN has involved immobilization in a total contact cast during the active phase of the disease process, followed by accommodative bracing of the acquired deformity. This method provides favorable clinical outcomes for resolution of infection and limb salvage however patient reported outcomes have demonstrated that CN treated in this manner significantly impairs quality of life in and does not improve it.14
Surgical treatment ranges from exostectomy and ulcer excision to major reconstruction with corrective osteotomies, arthrodeses and soft-tissue balancing.24 Patients with ankle and hindfoot CN deformities are highly prone to ulceration due to prominent malleoli therefore more likely requiring early limb salvage surgery7,15
3.1. Non operative management
Non weightbearing in a total contact cast until the warmth and oedema of the area subsides is the classical treatment method for CN(8). However CN treated in this manner does not correct deformity, is associated with an approximately 2.7% annual rate of amputation, a 23% risk of requiring bracing for more than 18 months, and a 49% risk of recurrent ulceration.8,9 These results along with patient reported outcome of no improvement in quality of life suggest that improved methods of care are needed for patients with CN8,9,14
3.2. Operative management of ankle/hindfoot CN
Limb salvage surgery of the ankle/hindfoot presents a unique set of problems for the orthopaedic surgeon. Frequently there is extensive scar tissue, gross deformity, osteopenia, infection and soft tissue constraints.18 Single-stage correction of deformity using an intramedullary hindfoot arthrodesis nail is the most ideal form of treatment for patients with CN ankle/hindfoot deformity however due to infection or gross deformity this may not be possible.21
Limb salvage surgery during the acute fragmentation phase (Eichenholtz 1) of CN is not a contraindication for surgery and is often preferred in our unit. The soft tissue and bony deformity are less rigid and deformity correction is easier to obtain. There have been no issues in obtaining anatomical reduction, union or stability and is consistent with the published literature.6,15
Patients with valgus CN deformity (87%) are more likely to achieve a favorable clinical outcome followed by dislocation pattern (70.3%) and then varus deformity (56.3%).14
3.3. Internal fixation
Most recent literature would suggest that the best operative options is a retrograde-locked intramedullary nailing followed by CFEF, or a hybrid combination of a nonlocked intramedullary nail and a CFEF.10 Retrograde tibiotalocalcaneal nails, which also can address subtalar deformity, have demonstrated fusion rates of 70%–100% and limb salvage rates of 75%–100%8
3.4. Circular frame external fixation
Correction and stabilization of ankle/hindfoot deformities with a circular frame external fixation (CFEF) is effective and allows correction of the deformities, while avoiding the complications of internal fixation. CFEF provides stability and optimal biomechanical characteristics for healing and versatility in salvage ankle fusions by neutralizing rotational and translational forces,.18 It also allows for complete access to the soft tissue envelope and the ability for postoperative adjustments. This includes gradual deformity corrections which may have been acutely limited by soft tissue constraints. Furthermore, CFEF is not contraindicated with acute infection and allows for surgical management of infection while providing stability and deformity correction simultaneously.2 It enables early weight-bearing, care of soft tissues, wound healing, prevention of skin ulceration and avoidance of amputation17,25
3.5. CN in the ankle/hindfoot with acute infection
Often infection in CN is obvious with ulceration, discharge along with radiological and biochemical markers of infection. However, in the presence of previous infection it can be difficult to determine if infection has been completely irradicated. Bone biopsy is the gold standard for diagnosis in this setting with samples sent for culture and histology.3
The principles of the management for osteomyelitis are.
-
1.
Debridement of infected and necrotic bone and soft tissue whilst protecting the neurovascular structures.
-
2.
Antibiotic delivery, either locally or systemically.
-
3.
Skeletal stability.
-
4.
Dead space management.
-
5.
Soft tissue coverage.
There is evidence for the effectiveness of local antibiotics in treating osteomyelitis. The primary benefit achieved with local antibiotic delivery vehicles is the ability to obtain extremely high levels of local antibiotics without increasing systemic toxicity.3
4. Surgical technique
Adherence to the surgical principles of CN surgery, combined with preoperative planning provides the best chance of successful outcomes. In our practice where possible, a static frame is preferred over a gradual deformity correction as it simplifies care for the patient and surgeon while still maintaining alignment and compression (Fig. 5). In this patient population simplifying treatment is essential and often patients must remain in hospital for gradual deformity correction as compliance is often an issue.
Fig. 5.
Algorithm for surgical management of ankle/hindfoot charcot neuroarthropathy.
Principles of Charcot foot and ankle surgery.
-
1.
Place incisions on the convex or long side of the deformity.
-
2.
Restore the mechanical alignment via soft tissue releases and bony corrections.
-
3.
Shorten the skeletal segments to aid with reduction and to reduce the tension in the soft tissues.
-
4.
Provide stable fixation that spans the zone of Charcot neuroarthropathy.
4.1. Incision
Incision planning prior to surgery is essential to avoid having it placed too close to pins or wires which increases the risk of wound complications and pin site infections. A distance of 2 cm between an incision and wire or pin is usually sufficient. Varus deformity is approached via lateral incision and valgus deformity via medial incision in-order to utilize the soft tissue for closure and minimise any tension on the wound.
4.2. Positioning/setup
The patient is positioned supine with the leg elevated on a radiolucent foam block. No tourniquet is used.
The image intensifier is positioned on the side opposite to the incision used for the bony resection. This allows the bony preparation to be done easily under fluoroscopy.
4.3. Haemostasis
Intraoperative bleeding can be reduced with topical application of a mixture of 1; 10,000 adrenaline and tranexamic acid applied directly onto the tissue using a 25 gauge syringe or soaked gauze.
4.4. Soft tissue releases
The achilles tendon is lengthened via percutaneous incisions or via gastrocnemius recession with or without soleus lengthening. It is performed in almost all cases to correct hindfoot equinous and any calcaneal valgus or varus. A posterior midline incision is preferred for gastrocnemius recession to avoid any fixation wires such as a medial face wire particularly at the proximal ring.
Medial or lateral soft tissue release is required when a varus or valgus deformity is present. The muscle tendon unit lengthening can be varied according to the amount of correction required and the technique of surgical dosing is often used. A minor correction can be performed via intramuscular tenotomy, if a greater correction is required then a Z lengthening is used. Large deformities may require a transection of the tendon to allow correction.
Varus deformities require a medial release of the tibialis posterior, flexor digitorum longus and possibly neurovascular bundle mobilisation may be required. Valgus deformities often requires a release or lengthening of the peroneal tendons and the calcaneofibular ligament if a lateral malleolar resection is not performed. Both medial and lateral soft tissue releases can be performed through longitudinal incision just proximal to the ankle and just posterior to the malleolus.
4.5. Bony resection/joint preparation
Bony resection aims to restore the mechanical alignment in the frontal and sagittal plane and create coplanar surfaces of cancellous bone and maximising bone contact area. Articular cartilage and avascular bone are removed, and the fusion surfaces created using an osteotome under the image intensifier. The malleoli may need to be resected to allow bony apposition at the tibiotalar joint. When preparing the subtalar joint all three facets of the subtalar joint should be prepared to maximise the bone contact and the surface area of the fusion.
Shortening is recommended to reduce the tension on the soft tissue and wound which aids in wound healing by minimising the tension on the microvasculature.
4.6. Reduction/provisional fixation/bone grafting/wound closure
The tibiotalar and subtalar joints are reduced and provisionally fixated with 2 mm smooth wires or Steinmann pins. The position and alignment is confirmed on fluoroscopy. Bone graft is then inserted where needed and the wounds closed. Wounds that cannot be closed can be managed with negative pressure wound therapy (NPWT). We recommend closing all wounds prior to frame application as it prevents skewering the soft tissue with wires or pin in positions that decrease wound mobility thus making closure difficult. Furthermore, closure of the wound or application of NPWT with the frame insitu is difficult and time consuming.
4.7. Circular frame external fixator
The configuration of the frame consists of a two-ring tibial block connected with threaded rods and a foot plate closed distally to create a ring. The distance between the rings is approximately 10–15 cm and the distal ring is about 7–10 cm proximal to the tibiotalar joint. The diameter of the rings should allow two fingers to pass between the rings and the leg.
Wire and pin fixation in the tibia, fibula, ankle and foot is via safe corridors defined previously26,27 Fixation in the tibia can be with wires or half pins. Our preference is a combination of wires and/or half pins with one point of fixation per 20 kg body mass in the tibia. In our experience this rough guide helps us estimate the amount of supplemental fixation required in the tibia and prevents wire/pin site loosening, breakage and infection. Wires are recommended for fixation in the foot. It is important to maximise the angle between fixation elements and to use rings that are appropriately sized to give the frame maximum stability which reduces the risk of loosening and complications. Insertion of wires or half pins should be done with intermittent drilling and cooling to minimise the risk of thermal necrosis.
A minimum of two fixation points per ring is required and stability can be increased by increasing the number of fixation elements per ring. This may be required when dealing with obese patients.
Once the frame has been applied then the reduction is confirmed on fluoroscopy. The provisional fixation is removed and compression is applied through the frame.
4.8. Circular frame external fixation and infection
CFEF is a valuable tool when treating infection in ankle/hindfoot CN. It provides stable fixation and avoids internal fixation at the zone of infection. Surgical treatment in this scenario requires adherence to both the principles of the management of osteomyelitis along with the principles of Charcot foot and ankle surgery as discussed above.
Two stage treatment of osteomyelitis is a well-recognised technique. This involves debridement of necrotic and infected bone and soft tissue coupled with insertion of an antibiotic impregnated polymethylmethacrylate (PMMA) spacer to provide local antibiotic delivery and dead space management. A static frame can be applied during the first stage to provide skeletal stability and aid with soft tissue management. Alternatively, provisional reduction can be performed with large wires or Steinman pins and bracing or plaster until the second stage of surgery is performed. After the initial first stage systemic antibiotics are given based on the intraoperative cultures and the advice of an infectious diseases specialist. Once the course of systemic antibiotics has completed a bone biopsy is performed two weeks after the systemic antibiotics have been ceased to exclude ongoing infection. Second stage surgery involves removal of the PMMA spacer, bony preparation of the fusion surfaces and definitive reduction and compression as required through the static frame.
Single stage surgery with resection of the infected bone, deformity correction and application of the static frame followed by systemic antibiotics has shown good results.28 The use of absorbable bone substitutes loaded with antibiotic is often used with single stage surgery with the advantage of high dose local antibiotic delivery and dead space management but without the need for a second operation to remove a spacer. This allows for single stage definitive surgery with high dose local antibiotic delivery to the site of infection and has the advantage of reducing the amount of time for treatment, number of operations and patient immobility (Figs. 1, Fig. 2).
Absorbable bone graft substitute with calcium sulphate and hydroxyapatite loaded with gentamicin or vancomycin can be delivered directly into the infected bone via a silo technique. It can also be used as paste or pellets to fill any dead space. Under fluoroscopy multiple drill holes using a 3.5 mm drill can be made in the infected bone and the drill holes are injected with the antibiotic loaded bone graft substitute while it is in paste form. As it hardens to putty, bone defects can be filled with it. As the antibiotic loaded bone graft substitute hardens, pellets can be formed to fill any other dead space between the bone surfaces.
Wound closure after debridement and provisional fixation is desirable if possible. In the case that the wound is not able to be closed primarily then NPWT can be used until the wound heals. Graft or flap coverage of the wound is a good alternative when those services are available.
5. Hybrid fixation
External fixation can be used simultaneously with internal fixation or it can be used to correct deformity prior to the insertion of internal fixation.
Hybrid fixation can be used to supplement any form of internal fixation in patients in whom there is concern regarding the quality of the bone for fixation or compliance to remain non weight bearing. The hindfoot fusion with internal fixation is performed in the usual fashion and the wound is closed. A static fixator as described above is then applied but the distal ring will need to be above the internal fixation. When inserting the wires or pins for the external fixator it is important to place them so that there is no contact between the wires or pins and the internal fixation. This is to help avoid deep infection of the internal hardware should a pin site infection develop. The frame is left on as long is required for its purpose and then removed as soon as possible.26,27 (Fig. 4).
Gradual correction using external fixation can be used in situations where the soft tissue is severely contracted, or a large wound exists with soft tissue infection and requires treatment prior to surgery. Alternatively, it can be used to stretch the soft tissue when planning to use a bone spacer to regain length with definitive fixating such as an intramedullary nail. (Fig. 3). A two ring tibial block and foot plate are applied in the usual method. Hexapod struts are used between the tibial ring block and the foot plate. A computer generated program provides the program for the desired correction. Once the planned correction has been attained then the frame is removed, and the definitive surgery performed in the same sitting.
5.1. Post-operative management
Following surgery, the usual care such as elevation, prophylactic antibiotics and thromboembolic prophylaxis and physiotherapy is provided. The expertise of an endocrinologist is recommended to keep tight peri-operative glycaemic control as this has been shown to reduce complications (23). A wound review and pin site dressing change is done at 48 h. Non weight bearing is recommended until the wounds have healed.
After discharge, pin site care is monitored via community nursing where possible and regular review in the outpatient clinic is mandatory. This allows regular review of the wound, pin site and the frame stability. X-rays are used to monitor progress to healing and the frame adjusted as required to promote healing.
Three months after surgery the frame is removed if the bone healing is satisfactory. The patient is then allowed to weight bear with a boot and crutches for another three months. During this phase oedema management is helpful and referral for definitive custom shoe wear should be made. At six months post-surgery patients can transition into custom shoe wear with a rocker sole.
5.2. Evidence and outcomes
The evidence in the literatures for the use CFEF in ankle/hindfoot CN is variable with no high level studies and most retrospective in nature. However, the consensus goal of all treatment methods is for prevention of amputation and providing a functional limb.
Retrograde arthrodesis nails have been reported to have excellent salvage rates of up to 100%. While CFEF has similar reports of excellent results of up to 92%–96%.1,2,15,29 Overall, reconstruction of ankle and hindfoot CN should strive for limb salvage rates approximating 90%15 with the aim for independent ambulation wearing a custom made shoe.
Ettinger reported in a cohort of 48 patients with CN treated with a Tibio-talo-calcaneal or Talo-Calcaneal fusion with internal or external fixation led to promising results. Internal fixation should be preferred when no indications of ulcer or infection are present.22 84.2% had achieved bone union after external fixation and 100% after intramedullary nail arthrodesis (22).
Fabrin reported results of Charcot ankle arthrodesis with external fixation in 12 feet of 11 patients (seven tibiotalar, five tibiocalcaneal) over a period of 12 years. Union was obtained in six ankles, and the other six had stable non-union (one tibiotalar, five tibiocalcaneal11
El-Gafary reported a 100% fusion rate in 20 patients and a mean time to regular shoe wear at an average of 26.5 weeks after use of an Ilizarov frame for an average span of 18 week25
Zarutsky et al. reported the results of circular wire external fixation in 43 cases of salvage ankle arthrodesis. Thirty-three patients (80.5%) went on to achieve a solid fusion or stable pseudarthrosis, the major complication rate was 51.2%, including 3 below-knee amputations (7.3%), 7 unstable non-union (17.1%), 7 cases of osteomyelitis and/or deep-space infection (16.3%), 3 malunions (7.3%), and 2 tibial stress fractures (18).
Elalfy found an Ilizarov external fixator resulted in a better union rate than intramedullary nailing. However, the complications with external fixation were higher than those with intramedullary nailing30
Pinzur et al. reported in a cohort of 178 patients a of limb salvage rate of 95.7%. In their study, 45 of 73 patients (62%) who had an ulcer achieved healing after, however this paper included patients with CN of the forefoot and hindfoot14,21
Wukich et al. reported his experience with circular fixation in 33 diabetic patients and compared them with a control group of 23 nondiabetic patients. They found that patients with diabetes mellitus carried a seven-fold risk of postoperative complication. They concluded that circular fixation, especially in a high-risk population, carries with it an inherent risk of postoperative complications24
6. Complications
Complications are common in patients undergoing CN reconstruction of the ankle and hindfoot. Overall complication rate of 43% in patients with diabetes who underwent TTC arthrodesis have been reported (15). 30% of patients experienced a superficial or deep infection, and 25% experienced a non-infectious complication (non-union, malunion or hardware failure). Additional unplanned surgery was required in 34% of the diabetic patients. Despite this high complication rate, overall patient satisfaction was 80%, and limb salvage was achieved in 97% of patients15
CFEF’s most common complication is pin site infection.24,31 Pin site infection is associated with loosening and may be related to the patients lack of proprioception and can be decreased with a period of non-weight bearing.2,22 Diabetics have a 7-fold risk for any wire complication compared to patients without diabetes.19 “Other complication associated with CFEF application include nerve or vessel injury, tendon impingement, skin traction, joint stiffness, oedema, wire breakage, fracture, and pain. These can occur during application, during the postoperative course, and/or after removal of the external fixator” (19). While these complications are common, they generally do not affect the ultimate outcome.15
Although bony union is preferred a stable fibrous union is sufficient to achieve a positive functional result, and, therefore is not a complication and an accepted outcome for this procedure if achieved (1,22).
6.1. Discussion/authors experience
Surgical success is defined preoperatively with a multidisciplinary team approach and working in conjunction with the patient to meet the same realistic goal of functional ambulation with a stable, shoeable foot (2,23). Understanding your patients’ needs along with their ability to comply with post-operative restrictions will also limit complications.
Since 2018 we have used CFEF for the management of ankle/hindfoot CN for 10 patients with a follow-up period of 2 years. 5 patients were males and 5 females with an average age of 59.1 and Hba1c of 9.65 at time of frame application. 8 patients presented with deformity and infection, 1 required a 2 stage correction with a CFEF and 1 patient required CFEF to supplement internal fixation. The average time to union was 24.4 weeks with the CFEF duration averaging 16.6 weeks. 7 patients achieved a bony union, 2 patients achieved an asymptomatic fibrous union, and 1 patient had a symptomatic non-union. There were no major amputations associated with this group of patients (Table 1).
Table 1.
Demographics of patients with ankle/hindfoot Charcot managed with Circular frame external fixator.
| Patient | Sex | Age | Hba1c | Frame Duration (weeks) | Union Type | Infection Status | Clinically Stale | Shoe Type | Ambulant | Ambulation Distance (m) | Complications |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 65 | 12.0 | 29.0 | Fibrous | Free | Yes | Custom | Yes | 5–10 | Frame Adjustment Required/Pin site Infection |
| 2 | M | 70 | 7.6 | nil | Non- Union | Free | Yes | N/A | Yes | 10–50 | Frame Adjustment Required/Pin site Infection |
| 3 | M | 52 | 11.0 | 36.0 | Bony | Free | Yes | Custom | Yes | 50–100 | Frame Adjustment Required/Pin site Infection |
| 4 | F | 57 | 12.0 | 14.0 | Bony | Free | Yes | Custom | Yes | 5–10 | Nil |
| 5 | F | 70 | 11.0 | 36.0 | Fibrous | Free | Yes | Custom | Yes | 5–10 | Frame Adjustment Required/Pin site Infection |
| 6 | F | 59 | 7.0 | 30.0 | Bony | Free | Yes | Custom | Yes | 25–50 | Nil |
| 7 | F | 64 | N/A | 23.0 | Bony | Free | Yes | Custom | Yes | 50–100 | Nil |
| 8 | M | 43 | N/A | 18.0 | Bony | Free | Yes | Custom | Yes | 5–10 | Nil |
| 9 | F | 51 | 10.5 | 20.0 | Bony | Free | Yes | Custom | Yes | 50–100 | Peri-Implant Fracture Requiring CFEF |
| 10 | M | 60 | 6.1 | 14.0 | Bony | Free | Yes | Custom | Yes | >500 | Nil |
Using the parameters for favorable outcomes, all 10 patients remained infection free, 9/10 were able to ambulate independently with custom made shoes and 9/10 patients were clinically stable.
Salvage ankle/hindfoot procedures are technically demanding with an appreciably steep learning curve. We recommend that the surgeon should be experienced with all surgical approaches and fixation methods for the ankle and hindfoot. Respecting the soft tissue along with detailed pre-operative planning is the main dictating factor for good outcomes. Previous surgeries, tissue quality, infections, perfusion, and deformities must be taken into consideration prior to any operative intervention. Incisions should utilize old scars, excise ulcers and be placed on the tension side of the deformity and avoid pin or wires that will be used to fixate the CFEF.
Our preference is intramedually fixation however if CFEF is indicated we find it advantageous by providing rigid stabilization with the ability to gradually correct deformity while still respecting the soft tissue. It can even be used in situations such as severe scarring and inadequate skin coverage while allowing to the patient to weight bear early (17). Our main indication for CFEF in the setting of ankle/hindfoot CN is infection and we employ best practice with a combination of aggressive surgical debridement, local and systemic antibiotic therapy and deformity correction with external fixation ideally in one stage.28
Declaration of competing interest
BM Conflict of interest – Dr Brian Martin has consultancy agreements with Orthofix and Bone Support. He also owns shares in BoneSupport.
JC Conflict of interest – none declared.
Contributor Information
Brian Martin, Email: admin@drbrianmartin.com.au.
Jason Chow, Email: drjasonchoworthopaedics@gmail.com.
References
- 1.DeVries J.G., Berlet G.C., Hyer C.F. A retrospective comparative analysis of Charcot ankle stabilization using an intramedullary rod with or without application of circular external fixator—utilization of the retrograde Arthrodesis intramedullary nail database. J Foot Ankle Surg. 2012 Jul 1;51(4):420–425. doi: 10.1053/j.jfas.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 2.Conway J.D. Charcot salvage of the foot and ankle using external fixation. Foot Ankle Clin. 2008 Mar 1;13(1):157–173. doi: 10.1016/j.fcl.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 3.Donegan R., Sumpio B., Blume P.A. Charcot foot and ankle with osteomyelitis. Diabet Foot Ankle. 2013 Jan 1;4(1):21361. doi: 10.3402/dfa.v4i0.21361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yousry A., Abdelhady A. Management of diabetic neuropathic ankle arthropathy by arthrodesis using an Ilizarov frame. Acta Orthop Belg. 2010 Dec 1;76:821–826. [PubMed] [Google Scholar]
- 5.Wukich D.K., Raspovic K.M., Hobizal K.B., Rosario B. Radiographic analysis of diabetic midfoot Charcot neuroarthropathy with and without midfoot ulceration. Foot Ankle Int. 2014 Nov 1;35(11):1108–1115. doi: 10.1177/1071100714547218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.B B., Vg Cc. Arthrodesis of the Charcot foot and ankle. Clin Podiatr Med Surg. 2004 Apr 1;21(2):271–289. doi: 10.1016/j.cpm.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 7.Schneekloth B.J., Lowery N.J., Wukich D.K. Charcot neuroarthropathy in patients with diabetes: an updated systematic review of surgical management. J Foot Ankle Surg. 2016 May 1;55(3):586–590. doi: 10.1053/j.jfas.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Strotman P.K., Reif T.J., Pinzur M.S. Charcot arthropathy of the foot and ankle. Foot Ankle Int. 2016 Nov 1;37(11):1255–1263. doi: 10.1177/1071100716674434. [DOI] [PubMed] [Google Scholar]
- 9.Saltzman C.L., Hagy M.L., Zimmerman B., Estin M., Cooper R. How effective is intensive nonoperative initial treatment of patients with diabetes and Charcot arthropathy of the feet? Clin Orthop Relat Res. 2005 Jun;435:185–190. doi: 10.1097/00003086-200506000-00026. [DOI] [PubMed] [Google Scholar]
- 10.Harkin E.A., Schneider A.M., Murphy M., Schiff A.P., Pinzur M.S. Deformity and clinical outcomes following operative correction of Charcot ankle. Foot Ankle Int. 2019 Feb 1;40(2):145–151. doi: 10.1177/1071100718805076. [DOI] [PubMed] [Google Scholar]
- 11.Fabrin J., Larsen K., Holstein P.E. Arthrodesis with external fixation in the unstable or misaligned Charcot ankle in patients with diabetes mellitus. Int J Low Extrem Wounds. 2007 Jun 1;6(2):102–107. doi: 10.1177/1534734607302379. [DOI] [PubMed] [Google Scholar]
- 12.Pinzur M. Surgical versus accommodative treatment for Charcot arthropathy of the midfoot. Foot Ankle Int. 2004 Aug 1;25(8):545–549. doi: 10.1177/107110070402500806. [DOI] [PubMed] [Google Scholar]
- 13.Pinzur M.S. Treatment of ankle and hindfoot Charcot arthropathy. Foot Ankle Clin. 2020 Jun 1;25(2):293–303. doi: 10.1016/j.fcl.2020.02.010. [DOI] [PubMed] [Google Scholar]
- 14.Pinzur M.S., Schiff A.P. Deformity and clinical outcomes following operative correction of Charcot foot: a new classification with implications for treatment. Foot Ankle Int. 2018 Mar 1;39(3):265–270. doi: 10.1177/1071100717742371. [DOI] [PubMed] [Google Scholar]
- 15.Wukich D.K., Raspovic K.M., Hobizal K.B., Sadoskas D. Surgical management of Charcot neuroarthropathy of the ankle and hindfoot in patients with diabetes. Diabetes Metabol Res Rev. 2016;32(S1):292–296. doi: 10.1002/dmrr.2748. [DOI] [PubMed] [Google Scholar]
- 16.Paola L.D., Ceccacci T., Ninkovic S., Sorgentone S., Marinescu M.G. Limb salvage in Charcot foot and ankle osteomyelitis: combined use single stage/double stage of arthrodesis and external fixation. Foot Ankle Int. 2009 Nov 1;30(11):1065–1070. doi: 10.3113/FAI.2009.1065. [DOI] [PubMed] [Google Scholar]
- 17.Karapinar H., Sener M., Kazimoglu C., Akgun U. Arthrodesis of neuropathic ankle joint by Ilizarov fixator in diabetic patients. J Am Podiatr Med Assoc. 2009 Jan 1;99(1):42–48. doi: 10.7547/0980042. [DOI] [PubMed] [Google Scholar]
- 18.Zarutsky E., Rush S.M., Schuberth J.M. The use of circular wire external fixation in the treatment of salvage ankle arthrodesis. J Foot Ankle Surg. 2005 Jan 1;44(1):22–31. doi: 10.1053/j.jfas.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 19.Wukich D.K., Belczyk R.J., Burns P.R., Frykberg R.G. Complications encountered with circular ring fixation in persons with diabetes mellitus. Foot Ankle Int. 2008 Oct 1;29(10):994–1000. doi: 10.3113/FAI.2008.0994. [DOI] [PubMed] [Google Scholar]
- 20.Vasukutty N., Jawalkar H., Anugraha A., Chekuri R., Ahluwalia R., Kavarthapu V. Correction of ankle and hind foot deformity in Charcot neuroarthropathy using a retrograde hind foot nail—the Kings’ Experience. Foot Ankle Surg. 2018 Oct 1;24(5):406–410. doi: 10.1016/j.fas.2017.04.014. [DOI] [PubMed] [Google Scholar]
- 21.Siebachmeyer M., Boddu K., Bilal A. Outcome of one-stage correction of deformities of the ankle and hindfoot and fusion in Charcot neuroarthropathy using a retrograde intramedullary hindfoot arthrodesis nail. The Bone & Joint Journal. 2015 Jan 1;97-B(1):76–82. doi: 10.1302/0301-620X.97B1.34542. [DOI] [PubMed] [Google Scholar]
- 22.Ettinger S., Plaass C., Claassen L., Stukenborg-Colsman C., Yao D., Daniilidis K. Surgical management of Charcot deformity for the foot and ankle—radiologic outcome after internal/external fixation. J Foot Ankle Surg. 2016 May 1;55(3):522–528. doi: 10.1053/j.jfas.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 23.King J.T., Goulet J.L., Perkal M.F., Rosenthal R.A. Glycemic control and infections in patients with diabetes undergoing noncardiac surgery. Ann Surg. 2011 Jan;253(1):158–165. doi: 10.1097/SLA.0b013e3181f9bb3a. [DOI] [PubMed] [Google Scholar]
- 24.Wukich D.K., Lowery N.J. The role of circular fixation in the treatment of Charcot foot. Current Orthopaedic Practice. 2010 Jun;21(3):240–244. [Google Scholar]
- 25.El-Gafary K.a.M., Mostafa K.M., Al-adly W.Y. The management of Charcot joint disease affecting the ankle and foot by arthrodesis controlled by an Ilizarov frame. J Bone Joint Surg. 2009 Oct 1;91-B(10):1322–1325. doi: 10.1302/0301-620X.91B10.22431. [DOI] [PubMed] [Google Scholar]
- 26.Kirienko A., Villa A., Calhoun J.H., Kirienko A. Marcel Dekker; New York: 2004. Ilizarov Technique for Complex Foot and Ankle Deformities. [Google Scholar]
- 27.Catagni M.A. second ed. 2003. Atlas for Insertion of Transosseous Wires and Half-Pins Ilizarov Method. [Google Scholar]
- 28.Pinzur M.S., Gil J., Belmares J. Treatment of osteomyelitis in Charcot foot with single-stage resection of infection, correction of deformity, and maintenance with ring fixation. Foot Ankle Int. 2012 Dec 1;33(12):1069–1074. doi: 10.3113/FAI.2012.1069. [DOI] [PubMed] [Google Scholar]
- 29.Caravaggi C.M.F., Sganzaroli A.B., Galenda P. Long-term follow-up of tibiocalcaneal arthrodesis in diabetic patients with early chronic Charcot Osteoarthropathy. J Foot Ankle Surg. 2012 Jul 1;51(4):408–411. doi: 10.1053/j.jfas.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 30.ElAlfy B., Ali A.M., Fawzy S.I. Ilizarov external fixator versus retrograde intramedullary nailing for ankle joint arthrodesis in diabetic Charcot neuroarthropathy. J Foot Ankle Surg. 2017 Mar 1;56(2):309–313. doi: 10.1053/j.jfas.2016.10.014. [DOI] [PubMed] [Google Scholar]
- 31.Tomczak C., Beaman D., Perkins S. Combined intramedullary nail coated with antibiotic-containing cement and ring fixation for limb salvage in the severely deformed, infected, neuroarthropathic ankle. Foot Ankle Int. 2019 Jan 1;40(1):48–55. doi: 10.1177/1071100718800836. [DOI] [PubMed] [Google Scholar]