Abstract
Primary carcinoma of the ureteral stump following a radical nephrectomy is rare, and it is even rarer that the cause of the nephrectomy is renal cell carcinoma (RCC). Treatment by complete ureterectomy with a bladder cuff is considered as the standard treatment. We report a case of a 70-year-old female with urothelial carcinoma with glandular differentiation that occurred in the ureteral stump after nephrectomy for left RCC. We performed a novel technique of pure laparoscopic resection of the ureteral stump with a bladder cuff.
Keywords: Renal cell carcinoma, Post nephrectomy, Ureteral stump, Urothelial carcinoma, Pure laparoscopic resection, Bladder cuff
Introduction
A primary carcinoma of the ureteral stump following a radical nephrectomy is rare, and it is even rarer that the cause of the nephrectomy is renal cell carcinoma (RCC). Treatment by complete ureterectomy with a bladder cuff is considered as the standard treatment. Generally, laparoscopic surgery has the advantage of being minimally invasive; however, the suturing technique is particularly difficult. We report a case of a 70-year-old female with urothelial carcinoma (UC) with glandular differentiation that occurred in the ureteral stump after nephrectomy for left RCC. We performed a novel technique of pure laparoscopic resection of the ureteral stump with a bladder cuff.
Case report
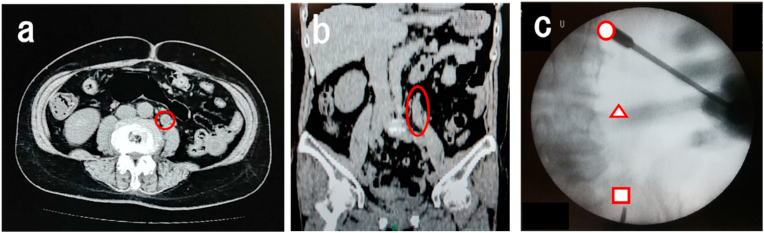
A 70-year-old female. Open nephrectomy was performed for left RCC of cT1bN0M0, and the histopathological diagnosis was clear cell-type RCC. Eleven years later, follow-up computed tomography showed residual ureteral dilatation associated with a mass lesion (Fig. 1a and b). She had no symptom and urine cytology showed no malignant findings. Ureteroscopy revealed a stenosis distal to the tumor site that could not be reached (Fig. 1c).
Fig. 1.
a) CT axial view shows the dilation of the ureteral stump at the umbilicus level. b) CT coronal view shows the longitudinal extension of the ureteral stump. c) Fluoroscopic findings during ureteroscopy. The circle represents the upper end of the lesion on CT. The triangle represents the height of the umbilicus. The triangle represents the limit that the ureteroscope reaches.
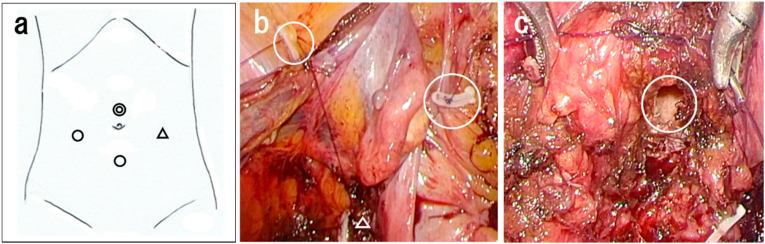
We performed pure laparoscopic resection of the ureteral stump with a bladder cuff. The patient was placed in a 15-degree head-down lithotomy position. A 12-mm camera port at 3 cm superior to the umbilicus, a 12-mm port between the pubis and the camera port, a 12-mm assistant port on the right outside, and a 5-mm port on the left outside were placed (Fig. 2a). The left external iliac artery was identified, and the left residual ureter was identified during the incision of the peritoneum. At first, we dissected the ureter towards the bladder. Before starting partial bladder resection, we dissected the cranial ureter. At the cranial end of the intersection with the common iliac artery, the residual ureter was dilated by the tumor. The cranial end of the residual ureter was dissected, and the entire ureter was released to the bladder. We pulled the bladder by suturing the bladder muscle layer just above the intramural ureter and the upper peritoneum with 3-0 monocryl (Fig. 2b). After partial bladder resection, we continuously sutured the bladder with 2-0 V-Loc (Fig. 2c). We performed a leak test and placed the drain.
Fig. 2.
a) Port placement. A 12-mm camera port at 3 cm superior to the umbilicus, a 12-mm port between the pubis and the camera port, a 12-mm assistant port on the right outside, and a 5-mm port on the left outside were placed. b) The circles represent the fixation of the support thread to the peritoneum. The bladder muscle layer is threaded at the triangle. c) The circle represents the partial bladder resection. Continuous suture is performed under a laparoscope.
There were no intraoperative complications. Total operating time was 3 hours and 6 minutes, insufflation time was 2 hours and 38 minutes, and there was little blood loss. We removed the drain on day 4. We performed cystography on day 6, and no leakage from the bladder cuff was observed. We removed the urethral catheter on day 7, and she was discharged from the hospital on day 8.
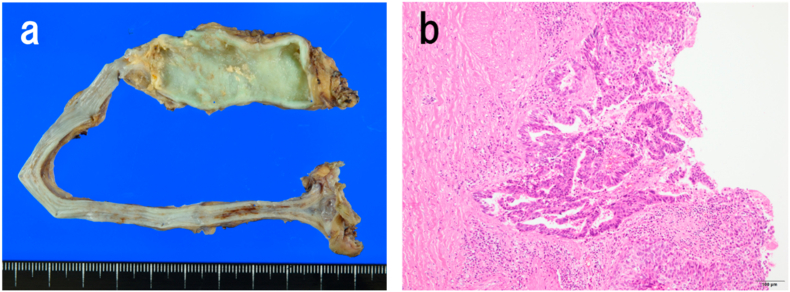
There was fluid in the 4.5 cm × 2.5 cm dilated ureter on the blind side, and a cytological test was positive. There was wall thickening, but no obvious mass was found (Fig. 3a). The histology was positive for invasive UC with glandular differentiation, pT3, INFb, ly0, v1, u-lt0, and RM0 (Fig. 3b). We recommended adjuvant chemotherapy, but she refused due to social background reasons. She was free of disease in the following 6 months.
Fig. 3.
a) Macro finding shows the 4.5 cm × 2.5 cm dilated ureter on the blind side. b) Pathological specimen of the left ureteral stump reveals high-grade urothelial carcinoma with glandular differentiation (hematoxylin & eosin staining, × 100).
Discussion
The incidence of primary carcinoma of the ureteral stump following nephrectomy is quite rare. Malek et al. reported that 4 of 4883 patients (0.08%) who underwent nephrectomy for benign renal disease, presented with a ureteral stump carcinoma.1 It is extremely rare that the reason of nephrectomy is RCC with only 10 cases reported by 2019.2 Rink et al. reported that 398 of 1648 patients (24.2%) had histological upper tract UC variants, and glandular differentiation was 4.4%.3 None of the 10 previously reported cases were associated with glandular differentiation.
When a tumor develops in the ureteral stump after nephrectomy due to RCC, it is necessary to distinguish between RCC and UC. In 2020, Oserowsky et al. reported the 57th case of ureteral stump metastasis of RCC4; thus, the frequency is lower in UC than RCC metastasis. Asymptomatic gross hematuria was the chief complaint of ureteral stump tumor. In diagnosis, urinary cytology is not useful because there is no urinary flow from the ureteral stump. In the present study, no gross hematuria was observed and urinary cytology was negative. Although ureteroscopy is useful, it should be used for diagnosis in combination with imaging. If there is a stenosis distal to the lesion, as in this patient, it may be overlooked.
Treatment by complete ureterectomy with a bladder cuff is considered as the standard treatment.1 In a systematic review of UC in the ureteral stump, 24 patients underwent open complete ureterectomy, and none had laparoscopic surgery.5 This is the first case of a residual ureterectomy being performed by pure laparoscopic surgery. In the majority of cases (94%), the malignancy was located in the lower 1/3 of the ureter5; therefore, this may be a factor that makes it difficult to perform laparoscopic surgery. Bourdoumis suggested that laparoscopic surgery was an option when performed by experienced surgeons in high-volume centers.5
Regarding the surgical procedure, it is better to perform a bladder-side dissection first to apply traction to the ureter. When the ureter is removed, the edge of the bladder wall falls into the bladder, so it is important to first suture the bladder muscle layer and the peritoneum. The bladder needs to be sutured in a narrow space under a laparoscopy. If the lesion is on the cranial side, pure laparoscopic resection could be a minimally invasive and useful treatment option.
Conclusion
We reported a case of UC with glandular differentiation that occurred in the ureteral stump after RCC. We performed a novel technique of pure laparoscopic resection of the ureteral stump with bladder cuff. If the lesion is on the cranial side, pure laparoscopic resection may be a minimally invasive and useful treatment option.
Footnotes
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
Masahiro Katsui, Email: katsui.masahiro@gmail.com.
Tomohiro Iwasawa, Email: tiwasawa217@gmail.com.
Sotaro Kitaoka, Email: tapioka40536@gmail.com.
Orikasa Hideki, Email: orihhym@js6.so-net.ne.jp.
Seiya Hattori, Email: seihat0109@hotmail.com.
Satoshi Hara, Email: uro.s-hara.0909@kmh.gr.jp.
References
- 1.Malek R.S., Moghaddam A., Furlow W.L. Symptomatic ureteral stumps. J Urol. 1971;106(4):521–528. doi: 10.1016/s0022-5347(17)61332-6. [DOI] [PubMed] [Google Scholar]
- 2.Masago T., Naka T., Yoshida H. Primary tumor of the ureteral stump after a radical nephrectomy for renal cell carcinoma: case report and literature review. Int Cancer Conf J. 2019;8(3):126–129. doi: 10.1007/s13691-019-00369-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rink M., Robinson B.D., Green D.A. Impact of histological variants on clinical outcomes of patients with upper urinary tract urothelial carcinoma. J Urol. 2012;188(2):398–404. doi: 10.1016/j.juro.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 4.Oserowsky A., Allison D., Weinstein S. Metastasis of renal cell carcinoma to the distal ureteral stump beyond recommended baseline surveillance duration. Urol Case Rep. 2020;19(32):101266. doi: 10.1016/j.eucr.2020.101266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bourdoumis A., Syed I., Soosay G. Transitional cell carcinoma of the ureteric stump: a systematic review of the literature. Urol Int. 2013;91(2):170–174. doi: 10.1159/000349884. [DOI] [PubMed] [Google Scholar]