Abstract
Background
HIV antibody testing has been included in the National Health and Nutrition Examination Survey, for ages 18–49 since 1999 and for ages 18–59 years since 2009 enabling estimation of trends in HIV prevalence as part of national surveillance in the U.S. household population. Self-reported HIV testing and antiretroviral (ARV) use was also included in the survey since 1999.
Setting
A continuous household-based probability sample of the U.S. population.
Methods
From 1999–2018, 29,020 participants age 18–49 years were tested for HIV antibody and 34,092 participants age 18–59 years were asked about self-report of any previous HIV testing.
Results
HIV prevalence was 0.41% among those aged 18–59 in 2009–2018 with a non-significant trend over time among those aged 18–49 years from 1999–2002 to 2015–2018. However, significant declines in prevalence were seen among those aged 18–39 years (0.37% to 0.11%), women (0.22% to 0.06%) and non-Hispanic black persons (2.14% to 0.80%). Participants age aged 18–39 self-reported a decline in HIV testing while those aged 40–49 and 50–59 years, non-Hispanic black persons and women reported an increase in getting a HIV test. Prevalence of infection and self-reported history of HIV testing varied by demographic and risk groups. HIV testing among HIV positive persons was 83.9%. ARV therapy among those HIV positive was under 50%.
Conclusion
Though total HIV prevalence and previous self-reported HIV testing remained stable for the last 20 years, there were significant declines in age and demographic subgroups. Prevalence for both outcomes varied by demographic and risk variables.
Keywords: HIV serology, National survey, self-reported HIV testing
Introduction
The Centers for Disease Control and Prevention (CDC) has been collecting surveillance data on HIV infection since the onset of the HIV/AIDS epidemic in the United States (U.S.) in 1981. HIV Surveillance reports are based on diagnosed cases of HIV infection. In the latest HIV Surveillance Report, the percentage of diagnosed infections among persons living with HIV at year-end 2018, compared with 2014, decreased while the prevalence of people living with HIV/AIDS incresed1.
The National Health and Nutrition Examination Survey (NHANES) is one of a series of health-related surveys conducted by CDC’s National Center for Health Statistics (NCHS)2. NHANES provides surveillance data to monitor the health and nutritional status of the U.S. household population and the HIV data in this report are based on the presence of HIV antibody in the general population. Results of serologic testing and self-reported history of HIV testing from earlier NHANES surveys has been previously published3–5. This report presents twenty-year trends from 1999 through 2018 of HIV prevalence on adults aged 18–49 and self-report of ever having had an HIV test on adults aged 18–59 and examines associations with demographic and risk factor data for 2009–2018 combined among adults aged 18–59. The demographic characteristics of those using anti-retroviral (ARV) treatment among people living with HIV were also examined.
METHODS
Sample design
The NHANES are a series of cross-sectional surveys designed to provide national statistics on the health and nutritional status of the general household population of the United States6. The survey consists of household interviews, a standardized physical examination and the collection of biologic samples in Mobile Examination Centers (MECs). The sampling plan for the survey is a stratified multistage probability cluster design that provides a sample of the 50 states and the District of Columbia7. In 1999, NHANES became a continuous survey with data released every two years. Data files from multiple cycles can be combined to produce more statistically reliable estimates.
In the NHANES sample, Non-Hispanic black persons in all survey cycles, Hispanic persons starting in 2007 and non-Hispanic Asian persons starting in 2011 were sampled at higher frequencies to obtain more reliable estimates. All adult participants provided informed consent, and the NHANES protocol was approved by the National Center for Health Statistics (NCHS) Research Ethics Review Board7.
For the NHANES cycles from 2009 to 2018, 64.6% of sampled persons ages 20–59 were interviewed (response rate ranged from 78.3% in 2009–2010 to 49.0% in 2017–2018) and 96.5% of those interviewed were also examined (response rate ranged from 97.8% in 2009–2010 to 95.0% in 2017–2018). To reduce the potential for nonresponse bias, base weights are adjusted for nonresponse at each stage of the survey (screening, interview, and examination)2.
Outcome measures
Serologic testing for HIV in NHANES was conducted on those aged 18–49 years from 1999–2008. Starting in 2009, the age range for HIV testing was expanded to include persons aged 50–59 years to accommodate the aging demographics of HIV prevalence post routine use of antiretroviral combination treatment.
Blood samples collected between 1999 and 2018 have been screened following different HIV testing algorithms. From 1999 to June 2004, samples were initially tested with HIV-1/HIV-2 Peptide Enzyme Immunoassay (EIA) (Bio-Rad Laboratories, Redmond, WA) for HIV antibody detection. From July 2004 through 2014 the antibody screening assay changed to the Bio-Rad Genetic System (GS) HIV-1/HIV-2 Plus O EIA. HIV-1 Western Blot (Calypte) was used as the confirmatory test between 1999 and 2014. In 2015 through 2018, the screening test was updated to the Bio-Rad GS Combo Ag/Ab EIA, which simultaneously determines the presence of the p24 antigen and HIV-1/HIV-2 antibodies. In 2015–2016 and in 2017–2018, the Bio-Rad Multispot HIV-1/HIV-2 Rapid Test and Geenius HIV-1/HIV-2 Supplemental Assay were used as HIV-1/HIV-2 differentiation supplemental tests, respectively. Following the updated recommendations, supplemental results that were negative, indeterminate or undifferentiated were further tested using the Aptima HIV-1 RNA Qualitative Assay (Hologic, San Diego, CA) to confirm HIV-1 infection8. The change in the diagnostic algorithm allowed the detection of acute HIV infections. In contrast, in previous survey years, HIV Western blot only confirmed established HIV infections.
For lifetime history of HIV testing status, respondents aged 18 and over were asked during the household interview “Except for tests you may have had as part of a blood donation have you ever been tested for the AIDS virus”.
Prevalence of anti-retroviral treatment among HIV-positive participants was also assessed using the NHANES prescription drug file. Survey participants were asked if they had taken a prescription medication in the past 30 days. Those who answered “yes” were asked to show the interviewer the medication containers of all prescription medications. For each drug reported, the interviewer recorded the product’s complete name from the container9. Lexicon Plus®, a proprietary drug database of Cerner Multum, Inc. was used to assist in data collection and data processing10. All reported drug names were converted to standard generic drug names in the data process. Use of ARV medication was defined as using at least one of the prescription ARV medications identified based on the generic drug names. A list of ARV medications can be found in the U.S. Food and Drug Administration website11.
Covariables
Demographic variables collected included: age (categorized as 18–39, 40–49, and 50–59 years), sex, and race and Hispanic origin (based on the respondents’ self-reported information and categorized as non-Hispanic white, non-Hispanic black, or Hispanic. Respondents who did not self-identify among these three groups were classified as “other,” which included all other non-Hispanic persons and persons reporting multiple races. Estimates for the “other” category were not reported separately however, these respondents were included when calculating estimates for the total population. Due to small numbers of HIV-positive participants in several race and Hispanic origin groups, the data were categorized as non-Hispanic black and all non-black persons for many analyses. Other demographic variables included: poverty index ratio (calculated by dividing family income by a poverty threshold specific for family size, using the U.S. Department of Health and Human Services’ poverty guidelines and categorized as either below poverty [less than 1] or at or above poverty [1 or more])12; education (self-categorized as having less than high school education, having completed high school or a General Educational Development high school equivalency diploma, or having more than a high school education); any current health insurance; ability to identify a regular source of health care; receipt of any health care in the past 12 months and marital status (married, widowed or living as married; divorces or separated; and never married).
Sensitive questions involving sexual behavior, drug use, sexually transmitted infections (STIs) were collected in the MEC using the audio computer-assisted self-interviewing (ACASI) and computer-assisted personal interviewing (CAPI) systems. Risk behavior data included lifetime number of sexual partners (0–4, 5–9 or 10 or more partners), age individual initiated sexual activity (< 18 years versus 18 years or older), history of same sex sexual partner (men only), illicit or injection drug use (based on combining the responses to the questions “Have you ever used cocaine, crack cocaine, heroin, or methamphetamine?” and “Have you ever, even once, used a needle to inject a drug not prescribed by a doctor? ” because there were insufficient numbers of injection-drug users), and serologic evidence of Herpes simplex virus type II (HSV-2) among those age 18–49 determined by a type specific immunodot assay13–14.
Statistical Methods
The association between demographic and risk behavior cofactors and either outcome (HIV prevalence and self-reported HIV testing history) was examined using the most recent 10 years of data combined (2009–2018) for those aged 18–59 and estimates were adjusted for age using the direct method to the 2000 projected U.S. population using the age groups mentioned above. Similarly, ARV use was examined using the combined surveys 2009–2018 and estimated for those HIV positive overall, and by sex and by race and Hispanic origin only.
Trends were examined over the 20-year period from 1999–2018, by age group, sex, and race and Hispanic origin using orthogonal linear contrasts. Analyses were conducted for HIV prevalence among those aged 18–49 only, since HIV status was not measured on those aged 50–59 years until 2009. Since the number of HIV positive sample persons in NHANES was small (often less than 5 positive persons per 2 year cycle for some demographic strata) and estimates based on two years of data were highly variable (relative confidence interval widths between 130% and 800%), we decided to combine 2-year cycles and create more stable 4-year estimates for the 5 periods (1999–2002, 2003–2006, 2007–2010, 2011–2014, 2015–2018) when examining trends in HIV prevalence. Significance of trends were also tested using 2-year estimates as recommended in the “NCHS Guidelines for analysis of trends” and were compared to those using 4-year estimates. Results were similar so 4-year trends are presented for consistency. Prevalence was much higher for self-reported HIV testing and 2-year estimates much more stable. Therefore, we utilized all 10 2-year estimates for those age 18–59 for the analysis of trends by demographic subgroups for self-reported HIV testing.
Examination sample weights that account for the differential probabilities of selection, nonresponse, and noncoverage, were incorporated into the estimation process. Standard error estimates were calculated using Taylor series linearization in SUDAAN version 10.0 (RTI International, Research Triangle Park, N.C.), a method that accounts for the complex sample design. Exact binomial ninety-five percent confidence intervals (95% CI) were computed using the Korn and Graubard method16. All estimates met NCHS data presentation standards for proportions unless otherwise noted17. Tests for trends were conducted using polynomial contrast procedure in SUDAAN’s Proc Descript and differences between subgroups were evaluated using Student’s t statistic both at the p<0.05 significance level.
Outcome item non-response
From 2009–2018, 93.0% of examined sampled persons aged 18–59 were tested for HIV. Response to testing varied by cycle and ranged from 91.8% in 2011–2012 through 94.5% in 2013–2014. Response also varied by race and Hispanic origin and was consistently lower for each 2-year cycle for non-Hispanic black (89.2%) compared to non-Hispanic white (94.6%), Hispanic (94.9%) and all non-black (94.1%) persons. There were no consistent differences by other demographic categories.
For the same 10-year period, 86.5% of those examined responded to the question on history of ever having been tested for HIV, ranging from 84.3% in 2011–2012 to 90.2% in 2017–2018. The percent who responded was lower among women (84.3%) as compared to men (88.7%) consistently for the period 2009–2018. There were no consistent differences by other demographic categories.
Results
The age-adjusted HIV prevalence in the U.S. was 0.41% (95% CI 0.27 to 0.61%) among those aged 18–59 years in 2009–2018 (Table 1). In both univariate analyses and multivariable models, HIV prevalence was higher among those age 50–59 (0.65%) compared with the youngest age group (age 18–39 years, 0.20%, p=0.005 from univariate analysis) (aOR 3.5 95% CI 1.8–6.6) . Prevalence was also higher among males (0.70%) compared to females (0.13%), p<0.001) (aOR 5.3 95% CI 3.3–8.3) and non-Hispanic black persons (1.61%) compared to all other race/ethnic groups combined (0.25%, p<0.001) (aOR 5.5 95% CI 3.0–9.8). Other significant differences seen were among those never married (0.98%) verses those married (0.33%, p=0.001) (aOR 2.0 95% CI 1.1–3.7), those who received health care in the past 12 months (0.48%) versus no health care (0.10, p=0.001) (aOR 3.9, 95% CI 1.3–12.1), those who had 10 or more (0.90%) lifetime number of sexual partners compared with 0–4 (0.07%) (p<0.001) (aOR 6.9 95% CI 2.6–17.9), those who had a history of a same sex sexual partners among men (8.84%) versus no history (0.18%) (p<0.001), and those positive to herpes type II (1.22%) compared to those negative (0.17%, p=0.004) (same sex sexual partners and herpes positivity were not included in multivariable model because data was not collected on all sample persons for those variables).
Table 1:
Age specific and age adjusted prevalence of HIV infection and HIV self-reported testing by demographic and behavioral risk factors for NHANES 2009–2018
| Percent HIV Positive | Percent HIV Tested | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cofactor | Sample Size | Percent | Lower 95% CI~ | Upper 95% CI | P-value* | Sample Size | Percent | Lower 95% CI | Upper 95% CI | P-value* | |
| Total | 18480 | 0.41 | 0.27 | 0.61 | 17173 | 44.2 | 42.7 | 45.7 | |||
| Age | |||||||||||
| 18–39 (Ref) | 9925 | 0.20 | 0.11 | 0.31 | 9263 | 43.6 | 41.8 | 45.4 | |||
| 40–49 | 4361 | 0.69 | 0.28 | 1.39 | 0.057 | 3989 | 50.0 | 47.4 | 52.6 | <0.001 | |
| 50–59 | 4194 | 0.65 | 0.38 | 1.02 | 0.005 | 3921 | 37.8 | 35.3 | 40.4 | <0.001 | |
| Sex | |||||||||||
| Men | 8871 | 0.70 | 0.44 | 1.06 | <0.001 | 8458 | 39.6 | 37.6 | 41.7 | <0.001 | |
| Women (Ref) | 9609 | 0.13 | 0.07 | 0.23 | 8715 | 49.0 | 47.3 | 50.7 | |||
| Race and Hispanic Origin1 | |||||||||||
| Non-Hispanic white | 6649 | 0.29 | 0.12 | 0.59 | <0.001 | 6171 | 42.4 | 40.5 | 44.3 | <0.001 | |
| Non-Hispanic black (Ref) | 3907 | 1.61 | 1.18 | 2.14 | 3823 | 64.3 | 61.8 | 66.7 | |||
| Hispanic | 4996 | 0.24 | 0.13 | 0.42 | <0.001 | 4596 | 39.6 | 37.1 | 42.1 | <0.001 | |
| All non-black2 | 14573 | 0.25 | 0.12 | 0.46 | <0.001 | 13350 | 41.4 | 39.9 | 42.9 | <0.001 | |
| Education | |||||||||||
| Less than highh school | 4000 | 0.36 | 0.18 | 0.63 | 0.597 | 3624 | 38.1 | 35.4 | 40.7 | <0.001 | |
| Completed high school/GED | 4256 | 0.38 | 0.19 | 0.68 | 0.737 | 4049 | 39.9 | 37.7 | 42.2 | <0.001 | |
| More than completed HS/GED (Ref) | 10214 | 0.43 | 0.24 | 0.73 | 9492 | 47.3 | 45.6 | 48.9 | |||
| Poverty Index Ratio3 | |||||||||||
| Below poverty | 4186 | 0.73 | 0.47 | 1.07 | 0.035 | 3885 | 46.2 | 43.8 | 48.7 | 0.108 | |
| At or above (Ref) | 12622 | 0.36 | 0.20 | 0.59 | 11801 | 44.1 | 42.4 | 45.7 | |||
| Marital Status | |||||||||||
| Married/ living / widowed (Ref) | 10581 | 0.33 | 0.16 | 0.61 | 9591 | 44.7 | 42.9 | 46.5 | |||
| Divorced/Separated | 2266 | 0.29 | 0.12 | 0.62 | 0.816 | 2107 | 57.0 | 54.5 | 59.5 | <0.001 | |
| Never married | 4317 | 0.98 | 0.71 | 1.32 | 0.001 | 4135 | 48.5 | 45.7 | 51.4 | 0.023 | |
| Health Insurance | |||||||||||
| Any (Ref) | 13445 | 0.42 | 0.25 | 0.64 | 0.774 | 12499 | 45.1 | 43.5 | 46.7 | <0.001 | |
| None | 5004 | 0.37 | 0.16 | 0.72 | 4645 | 41.0 | 38.8 | 43.3 | |||
| Regular place for health care | |||||||||||
| Any (Ref) | 14329 | 0.45 | 0.29 | 0.68 | 0.281 | 13288 | 46.0 | 44.4 | 47.7 | <0.001 | |
| None | 4150 | 0.26 | 0.07 | 0.66 | 3884 | 38.1 | 35.9 | 40.4 | |||
| Health Care in the past 12 months | |||||||||||
| Any (Ref) | 14508 | 0.48 | 0.31 | 0.72 | 0.001 | 13466 | 46.7 | 45.1 | 48.4 | <0.001 | |
| None | 3949 | 0.10 | 0.03 | 0.26 | 3685 | 34.4 | 31.9 | 37.0 | |||
| Lifetime number of sexual partners | |||||||||||
| 0–4 (Ref) | 6993 | 0.07 | 0.02 | 0.17 | 7167 | 29.3 | 27.8 | 30.8 | |||
| 5–9 | 4037 | 0.22 | 0.10 | 0.41 | 0.035 | 4118 | 46.7 | 44.5 | 48.9 | <0.001 | |
| 10 or more | 5270 | 0.90 | 0.54 | 1.41 | 0.001 | 5400 | 60.3 | 58.0 | 62.7 | <0.001 | |
| Age of first intercourse | |||||||||||
| <18 years | 9389 | 0.47 | 0.31 | 0.69 | 0.380 | 9633 | 50.7 | 48.9 | 52.4 | <0.001 | |
| 18 or older (Ref) | 7006 | 0.37 | 0.17 | 0.69 | 7161 | 35.3 | 33.5 | 37.2 | |||
| History of sexual contact with same sex among men | |||||||||||
| Any | 423 | 8.84 | 5.05 | 14.11 | <0.001 | 432 | 69.2 | 62.4 | 75.4 | <0.001 | |
| None (Ref) | 7657 | 0.18 | 0.08 | 0.35 | 7864 | 37.8 | 35.8 | 39.8 | |||
| Ever used injection or illicit drugs | |||||||||||
| Any | 2818 | 0.84 | 0.41 | 1.53 | 0.021 | 2863 | 55.4 | 52.8 | 58.0 | <0.001 | |
| None (Ref) | 13603 | 0.30 | 0.19 | 0.45 | 13957 | 41.7 | 40.2 | 43.3 | |||
| Herpes Simplex virus type 2 infection status4 | |||||||||||
| Positive HSV-2 | 2537 | 1.22 | 0.51 | 2.44 | 0.004 | 2207 | 66.3 | 62.9 | 69.6 | <0.001 | |
| Negative HSV-2 (Ref) | 11728 | 0.17 | 0.05 | 0.41 | 10265 | 41.8 | 39.6 | 43.9 | |||
Ref=Reference Group
Confidence Interval
p-value from linear contrast comparing subgroup to reference group
All non-Hispanic others including multiracial are not reported individually but are included in the estimates for the total population and all non-black persons
Consists of all non-Hispanic white, Hispanic, and non-Hispanic others combined
Below vs at or above the poverty line based on the U.S. Department of Health and Human Services poverty index ratio adjusted for family size.
Measured only on those age 18–49
Comparisons whose p-value in the univariate analyses were near the cut point of p<0.05 and whose 95% CI’s overlapped (those living below poverty versus at or above (p=0.035), 5–9 sex partners versus 0–4 (p=0.035) and history of injection or illicit drug use (p=0.021)) were no longer significant in the multivariable models.
The age-adjusted prevalence of self-reported ever being tested for HIV in the U.S. for the period 2009–2018 was 44.2% (95% CI 42.7–45.7%) (Table 1). Self-reported HIV testing history was lower among those age 50–59 (37.8%) compared to those age 18–39 (43.6%) (aOR 0.55 95% CI 0.47–0.64) and higher among those aged 40–49 (50.0%) (p<0.001 for all comparisons from univariate analyses). The difference between those age 40–49 versus 18–39 was no longer significant (p=0.605) in the multivariate model (aOR 0.97 95% CI 0.86–1.10). Testing was greater among non-Hispanic black (64.3%, p<0.001) as compared to all other race/ethnic groups combined (41.4%, p<0.001) (aOR 2.4 95% CI 2.1–2.7), lower among males (39.6%) compared to females (49.0%), p<0.001) (aOR 0.62 95% CI 0.56–0.68), higher with increasing education, higher among divorced/separated compared to those married, higher among those with any health insurance, a regular place for health care, or who received health care in the past twelve months, and higher among those with 5–9 or 10 or more lifetime sexual partners, history of same sex sexual contact, history of injection or illicit drug use or herpes positivity (see Table 1, p<0.001 for all comparisons except those never married p=0.045). All variables remained significant in multivariate models except where noted (data not shown). ).
HIV infection was greater (0.87%, 95% CI 0.55–1.31%) among those who were ever tested for HIV compared to those never tested (0.12%, 95% CI 0.04–0.26%) (p<0.001). As expected, history of ever being tested for HIV was greater among those HIV-positive (83.9%, 95% CI 70.3–93.0%) compared to those HIV-negative (43.6%, 95% CI 42.2–45.1%) (p<0.001) (data not shown).
Antiretroviral Therapy
Of the 91 HIV-positive participants from all five 2-year cycles combined from 2009 through 2018, 46.1% (95% CI 32.6–60.1%) were on ARV medication. ARV use was greater among men (51.9%, 95% CI 35.6 −68.0%) as compared to women (17.7%, 95% CI 5.1–39.1%) (p<0.001). ARV use also was greater among HIV positive persons who were non-black (57.5%, 95% CI 14.9–92.8%) compared to those who were non-Hispanic black (34.5%, 95% CI 19.7–51.9%) but this difference did not reach statistical significance (p=0.112). When examining change over time (1999–2008 vs 2009–2018) among those age 18–49 by age, gender and race and Hispanic origin we saw an increase in ARV use among those who were non-Hispanic black that approached significance (p=0.077). However, all estimates and results from comparisons by sex as well as non-Hispanic black race should be interpreted cautiously since they are based on small sample sizes, large confidence intervals and did not meet the NCHS data presentation standards for proportions (data not shown).
Trends in HIV prevalence and HIV self-reported testing history
Although prevalence appeared to decrease over time, there was no significant trend over the 20-year period examining five 4-year cycles in HIV prevalence among all US adults aged 18–49 years. Prevalence ranged from 0.43% in 1999–2002 to 0.40% in 2015–2018 (Figure 1 p=0.541, linear trend). However, HIV prevalence decreased significantly among those age 18–39 from 0.37% in 1999–2002 to 0.11% in 2015–2018 (Figure 1) (p=0.025, linear trend), among women from 0.22% in 1999–2002 to 0.06% in 2015–2018 (Figure 2, p=0.026, linear trend) and among non-Hispanic black persons from 2.14% in 1999–2002 to 0.80% in 2015–2018 (Figure 2, p=0.017, linear trend ). There were no statistically significant trends over time in the other age, sex, or race and Hispanic origin subgroups.
Figure 1:
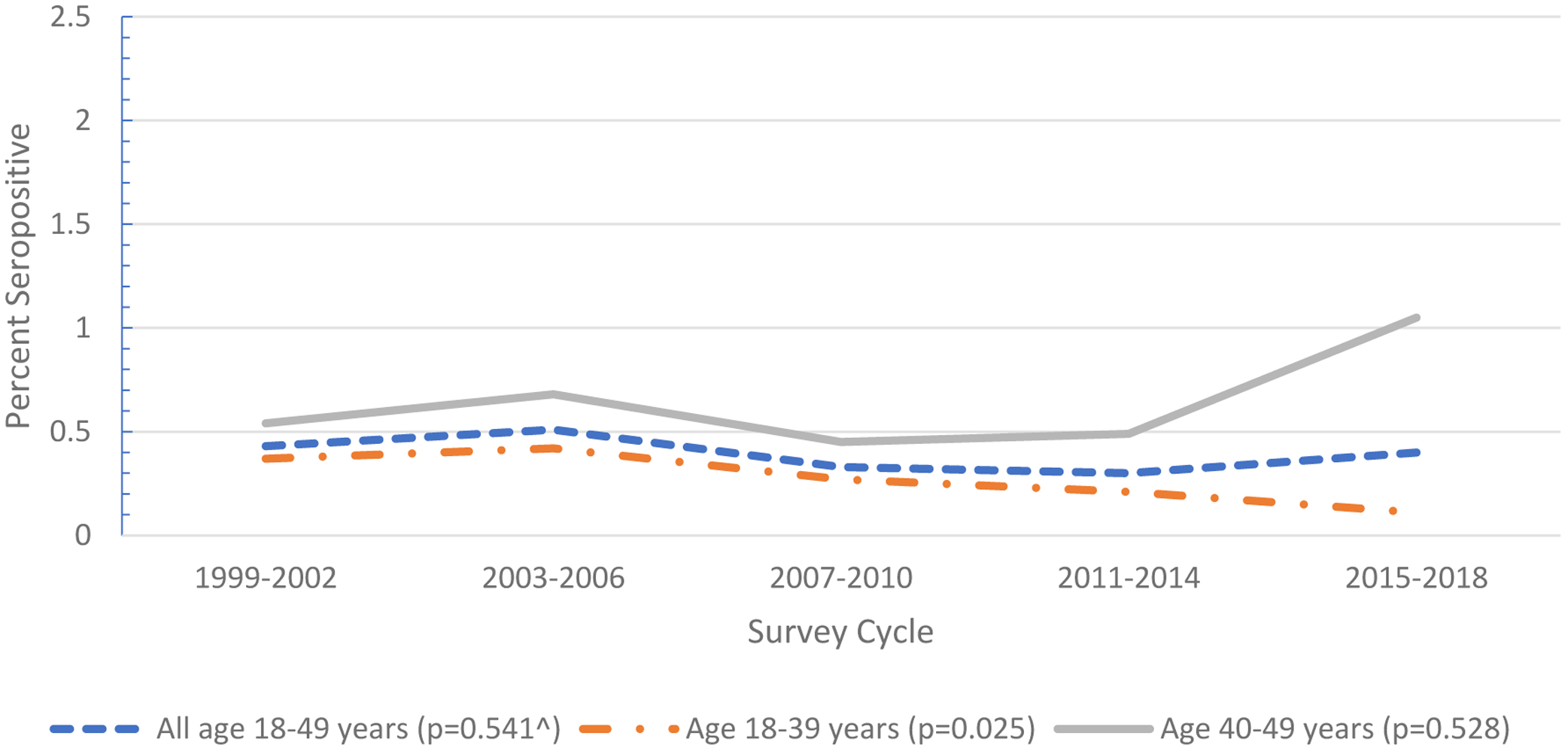
Trends in prevalence of HIV infection for adults aged 18–49 years, all and by age group: NHANES 1999–2018 (p-value for test of linear trend over the 5 four-year cycles from 1999–2018)
Figure 2:
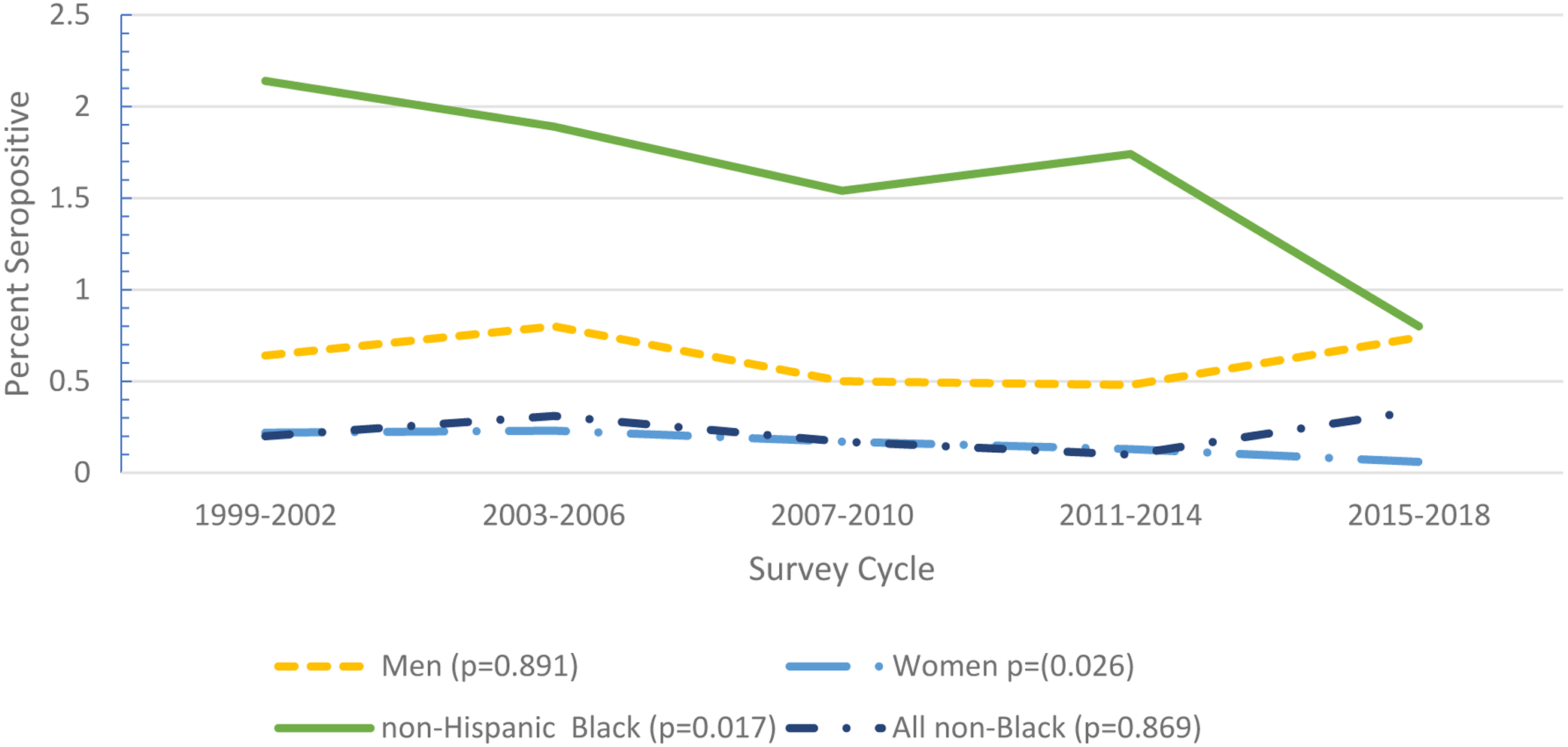
Trends in prevalence of HIV infection for adults aged 18–49 years by gender and race and Hispanic origin: NHANES 1999–2018 (p-value for test of linear trend over the 5 four-year cycles from 1999–2018)
Self-reported history of HIV testing increased from 44.5% in 1999–2000 to 47.9% in 2017–2018 for all adults 18–59 years but this trend was not statistically significant (p=0.102)(Figure 3). However, testing did increase significantly over the 20 year period among those aged 40–49 (41.4% in 1999–2000 to 54.2% in 2017–2018, p<0.001, linear trend) and aged 50–59 (30.0% in 1999–2000 to 44.8% in 2017–2018, p<0.001, linear trend) but decreased among those 18–39 (50.1% in 1999–2000 to 46.8% in 2017–2018, p=0.011, linear trend). HIV testing also increased among non-Hispanic black persons (Figure 4, 53.2% in 1999–2000 to 67.4% in 2017–2018, p<0.001, linear trend) and in women (48.2% to 53.2%, p=0.014, linear trend). There were no significant trends in self-reported HIV status among the other demographic subgroups.
Figure 3:
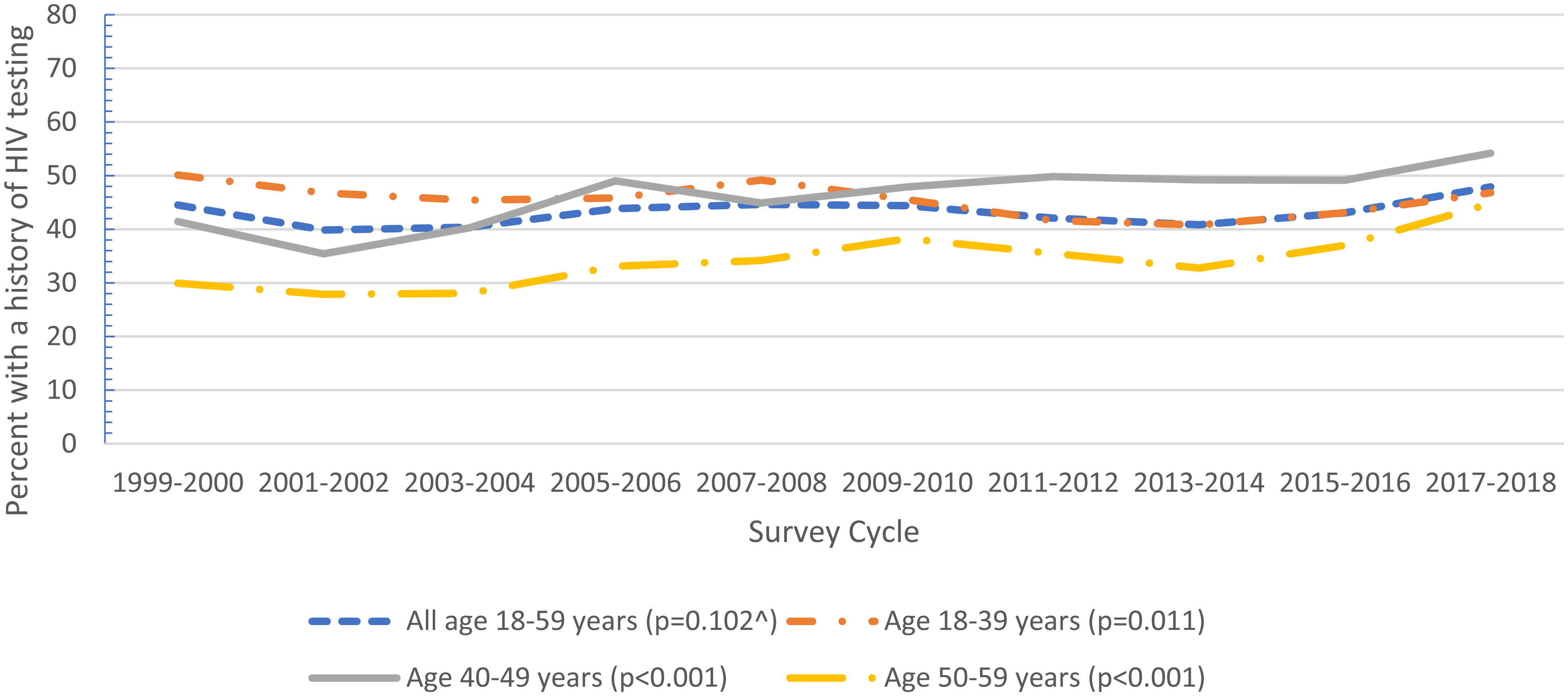
Trends in the percent of adults aged 18–59 with a self-reported history of HIV testing, all and by age group: NHANES 1999–2018 (p-value for test of linear trend over the 10 two-year cycles from 1999–2018)
Figure 4:
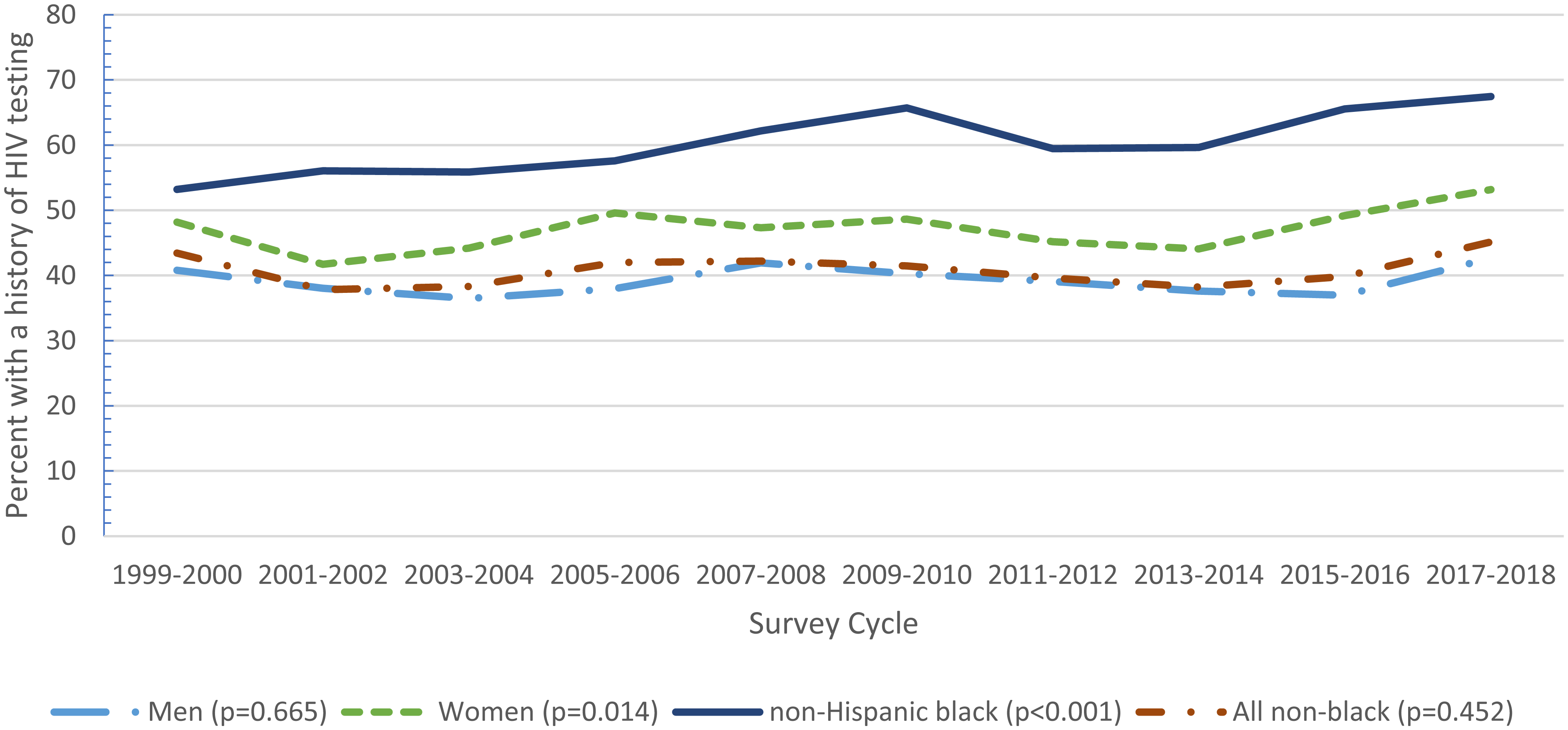
Trends in the percent of adults aged 18–59 with a self-reported history of HIV testing, by gender and race and Hispanic origin: NHANES 1999–2018 (p-value for test of linear trend over the 10 two-year cycles from 1999–2018)
Discussion
HIV prevalence in US adults 18–49 years did not change over the 20-year period studied even after changing the HIV diagnostic algorithm that allows detection of HIV infection earlier than the antibody-based algorithm. There was, though, a significant decline in prevalence in adults aged 18–39 years and a corresponding non-significant increase in prevalence among the oldest age group. This may reflect a decline in incidence among younger people that is supported by declines in the annual rate of HIV diagnoses observed in the most recent HIV surveillance report2. There was also a decline in HIV prevalence among women and non-Hispanic black persons over the 20 years of data examined from 1999–2018 even though this race and Hispanic origin subgroup had a significantly higher HIV prevalence compared to the non-black population.
In 2006, CDC revised recommendations for HIV testing from at-risk populations to all persons aged 13–64 years18. Despite the change in testing recommendations, NHANES data on self-reported HIV testing demonstrated that there was not a consistent overall linear trend in reported HIV testing for 1999–2018, and less than 50% of participants self-reported HIV testing in all cycles except for non-Hispanic black persons in all cycles, adults aged 18–39 in 1999–2000, and both women and adults aged 40–49 in 2017–2018. Trends in self-reported testing increased for non-Hispanic black adults, women and those age 40–49 and 50–59 but contrary to the recommendations, testing decreased among young adults aged 18–39 years. This decrease in HIV testing among those age 18–39 corresponded to a decrease in HIV infection. In contrast, decreases in HIV seroprevalence among women and non-Hispanic black persons corresponded to increases in self-reported testing.
The 2006 recommendations also set a goal of 90% of HIV-infected individuals to be tested for the virus by 2020. NHANES data for 2009–2018 demonstrate that this goal is close to being met with approximately 84% of HIV-positive participants reporting they had been tested for HIV.
Race and Hispanic origin were strongly associated with increased HIV prevalence with non-Hispanic black persons having a significantly higher prevalence compared to all other race and Hispanic origin groups. Poverty, having never married and high-risk sexual behavior cofactors continue to be predictors of increased infection as observed in our previous reports4–5.
NHANES has an extensive medication database so we were able to look at changes in ART use among demographic categories. In a previous report4, we saw that though non-Hispanic blacks had a significantly higher prevalence of HIV infection compared to all other race/ethnic groups, but they also had significantly lower ART medication use. Although our estimates of ART medication use by race and Hispanic origin subgroup are based on small sample sizes and should be interpreted cautiously, an increase in ART use among non-Hispanic blacks from 1999–2008 to 2009–2018 approached significance and differences by non-Hispanic black race in ART use in 2009–2018 were no longer statistically significant showing a possible improvement in racial disparities.
The limitations of NHANES have been previously reported4–5. Item non-response to HIV serologic testing in the survey was higher among non-Hispanic black persons who were more likely to be HIV-positive so we may have underestimated HIV prevalence in the total population. Non-response to self-reported HIV testing was higher among women than men and women were more likely to have been previously tested, so our estimate for having a history of HIV testing may also be underestimated. Small numbers overall in the number of HIV-positive participants in various demographic and high-risk subgroups required the combining of survey cycles to produce stable estimates of prevalence when examining both associations with demographic and risk behavior cofactors and when examining trends over time. Because the NHANES survey sample is drawn from the general household population, it does not capture marginalized populations such as the homeless who may be more at risk for infection with this virus. Despite these limitations, the data from NHANES allows the ability to look at both socio-demographic factors and risk behaviors associated with infection in the U.S. household population and determine trends over time in both HIV prevalence and self-reported testing and these data complement CDC’s case report surveillance1.
Acknowledgments
Funding was provided by CDC/NHANES appropriated federal funds. No other funding was obtained.
References
- 1.Centers for Disease Control and Prevention. HIV Surveillance Report, 2018 (Updated); vol. 31. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published May 2020. Accessed December 4, 2020.
- 2.Chen CI, Clark J, Riddles MK, Mohadjer LK, Fakhouri TH. National Health and Nutrition Examination Survey, 2015−2018: Sample design and estimation procedures. National Center for Health Statistics. Vital Health Stat 2(184). 2020 [PubMed] [Google Scholar]
- 3.McQuillan GM, Kruszon-Moran D, Kottiri BJ, et al. Prevalence of HIV in the US Household Population. The National Health and Nutrition Examination Surveys, 1988–2002. J Acquir Immune Defic Syndr. 2006;41: 651–656. [DOI] [PubMed] [Google Scholar]
- 4.McQuillan GM, Kruszon-Moran D, Granade T, et al. Seroprevalence of HIV in the US household population aged 18–49 years: The National Health and Nutrition Examination Surveys, 1999–2006. J Acquir Immune Defic Syndr. 2010; 54:117–123. [DOI] [PubMed] [Google Scholar]
- 5.Woodring J, Kruszon-Moran D, McQuillan G. HIV Infection in the U.S. household population Aged 18–59: Data from the National Health and Nutrition Examination Survey, 2007–2012. National Health Statistics Reports; no 83. Hyattsville MD: National Center for Health Statistics. 2015. [PubMed] [Google Scholar]
- 6.Zip G, Chiappa M, Porter KS. National Health and Nutrition Examination Survey: plan and operations 1999–2010. National Center for health Statistics. Vital Health Stat 2013:1. https://www.cdc.gov/nchs/data/series/sr_01/sr01_056.pdf. [PubMed] [Google Scholar]
- 7.National Center for Health Statistics. About the National Health and Nutrition Examination Survey. Hyattsville, MD. 2020. Available from: https://www.cdc.gov/nchs/nhanes/about_nhanes.htm. [Google Scholar]
- 8.Centers for Disease Control and Prevention and Association of Public Health Laboratories, Laboratory testing for the diagnosis of HIV infection: updated recommendations. 2014. https://stacks.cdc.gov/view/cdc/23447. Accessed June 12,2020
- 9.National Center for Health Statistics. NHANES 2015–2016 prescription medication file documentation. Available at: https://wwwn.cdc.gov/Nchs/Nhanes/2017-2018/RXQ_RX_J.htm Accessed March 24, 2020.
- 10.National Center for Health Statistics. NHANES 1999–2018 Data Documentation: Prescription Medications - Drug Information Available from: https://wwwn.cdc.gov/Nchs/Nhanes/1999-2000/RXQ_DRUG.htm. Accessed March 24, 2020.
- 11.Food and Drug Administration. HIV treatment for adults. Available at: https://www.fda.gov/drugs/hiv-treatment/hiv-treatment-information-adults. Accessed May 6, 2020.
- 12.U.S. Department of Health and Human Services, US Poverty Guidelines 2017 82[FR]8613, January 31, 2017. [Google Scholar]
- 13.Lee FK, Pereira L, Griffin C, Reid E, Nahmias A. A novel glycoprotein (gG-1) for detection of herpes simplex virus specific antibodies. J Virol Methods. 1986; 14:111–118 [DOI] [PubMed] [Google Scholar]
- 14.Ashley RL, Militoni J, Lee F, Nahmias A, Corey L. Comparison of western blot (immunoblot) and glycoprotein G-specific immunodot enzyme assay for detecting antibodies to herpes simplex virus type 1 and type 2 in human sera. J Clin Microbiol 1988; 26:662–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parker JD, Talih M, Malec DJ, et al. National Center for Health Statistics Data Presentation Standards for Proportions. National Center for Health Statistics. Vital Health Stat 2(175). 2017. https://www.cdc.gov/nchs/data/series/sr_02/sr02_175.pdf, Accessed June 10,2020. [PubMed] [Google Scholar]
- 16.Korn EL Graubard BL. Confidence intervals for proportions with small expected number of positive counts estimated from survey data. Surv Methodol. 1998; 23(2):193–201 [Google Scholar]
- 17.Parker JD, Talih M, Malec DJ, et al. National Center for Health Statistics Data presentation Standards for Proportions. National Center for Health Statistics. Vital Health Stat 2017; 2(175). [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Revised recommendations for HIV testing of adults, adolescents and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14:1–17. [PubMed] [Google Scholar]


