Abstract
During aging, the skin undergoes changes in architecture and composition. Skin aging phenotypes occur due to accumulated changes in the genome/epigenome, cytokine/cell adhesion, cell distribution/extracellular matrix (ECM), etc. Here we review data suggesting that tissue mechanics also plays a role in skin aging. While mouse and human skin share some similarities, their skin architectures differ in some respects. However, we use recent research in haired murine skin because of the available experimental data. Skin suffers from changes in both its appendages and inter-appendage regions. The elderly exhibit wrinkles and loose dermis and are more likely to suffer from wounds and superficial abrasions with poor healing. They also have a reduction in the number of skin appendages. While telogen is prolonged in aging murine skin, hair follicle stem cells can be rejuvenated to enter anagen if transplanted to a young skin environment. We highlight recent single-cell analyses performed on epidermis and aging human skin which identified new basal cell subpopulations that shift in response to wounding. This may be due to alterations of basement membrane stiffness which would change tissue mechanics in aging skin, leading to altered homeostatic dynamics. We propose that the extracellular matrix (ECM) may play a key role as a chemo-mechanical integrator of the multi-layered senescence-associated signaling pathways, dictating the tissue mechanical landscape of niche microenvironments in aging phenotypes. We show examples where failed chemo-mechanical signaling leads to deteriorating homeostasis during skin aging and suggest potential therapeutic strategies to guide future research to delay the aging processes.
Keywords: skin aging, extracellular matrix, macroenvironment, hair regeneration, skin tension, tissue mechanics, tensional homeostasis, microenvironment
Introduction
As skin ages, it undergoes physiological and pathological changes causing a decline in both structure and function (Gilchrest, 1989; Tobin, 2017). These changes affect many aspects of skin biology, including (1) compromised barrier function and mechanical protection, (2) dampened immune responses, (3) impaired thermoregulation, (4) decreased sweat and sebum production, (5) delayed hair cycling (Chueh et al., 2013; Chen et al., 2016), and (6) delayed wound healing (Gosain and DiPietro, 2004). Aging is complex involving both intrinsic and extrinsic factors. Earlier work by Hayflick suggests cells have a fixed cellular lifespan, leading to the identification of roles of telomere in aging (Kameda et al., 2020). Recent epigenetic studies identified unique age-related methylome changes associated with the aging epigenome (Zhang et al., 2020). Environmental stresses such as somatic mutations, free radical damage, senescence-associated secretory phenotype, autophagy, chronic inflammation, etc. can also promote senescence (Di Micco et al., 2020; Tabibzadeh, 2021). These findings have identified new concepts and therapeutic targets fostering the hope that aging can be delayed and perhaps tissues can be rejuvenated by modifying the epigenome (Guarasci et al., 2019) or by activating resident tissue stem cells (Fuchs and Blau, 2020). While these are important aspects of the aging process, in this mini-review, we discuss the role of tissue mechanics in the aging skin. Tensional homeostasis, a process that balances the extracellular forces exerted on cells by extracellular matrix (ECM) or neighboring cells and the reciprocal forces, is essential to maintain cell function and tissue remodeling. While we consider this concept has a role in both human and mouse aging skin, we will focus more on the haired murine skin because of the available reports. During mouse skin aging, the tissue mechanics landscape shifts greatly, as skin homeostasis declines. Based on these reports, we suggest some potential therapeutic strategies at the end.
The Aging Skin
Manifestations of the aging skin include rough skin textures, wrinkles, laxity, atrophy, pigmentary changes, loss of underlying fat, dry and itchy skin, inability to perspire sufficiently, hair graying, hair loss, thinning of nail plates amongst others (Farage et al., 2013). Recent reports show these traits are affected by both intrinsic (chronological) and extrinsic (non-genetic) factors (Parsons, 1996; Gunn et al., 2009; Tobin, 2017).
Human Skin Aging and Related Diseases
Intrinsically aged skin appears dry and pale with fine wrinkles and increased laxity. This results from gradual physiologic changes include reductions of cell number, collagen production, blood flow, lipids, and rete ridges (Montagna et al., 1989; Tobin, 2017). Extrinsic human skin aging entails changes caused by environmental factors, including ultraviolet light (UV). UV damage upregulates matrix metalloproteases (MMP) (Fisher et al., 1996; Quan et al., 2013) and impacts collagen degradation and synthesis (Varani et al., 2006), as well as the production of elastotic materials in the skin. This creates a microenvironment of fragmented collagen and leads to aberrant collagen homeostasis. There is controversy regarding the effect of aging, whether intrinsic or extrinsic, on epidermal thickness (El-Domyati et al., 2002). Some studies have suggested that intrinsic aging tends to cause a slight overall thinning of the viable epidermis (Lavker, 1979; Lavker and Kligman, 1988; Branchet et al., 1990), while others have found that extrinsic aging tends to cause irregular thickening of the epidermis (Gilchrest, 1989). Recently, single-cell RNA analyses revealed a progressive accumulation of photoaging-related changes and increased chronic inflammation in aging human eyelid skin (Zou et al., 2020). Hair follicular stem cells (HFSC) were shown to be nearly normal in human androgenetic alopecia; the problem is the failure of the niche to convert bulge stem cells (SC) into hair germs, hence resulting in prolonged telogen (Garza et al., 2011). These changes also contribute to hair follicle miniaturization and lowered hair density (Matsumura et al., 2016) and the competition of HFSC fates (Liu et al., 2019).
Solar elastosis, characterized by the replacement of normal elastic fibers with a disordered mass of elastotic material near the dermal-epidermal junction, is the hallmark of photodamaged dermis (Yaar and Gilchrest, 2007). Senile purpura, characterized by recurrent formation of ecchymoses on the sun-exposed extensor surfaces of the extremities, is another disease related to reduction of connective tissue in the dermis. Age-related skin thinning and sun-induced damage of the dermal connective tissue results in inadequate support, increased fragility and rupture of the microvasculature (Fenske and Lober, 1986) as well as decreased wound tensile strength (Thomas, 2001); its cosmetic concerns can negatively impact a patient’s quality of life (McKnight et al., 2015).
Structural and Functional Changes in Aging Skin
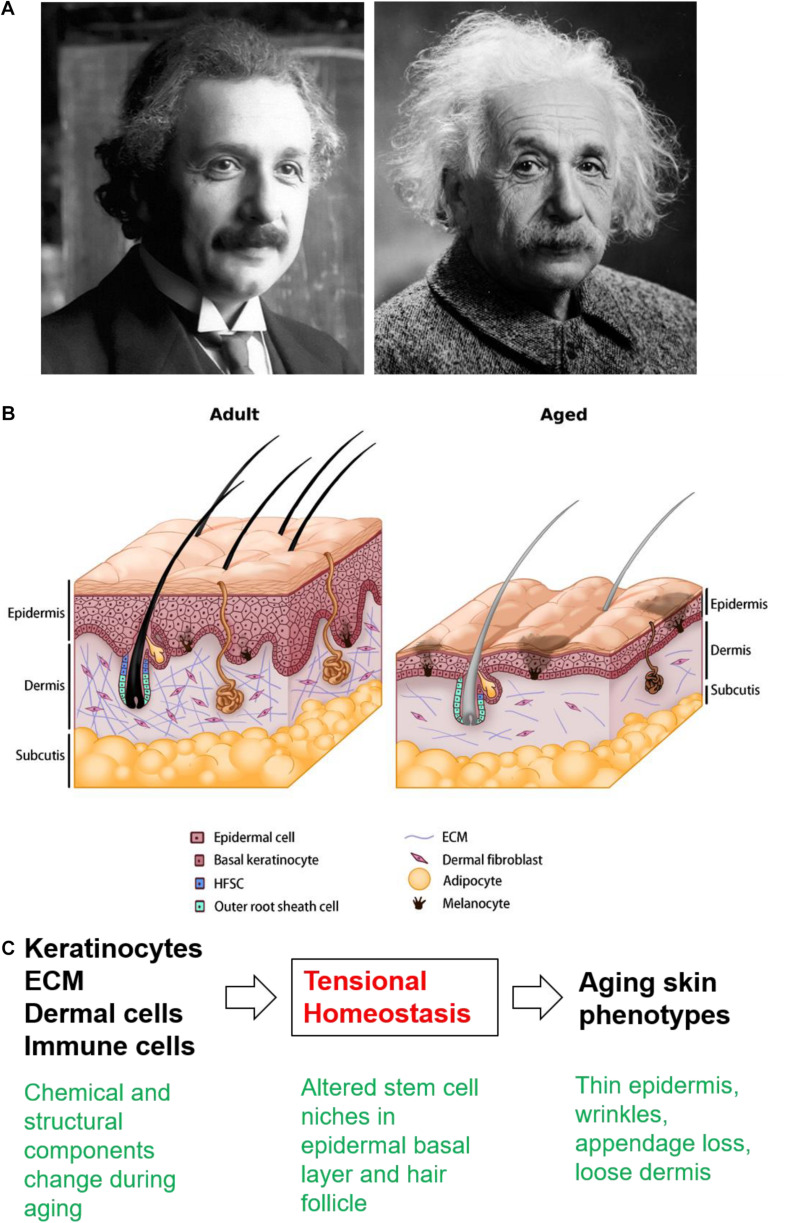
Within the aging mouse skin, the cell number and turnover rate decrease across all cell types (Farage et al., 2013), which impacts epidermal thickness and barrier integrity (Minematsu et al., 2011). Langerhans cells also decrease in number, leading to impaired immune responses (Wulf et al., 2004). Melanocytes lose their enzyme activity, resulting in uneven pigmentation (Nishimura et al., 2005). The flattening of the dermo-epidermal junction alters the epidermal anchoring system (Le Varlet et al., 1998), and hence the skin becomes more vulnerable to dermo-epidermal separation. In the aging dermis, the cellularity, vascularity, innervation, and ECM content also decrease (Makrantonaki and Zouboulis, 2007). The structure of sweat glands becomes distorted and the number of functional sweat glands decreases (Fenske and Lober, 1986). The loss of adipose tissue hinders thermoregulatory function and other signaling roles (Zwick et al., 2018). Interestingly, aging-associated decreases in dermal thickness corresponds with increases in dermal white adipose tissue (dWAT) thickness (Kruglikov et al., 2019b; Zhang et al., 2021). Mature dermal adipocytes de-differentiate and release free fatty acids into the surrounding ECM, which further changes the metabolism and strongly modulates the physiology of adjacent dermal fibroblasts, significantly influencing their collagen expression (Kruglikov and Scherer, 2016). The reduced number and activity of fibroblasts were implicated as the cause of decreased dermal ECM synthesis, leading to deranged ECM support and adequate functions for the skin and skin appendages (Cole et al., 2018). Low fibroblast activity also affects collagen fibril crosslinking (Yang et al., 2008), resulting in a rigid but weakened dermis (Silver et al., 2003). Disorganized ECM also decreases the amount of mechanical loading experienced by the dermal fibroblasts and a possibly diminished ability of the skin to respond to mechanical stimuli, creating a vicious cycle that further deteriorates the homeostasis and physiological functioning of the aged skin (Wu et al., 2011). The structural changes in aging skin and the multilayer control of skin homeostasis (Figures 1A,B), wound healing, and HFSC interaction with the surrounding ECM will be further discussed.
FIGURE 1.
The aging skin. (A) Young and old Albert Einstein used to illustrate the changes in the appearance of aging skin. Source: Pixabay. (B) Schematic drawing showing skin architecture in the adult and aged skin. In aged skin, the overall thickness decreases progressively across all layers, accompanied by wrinkles, pigmentary changes, loss of underlying fat, hair graying, hair loss, and decreased sebaceous gland function. The reduced number and altered activity of fibroblasts have been implicated as the underlying cause of decreased dermal ECM synthesis, leading to deranged ECM support and affects collagen fibril crosslinking. The changes in decreasing cell numbers and altered ECM production and assembly also contribute to hair follicle miniaturization and lowered hair density in aged skin. (C) Cellular/molecular events reviewed in the text present potential new therapeutic targets.
Factors Underlying How Aging Changes the Murine Skin
Adult skin SC are vital for replacing cells in tissues, but their capacity declines with age. SC are regulated by both macroenvironmental signals (Chen and Chuong, 2012; Chen et al., 2016) and their microenvironmental niche (Ge et al., 2020). On the macroenvironment level, the hair cycle in aged mouse skin shows higher and longer expression of HFSC activation inhibitors such as BMPs, DKK1, and SFRPs in the dermis (Chen et al., 2014). On the cellular level, HFSC from aged skin show defects in Nfatc1 (Keyes et al., 2013) and FoxC1 (Lay et al., 2016; Wang et al., 2016). Microenvironmental factors including ECM (Ge et al., 2020), immune, sensory nerves and arrector pili (Shwartz et al., 2020) all take part in regulating HFSC activity. Expression and maintenance of the hemidesmosome component Col17A1 are critical for skin homeostasis and skin epithelial stem cell retention (Matsumura et al., 2016; Liu et al., 2019). Tenascin C (Tnc), an element of the ECM, is shown to promote ECM integrity and is reduced in aged skin (Choi et al., 2020). Thus, both intrinsic and extrinsic factors play a role in the aging of HFSC (Lei and Chuong, 2016).
Tensional Homeostasis: Balanced Tissue Mechanics
Tissue mechanics (Kenedi et al., 1975; Hsu et al., 2018a) can provide a new approach in contemplating stem cell regeneration in the aged skin.
ECM/MMP and Tissue Mechanics in the Skin
The skin cells interact dynamically with the basement membrane (BM), ECM, and the dermis to shape the structure and function of the skin (Fiore et al., 2020). The dermis contains the greatest volume of ECM, which interacts with the dermal cells that generate contractile forces, especially in face of injury (Hsu et al., 2018a; Harn et al., 2019). The amount, content, and organization of ECM being synthesized and remodeled by the MMPs in the dermis is in an intricate balance to maintain the homeostasis of the skin and in aging (Naylor et al., 2011; Tracy et al., 2016). In turn, the ECM provides not only biochemical but also mechanical cues to impact cell behavior (Watt and Fujiwara, 2011). Cells sense mechanical stimuli via mechanosensors (e.g., integrin, hemidesmosomes, adherent junctions, stretch-sensitive ion channels) and translocate these signals into the nucleus for transcriptional response in the mechanotransduction process (Wong et al., 2011). Tensional homeostasis, a concept introduced by Weaver and colleagues to describe the balance between the extracellular forces exerted on the cells by neighboring cells, ECM and reciprocal forces generated by the cells (Paszek et al., 2005), is also essential for maintaining cell function and tissue remodeling in the skin (Harn et al., 2019).
Heterogeneity of the Basal Layer and HF Niche
Recent single-cell analyses identify new sub-populations of basal cells that specifically localize at the top or bottom of rete ridges (Wang et al., 2020), suggesting a mechanical control. Interfollicular epithelial cell differentiation is best described as a single step gradualistic process with a large number of transition cells between the basal and spinous layer (Lin et al., 2020). Their homeostatic states also shift in response to wounding into four different cell states that govern cell proliferation or differentiation (Haensel et al., 2020). We speculate this flexibility of cell states shown during homeostasis is also reflected on cell mechanics; the dynamic changes of cell states also create physical changes to cellular forces that drive cell migration and collective morphological changes.
Rete ridge reductions and tissue mechanical landscape changes in aging skin can either be the cause or consequence of changes in these basal layer sub-populations. Additionally, the basement membrane (BM) adjacent to HFSC serves as an arrector pili muscle (APM) niche (Fujiwara et al., 2011), which together with the sympathetic nerve can form a dual-component niche to modulate HFSC activity (Shwartz et al., 2020). ECM dysregulation that accumulates during skin aging could also affect BM properties chemically and mechanically, which in turn alters APM homeostasis and HFSC regulation.
Tissue Mechanics in Aging Skin: ECM Dysregulation, Wrinkling, and Wound Healing
The changes in ECM synthesis, assembly and dampened cellular response to mechanical stimuli in aged skin lead to low proliferation, discontinued migration, prolonged cell-cycle arrest, and eventually cell death (Sherratt, 2009; Wu et al., 2011). Kruglikov and Scherer reported wrinkling as a mechanical phenomenon where the mismatch of mechanical modules between adjacent epidermal-dermal or dermal-subcutaneous junctions, leads to structural instabilities inside the skin (Kruglikov and Scherer, 2018). We view wrinkles as an excessively stiff apical surface area (stratified epidermis) with a decreased basal dimension and resistance (reduced ECM, dermal cell, adipose tissue) that leads to tissue folding (Varner and Nelson, 2014). In multilayered epithelial tissue, softening, and enhanced remodeling of the BM promote tumor budding, while stiffening of the BM promotes tissue folding (Fiore et al., 2020). In parallel, what factors could contribute to the reduced rete ridges and increased wrinkles in aging skin? We propose 3 possible scenarios: (1) BM stiffness increases in aging skin, (2) loss of Col17A1 causes an increase in the ratio of differentiated cells to basal progenitor cells, and (3) decreases in dermis stiffness and length force the attached apical epidermis to bend and fold upward. The precise mechanical changes of these constituents in aging skin remains to be investigated.
Wound healing in a healthy, aged individual is delayed but not defective (Gerstein et al., 1993). This is due to their dampened cellular activity and asynchronization of pro and anti-inflammatory responses to injury (Ashcroft et al., 2002). The reduced number, activity, and migration of keratinocytes and fibroblasts in aged skin lead to delayed re-epithelialization, wound closure, and tissue reformation (Moulin et al., 2000; Ashcroft et al., 2002). On the other hand, although aged skin shows little capacity to regenerate, it is less prone to form hypertrophic scars and keloids (Hsu et al., 2018b), whose etiology is mechanically sensitive (Harn et al., 2015, 2016). Aging skin is characterized by reduced ECM deposition brought about by (1) low skin tension, (2) dampened cellular responses to mechanical stimuli coupled with (3) low pro-inflammatory signaling, and (4) the reduced capacity of dermal adipocytes to transdifferentiate into myofibroblasts (Varani et al., 2006; Zhang et al., 2019) which could underlie reduced scarring after wounding.
Impacts With Perturbed Tensional Homeostasis
Perturbation to tissue mechanics or disruption of tensional homeostasis impacts physiological functioning of the skin, including hair cycling and wound healing (Hsu et al., 2018a; Harn et al., 2019).
Skin Tension and Scarring vs. Regeneration
Generally, increasing skin tension or stiffness leads to higher cell activity and ECM synthesis. Molecules responsible for mechanotransduction are also important in regulating tensional homeostasis. Epidermal-specific deletion of integrin or focal adhesion kinase (FAK) results in disfigured hair follicles and dysregulated hair cycle propagation (Essayem et al., 2006). Activation of TRPV1, a transient receptor potential cation channel involved in mechano-transduction, inhibits hair shaft lengthening and induces premature catagen (Biro et al., 2006). Tension across the wound has been demonstrated as a key inducer of scarring in hypertrophic scars and keloids (Harn et al., 2019). FAK and integrins could be important mediators of these mechanotransduction processes (Wong et al., 2012), although the reduced capacity of dermal adipocytes to de- and transdifferentiate into myofibroblasts could also be an underlying factor (Zhang et al., 2019). In contrast, the African Spiny mice skin expresses a high collagen III to I ratio producing an exceptionally soft substrate (Seifert et al., 2012). Spiny mice can regenerate their skin and all of their appendages after full-thickness wounding (Jiang et al., 2019).
Cyclic Stretch of the Dorsal Murine Skin Activates HFSC
The impact of skin “loosening” during aging can be deduced from the effects of mechanical force on the homeostasis of HFSC. The amount and duration of skin mechanical stretching result in HFSC proliferation (Chu et al., 2019). This depends on three major components. First, the counterbalance between Wnt and BMP-2; second, M2 subtype macrophage polarization; third, growth factor secretion, especially HGF and IGF-1 (Chu et al., 2019). However, this mechanical activation of hair cells seems compromised in the stiff and less extendable aged mice skin (Lynch et al., 2017; Meador et al., 2020) which has difficulty in eliciting a desirable regeneration response via stretching. How mechanical force, ECM and immune cells contribute to aging skin’s inadequate regenerative activity remains to be explored.
Hair Plucking in the Dorsal Murine Skin Triggers a Regenerative Immune Response
External mechanical forces such as hair plucking can also trigger the immune response-mediated regenerative process. Properly arranged hair plucking can trigger an efficient regenerative response mediated through a two-step immune response cascade, called quorum sensing (Chen et al., 2015). These examples demonstrate the importance of tissue mechanics on maintaining homeostasis of the skin and its response to injury.
Recent Discoveries for Therapeutic Strategies Against Aging Skin
Although currently there is no prominent strategy for developing new drugs against skin aging, there are a few chemical and mechanical approaches that have demonstrated potential.
Chemical-Based Approach: PRP, Follistatin, HES1, ADSC, and dWAT
Platelet-rich plasma (PRP) has been adopted to treat many degenerative disorders including hair loss (Li et al., 2012; Khatu et al., 2014) with reasonable success despite variations in current protocols (Ayatollahi et al., 2017; Picard et al., 2017). In principle, this approach is based on the various growth factors released (Gentile et al., 2017); however, its precise mechanism has not been elucidated. Charles-de-Sa et al. demonstrated that dWAT completely disappears after PRP injection and is replaced by fibrotic tissue, which is very similar to the effect observed after Bleomycin injection (Charles-de-Sa et al., 2018).
Replenishing effective growth factors or activating specific downstream genes such as Wnt-follistatin and follistatin-like 1 protein have been tested as a treatment for alopecia (Zimber et al., 2011; Chen et al., 2014). Pharmacological activation of HES1 alleviated the cellular senescence of aged dermal fibroblasts (Zou et al., 2020). Adipose-derived stem cells (ADSC) have shown effects related to dermal fibroblast activation via secretion of growth factors (Kim et al., 2011). Subcutaneous injection of ADSC significantly increased collagen density, dermal thickness, and fibroblast number in hairless mice (Fukuoka et al., 2017), and also stimulated collagen synthesis of human dermal fibroblasts (Kim et al., 2009).
The adipocytes in the dWAT have high plasticity and undergo reversible dedifferentiation, in which adipocyte-derived preadipocytes trans-differentiate into myoblasts and are involved not only in the physiological hair cycle but also under pathological conditions such as hypertrophic scarring, systemic sclerosis and androgenetic alopecia (Zhang et al., 2019). During proliferation, differentiation and dedifferentiation, various extracellular vesicles are secreted to the nearby HF and in turn stimulate its hair cycle (Kruglikov et al., 2019b). Lastly, Caveolin-1 (Cav-1) is upregulated in aged skin and is associated with altered dermal thickness, dWAT expansion and ECM expression, which sequentially influences the mechanical properties of the skin layers (Kruglikov et al., 2019a,b). This makes Cav-1 a potential candidate for anti-aging treatment especially since Mevastatin has been shown to target Cav-1 as an effective treatment for chronic wound healing (Sawaya et al., 2019).
Mechanical Approach: Stretching and ECM/MMP Perturbation
Although the effectiveness of stretching-induced HF activation is less pronounced in aging mice (Chu et al., 2019), interestingly, subcutaneous injection of cross-linked hyaluronic acid stimulates collagen synthesis and partially restores dermal ECM that are lost in photodamaged skin (Bukhari et al., 2018; Yamada and Prow, 2020). It is speculated that this effect is achieved by mechanical stretching of the dermis and the activation of dermal fibroblasts (Chu et al., 2019). It also was demonstrated that cross-linked HA can significantly influence dWAT and subcutaneous WAT which modifies the dermal-subcutaneous junction (Kruglikov and Wollina, 2015), and directly but differentially affects the mature adipocytes and preadipocytes (Nadra et al., unpublished). Other studies have also focused on securing collagen integrity via suppressing MMP production and activity (Oh et al., 2020a), particularly in alleviating UVA-mediated suppression of collagen expression by stimulating TGF-β/Smad signaling (Oh et al., 2020b).
Summary
We review the physiological changes associated with skin aging (Table 1 and Figure 1C) and highlight the potential role of tensional homeostasis. Utilizing and providing a chemically or mechanically induced young environment might rescue aging phenotypes in the skin. This approach could potentially rescue basal layer homeostasis to control (1) epidermal thickness, (2) wound healing, (3) activation of HFSC, and (4) cell reprogramming during wound-induced hair neogenesis (Bhoopalam et al., 2020). While the haired murine skin provides an experimental model that reveals new molecular understanding summarized here, aging human skin has features that do not exist in the mouse model and await further exploration.
TABLE 1.
Comparison of key differences between young and aged skin.
| Category | Young skin | Aged skin | References |
| Structural features | Moist, smooth skin surface. Rete ridges, and sufficient subcutaneous fat, normal perspire function. Normal hair density and pigmentation. | Decrease thickness, dry, fine wrinkles, pigmentary changes. Reduced rete ridges and underlying fat, inability to perspire sufficiently, hair graying, hair loss, decrease sebaceous gland function, thinning of nail plates. | Farage et al., 2013; Tobin, 2017 |
| Macroenvironment | Regulated hair cycle, homeostasis, normal physiological function, ECM and MMP balance, regulated expression of inhibitory and activating factors. Normal wound healing. | Prolonged telogen, deteriorated homeostasis and physiological function. Higher expression of MMPs. Longer expression of BMPs, DKK1, SFRP, downregulation of follistatin. Delayed wound healing. Somatic mutation, free radical damage, senescence-associated secretory phenotype, autophagy, chronic inflammation. | Chen et al., 2014; Fuchs and Blau, 2020; Kameda et al., 2020 |
| Microenvironment | Normal HFSC and dermal cell number and function. Low DNA damage. Normal Nfatc1, FoxC1 expression. Normal and proper ECM production and crosslinking. COL17A1 maintenance. High Tnc expression. | Reduced HFSC and dermal cell number. Accumulated DNA damage. Defect Nfatc1 and FoxC1 expression. Reduced ECM production and deranged crosslinking. Increased COL17A1 proteolysis. Reduced Tnc expression. Aging epigenome. | Keyes et al., 2013; Lay et al., 2016; Matsumura et al., 2016; Wang et al., 2016; Guarasci et al., 2019; Liu et al., 2019; Choi et al., 2020; Di Micco et al., 2020; Zhang et al., 2020; Tabibzadeh, 2021 |
| Tissue mechanics | Prone to hypertrophic scar and keloid. Activation of TRPV1 induces premature catagen. Cyclic stretch induces anagen re-entry. Hair plucking triggers a regenerative immune response. | Rigid dermis, less resistant to shearing force. Dampened cellular activity to mechanical stimuli. Less prone to scaring. | Chen et al., 2015; Chu et al., 2019; Harn et al., 2019 |
Summary of changes during the aging of haired murine skin, the micro- and macroenvironmental signals contributing to HFSC maintenance.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Written informed consent was not obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
CCC and SPW contributed more to the clinical aspect. HICH, ML, and CMC contributed more to the basic research elements. All authors contributed to the writing, organization, and editing of the manuscript. The manuscript was proofread by Dr. R. B. Widelitz.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Funding. HICH was supported by the Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE), The Excellent Research Center Program by the Ministry of Science and Technology (MOST 107-3017-F-006-002) in Taiwan, and NIGMS, NIH. CCC was funded by Ministry of Science and Technology (109-2314-B-010 -014 -MY3). ML was supported by the National Natural Science Foundation of China (82003384), Fundamental Research Funds for the Central Universities (2020CDJYGSG003), Chongqing Talents Program (CQYC2020058022), and Scientific Research Foundation from Chongqing University (02210011044110). CMC was funded by NIGMS, NIH (5R01GM 125322-02).
References
- Ashcroft G. S., Mills S. J., Ashworth J. J. (2002). Ageing and wound healing. Biogerontology 3 337–345. 10.1023/a:1021399228395 [DOI] [PubMed] [Google Scholar]
- Ayatollahi A., Hosseini H., Gholami J., Mirminachi B., Firooz F., Firooz A. (2017). Platelet rich plasma for treatment of non-scarring hair loss: systematic review of literature. J. Dermatolog. Treat. 28 574–581. 10.1080/09546634.2017.1303571 [DOI] [PubMed] [Google Scholar]
- Bhoopalam M., Garza L. A., Reddy S. K. (2020). Wound induced hair neogenesis – a novel paradigm for studying regeneration and aging. Front. Cell Dev. Biol. 8:582346. 10.3389/fcell.2020.582346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biro T., Bodo E., Telek A., Geczy T., Tychsen B., Kovacs L., et al. (2006). Hair cycle control by vanilloid receptor-1 (TRPV1): evidence from TRPV1 knockout mice. J. Invest. Dermatol. 126 1909–1912. 10.1038/sj.jid.5700321 [DOI] [PubMed] [Google Scholar]
- Branchet M. C., Boisnic S., Frances C., Robert A. M. (1990). Skin thickness changes in normal aging skin. Gerontology 36 28–35. 10.1159/000213172 [DOI] [PubMed] [Google Scholar]
- Bukhari S. N. A., Roswandi N. L., Waqas M., Habib H., Hussain F., Khan S., et al. (2018). Hyaluronic acid, a promising skin rejuvenating biomedicine: a review of recent updates and pre-clinical and clinical investigations on cosmetic and nutricosmetic effects. Int. J. Biol. Macromol. 120(Pt B) 1682–1695. 10.1016/j.ijbiomac.2018.09.188 [DOI] [PubMed] [Google Scholar]
- Charles-de-Sa L., Gontijo-de-Amorim N. F., Takiya C. M., Borojevic R., Benati D., Bernardi P., et al. (2018). Effect of use of platelet-rich plasma (PRP) in skin with intrinsic aging process. Aesthet. Surg. J. 38 321–328. 10.1093/asj/sjx137 [DOI] [PubMed] [Google Scholar]
- Chen C. C., Chuong C. M. (2012). Multi-layered environmental regulation on the homeostasis of stem cells: the saga of hair growth and alopecia. J. Dermatol. Sci. 66 3–11. 10.1016/j.jdermsci.2012.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C. C., Murray P. J., Jiang T. X., Plikus M. V., Chang Y. T., Lee O. K., et al. (2014). Regenerative hair waves in aging mice and extra-follicular modulators follistatin, dkk1, and sfrp4. J. Invest. Dermatol. 134 2086–2096. 10.1038/jid.2014.139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C. C., Plikus M. V., Tang P. C., Widelitz R. B., Chuong C. M. (2016). The modulatable stem cell niche: tissue interactions during hair and feather follicle regeneration. J. Mol. Biol. 428 1423–1440. 10.1016/j.jmb.2015.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C. C., Wang L., Plikus M. V., Jiang T. X., Murray P. J., Ramos R., et al. (2015). Organ-level quorum sensing directs regeneration in hair stem cell populations. Cell 161 277–290. 10.1016/j.cell.2015.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi Y. E., Song M. J., Hara M., Imanaka-Yoshida K., Lee D. H., Chung J. H., et al. (2020). Effects of tenascin C on the integrity of extracellular matrix and skin aging. Int. J. Mol. Sci. 21:8693. 10.3390/ijms21228693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu S. Y., Chou C. H., Huang H. D., Yen M. H., Hong H. C., Chao P. H., et al. (2019). Mechanical stretch induces hair regeneration through the alternative activation of macrophages. Nat. Commun. 10:1524. 10.1038/s41467-019-09402-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chueh S. C., Lin S. J., Chen C. C., Lei M., Wang L. M., Widelitz R., et al. (2013). Therapeutic strategy for hair regeneration: hair cycle activation, niche environment modulation, wound-induced follicle neogenesis, and stem cell engineering. Expert Opin. Biol. Ther. 13 377–391. 10.1517/14712598.2013.739601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole M. A., Quan T., Voorhees J. J., Fisher G. J. (2018). Extracellular matrix regulation of fibroblast function: redefining our perspective on skin aging. J. Cell Commun. Signal. 12 35–43. 10.1007/s12079-018-0459-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Micco R., Krizhanovsky V., Baker D., d’Adda di Fagagna F. (2020). Cellular senescence in ageing: from mechanisms to therapeutic opportunities. Nat. Rev. Mol. Cell Biol. 22 75–95. 10.1038/s41580-020-00314-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Domyati M., Attia S., Saleh F., Brown D., Birk D. E., Gasparro F., et al. (2002). Intrinsic aging vs. photoaging: a comparative histopathological, immunohistochemical, and ultrastructural study of skin. Exp. Dermatol. 11 398–405. 10.1034/j.1600-0625.2002.110502.x [DOI] [PubMed] [Google Scholar]
- Essayem S., Kovacic-Milivojevic B., Baumbusch C., McDonagh S., Dolganov G., Howerton K., et al. (2006). Hair cycle and wound healing in mice with a keratinocyte-restricted deletion of FAK. Oncogene 25 1081–1089. 10.1038/sj.onc.1209130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farage M. A., Miller K. W., Elsner P., Maibach H. I. (2013). Characteristics of the aging skin. Adv. Wound Care (New Rochelle) 2 5–10. 10.1089/wound.2011.0356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenske N. A., Lober C. W. (1986). Structural and functional changes of normal aging skin. J. Am. Acad. Dermatol. 15(4 Pt 1) 571–585. 10.1016/s0190-9622(86)70208-9 [DOI] [PubMed] [Google Scholar]
- Fiore V. F., Krajnc M., Quiroz F. G., Levorse J., Pasolli H. A., Shvartsman S. Y., et al. (2020). Mechanics of a multilayer epithelium instruct tumour architecture and function. Nature 585 433–439. 10.1038/s41586-020-2695-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher G. J., Datta S. C., Talwar H. S., Wang Z. Q., Varani J., Kang S., et al. (1996). Molecular basis of sun-induced premature skin ageing and retinoid antagonism. Nature 379 335–339. 10.1038/379335a0 [DOI] [PubMed] [Google Scholar]
- Fuchs E., Blau H. M. (2020). Tissue stem cells: architects of their niches. Cell Stem Cell 27 532–556. 10.1016/j.stem.2020.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujiwara H., Ferreira M., Donati G., Marciano D. K., Linton J. M., Sato Y., et al. (2011). The basement membrane of hair follicle stem cells is a muscle cell niche. Cell 144 577–589. 10.1016/j.cell.2011.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuoka H., Narita K., Suga H. (2017). Hair regeneration therapy: application of adipose-derived stem cells. Curr. Stem Cell Res. Ther. 12 531–534. 10.2174/1574888X12666170522114307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garza L. A., Yang C. C., Zhao T., Blatt H. B., Lee M., He H., et al. (2011). Bald scalp in men with androgenetic alopecia retains hair follicle stem cells but lacks CD200-rich and CD34-positive hair follicle progenitor cells. J. Clin. Invest. 121 613–622. 10.1172/JCI44478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge Y., Miao Y., Gur-Cohen S., Gomez N., Yang H., Nikolova M., et al. (2020). The aging skin microenvironment dictates stem cell behavior. Proc. Natl. Acad. Sci. U.S.A. 117 5339–5350. 10.1073/pnas.1901720117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentile P., Cole J. P., Cole M. A., Garcovich S., Bielli A., Scioli M. G., et al. (2017). evaluation of not-activated and activated PRP in hair loss treatment: role of growth factor and cytokine concentrations obtained by different collection systems. Int. J. Mol. Sci. 18:408. 10.3390/ijms18020408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerstein A. D., Phillips T. J., Rogers G. S., Gilchrest B. A. (1993). Wound healing and aging. Dermatol. Clin. 11 749–757. [PubMed] [Google Scholar]
- Gilchrest B. A. (1989). Skin aging and photoaging: an overview. J. Am. Acad. Dermatol. 21(3 Pt 2) 610–613. 10.1016/s0190-9622(89)70227-9 [DOI] [PubMed] [Google Scholar]
- Gosain A., DiPietro L. A. (2004). Aging and wound healing. World J. Surg. 28 321–326. 10.1007/s00268-003-7397-6 [DOI] [PubMed] [Google Scholar]
- Guarasci F., D’Aquila P., Montesanto A., Corsonello A., Bellizzi D., Passarino G. (2019). Individual DNA methylation profile is correlated with age and can be targeted to modulate healthy aging and longevity. Curr. Pharm. Des. 25 4139–4149. 10.2174/1381612825666191112095655 [DOI] [PubMed] [Google Scholar]
- Gunn D. A., Rexbye H., Griffiths C. E., Murray P. G., Fereday A., Catt S. D., et al. (2009). Why some women look young for their age. PLoS One 4:e8021. 10.1371/journal.pone.0008021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haensel D., Jin S., Sun P., Cinco R., Dragan M., Nguyen Q., et al. (2020). Defining epidermal basal cell states during skin homeostasis and wound healing using single-cell transcriptomics. Cell Rep. 30 e3932–e3936. 10.1016/j.celrep.2020.02.091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harn H. I., Hsu C. K., Wang Y. K., Huang Y. W., Chiu W. T., Lin H. H., et al. (2016). Spatial distribution of filament elasticity determines the migratory behaviors of a cell. Cell Adh. Migr. 10 368–377. 10.1080/19336918.2016.1156825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harn H. I., Ogawa R., Hsu C. K., Hughes M. W., Tang M. J., Chuong C. M. (2019). The tension biology of wound healing. Exp. Dermatol. 28 464–471. 10.1111/exd.13460 [DOI] [PubMed] [Google Scholar]
- Harn H. I., Wang Y. K., Hsu C. K., Ho Y. T., Huang Y. W., Chiu W. T., et al. (2015). Mechanical coupling of cytoskeletal elasticity and force generation is crucial for understanding the migrating nature of keloid fibroblasts. Exp. Dermatol. 24 579–584. 10.1111/exd.12731 [DOI] [PubMed] [Google Scholar]
- Hsu C. K., Lin H. H., Harn H. I., Hughes M. W., Tang M. J., Yang C. C. (2018a). Mechanical forces in skin disorders. J. Dermatol. Sci. 90 232–240. 10.1016/j.jdermsci.2018.03.004 [DOI] [PubMed] [Google Scholar]
- Hsu C. K., Lin H. H., Harn H. I., Ogawa R., Wang Y. K., Ho Y. T., et al. (2018b). Caveolin-1 controls hyperresponsiveness to mechanical stimuli and fibrogenesis-associated RUNX2 activation in keloid fibroblasts. J. Invest. Dermatol. 138 208–218. 10.1016/j.jid.2017.05.041 [DOI] [PubMed] [Google Scholar]
- Jiang T. X., Harn H. I., Ou K. L., Lei M., Chuong C. M. (2019). Comparative regenerative biology of spiny (Acomys cahirinus) and laboratory (Mus musculus) mouse skin. Exp. Dermatol. 28 442–449. 10.1111/exd.13899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kameda M., Mikawa T., Yokode M., Inagaki N., Kondoh H. (2020). Senescence research from historical theory to future clinical application. Geriatr. Gerontol. Int. 10.1111/ggi.14121 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Kenedi R. M., Gibson T., Evans J. H., Barbenel J. C. (1975). Tissue mechanics. Phys. Med. Biol. 20 699–717. 10.1088/0031-9155/20/5/001 [DOI] [PubMed] [Google Scholar]
- Keyes B. E., Segal J. P., Heller E., Lien W. H., Chang C. Y., Guo X., et al. (2013). Nfatc1 orchestrates aging in hair follicle stem cells. Proc. Natl. Acad. Sci. U.S.A. 110 E4950–E4959. 10.1073/pnas.1320301110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatu S. S., More Y. E., Gokhale N. R., Chavhan D. C., Bendsure N. (2014). Platelet-rich plasma in androgenic alopecia: myth or an effective tool. J. Cutan. Aesthet. Surg. 7 107–110. 10.4103/0974-2077.138352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J. H., Jung M., Kim H. S., Kim Y. M., Choi E. H. (2011). Adipose-derived stem cells as a new therapeutic modality for ageing skin. Exp. Dermatol. 20 383–387. 10.1111/j.1600-0625.2010.01221.x [DOI] [PubMed] [Google Scholar]
- Kim W. S., Park B. S., Park S. H., Kim H. K., Sung J. H. (2009). Antiwrinkle effect of adipose-derived stem cell: activation of dermal fibroblast by secretory factors. J. Dermatol. Sci. 53 96–102. 10.1016/j.jdermsci.2008.08.007 [DOI] [PubMed] [Google Scholar]
- Kruglikov I. L., Scherer P. E. (2016). Dermal adipocytes: from irrelevance to metabolic targets? Trends Endocrinol. Metab. 27 1–10. 10.1016/j.tem.2015.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruglikov I. L., Scherer P. E. (2018). Skin aging as a mechanical phenomenon: the main weak links. Nutr. Healthy Aging 4 291–307. 10.3233/NHA-170037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruglikov I. L., Wollina U. (2015). Soft tissue fillers as non-specific modulators of adipogenesis: change of the paradigm? Exp. Dermatol. 24 912–915. 10.1111/exd.12852 [DOI] [PubMed] [Google Scholar]
- Kruglikov I. L., Zhang Z., Scherer P. E. (2019a). Caveolin-1 in skin aging – from innocent bystander to major contributor. Ageing Res. Rev. 55:100959. 10.1016/j.arr.2019.100959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruglikov I. L., Zhang Z., Scherer P. E. (2019b). The role of immature and mature adipocytes in hair Cycling. Trends Endocrinol. Metab. 30 93–105. 10.1016/j.tem.2018.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavker R. M. (1979). Structural alterations in exposed and unexposed aged skin. J. Invest. Dermatol. 73 59–66. 10.1111/1523-1747.ep12532763 [DOI] [PubMed] [Google Scholar]
- Lavker R. M., Kligman A. M. (1988). Chronic heliodermatitis: a morphologic evaluation of chronic actinic dermal damage with emphasis on the role of mast cells. J. Invest. Dermatol. 90 325–330. 10.1111/1523-1747.ep12456193 [DOI] [PubMed] [Google Scholar]
- Lay K., Kume T., Fuchs E. (2016). FOXC1 maintains the hair follicle stem cell niche and governs stem cell quiescence to preserve long-term tissue-regenerating potential. Proc. Natl. Acad. Sci. U.S.A. 113 E1506–E1515. 10.1073/pnas.1601569113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Varlet B., Chaudagne C., Saunois A., Barre P., Sauvage C., Berthouloux B., et al. (1998). Age-related functional and structural changes in human dermo-epidermal junction components. J. Investig. Dermatol. Symp. Proc. 3 172–179. 10.1038/jidsymp.1998.34 [DOI] [PubMed] [Google Scholar]
- Lei M., Chuong C. M. (2016). Stem cells. aging, alopecia, and stem cells. Science 351 559–560. 10.1126/science.aaf1635 [DOI] [PubMed] [Google Scholar]
- Li Z. J., Choi H. I., Choi D. K., Sohn K. C., Im M., Seo Y. J., et al. (2012). Autologous platelet-rich plasma: a potential therapeutic tool for promoting hair growth. Dermatol. Surg. 38(7 Pt 1) 1040–1046. 10.1111/j.1524-4725.2012.02394.x [DOI] [PubMed] [Google Scholar]
- Lin Z., Jin S., Chen J., Li Z., Lin Z., Tang L., et al. (2020). Murine interfollicular epidermal differentiation is gradualistic with GRHL3 controlling progression from stem to transition cell states. Nat. Commun. 11:5434. 10.1038/s41467-020-19234-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu N., Matsumura H., Kato T., Ichinose S., Takada A., Namiki T., et al. (2019). Stem cell competition orchestrates skin homeostasis and ageing. Nature 568 344–350. 10.1038/s41586-019-1085-7 [DOI] [PubMed] [Google Scholar]
- Lynch B., Bonod-Bidaud C., Ducourthial G., Affagard J. S., Bancelin S., Psilodimitrakopoulos S., et al. (2017). How aging impacts skin biomechanics: a multiscale study in mice. Sci. Rep. 7:13750. 10.1038/s41598-017-13150-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makrantonaki E., Zouboulis C. C. (2007). Molecular mechanisms of skin aging: state of the art. Ann. N. Y. Acad. Sci. 1119 40–50. 10.1196/annals.1404.027 [DOI] [PubMed] [Google Scholar]
- Matsumura H., Mohri Y., Binh N. T., Morinaga H., Fukuda M., Ito M., et al. (2016). Hair follicle aging is driven by transepidermal elimination of stem cells via COL17A1 proteolysis. Science 351:aad4395. 10.1126/science.aad4395 [DOI] [PubMed] [Google Scholar]
- McKnight B., Seidel R., Moy R. (2015). Topical human epidermal growth factor in the treatment of senile purpura and the prevention of dermatoporosis. J. Drugs Dermatol. 14 1147–1150. [PubMed] [Google Scholar]
- Meador W. D., Sugerman G. P., Story H. M., Seifert A. W., Bersi M. R., Tepole A. B., et al. (2020). The regional-dependent biaxial behavior of young and aged mouse skin: a detailed histomechanical characterization, residual strain analysis, and constitutive model. Acta Biomater. 101 403–413. 10.1016/j.actbio.2019.10.020 [DOI] [PubMed] [Google Scholar]
- Minematsu T., Yamamoto Y., Nagase T., Naito A., Takehara K., Iizaka S., et al. (2011). Aging enhances maceration-induced ultrastructural alteration of the epidermis and impairment of skin barrier function. J. Dermatol. Sci. 62 160–168. 10.1016/j.jdermsci.2011.03.005 [DOI] [PubMed] [Google Scholar]
- Montagna W., Kirchner S., Carlisle K. (1989). Histology of sun-damaged human skin. J. Am. Acad. Dermatol. 21(5 Pt 1) 907–918. 10.1016/s0190-9622(89)70276-0 [DOI] [PubMed] [Google Scholar]
- Moulin V., Auger F. A., Garrel D., Germain L. (2000). Role of wound healing myofibroblasts on re-epithelialization of human skin. Burns 26 3–12. 10.1016/s0305-4179(99)00091-1 [DOI] [PubMed] [Google Scholar]
- Naylor E. C., Watson R. E., Sherratt M. J. (2011). Molecular aspects of skin ageing. Maturitas 69 249–256. 10.1016/j.maturitas.2011.04.011 [DOI] [PubMed] [Google Scholar]
- Nishimura E. K., Granter S. R., Fisher D. E. (2005). Mechanisms of hair graying: incomplete melanocyte stem cell maintenance in the niche. Science 307 720–724. 10.1126/science.1099593 [DOI] [PubMed] [Google Scholar]
- Oh J. H., Joo Y. H., Karadeniz F., Ko J., Kong C. S. (2020a). Syringaresinol inhibits UVA-induced MMP-1 expression by suppression of MAPK/AP-1 Signaling in HaCaT keratinocytes and human dermal fibroblasts. Int. J. Mol. Sci. 21:3981. 10.3390/ijms21113981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh J. H., Karadeniz F., Kong C. S., Seo Y. (2020b). Antiphotoaging effect of 3,5-dicaffeoyl-epi-quinic acid against UVA-induced skin damage by protecting human dermal fibroblasts in vitro. Int. J. Mol. Sci. 21:7756. 10.3390/ijms21207756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons P. A. (1996). The limit to human longevity: an approach through a stress theory of ageing. Mech. Ageing Dev. 87 211–218. 10.1016/0047-6374(96)01710-1 [DOI] [PubMed] [Google Scholar]
- Paszek M. J., Zahir N., Johnson K. R., Lakins J. N., Rozenberg G. I., Gefen A., et al. (2005). Tensional homeostasis and the malignant phenotype. Cancer Cell 8 241–254. 10.1016/j.ccr.2005.08.010 [DOI] [PubMed] [Google Scholar]
- Picard F., Hersant B., Niddam J., Meningaud J. P. (2017). Injections of platelet-rich plasma for androgenic alopecia: a systematic review. J. Stomatol. Oral Maxillofac. Surg. 118 291–297. 10.1016/j.jormas.2017.06.011 [DOI] [PubMed] [Google Scholar]
- Quan T., Little E., Quan H., Qin Z., Voorhees J. J., Fisher G. J. (2013). Elevated matrix metalloproteinases and collagen fragmentation in photodamaged human skin: impact of altered extracellular matrix microenvironment on dermal fibroblast function. J. Invest. Dermatol. 133 1362–1366. 10.1038/jid.2012.509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawaya A. P., Jozic I., Stone R. C., Pastar I., Egger A. N., Stojadinovic O., et al. (2019). Mevastatin promotes healing by targeting caveolin-1 to restore EGFR signaling. JCI Insight 4:e129320. 10.1172/jci.insight.129320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seifert A. W., Kiama S. G., Seifert M. G., Goheen J. R., Palmer T. M., Maden M. (2012). Skin shedding and tissue regeneration in African spiny mice (Acomys). Nature 489 561–565. 10.1038/nature11499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherratt M. J. (2009). Tissue elasticity and the ageing elastic fibre. Age (Dordr) 31 305–325. 10.1007/s11357-009-9103-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shwartz Y., Gonzalez-Celeiro M., Chen C. L., Pasolli H. A., Sheu S. H., Fan S. M., et al. (2020). Cell types promoting goosebumps form a niche to regulate hair follicle stem cells. Cell 182 578–593.e19. 10.1016/j.cell.2020.06.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silver F. H., Siperko L. M., Seehra G. P. (2003). Mechanobiology of force transduction in dermal tissue. Skin Res. Technol. 9 3–23. 10.1034/j.1600-0846.2003.00358.x [DOI] [PubMed] [Google Scholar]
- Tabibzadeh S. (2021). Cell-centric hypotheses of aging. Front. Biosci. (Landmark Ed.) 26 1–49. 10.2741/4888 [DOI] [PubMed] [Google Scholar]
- Thomas D. R. (2001). Age-related changes in wound healing. Drugs Aging 18 607–620. 10.2165/00002512-200118080-00005 [DOI] [PubMed] [Google Scholar]
- Tobin D. J. (2017). Introduction to skin aging. J. Tissue Viability 26 37–46. 10.1016/j.jtv.2016.03.002 [DOI] [PubMed] [Google Scholar]
- Tracy L. E., Minasian R. A., Caterson E. J. (2016). Extracellular matrix and dermal fibroblast function in the healing wound. Adv. Wound Care (New Rochelle) 5 119–136. 10.1089/wound.2014.0561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varani J., Dame M. K., Rittie L., Fligiel S. E., Kang S., Fisher G. J., et al. (2006). Decreased collagen production in chronologically aged skin: roles of age-dependent alteration in fibroblast function and defective mechanical stimulation. Am. J. Pathol. 168 1861–1868. 10.2353/ajpath.2006.051302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., Siegenthaler J. A., Dowell R. D., Yi R. (2016). Foxc1 reinforces quiescence in self-renewing hair follicle stem cells. Science 351 613–617. 10.1126/science.aad5440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Drummond M. L., Guerrero-Juarez C. F., Tarapore E., MacLean A. L., Stabell A. R., et al. (2020). Single cell transcriptomics of human epidermis identifies basal stem cell transition states. Nat. Commun. 11:4239. 10.1038/s41467-020-18075-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt F. M., Fujiwara H. (2011). Cell-extracellular matrix interactions in normal and diseased skin. Cold Spring Harb. Perspect. Biol. 3:a005124. 10.1101/cshperspect.a005124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong V. W., Akaishi S., Longaker M. T., Gurtner G. C. (2011). Pushing back: wound mechanotransduction in repair and regeneration. J. Invest. Dermatol. 131 2186–2196. 10.1038/jid.2011.212 [DOI] [PubMed] [Google Scholar]
- Wong V. W., Longaker M. T., Gurtner G. C. (2012). Soft tissue mechanotransduction in wound healing and fibrosis. Semin. Cell Dev. Biol. 23 981–986. 10.1016/j.semcdb.2012.09.010 [DOI] [PubMed] [Google Scholar]
- Wu M., Fannin J., Rice K. M., Wang B., Blough E. R. (2011). Effect of aging on cellular mechanotransduction. Ageing Res. Rev. 10 1–15. 10.1016/j.arr.2009.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wulf H. C., Sandby-Moller J., Kobayasi T., Gniadecki R. (2004). Skin aging and natural photoprotection. Micron 35 185–191. 10.1016/j.micron.2003.11.005 [DOI] [PubMed] [Google Scholar]
- Yaar M., Gilchrest B. A. (2007). Photoageing: mechanism, prevention and therapy. Br. J. Dermatol. 157 874–887. 10.1111/j.1365-2133.2007.08108.x [DOI] [PubMed] [Google Scholar]
- Yamada M., Prow T. W. (2020). Physical drug delivery enhancement for aged skin, UV damaged skin and skin cancer: translation and commercialization. Adv. Drug Deliv. Rev. 153 2–17. 10.1016/j.addr.2020.04.008 [DOI] [PubMed] [Google Scholar]
- Yang L., van der Werf K. O., Fitie C. F., Bennink M. L., Dijkstra P. J., Feijen J. (2008). Mechanical properties of native and cross-linked type I collagen fibrils. Biophys. J. 94 2204–2211. 10.1529/biophysj.107.111013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W., Qu J., Liu G. H., Belmonte J. C. I. (2020). The ageing epigenome and its rejuvenation. Nat. Rev. Mol. Cell Biol. 21 137–150. 10.1038/s41580-019-0204-5 [DOI] [PubMed] [Google Scholar]
- Zhang Z., Kruglikov I., Zhao S., Zi Z., Gliniak C. M., Li N., et al. (2021). Dermal adipocytes contribute to the metabolic regulation of dermal fibroblasts. Exp. Dermatol. 30 102–111. 10.1111/exd.14181 [DOI] [PubMed] [Google Scholar]
- Zhang Z., Shao M., Hepler C., Zi Z., Zhao S., An Y. A., et al. (2019). Dermal adipose tissue has high plasticity and undergoes reversible dedifferentiation in mice. J. Clin. Invest. 129 5327–5342. 10.1172/JCI130239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimber M. P., Ziering C., Zeigler F., Hubka M., Mansbridge J. N., Baumgartner M., et al. (2011). Hair regrowth following a Wnt- and follistatin containing treatment: safety and efficacy in a first-in-man phase 1 clinical trial. J. Drugs Dermatol. 10 1308–1312. [PubMed] [Google Scholar]
- Zou Z., Long X., Zhao Q., Zheng Y., Song M., Ma S., et al. (2020). A single-cell transcriptomic atlas of human skin aging. Dev. Cell 10.1016/j.devcel.2020.11.002 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Zwick R. K., Guerrero-Juarez C. F., Horsley V., Plikus M. V. (2018). Anatomical, physiological, and functional diversity of adipose tissue. Cell Metab. 27 68–83. 10.1016/j.cmet.2017.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.