Abstract
Background
Black populations in the United States are being disproportionately affected by the COVID-19 pandemic, but the increased mortality burden after accounting for health and other demographic characteristics is not well understood. We examined characteristics of individuals who died from COVID-19 in Michigan by race stratified by their age, sex and comorbidity prevalence to illustrate and understand this disparity in mortality risk.
Methods
We evaluate COVID-19 mortality in Michigan by demographic and health characteristics, using individual-level linked death certificate and surveillance data collected by the Michigan Department of Health and Human Services from March 16 to October 26, 2020. We identified differences in demographics and comorbidity prevalence across race among individuals who died from COVID-19 and calculated mortality rates by age, sex, race, and number of comorbidities.
Findings
Among the 6,065 COVID-19 related deaths in Michigan, Black individuals are experiencing 3·6 times the mortality rate of White individuals (p<0.001), with a mortality rate for Black individuals under 65 years without comorbidities that is 12·6 times that of their White counterparts (p<0.001). After accounting for age, race, sex, and number of comorbidities, we find that Black individuals in all strata are at higher risk of COVID-19 mortality than their White counterparts.
Interpretation
Our findings demonstrate that Black populations are disproportionately burdened by COVID-19 mortality, even after accounting for demographic and underlying health characteristics. We highlight how disparities across race, which result from systemic racism, are compounded in crises.
Funding
ASP, AP and APG were funded by NSF Expeditions grant 1918784, NIH grant 1R01AI151176-01, NSF Rapid Response Research for COVID-19 grant RAPID-2027755, and the Notsew Orm Sands Foundation. MCF was supported by NIH grant K01AI141576.
Keywords: Covid-19, Pandemics, Race factors, Racism, Emerging infectious diseases, United States, Michigan
Research In Context.
Evidence before this study
Through searches of peer-reviewed and gray literature, we found that racialized populations worldwide have borne the brunt of the COVID-19 pandemic, and that Black populations across the United States in particular have been disproportionately affected. It has been posited that demography and underlying health status are primary drivers of this disparity in the United States. However, the extent to which race influences COVID-19 mortality, after adjusting for age, sex, and comorbidity burden, is less understood.
Added value of this study
We evaluated racial disparities in COVID-19 mortality for Michigan, using individual-level linked death certificate and surveillance data on all COVID-19 deaths statewide. We found that the mortality rate for the Black population overall was 3·6 times the mortality rate for the White population (p<0.001). Statistically significant racial differences were present across all strata by age, sex, and number of comorbidities. Strikingly, Black individuals under 65 years without comorbidities had 12·6 times the mortality rate of their White counterparts. Overall, the median age of Black decedents was nine years younger than White decedents. In addition, we found a longer time from symptom onset to hospitalization and an earlier peak in incidence among Black populations compared to White, indicating potentially heightened exposure alongside reduced access to care.
Implications of all the available evidence
Our findings indicate that prevalence of comorbidities does not account for the elevated mortality rate observed among Black individuals. Additionally, we demonstrate earlier exposure to COVID-19 and delayed hospitalization in the Black population. In the context of literature on systemic racism as an infectious disease risk factor, we find multiple factors have contributed to racial disparities in COVID-19 mortality.
Alt-text: Unlabelled box
1. Introduction
Throughout history, epidemics have inequitably affected vulnerable populations in our societies, [1,2] and the COVID-19 pandemic is no exception. In particular, Black and Hispanic/Latinx populations are disproportionately experiencing severe COVID-19 morbidity and mortality in the United States (US) [3,4]. According to data from the Centers for Disease Control, 53% and 23% of all COVID-19 deaths in the US are among White and Black individuals, respectively, while these races represent 42.1% and 17.0% of the population [5,6]. In Michigan, the disparities are even starker: while Black Americans represent 14.1% of the total population [7], 35.0% of state-wide COVID-19 deaths as of November 5, 2020 and 23.1% of state-wide deaths as of January 21, 2021 occurred in this group [8]. Underlying this disparate burden are systemic inequities in socioeconomic conditions, health, and access to care by race, which impact infection exposure and survival [9,10].
Such inequalities in health are often perpetuated by systemic racism, which can result in reduced access to healthcare and increased risks for health [11,12]. Systemic racism refers to the embedded power in institutions and other structures led by those with both known and unrecognized biases that are reflected in regulations, policies and practices, perpetuating inequitable access to resources and opportunities [13]. Amongst Black communities, longstanding marginalization has led to higher rates of housing instability, financial insecurity, and essential service inaccessibility compared to White communities [14], [15], [16]. For instance, Black families in Michigan report 2.5 times higher rates of poverty [17] and 43% lower household incomes [18] than White families. With lower socioeconomic status, health related costs can create significant challenges for obtaining medical care, medical insurance, and often delay diagnoses and treatments [19,20]. Flint and Detroit, the residents of which are predominantly Black, are the second and fourth poorest cities in the US, respectively [21]. With the confluence of housing, urbanization and socioeconomic disadvantage, Black communities are uniquely placed to face the brunt of contagious and widespread infections. Socioeconomic disparities can influence community-level COVID-19 transmission, as smaller living space, greater household sizes, and reliance on public transportation each impact the potential risk for COVID-19 infection [22,23]. In addition to disparities in access to healthcare [24], other aspects of structural racism such as environmental injustice and inequities in built environment [11], contribute to higher rates of chronic health conditions in Black populations such as diabetes, [25] obesity, [26] asthma, [27] and cardiovascular disease [28] in comparison to White populations, which affect the severity of disease following infection [29].
This multitude of factors creates a challenge for individuals in general, and especially those with underlying medical conditions, to protect themselves from infection. The “stay at home” public health guidelines implemented during the COVID-19 pandemic are in tension with the need for stable employment, wages, and housing. Pandemic related job losses have been experienced predominantly by those in lower income brackets, [16] those in Black and Hispanic/Latinx communities, [16] and those unable to perform work tasks at home [30]. When a certain segment of the population is fundamentally unable to avoid risk and placed in a position to ignore infection prevention guidelines, disparities in morbidity and mortality inevitably arise.
The extent to which Black individuals are being disproportionately killed by the pandemic is not well-quantified. In this study, we aim to uncover whether disparities by race in COVID-19 mortality can be explained by demographic and underlying health characteristics alone. We analyzed individual-level data on people who died from COVID-19 in Michigan, stratified by demographic characteristics, chronic conditions, and geographical location. Then, we assessed disparities in mortality risk by race within each ZIP Code Tabulation Area between March 16 to October 26, 2020, thereby evaluating the interdependent crises of the COVID-19 epidemic and systemic racism in Michigan. Further, we used statistical analyses to assess disparities across races among individuals dying from COVID-19 in Michigan. We found that Black individuals have 3.6 times the risk of dying from COVID-19 as White individuals in Michigan overall (p<0.001). Among those with no comorbidities under the age of 65, Black individuals have 12.6 times the mortality rate of White individuals (p<0.001).
2. Methods
2.1. Data sources
2.1.1. Linked individual-level COVID-19 surveillance and death certificate data
Yale IRB deemed the study as not Human Subjects research and as such, IRB approval was not required. As the data obtained for research purposes were de-identified, patient consent was also not required. Linked death certificate and COVID-19 surveillance data were obtained from the Michigan Department of Health and Human Services. The Division of Vital Records and Health Statistics provided death certificate data for individuals with an International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) code for COVID-19 (U07.1 or U07.2) as an underlying or related cause of death and the Communicable Diseases Division provided data from the Michigan Disease Surveillance System (MDSS) on COVID-19 deaths occurring between March 16 and October 26, 2020. As per the Data Use Agreement, ASP, AP, IM, and LM were given access to the linked data on November 10, 2020 for analysis. All COVID-19 related deaths occurred in the state of Michigan. Datasets were linked based on string values of first name, last name, and date of birth. Names and dates of birth were formated uniformly and combined into string variables, and then linked using a Generalized edit distance technique which measures dissimilarity between two strings. Generalized edit distance scores of 0 were considered exact matches while scores ≥325 were automatically excluded as non-matches. Linkages with scores ranging from 1 to 324 were subject to individual manual review where commonality of first or last name, suffixes, sensical misspellings, and single differences in date of birth were considered.
Individual level data were collected on age, sex, race, ZIP Code Tabulation Area (ZCTAs) of residence, underlying and related causes of death, other medical conditions of interest, pre-existing conditions, immunosuppressive medications, retirement or unemployment status, and residence or employment at a high risk or congregate living facility. ZCTAs are generalized area representations of the US Postal Service Zip Code service areas. Our dataset exclusively contains those who were diagnosed with and whose death was attributed to COVID-19 in Michigan.
Comorbidities were identified by combining information on underlying causes of death, related causes of death, and other medical conditions of interest from death certificates with information on pre-existing conditions and medications from the Surveillance System case report forms. Comorbidities were categorized as follows: asthma or reactive airway disease, cardiovascular disease, cancer, chronic lung disease, diabetes mellitus, neurologic disease, chronic liver disease, chronic renal disease, other immunosuppressive conditions, and other chronic diseases. Other immunosuppressive conditions included rheumatoid arthritis and bullous pemphigoid, among others, as well as those unspecified but noted as immunosuppressive. Other chronic diseases included anemia, depression, and chronic venous thromboembolism as well as those unspecified (See Supplement). Cardiovascular disease corresponded to ICD-10 codes I00-I78, and includes heart attacks and strokes. Comorbidity of cancer represented any history of cancer.
ZCTA of residence was obtained primarily from death certificate data and from surveillance system case reports in instances of missing ZCTA on the death certificate. Only individuals who resided in Michigan were included in the mapping. Individuals who died from COVID-19 were categorized by their status of being residents or employees of high risk or congregate living facilities, which include: long-term care homes, skilled nursing facilities, assisted living facilities, homeless shelters, federal prisons, Michigan Department of Corrections prisons, county jail, juvenile justice facilities, foster care, and others, including senior, retirement, and group homes.
2.1.2. Population-level demographic data
Data on Michigan population demographics by age group, sex, and race were obtained from the Michigan Department of Health and Human Services [31]. The prevalence of comorbidities in the Michigan population by age group, sex, and race were estimated using a combination of 2017 Michigan Medicare data [32], [33], [34] and National Health Interview Survey data on national comorbidity distribution by age group and sex [35] (Table S3). Given data available to us on morbidity burden in the Michigan population, we assumed that the distribution of age and race and the distribution of sex and race were independent. Populations by ZCTA for all races were obtained from the United States Census Bureau Decennial Census [36].
2.2. Analysis
With a two-sample Z-test, we assessed equality of proportions of decedents that are White and Black with continuity corrections in the matched and unmatched data. Using a Chi-Square test, we determined whether a statistically significant difference (α = 0.05) existed between the proportions of deaths which occurred among Black and White individuals in Michigan, and the proportions of the overall population who are Black and White in Michigan.
We also performed univariate and bivariate analyses on COVID-19 mortality by demographic characteristics and presence of single or multiple comorbidities. Specifically, Chi-square and Kruskal-Wallis tests were used to identify differences in the following variables by race: age, sex, number of comorbidities, presence of specific COVID-19 related comorbidities and comorbidity combinations, employment status, and high-risk or congregate living facility exposure as resident or staff. Age was analyzed as both a continuous variable, categorical variable (<40, 40–64, 65–79, ≥80 years), and as a binary variable (<65, ≥65 years). In addition, COVID-19 mortality rates and mortality rate ratios were calculated for the overall sample, as well as by race, age, sex, and number of comorbidities both separately and in combination. Chi-square tests were performed to identify differences in these mortality rates by race.
We combined the individual-level data on COVID-19 deaths with ZCTA level data on total population and population by race to evaluate geographic heterogeneity in mortality. For each ZCTA, we calculated the COVID-19 mortality rate overall and by race, as well as the mortality rate ratio of Black to White deaths. A one-tailed Wilcoxon signed-rank test was used to compare whether the mortality rates among Black individuals were greater than those of White individuals across ZCTAs throughout Michigan.
We conducted descriptive analyses of the dates of COVID-19 symptom onset, hospitalization, and death due to COVID-19, stratified by race, to characterize epidemic progression. We also fit distributions to the time from symptom onset to hospitalization by race. All data were analyzed using Python 3.7.4 and R-3.5.1.
2.3. Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
3. Results
3.1. Demographics of COVID-19 decedents
Between March 16 and October 26, 2020, a total of 6065 COVID-19 related deaths were recorded in the linked surveillance and death certificate databases across Michigan, of which 96.3% (5838) occurred among Black or White individuals (Fig S1). Of the total decedents, the races and ethnicities were as follows: 3497 (57.7%) White, 2341 (38.6%) Black, 18 (0.3%) Native American, 28 (0.5%) South Asian, 25 (0.4%) Southeast Asian, 11 (0.2%) East Asian, 30 (0.5%) other Asian ethnicity, and 115 (1.9%) were decedents of other races or did not have a race reported. A total of 159 (2.6%) decedents were Hispanic/Latinx, 5798 (95.6%) were non-Hispanic/Latinx, and 108 (1.8%) had missing data for this variable. Among White decedents, 1.4% were Hispanic/Latinx in contrast to 0.4% of Black decedents. We focused our analyses on individuals who were White and Black, given the small proportions of individuals of other races and ethnicities. Among the 865 unmatched records, 469 (54.2%) were White decedents and 349 (40.3%) were Black decedents. Proportions of White and Black decedents were not significantly different between matched and unmatched records (White: p = 0.061, Black: p = 0.342).
Black individuals represent 15.7% of the combined Black and White population of Michigan [31] yet accounted for 40.1% of the COVID-19 deaths during our study period. The proportion of deaths reported among Black individuals in Michigan is significantly higher than the proportion of deaths we would expect based on population representation alone (p<0.001).
Black individuals who died from COVID-19 were significantly younger (median [IQR]: 72 [63, 81], p<0.001) than White individuals (81 [72, 89]) and reported lower rates of being to be retired or unemployed (12.9%, p<0.001) than White decedents (22.2%) (Table 1). Among all COVID-19 deaths, 44.0% were either residents or employees of high-risk or congregate living facilities, such as long-term care and senior homes, homeless shelters, and prisons. Black decedents (29.7%) had lower rates of living or working in high-risk or congregate living facilities than White individuals (54.8%, p<0.001). Among all decedents who worked or resided in these facilities, 90.6% were aged 65 and older (Table S1).
Table 1.
Demographic characteristics of individuals who died from COVID-19 in Michigan overall and by race. Data are median [IQR], n (%), or n/N (%), and p-values were calculated by Chi-Square tests or Kruskal-Wallis tests as appropriate. The study population overall includes deaths among individuals of all races, of which Black and White individuals make up 96.3%.
| Race |
Overall* (n = 6065) | |||
|---|---|---|---|---|
| Black n = 2341 (38.6%) | White n = 3497 (57.7%) | p-value | ||
| Sex | 0.006 | |||
| Male | 1274 (54.4) | 1773 (50.7) | 3186 (52.5) | |
| Female | 1067 (45.6) | 1724 (49.3) | 2879 (47.5) | |
| Age, years (median [IQR]) | 72 [63, 81] | 81 [72, 89] | <0.001 | 77 [68, 86] |
| <40 | 44 (1.9) | 26 (0.7) | <0.001 | 74 (1.2) |
| 40–65 | 602 (25.7) | 399 (11.4) | 1053 (17.4) | |
| 65–80 | 1011 (43.2) | 1170 (33.5) | 2283 (37.6) | |
| ≥80 | 684 (29.2) | 1902 (54.4) | 2655 (43.8) | |
|
Congregate Living Facility Resident or Employee** |
695 (29.7) | 1915 (54.8) | <0.001 | 2666 (44.0) |
| Retired or Unemployed | 302 (12.9) | 776 (22.2) | <0.001 | 1128 (18.6) |
| Number of Comorbidities | <0.001 | |||
| None | 675 (28.8) | 566 (16.2) | 1293 (21.3) | |
| One | 428 (18.3) | 636 (18.2) | 1116 (18.4) | |
| Two or more | 1238 (52.9) | 2295 (65.6) | 3656 (60.3) | |
| Comorbidities | ||||
| Asthma or Reactive Airway Disease | 149 (6.4) | 170 (4.9) | 0.016 | 341 (5.6) |
| Cardiovascular Disease | 1235 (52.8) | 2293 (65.6) | <0.001 | 3647 (60.1) |
| Cancer | 191 (8.2) | 425 (12.2) | <0.001 | 639 (10.5) |
| Chronic Lung Disease | 369 (15.8) | 826 (23.6) | <0.001 | 1226 (20.2) |
| Diabetes Mellitus | 744 (31.8) | 978 (28.0) | 0.002 | 1819 (30.0) |
| Neurologic Disease | 460 (19.6) | 1242 (35.5) | <0.001 | 1741 (28.7) |
| Chronic Liver Disease | 64 (2.7) | 76 (2.2) | 0.199 | 149 (2.5) |
| Chronic Renal Disease | 498 (21.3) | 637 (18.2) | 0.004 | 1181 (19.5) |
| Other Immunosuppressive Conditions | 134 (5.7) | 204 (5.8) | 0.906 | 348 (5.7) |
| Other Chronic Diseases | 215 (9.2) | 505 (14.4) | <0.001 | 741 (12.2) |
| Relevant Comorbidity Combinations*** | ||||
| Diabetes Mellitus, Cardiovascular, and Chronic Renal Disease |
214 (9.1) | 244 (7.0) | 0.003 | 488 (8.0) |
| Diabetes Mellitus and Cardiovascular Disease | 576 (24.6) | 828 (23.7) | 0.435 | 1480 (24.4) |
| Cardiovascular and Chronic Lung Diseases | 281 (12.0) | 660 (18.9) | <0.001 | 964 (15.9) |
| Cardiovascular and Neurologic Disease | 353 (15.1) | 935 (26.7) | <0.001 | 1312 (21.6) |
* Races and ethnicities of decedents presented in the column labeled Overall (n = 6065) are White (57.7%), Black (38.6%), Native American (0.3%), South Asian (0.5%), Southeast Asian (0.4%), East Asian (0.2%), other Asian ethnicity (0.5%), and other not specified races and individuals for whom race was not reported (1.9%).
** The number of individuals living in congregate living facilities by age group, sex, and race is presented in Table S1.
*** Comorbidity combinations included here represent those typical among patients with the following medical and behavioural conditions in order: uncontrolled diabetes, obesity, long-term smoker, and dementia. These conditions have been found to be associated with COVID-19 mortality [46].
The most common comorbidity dyads among all COVID-19 deaths were diabetes and cardiovascular disease (24.4%), and cardiovascular and neurologic disease (21.6%). Black decedents had significantly higher rates of reporting asthma (p = 0.016), diabetes (p = 0.002), and chronic renal disease (p = 0.004) than White individuals who died from COVID-19, but significantly lower rates of cardiovascular disease (p<0.001), cancer (p<0.001), chronic lung disease (p<0.001), and neurologic disease (p<0.001). Additionally, Black decedents had higher rates of to have the combination of diabetes mellitus, cardiovascular disease, and chronic renal disease (p = 0.003) than White decedents, and lower rates of the combinations of cardiovascular and chronic lung disease (p<0.001) and cardiovascular and neurologic disease (p<0.001).
3.2. Mortality rates
Between March 16 to October 26, 2020, we calculated that the COVID-19 mortality rate in Michigan was 5.4 per 10,000 population [31]. Stratifying by race, the mortality rate was 3.6 times higher for Black populations (15.6 per 10,000 population) than White populations (4.3 per 10,000 population, p<0.001). Stratifying by age, the mortality rate for Black individuals under 40 years of age (0.50 per 10,000 population) is 7.4 times that for White individuals in the same age group (0.07 per 10,000 population, p<0.001). Among those aged 40 to 69 years, the mortality rate for Black individuals (18.4 per 10,000) was 8.5 times that of White individuals (2.2 per 10,000, p<0.001). Mortality risk for both races increased with age, where Black individuals aged 70 years and older had a mortality rate of 121.1 per 10,000 population and White individuals had a mortality rate of 27.7 per 10,000 population (p<0.001).
While the mortality rate in the White population did not vary significantly by sex (4.5 per 10,000 population for males and 4.2 per 10,000 for females, p = 0.167), Black males have a significantly greater (31.2%) mortality rate than their female counterparts (p<0.001). Comparing males and females under the age of 40, the Black male mortality rate (0.77 per 10,000 population) is 10.8 times that of White males (0.07 per 10,000 population, p<0.001), and the Black female mortality rate (0.23 per 10,000 population) was 3.56 times that of White females in the same age group (0.06 per 10,000 population, p<0.001).
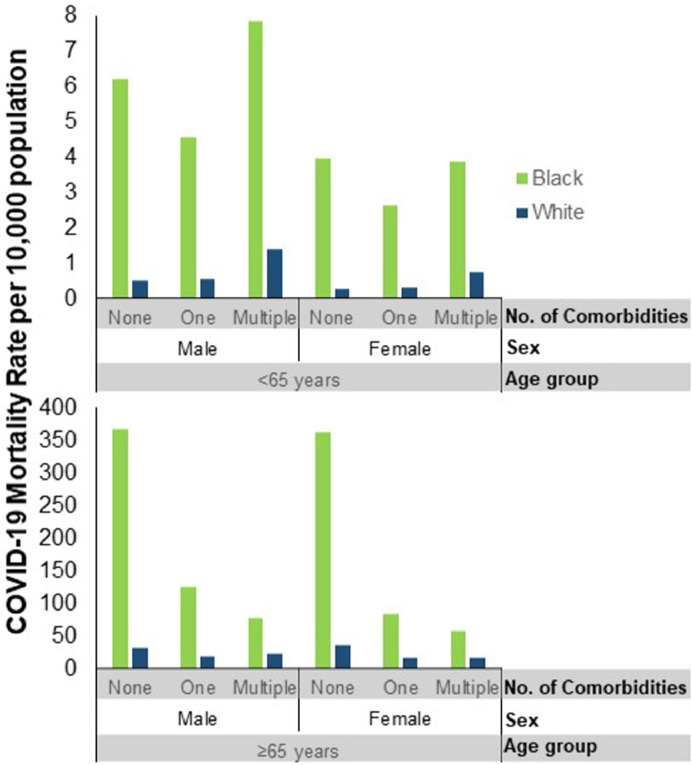
When stratified by age, sex, and number of comorbidities, the mortality rate for the Black population was significantly higher than that for the White population for every pair-wise comparison (p<0.001). Among those with no comorbidities under the age of 65, Black individuals have 12.6 times the mortality rate of White individuals (p<0.001). Black males under the age of 65 years with no comorbidities had a COVID-19 mortality rate of 6.2 per 10,000 population, while White males with no comorbidities in the same age group experienced a lower mortality rate of 0.53 per 10,000 (p<0.001, Fig 1). Among males aged 65 and older with no comorbidities, the COVID-19 mortality rate was 367.5 per 10,000 for Black decedents and 31.6 per 10,000 for White decedents (p<0.001). Black females without comorbidities aged 65 and older had mortality rates of 363.1 per 10,000 in contrast to white females in the same stratum who experienced mortality rates of 35.9 per 10,000 (p<0.001). The relative difference in mortality rate is also stark when comparing Black and White individuals with comorbidities. Black males aged 65 and older with multiple comorbidities had a mortality rate that was 3.5 times that of White males with multiple comorbidities (p<0.001).
Fig 1.
COVID-19 mortality per 10,000 population in Michigan by age, sex, number of comorbidities, and race. The population was first stratified by individuals under 65 years (top) and 65 years and older (bottom) then by sex (male, female), number of comorbidities (none, one, multiple), and race (Black and White). These mortality rates are based on 6065 COVID-19 deaths that occurred in the state of Michigan between March 16 and October 26, 2020. Differences between the mortality rate of Black and White populations are statistically significant for every comparison (p<0.001). Absolute numbers of deaths in each stratum are presented in Table S2.
3.3. Geographical distribution
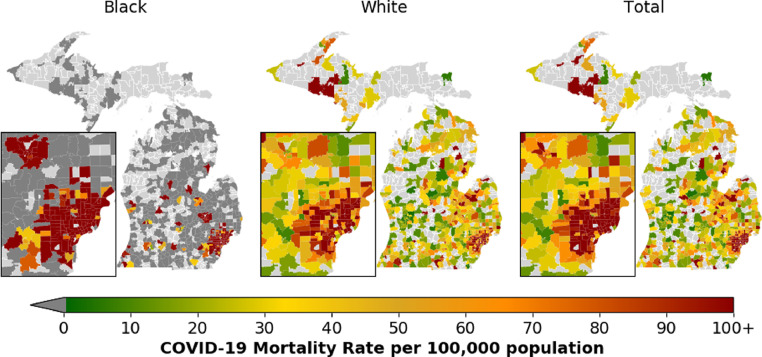
Across the 198 ZCTAs in which at least one Black and at least one White individual died from COVID-19, the median mortality rate for Black populations was 167.9 per 100,000 [IQR: 89.4–251.8] compared to the median mortality rate of 64.0 per 100,000 population [IQR: 34.5–97.0] among white populations (Fig 2). Among all 569 ZCTAs in which a COVID-19 related death took place, 253 ZCTAs reported ≥5 deaths.
Fig 2.
COVID-19 Mortality rates per 100,000 population among Black and White Michigan residents and Michigan residents overall by ZIP Code Tabulation Area (ZCTA). Mortality rate per 100,000 population ranges from 0 (green) to 100+ (red). The highest mortality rate per 100,000 population is 5263. Dark gray regions indicate ZCTAs where no COVID-19 deaths for a particular race occurred and light gray regions indicate ZCTAs where no COVID-19 related deaths took place. These mortality rates are based on 6027 COVID-19 deaths among Michigan residents spread across the state between March 16 and October 26, 2020, of whom 5809 individuals are either White or Black. Total includes individuals of all races. The inset map represents the Detroit Metropolitan Area and Flint. See Supplement for the number of COVID-19 related deaths by ZCTA (Fig S1) and the population of Black individuals by ZCTA (Fig S2).
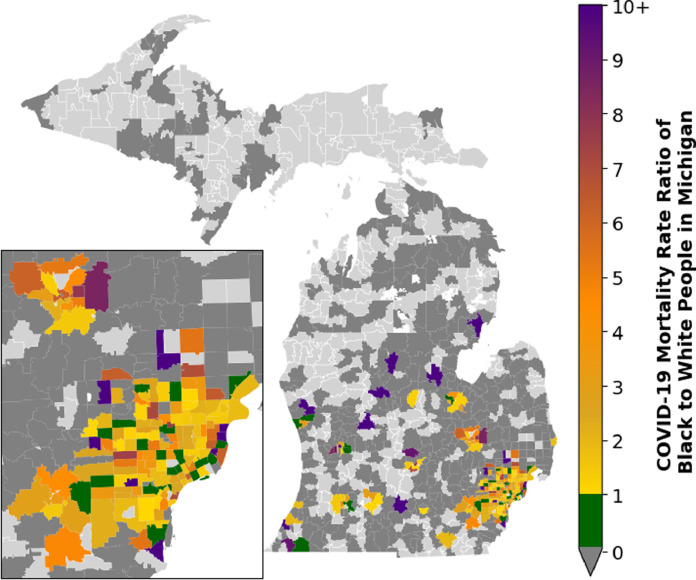
We found that mortality rates were higher among Black individuals in 84.8% of these 198 ZCTAs (Fig 2, Fig 3). For those ZCTAs in which individuals of both races died, mortality rates were significantly higher among Black individuals, as determined by Wilcoxon signed-rank test (p<0.001). In these ZCTAs, Black individuals had a median of 2.3 times [IQR:1.3–4.8] greater odds of dying from COVID-19 than White individuals (Fig 3). Detroit (524,634) and Flint (51,686) have the largest Black populations in Michigan and were both devastated by COVID-19 mortality (Fig S2) [5].
Fig. 3.
Mortality rate ratio for Black to White populations at the ZIP Code Tabulation Area (ZCTA) level of residence in Michigan. There were 30 ZCTAs where deaths among Black individuals occurred yet the White COVID-19 mortality rate exceeded the Black mortality rate (green). The Black COVID-19 mortality rate exceeds White mortality rate in 178 ZCTAs (yellow to purple). Dark gray regions indicate ZCTAs where COVID-19 deaths occurred only among one race, Black or White. Light gray regions indicate ZCTAs where no COVID-19 related deaths took place. The inset map represents the Detroit Metropolitan Area and Flint. These mortality rates are based on 5809 COVID-19 deaths among Black and White Michigan residents spread across the state between March 16 and October 26, 2020.
3.4. Date of symptom onset, hospitalization, and death
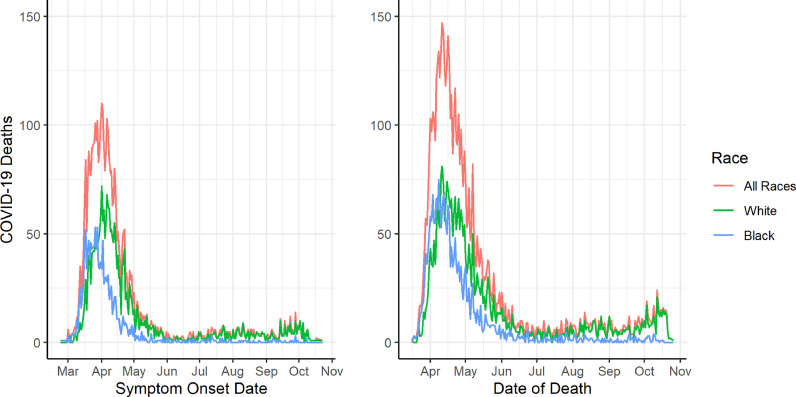
The transmission intensity driven by exposure risk within a population is reflected by the timing of the peaks in symptom onset and mortality. Date of symptom onset was recorded for 4110 of the individuals in our study (67.8%), with missing data on 1955 individuals (32.2%). Among White and Black individuals, 28.2% and 39.1% of individuals are missing symptom onset date data, respectively. Among all COVID-19 decedents in Michigan, dates of symptom onset and death were earlier for Black populations in comparison to White populations (Fig 4), indicating a steeper escalation in risk for Black individuals. The peak in symptom onset for Black individuals in Michigan was 6 days earlier (March 26, 2020) than White individuals (April 1, 2020). Duration of hospitalization was 2 days longer for Black individuals (median of 10 days vs. 8 days) compared to White (p<0.001). The median onset date and median date of death were 13 days earlier for Black individuals who died than White, and peak daily deaths occurred 3 days earlier for Black individuals than White (April 8, 2020 vs April 11, 2020).
Fig. 4.
Date of symptom onset and date of death over time among individuals who died from COVID-19 in Michigan by race. Date of symptom onset (n = 4110) and death (n = 6065) are displayed from February 23 to October 23, 2020 and March 16 to October 26, 2020, respectively. Date of symptom onset was missing for 1955 individuals.
Prompt medical attention is an important component of recovery. The time between symptom onset and hospitalization was a median of 1 day longer for Black decedents compared to White (4 days vs 3 days). Upon fitting negative binomial distributions to the time from symptom onset to hospitalization, we observed a median of 2 days (mean: 4.51 days) for White individuals and a median of 3 days (mean: 5.05 days) for Black individuals (Fig S3).
4. Discussion
Our highly granular analyses demonstrate that at the individual, ZCTA and state levels, racial disparities in the burden and impact of COVID-19 are salient and reflective of pervasive inequities. By accounting for pre-existing comorbidities, we show that these underlying health conditions alone do not explain the racial disparities in COVID-19 mortality. In fact, when adjusting for age and health status, the gap becomes even more striking. Overall, Black populations in Michigan have 3.6 times the mortality rate of White populations. When subset to individuals under 65 years old and without comorbidities, Black individuals have 12.6 times the mortality rate of White individuals. As we consider the substantial disparities highlighted by the COVID-19 pandemic in Michigan, we can see similar patterns elsewhere in the US and around the world [37]. In the United Kingdom (UK), a study on over 17 million adults documented increased COVID-19-related mortality risk among those of Black and South Asian race compared to White people (Hazard ratio 1.48, 1.30–1.69 and 1.44, 1.32–1.58, respectively), even after adjusting for relevant risk factors [38]. Our findings are consistent with race-based COVID-19 mortality risk results from other studies in the UK and the US [10,[39], [40], [41]].
The racial disparity in mortality rate is most pronounced at younger ages. The significantly younger median age of Black deaths (72 vs. 81 years) results in even more years of life lost in this community than the differential mortality rate alone would suggest. Among deceased individuals, peak incidence occurred six days earlier among Black individuals. Although this data is a subset of all exposures and there is incomplete data on symptom onset date, our finding suggests that Black individuals may experience heightened exposure to COVID-19.
We found that White decedents overall and particularly those of older age were more likely to have been living in high-risk congregate living facilities than Black decedents. This may indicate that White decedents were exposed primarily due to their living circumstances in long-term care and assisted living facilities. As Black descendents were younger overall, this population's exposure may be attributed to the vulnerabilities of individuals unable to participate in stay-at-home orders during the pandemic. For instance, the flexibility to work from home is often linked to higher income and to industries in which Black individuals are underrepresented. While 47 to 49% of White individuals report being able to work from home, only 34 to 39% of Black individuals have the same privilege [42]. Furthermore, Black Americans are disproportionately employed in low-wage and high-contact essential service industries [43] within which sick leave is often discouraged and uncompensated. Compounding these issues, low-wage earners have more children [44] with an average of 2.4 dependent family members [45]. In the absence of sick leave benefits under these circumstances, infectious individuals in essential service industries are more likely to spread COVID-19 to their disproportionately Black coworkers [43]. Similar factors may be driving the higher mortality rate observed in Black males compared to Black females, in addition to the significantly higher risk of COVID-19 mortality experienced by men compared to women [46] and the higher baseline mortality rate experienced by Black men [47].
Our results regarding the duration between symptom onset and hospitalization indicate that Black COVID-19 patients do not receive medical attention as promptly as their White counterparts, a factor which is known to influence survival [48]. Financial barriers and distrust deterring care-seeking, [43,49] test scarcity, and racial bias among healthcare providers [50] may be driving this delay, among other factors. In the US, Black and Hispanic/Latinx populations represent 12.3% and 17.6% of the total employed population, and make up 25% to 40% of those employed in industries experiencing the highest proportion of job losses due to COVID-19 [30,51]. The disproportionate burden of unemployment in these communities, and the precarious linkage of health insurance to employment in this country, may be serving as a deterrent to care-seeking when COVID-19 symptoms arise. As families struggle to endure job losses with limited resources, the COVID-19 pandemic places the most vulnerable in the precarious situation of having to decide between staying at home and safeguarding against infection or seeking out employment as a means for financial survival. Furthermore, with the longstanding history of unethical treatment in public health and medicine, new challenges may arise as medical advances become available. Individuals may distrust the medical system due to historical unethical and inhumane treatment of marginalized populations, which could delay treatment [43]. Upon seeking medical attention, those living in densely populated inner cities have faced inadequate access to testing [52]. These issues interplay with the racial composition of an area. Detroit, the most populous city in Michigan, is also home to a larger proportion of Black individuals than any other city in the United States. Additionally, the SARS-CoV-2 test used in Detroit during the early months of the pandemic was found to miss 45% of positive cases [53,54]. Patients receiving these false negative results are likely to have received delayed or inappropriate care, compounding the other factors described above. Finally, physician racial biases may affect patient health outcomes [50,55].
Racial disparities in access to healthcare, educational opportunities and economic security predate the COVID-19 epidemic. At least 90% of the ZCTAs within the predominantly Black cities of Detroit and Flint have rates of child poverty that are higher than the national average [56]. The anti-Black systemic racism in our political system is paralleled by the racialized nature of COVID-19 [43]. Inadequate governance nationwide has hindered pandemic response, analogous to the ongoing mishandling of the Flint water crisis that has arisen from a series of misguided governmental, social, and economic policies [57]. The effects of COVID-19 shown here highlight a need for corrective resource allocation by federal and local governments that would mitigate the toll of public health crises on vulnerable populations. Universal healthcare, living wages for all workers, and paid sick leave are essential public health interventions for addressing racial inequities in the US.
Moreover, public health must also concentrate efforts to target and eliminate pathways to inequality. In the face of the COVID-19 pandemic, institutionalized drivers of inequality such as the prison industrial complex have highlighted the glaring disparities affecting racial minorities. In 2018, the State of Michigan had 8604 commitments. While breakdowns for specific races are not available, a total of 47.0% of the male prison population and 32.2% of the female prison population were non-White despite the state's population being 79.2% White [58]. Estimates from research centers suggest Black individuals comprise 53% of the prison population and 37% of the jail population while only comprising 15% of the state population [59]. With overcrowding, inability to maintain social distancing, reduced access to soap or sanitizers, and reduced availability of personal protective equipment, incarceration presents an avenue for widespread transmission of disease in the Black prison, jail and detention center populations as a whole [60]. As public health practitioners, we must work diligently to eliminate such drivers of inequality and work to fundamentally restructure prison systems as a public health intervention to reduce disparities and promote health.
Over the course of the epidemic in Michigan, several public health measures were implemented to curb transmission. A statewide stay-at-home order was placed between March 24 and June 1, 2020, alongside business restrictions such as prohibiting dining at restaurants and large gatherings. Other factors such as household size, employment in essential services, use of public transportation, and adherence to mask-wearing and stay-at-home orders can also impact infection exposure as well as mortality risk. In Detroit, the most impacted area in Michigan, social distancing in April was adhered to by 48.3% of non-Black individuals and 41.7% of Black individuals [61]. These measures likely contributed towards limiting exposure to infection which may have impacted the eventual decline in mortality after mid-April. However, due to lack of sufficient data, we were unable to integrate these characteristics into our study framework. We were only able to deduce time to hospitalization for a subset of all decedents due to missing data on symptom onset date, hospitalization date or both. There was also heterogeneity in missingness of this data across races, indicating a possible association with delays in receiving care. By conducting a Chi-Square test (Table S4), we compared the demographic profile of decedents for whom time to hospitalization could not be ascertained from data with the rest of the decedents. The demographic profile of individuals with missing time to hospitalization best resembled individuals who were hospitalized within 3 days of symptom onset. Therefore, it may be unlikely that missing data is associated with delays in hospitalizations, but a deeper understanding of this relationship requires additional evidence.
There is also a complex relationship between economic deprivation and systemic racism in terms of COVID-19 mortality risk. These underlying factors could provide deeper insight into the drivers of racial disparities in COVID-19 mortality across Michigan, as well as other US states. Under-reporting of COVID-19 may also be driven by racial disparities, which would exacerbate the current situation. To address this issue, further analysis and data is required to investigate the relationship between COVID-19 testing availability and healthcare accessibility throughout the state. While our analysis of COVID-19 deaths is specific to Michigan, our findings of increased mortality rates after stratifying for key demographic and health variables are consistent with the increased mortality burden experienced by Black individuals nationwide [4]. The mortality of COVID-19 is skewed towards the elderly and those with one or more comorbidities, as also observed in our data. Our study was limited by the absence of population-level comorbidity data for those under age 65 in the state of Michigan, and thus national-level estimates were used instead. However, given the similar comorbidity burdens observed nationally and in Michigan for those 65 and older, [33] this is unlikely to alter our overall findings.
As the COVID-19 pandemic continues to unfold, it is imperative to ameliorate disparities as both a pandemic response and prevention measure. Systemic disenfranchisement of Black individuals in the US underlies circumstances leading to racial disparities in COVID-19 exposure, the timeliness of treatment and case fatality rates [43]. While structural racism as an infectious disease risk factor is increasingly being recognized, [62] the US response to this pandemic demonstrates our society's continued negligence toward the wellbeing of all Americans. It is not only the longstanding increased risk of comorbidities in the Black population that drives racial disparities in COVID-19 mortality, but socio-political and economic factors that impact COVID-19 exposure and medical care. Rectifying these inequities is urgent both to limit the devastation of COVID-19 and to protect against future public health crises.
Author contributions
ASP and APG conceived the study. LM, JD, and JC collected the data. ASP, AP, IM, and CRW designed the study. ASP conducted data analysis. ASP drafted the manuscript with contributions from AP, IM, CRW, and AES. MCF and APG revised the manuscript. AP and APG supervised the research. All authors reviewed the manuscript and agreed to be responsible for all aspects of the work.
Data sharing
Individual-level data used in this study cannot be made publicly available but aggregated COVID-19 data provided by the Michigan Department of Health and Human Services is freely available to the public. ASP, AP, IM, and LM had access to the data used in the study.
Funding
ASP, AP and APG were funded by NSF Expeditions grant 1918784, NIH grant 1R01AI151176-01, NSF Rapid Response Research for COVID-19 grant RAPID-2027755, and the Notsew Orm Sands Foundation. MCF was supported by NIH grant K01AI141576.
Declaration of Competing Interest
All authors have nothing to disclose.
Acknowledgments
We would like to thank Seth Eckel and Adam Hart for linking Vital Records and MDSS data, and to remember all those in Michigan who lost their lives to COVID-19.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.eclinm.2021.100761.
Appendix. Supplementary materials
References
- 1.Dee D.L., Bensyl D.M., Gindler J. Racial and ethnic disparities in hospitalizations and deaths associated with 2009 pandemic Influenza A (H1N1) virus infections in the United States. Ann Epidemiol. 2011;21:623–630. doi: 10.1016/j.annepidem.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 2.P. Andrulis D., Siddiqui N.J., Purtle J., Cooper M.R. H1N1 Influenza pandemic and racially and ethnically diverse communities in the United States. Office of Minority Health U.S. Department of Health and Human Services, 2012 https://www.texashealthinstitute.org/uploads/1/3/5/3/13535548/thi_pandemic_influenza__equity_report_2012.pdf.</bib>
- 3.Stokes E.K., Zambrano L.D., Anderson K.N. Coronavirus disease 2019 case surveillance - United States, January 22-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:759–765. doi: 10.15585/mmwr.mm6924e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wortham J.M., Lee J.T., Althomsons S. Characteristics of persons who died with COVID-19 - United States, February 12-May 18, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:923–929. doi: 10.15585/mmwr.mm6928e1. [DOI] [PubMed] [Google Scholar]
- 5.United States Census Bureau QuickFacts. https://www.census.gov/quickfacts/fact/table/US/PST045219 (accessed July 14, 2020).
- 6.COVID-19 provisional counts - weekly updates by select demographic and geographic characteristics. 2020; published online May 20. https://www.cdc.gov/nchs/nvss/vsrr/covid_weekly/index.htm (accessed May 22, 2020).
- 7.Population By County–Five Year Age Groups. https://www.mdch.state.mi.us/pha/osr/Population/FiveYearPopCo.asp (accessed June 1, 2020).
- 8.Michigan Disease Surveillance System and Vital Records. Coronavirus - Michigan Data. State of Michigan. https://www.michigan.gov/coronavirus/0,9753,7-406-98163_98173—,00.html (accessed Jan 21, 2021).
- 9.Khazanchi R., Evans C.T., Racism Marcelin JR. Not race, drives inequity across the COVID-19 continuum. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.19933. [DOI] [PubMed] [Google Scholar]
- 10.Golestaneh L., Neugarten J., Fisher M. The association of race and COVID-19 mortality. EClinicalMedicine. 2020 doi: 10.1016/j.eclinm.2020.100455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gee G.C., Ford C.L. Structural racism and health inequities: old issues, new directions. Du Bois Rev. 2011;8:115–132. doi: 10.1017/S1742058X11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams D.R., Lawrence J.A., Davis B.A. Racism and health: evidence and needed research. Annu Rev Public Health. 2019;40:105–125. doi: 10.1146/annurev-publhealth-040218-043750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tourse R.W.C., Hamilton-Mason J., Wewiorski N.J. Springer; Cham: 2018. Systemic racism in the United States: scaffolding as social construction. [Google Scholar]
- 14.Schulz A.J., Williams D.R., Israel B.A., Lempert L.B. Racial and spatial relations as fundamental determinants of health in Detroit. Milbank Q. 2002;80:677–707. doi: 10.1111/1468-0009.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mehdipanah R., Ramirez J., Abedin S., F. Brown S. Housing discrimination and health: understanding potential linking pathways using a mixed-methods approach. Soc Sci. 2018;7:194. [Google Scholar]
- 16.Karpman M., Zuckerman S., Gonzalez D., Kenney G.M. Urban Institute; 2020. The COVID-19 pandemic is straining families’ abilities to afford basic needs.https://www.urban.org/research/publication/covid-19-pandemic-straining-families-abilities-afford-basic-needs published online April 27. (accessed July 14, 2020) [Google Scholar]
- 17.Kaiser Family Foundation . Kaiser Family Foundation; 2019. Poverty rate by race/ethnicity. published online Dec 4. https://www.kff.org/other/state-indicator/poverty-rate-by-raceethnicity/?currentTimeframe=0&sortModel =%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D (accessed July 15, 2020) [Google Scholar]
- 18.MiCalhoun. MiCalhoun: demographics: State: Michigan. http://www.micalhoun.org/index.php?module=DemographicData&controller=index&action=index (accessed July 14, 2020).
- 19.Hong R., Baumann B.M., Boudreaux E.D. The emergency department for routine healthcare: race/ethnicity, socioeconomic status, and perceptual factors. J Emerg Med. 2007;32:149–158. doi: 10.1016/j.jemermed.2006.05.042. [DOI] [PubMed] [Google Scholar]
- 20.Canedo J.R., Miller S.T., Schlundt D., Fadden M.K., Sanderson M. Racial/ethnic disparities in diabetes quality of care: the role of healthcare access and socioeconomic status. J Racial Ethn Health Disparities. 2018;5:7–14. doi: 10.1007/s40615-016-0335-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mack J. mlive; 2019. Flint and Detroit among nation's top 5 poorest cities, new census data shows.https://www.mlive.com/news/2019/09/flint-and-detroit-among-nations-top-5-poorest-cities-new-census-data-shows.html published online Sept 26. (accessed Sept 4, 2020) [Google Scholar]
- 22.Shen Y., Li C., Dong H. Community outbreak investigation of SARS-CoV-2 transmission among bus riders in Eastern China. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.5225. published online Sept 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Finch W.H., Hernández Finch M.E. Poverty and covid-19: rates of incidence and deaths in the United States during the first 10 weeks of the pandemic. Front Sociol. 2020;5 doi: 10.3389/fsoc.2020.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fiscella K., Franks P., Gold M.R., Clancy C.M. Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2000;283:2579–2584. doi: 10.1001/jama.283.19.2579. [DOI] [PubMed] [Google Scholar]
- 25.Gaskin D.J., Thorpe R.J., Jr, McGinty E.E. Disparities in diabetes: the nexus of race, poverty, and place. Am J Public Health. 2014;104:2147–2155. doi: 10.2105/AJPH.2013.301420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.ICNARC report on COVID-19 in critical care. Intensive care national audit & research centre, 2020 https://www.icnarc.org/About/Latest-News/2020/03/22/Report-On-196-Patients-Critically-Ill-With-Covid-19?fbclid=IwAR22TXPZ8p_Ow8HF9ZzvHcVrvn8jPQO4lAJ55h3arOpM7WwdjlI3Bi0hcO4.
- 27.Products - Data Briefs - Number 94 - May 2012. 2019; published online June 6. https://www.cdc.gov/nchs/products/databriefs/db94.htm (accessed Sept 3, 2020).
- 28.Kochanek K.D., Murphy S.L., Xu J., Arias E. Deaths: final data for 2017. National Vital Statistics Reports. 2019;68:1–77. [PubMed] [Google Scholar]
- 29.Guan W.-.J., Liang W.-.H., Zhao Y. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55 doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Adams-Prassl A., Boneva T., Golin M., Rauh C. 2020. Inequality in the impact of the coronavirus shock: evidence from real time surveys. 2020.https://papers.ssrn.com/abstract=3594297 published online April 1. (accessed June 1. [Google Scholar]
- 31.Population By County–Five Year Age Groups. https://www.mdch.state.mi.us/pha/osr/Population/FiveYearPopCo.asp (accessed June 15, 2020).
- 32.Chronic conditions | CMS. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/CC_Main (accessed June 15, 2020).
- 33.Multiple chronic conditions | CMS. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/MCC_Main (accessed June 15, 2020).
- 34.Co-morbidity | CMS. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/Co-morbidity (accessed June 15, 2020).
- 35.Health policy data requests - percent of U.S. Adults 55 and over with chronic conditions. 2019; published online Feb 7. https://www.cdc.gov/nchs/health_policy/adult_chronic_conditions.htm (accessed June 16, 2020).
- 36.Decennial Census All 5-digit ZIP code tabulation areas fully/partially within Michigan. United States Census Bureau. 2010 https://data.census.gov/cedsci/table?q=All%205-Digit%20ZIP%20Code%20Tabulation%20Areas%20fully%2F partially%20within%20Michigan&tid=DECENNIALSF12010.P1&hidePreview=false (accessed July 11, 2020) [Google Scholar]
- 37.United Nations. ‘The pandemic is exposing and exploiting inequalities of all kinds, including gender inequality’ | United Nations. https://www.un.org/en/un-coronavirus-communications-team/pandemic-exposing-and-exploiting-inequalities-all-kinds-including (accessed Aug 5, 2020).
- 38.Williamson E.J., Walker A.J., Bhaskaran K. OpenSAFELY: factors associated with COVID-19 death in 17 million patients. Nature. 2020 doi: 10.1038/s41586-020-2521-4. published online July 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Public Health England Disparities in the risk and outcomes of COVID-19. Public Health England. 2020 https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/908434/Disparities_in_the_risk_and_outcomes_of_COVID_August_2020_update.pdf [Google Scholar]
- 40.Raisi-Estabragh Z., McCracken C., Bethell M.S. Greater risk of severe COVID-19 in Black, Asian and minority ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: study of 1326 cases from the UK Biobank. J Public Health. 2020;42:451–460. doi: 10.1093/pubmed/fdaa095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.White C., Coronavirus Nafilyan V. England and Wales - Office for National Statistics. Office for National Statistics; 2020. COVID-19) related deaths by ethnic group.https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/coronavirusrelateddeathsbyethnicgroupenglandandwales/latest (accessed Sept 3, 2020) [Google Scholar]
- 42.Dey M., Frazis H., Loewenstein M.A., Sun H. 2020. Ability to work from home: evidence from two surveys and implications for the labor market in the COVID-19 pandemic.https://www.bls.gov/opub/mlr/2020/article/ability-to-work-from-home.htm published online June 24. (accessed Oct 30, 2020) [Google Scholar]
- 43.Poteat T., Millett G., Nelson L.E., Beyrer C. Understanding COVID-19 risks and vulnerabilities among black communities in America: the lethal force of syndemics. Ann Epidemiol. 2020 doi: 10.1016/j.annepidem.2020.05.004. published online May 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.US Census Bureau . US Census Bureau; 2019. Household income and income per household member among women with a birth in the past year, by marital status: 2006-2017.https://www.census.gov/data/tables/time-series/demo/fertility/household-income.html published online Sept 23. (accessed Nov 2, 2020) [Google Scholar]
- 45.Oxfam America . 2014. Working poor in America.https://s3.amazonaws.com/oxfam-us/www/static/media/files/Working-Poor-in-America-report-Oxfam-America.pdf [Google Scholar]
- 46.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Michigan Department of Health and Human Services . 2019. Life expectancy by sex and race, Michigan. Michigan department of community health.https://www.mdch.state.mi.us/osr/deaths/lifesxrctrend.asp published online July. (accessed Dec 18, 2020) [Google Scholar]
- 48.Wiersinga W.J., Rhodes A., Cheng A.C., Peacock S.J., Prescott H.C. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;324:782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- 49.Galvani A.P., Parpia A.S., Pandey A., Zimmer C., Kahn J.G., Fitzpatrick M.C. The imperative for universal healthcare to curtail the COVID-19 outbreak in the USA. EClinicalMedicine. 2020;23 doi: 10.1016/j.eclinm.2020.100380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hall W.J., Chapman M.V., Lee K.M. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105:e60–e76. doi: 10.2105/AJPH.2015.302903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Employed persons by detailed occupation, sex, race, and Hispanic or Latino ethnicity. 2020; published online Jan 22. https://www.bls.gov/cps/cpsaat11.htm (accessed June 1, 2020).
- 52.Stockman F. The New York Times; 2020. Sick people across the U.S. say they are being denied the coronavirus test.https://www.nytimes.com/2020/03/12/us/coronavirus-testing-challenges.html published online March 12. (accessed Sept 3, 2020) [Google Scholar]
- 53.Basu A., Zinger T., Inglima K. Performance of Abbott ID Now COVID-19 rapid nucleic acid amplification test using nasopharyngeal swabs transported in viral transport media and dry nasal swabs in a New York city academic institution. J Clin Microbiol. 2020;58 doi: 10.1128/JCM.01136-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.2020. Covid-19 test used by detroit misses half of positive cases, study finds.https://www.deadlinedetroit.com/articles/25267/covid-19_test_used_by_detroit_misses_half_of_positive_cases_study_finds (accessed Oct 15. [Google Scholar]
- 55.Greenwood B.N., Hardeman R.R., Huang L., Sojourner A. Physician-patient racial concordance and disparities in birthing mortality for newborns. Proc Natl Acad Sci U S A. 2020;117:21194–21200. doi: 10.1073/pnas.1913405117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.United States Census Bureau. Poverty status in the past 12 months. 2019 American community survey 5-year estimates subject tables. 2020. https://data.census.gov/cedsci/table?t=Income%20and%20Poverty&g=0100000US.860000&tid=ACSST5Y2018.S1701&hidePreview=false (accessed Nov 3, 2020).
- 57.Sadler R.C., Highsmith A.R. Rethinking tiebout: the contribution of political fragmentation and racial/economic segregation to the flint water crisis. Environ Justice. 2016;9:143–151. [Google Scholar]
- 58.Michigan department of corrections. Michigan department of corrections 2018 statistical report. Michigan department of corrections, 2019 https://www.michigan.gov/documents/corrections/MDOC_2018_Statistical_Report_-_2019.07.18_662129_7.pdf.
- 59.Vera Institute of Justice. Incarceration Trends in Michigan. Vera Institute of Justice. 2019. https://www.vera.org/downloads/pdfdownloads/state-incarceration-trends-michigan.pdf (accessed Jan 27, 2021).
- 60.Simpson P.L., Butler T.G. Covid-19, prison crowding, and release policies. BMJ. 2020;369:m1551. doi: 10.1136/bmj.m1551. [DOI] [PubMed] [Google Scholar]
- 61.Henry-Nickie M., Hudak J. Social distancing in Black and white neighborhoods in Detroit: a data-driven look at vulnerable communities. Brookings. 2020 https://www.brookings.edu/blog/fixgov/2020/05/19/social-distancing-in-black-and-white-neighborhoods-in-detroit-a-data-driven-look-at-vulnerable-communities/ published online May 19. (accessed Dec 26, 2020) [Google Scholar]
- 62.Bailey Z.D., Krieger N., Agénor M., Graves J., Linos N., Bassett M.T. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389:1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.