Abstract
Compared with traditional tumor therapy strategies, hydrogel as a drug reservoir system can realize on-demand drug release and deep tissue penetration ability. It also exhibits great tumor-site retention to enhance the permeability and retention effect of tumor treatment. This can significantly overcome the drug's resistance and severe side effects. Inorganic/organic composite hydrogel has attracted wide attention due to its combined effects, enhancing therapeutic effects against various kinds of tumors. In situ injectable hydrogel can securely restrict the drugs in the lesion sites without leakage and guarantee better biosafety. Moreover, hydrogel possesses interconnected macropores which can provide enough space for nutrient transport, cellular activity, and cell–cell interactions. Thermal therapy is an effective strategy for tumor therapy due to its minimal invasiveness and high selectivity. Because the location temperature can be precisely controlled and helps avoid the risks of destroying the body's immune system and ablate normal cells, thermal therapy exhibits significant treatment outcomes. Nonetheless, when the cellular temperature reaches approximately 43 °C, it causes long-term cell inactivation. Based on these merits, thermosensitive hydrogel formulation with adaptive functions shows excellent efficacy, unlimited tissue penetration capacity, and few deleterious side effects. Furthermore, the thermosensitive hydrogel has unique physical properties under the external stimuli, which is the ideal drug delivery system for on-demand release in tumor treatment. This article will review the state of the thermosensitive hydrogel in clinic application for cancer therapy.
Keywords: Thermosensitive, Hydrogel, Tumor, Thermotherapy
Introduction
Over the past years, researchers have focused their attention on 3D biomaterials since the cross-linked macropores provide enough space for nutrient transport, cell activity, and cell–cell interactions [1]. As the ideal drug carriers, the hydrogel has minimal invasiveness. It can form desired shapes to meet the requirement of irregular lesion sites in cancer therapy [2]. The traditional hydrogel is usually fabricated through physical interaction or chemical binding of constituting polymer, which has minimal effects on their function [3]. Hydrogel as a drug delivery system should respond to endogenous/exogenous stimuli, thereby ensuring the drug on-demand release in the lesion sites and reducing unnecessary side effects on normal tissues [4]. Functional inorganic nanomaterial incorporated into the hydrogel can significantly overcome the intrinsic limits, which has other fascinating properties and remarkably improves stimuli-responsive therapeutic efficacy [5–7].
Thermal therapy has the advantages of local temperature controlling and minimal invasiveness, which became a novel therapy approach after chemotherapy, radiotherapy, and surgical intervention in current tumor treatment [8]. Based on hydrogel inorganic material mediated thermotherapy with the unique physical feature under certain stimuli, it is the ideal agent delivery platform for on-demand drug dose therapy in lesion sites [9–11]. Compared with traditional synergistic therapeutic approaches (chemo/radiotherapy, chemo/photodynamic therapy, and photodynamic/photothermal therapy), thermosensitive hydrogel loaded with antitumor drugs. This can help penetrate drugs into deep tissues, form desired shapes to fill the irregular tissues, and promote wounds healing [12]. Also, mild temperature heating can enhance chemotherapy outcomes by improving cytomembrane's permeability to increase cellular uptake of drugs and control drug release from the hydrogel. When the cellular temperature exceeds 41 °C, protein denaturation and temporary cell inactivation occur, and this lasts for several hours. When the temperature reaches approximately 43 °C, it causes long-term cell inactivation [13]. Moreover, injecting thermosensitive hydrogel in situ into the lesion sites can avoid the risk of drug accumulation at the liver and spleen to improve therapy outcomes and guarantee better biosafety in vivo [14].
The benefit of the thermosensitive hydrogel in the clinic can facilitate administration, improve therapeutic efficacy in the lesion region, and reduce unnecessary damage to normal tissues, thereby improving patient compliance. This article will summarize some thermosensitive hydrogels to improve disease treatment and make the current state of the hydrogel in clinic application.
Magnetic Hyperthermia Hydrogel
It is well known that the doping concentration of inorganic nanoparticles into the hydrogel can inevitably affect the intrinsic hydrogel properties, which usually shows dose-dependence [15]. The high concentration of agents would enhance the therapeutic efficacy. However, unnecessarily it deteriorates the rheological properties of the hydrogel, resulting in burst release, uncontrolled treatment, and severe side effects on normal tissues [16].
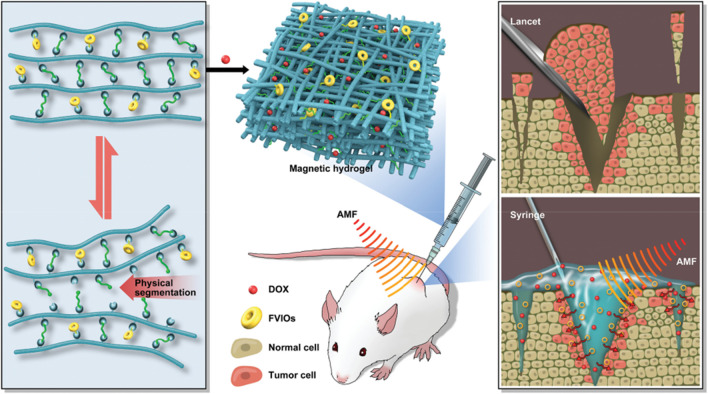
It is challenging to fabricate high-performance nanoparticle hydrogel, which should balance hydrogel's intrinsic properties and associate the functions associated with the inorganic nanoparticle loading process. This contradiction is very obvious in designing magnetic hydrogel in the synergistic thermos-chemotherapy for highly efficient postsurgical treatment [17]. This shortcoming would be effectively overcome, providing good rheological properties and sufficient heating efficiency. This is based on glycol-chitosan, difunctional telechelic poly (ethylene glycol) (DT-PEG), and ferromagnetic vortex-domain iron oxide (FVIOs) as the raw materials (Fig. 1) [18]. Compared with traditional magnetic hydrogel, the obtained magnetic hydrogel overcomes the side effects and exhibits remarkable rheological properties and high heating convert ability in an alternating magnetic field [19]. Further, this self-adapting magnetic hydrogel regulates the drug in a long-term sustainable manner. It directly targets the lesion sites. Magnetic hyperthermia can promote the internalization of a drug, eventually causes cancer cells apoptosis and reducing tumor size. The FVIO-incorporated hydrogel has the features of self-healing, fast gelation, and self-confirming ability, which can satisfy synergistic thermos-chemotherapy and provide an alternative strategy for addressing the unmet clinical need. This work underlines the potential promise for the precision of the injection sites. It enhances the magnetic hyperthermia efficiency for xenograft tumor treatment.
Fig. 1.
Illustrates FVIO-functionalized magnetic hydrogel with optimal adaptive functions for breast cancer postoperative recurrence prevention [18]. Copyright 2019 Adv. Healthcare Mater
Near-Infrared Light Absorption Hydrogel
Photothermal therapy (PTT) has attracted wide attention due to its unbeatable advantages in cancer treatment, including control treatment and satisfactory cancer eradication outcomes [20–22]. However, conventional PTT has poor penetration into the site of the deep lesions, bring harmful effects on therapy. Chemotherapy and PTT synergistic strategy might be a well-pleasing candidate to enhance the tumor therapeutic efficacy [23].
Various photothermal materials have been widely exploited as drug delivery carriers or coupling reagents for cancer therapy, including metal–organic frameworks and carbon dots [24–27]. Among these materials, conjugated polymer dots (Pdots) are biocompatible, degradable, and nontoxic biomaterial with easy functionalization. These are small in size and extraordinary photophysical properties [28–31]. More importantly, Pdots with strong optical absorption properties and photostabilities in the near-infrared (NIR) light window are satisfying agents for PTT and photoacoustic imaging (PAI) [32–34]. Iohexol is an efficient and safe contrast agent approved by U.S. Food and Drug Administration for body computed tomography (CT) imaging [35]. However, the time of Iohexol for CT imaging is very short, and this inevitable shortcoming limits Iohexol widely used in the clinic [26]. Grating iohexol into Pdots-DOX-based thermosensitive hydrogel can successfully overcome this disadvantage of iohexol for enhanced CT imaging ability. This makes hydrogel an excellent candidate used in cancer theranostics.
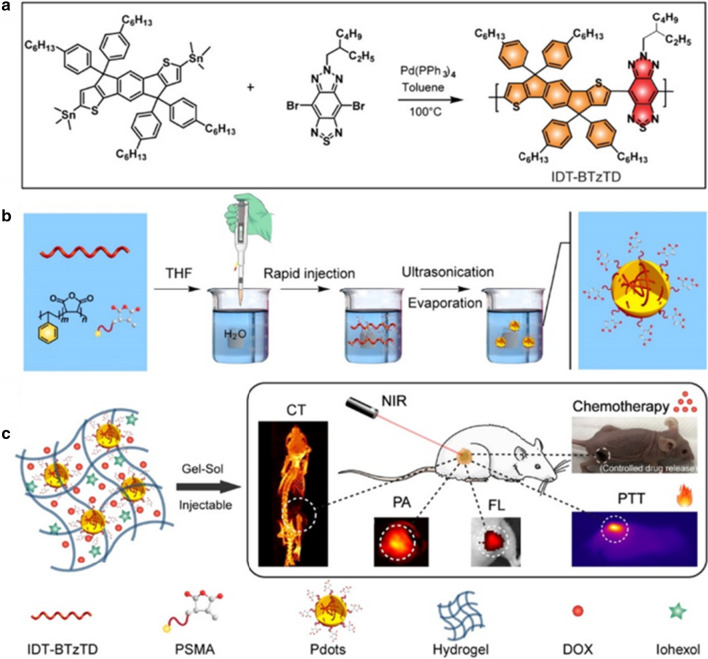
Based on these merits, Men et al. introduced a multifunction Pdots@hydrogel drug delivery platform with good biodegradability, strong NIR absorption ability, high photothermal conversion efficiency, and controlling drug release, well-pleased CT/PA/fluorescence imaging ability, and enhanced tumor therapeutic outcomes (Fig. 2) [36]. The obtained NIR light-mediated Pdots-DOX-iohexol@hydrogel system exhibits strong photothermal effects. It achieved dose-control chemotherapy by interval NIR light irradiation, superior tissue penetration, and minimal invasion in cancer treatment, thus inhibiting tumor growth. More importantly, the nanoengineering modality for the Pdots-DOX-iohexol@hydrogel possesses excellent CT/FL/PA imaging ability and high biocompatibility for cancer detection. Therefore, the concept of integrating various diagnostic/therapeutic agents into one system can be potentially applied to various perspectives of disease therapy in the clinic.
Fig. 2.
a Schematic of the fabrication of conjugated polymer IDT − BTzTD. b Schematic of the fabrication of IDT − BTzTD Pdots. b Schematic of the Pdots − DOX − iohexol@hydrogel for trimodal FL/PA/CT imaging-guided synergistic chemo-photothermal cancer therapy [36]. Copyright 2020 ACS Appl. Mater. Interfaces
Photothermal Effects Bifunctional Hydrogel
At present, the treatment of bone tumors mainly depends on surgical intervention and chemo/radiotherapy synergetic approaches, which significantly improves patients' survival rate [37]. However, surgical intervention always causes bone defects. It incompletely removes tumor cells, making bone tissues hard to heal by themselves, and residual cancer cells proliferate within several days. Therefore, it is significant to develop a biomaterial with tumor therapy and simultaneously promote bone regeneration after surgery.
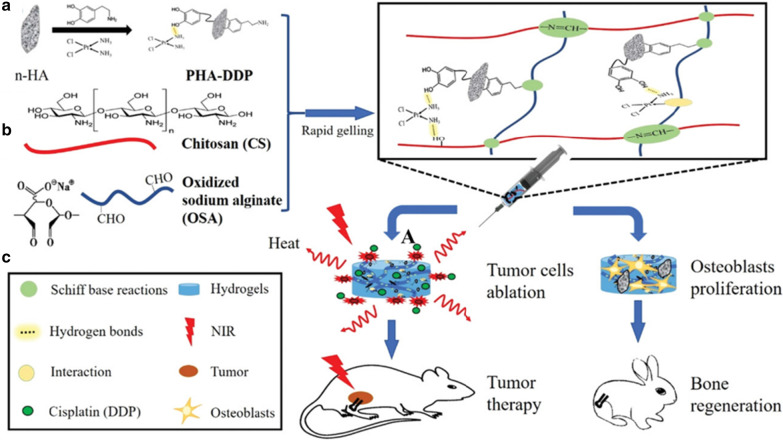
Injectable hydrogel as a promising alternative approach can form desired shapes to fill defects tissues. Its components are very similar to bone tissues for improving osteogenic ability [38]. The injectable hydrogel applied in bone tissue engineering should be slow enough to meet surgical handing and simultaneously be fast enough to realize stability and function after injection in vivo [39]. In order to solve these issues, Luo and his co-works provided a novel bifunctional injectable hydrogel. This hydrogel used polydopamine (PDA) to modify nano-hydroxyapatite (n-HA) and immobilize cisplatin (DDP) to fabricate PHA-DDP particles. It was then introduced PHA-DDP particles into the Schiff based on the reaction system between chitosan (CS) and oxidized sodium alginate (OSA) (Fig. 3) [40]. Nano-hydroxyapatite (n-HA) played an important role in bone formation, which is the major inorganic material in bone tissues and composed of calcium and phosphorus elements [41]. Mussel-inspired PDA as the ideal candidate for photothermal agents has good biocompatibility and biodegradability and has abundant functional groups. Mussel-inspired PDA easily deposits on various substances, such as loading antitumor drugs (cisplatin, DDP) through hydrogen bonding or other interactions [42–44]. Additionally, n-HA was modified into PDA to obtain PDA decorated n-HA (PHA), improving cell adhesion and proliferation [45].
Fig. 3.
Schematic illustration of the formation of bifunctional OSA-CS-PHA-DDP hydrogels and bioapplication [40]. Copyright 2019 Macromol. Biosci
The successfully obtained OSA-CS-PHA-DDP injectable hydrogel has excellent PDA photothermal effects of inhibiting tumor growth via local hyperthermia under laser irradiation. Further, mild photothermal effects can improve the permeability of cytomembrance to increase the cellular uptake of antitumor drugs. They can destroy hydrogen bond interactions between DDP and PDA to improve drug release and enhance tumor treatment effects. More importantly, PDA's abundant functional group can promote bone mesenchymal stem cell proliferation and adhesion and further facilitate new bone tissue formation. This bifunctional hydrogel integrates tumor treatment with bone regeneration based on these properties. It shows a promising approach for tumor-related bone defects in the clinic.
PTT/PDT-Responsive Agarose Hydrogel
Tumor vascularity has poor integrity of structure, resulting in insufficient oxygen supply in tumor regions. Hypoxia condition causing an acidic tumor microenvironment by increasing production of lactic acid via anaerobic glycolysis [46]. Thus, hypoxia and low pH are the common features of tumor microenvironment severely compromising therapeutic efficacy.
Photothermal therapy destructs tumor tissues based on local hyperthermia mediated by photothermal agents under laser irradiation [47]. Thus, various kinds of photothermal agents have been developed to satisfy PTT performance [48]. However, most of them still have some drawbacks in clinical application, such as non-degradability, low biosafety and complex synthesis progress. Humic acid (HA) has excellent photothermal conversion ability and photoacoustic (PA) imaging, which is extracted from biochemical humification of animal and plants matter and it has attracted increasing attention in PTT [49]. Meanwhile, photodynamic therapy (PDT) is another effective strategy for tumor therapy by utilizing the oxygen reactive species (ROS) generated from oxygen molecules in the presence of photosensitizers (PS) under laser excitation [50]. Chlorin e6 has high ROS production yield and low dark toxicity, which has been widely used in PDT [51]. But, intrinsic hypoxia microenvironment can compromise therapeutic effects during PDT progress.
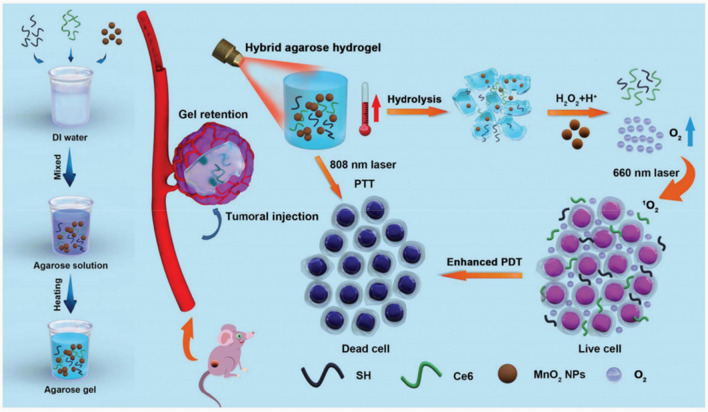
LMP agarose hydrogel melts at the temperature above 65 °C and sol-to-gel transition begins at the temperature under 25 °C during the cooling process, which displays great potential for on-demand drug administration by precisely regulating various temperature [7, 52]. Therefore, rational designed and functionalized LMP agarose hydrogel is a promising approach to realizing high drug bioavailability and enhancing therapeutic outcome through one single injection. As Fig. 4 is shown, Hou et al. provided a novel “co-trapped” approach by simultaneously incorporating SH, Ce6 and MnO2 nanoparticles into low melting point (LMP) agarose, and the obtained agarose@SH/MnO2/Ce6 hybrid hydrogel was successfully used to improve PTT/PDT through ameliorate tumor hypoxia environment [53]. After, as-synthesized hybrid hydrogel was injected into the tumor areas, exhibiting excellent biocompatibility and biodegradability, especially when it was precisely introduced into the innermost. Further, MnO2 and Ce6 can be continuously permeated into the surrounding environment by softening and hydrolyzing hybrid hydrogel. More importantly, SH as light absorber converts light into thermal under laser irradiation, thus hydrogel itself can be applied in PTT. What’s more, MnO2 released from hydrogel can catalyze excessive H2O2 in tumor tissues to generate oxygen, which can enhance PDT outcomes upon being exposed under 660 nm laser and attenuate tumor hypoxia environment. This multifunction agarose@SH/MnO2/Ce6 hybrid hydrogel was injected into the tumor sites without entering the circulatory system, which help avoid potential biohazard and being cleared by the body immune system. Therefore, it achieves “one injection, multiple therapies”, and inspires us to exploit suitable hydrogel-based approaches to various disease therapy in clinic.
Fig. 4.
Schematic diagram of the synthesis process and working principle of the agarose@SH/MnO2/Ce6 hydrogel. Effective tumor inhibition was accomplished through enhanced photo-induced tumor therapy on the basis of the relief of tumor hypoxia [53]. Copyright 2020 Biomater Sci
Perspectives
Thermal therapy has the advantages of minimal invasiveness and high selectivity, which is an effective strategy for tumor therapy in clinic [54, 55]. Compared with conventional approaches, thermal therapy can precisely control local temperature and effectively avoid unnecessary side effects such as damaging normal issues and destroying body immune system [56]. When the cell temperature reaches 41 °C, cell becomes temporarily inactive and causes protein denaturation, and this condition lasts for several hours. As the temperature arrives at 43 °C, it may cause long-term cells inactivation. Although thermal therapy has achieved much exciting progress in the field of tumor therapy, there is still a lack of safe and effective photothermal agents or drug carriers with good biocompatibility and biodegradability.
Hydrogel is the ideal candidate for drugs carrier with good biocompatibility and biodegradability in current tumor treatment. Incorporating inorganic/organic into hydrogel has attracted widely attention due to their cooperative effects which can enhance therapy effects against tumor. Among various responsive hydrogel, thermosensitive hydrogel can precisely and continuously control drug release through temperature stimulus in tumor tissues. Compared with percutaneous and intravenous injection methods, the accurate locate injected administration hydrogel within the agents has better biosafety in vivo [57].
Conclusions
Despite the significant merits of hydrogel, the clinical application has been limited due to unsatisfactory biodistribution, poor biocompatibility, and poor tumor penetration ability. In this article, thermosensitive hydrogel has the advantages of better biocompatibility, excellent tumor inhibit ability, and no unnecessary side effects. These merits will further promote their application in clinic for various disease treatment.
Acknowledgements
Not applicable.
Abbreviations
- DT-PEG
Difunctional telechelic poly (ethylene glycol)
- FVIOs
Ferromagnetic vortex-domain iron oxide (FVIOs)
- PTT
Photothermal therapy
- Pdots
Polymer dots
- NIR
Near-infrared
- PAI
Photoacoustic imaging
- CT
Computed tomography
- PDA
Polydopamine
- N-HA
Nano-hydroxyapatite (n-HA)
- DDP
Immobilize cisplatin
- CS
Chitosan (CS)
- OSA
Oxidized sodium alginate
- DDP
Cisplatin
- HA
Humic acid
- HA
Humic acid
- PDT
Photodynamic therapy
- ROS
Oxygen reactive species
- PS
Photosensitizers
- LMP
Low melting point
- SH
Sodium humate
- Ce6
Chlorin e6
- MnO2
Manganese oxide
Authors’ contributions
Nian Ma made substantial contributions to the conception, paper collecting, and analyzing of the work; and drafting the work; and final approval of the version to be published, Zhihui Yan made substantial contributions to conception of the work; and revising it critically for important intellectual content; and final approval of the version to be published; and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors read and approved the final manuscript.
Funding
This work was supported by Huai’an “Tianyixing” Key Laboratory of Medical Examination (HAP202004).
Availability of data and materials
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Li Y, Rodrigues J, Tomas H. Injectable and biodegradable hydrogels: gelation, biodegradation and biomedical applications. Chem Soc Rev. 2012;41:2193–2221. doi: 10.1039/C1CS15203C. [DOI] [PubMed] [Google Scholar]
- 2.Ren K, He C, Xiao C, Li G, Chen X. Injectable glycopolypeptide hydrogels as biomimetic scaffolds for cartilage tissue engineering. Biomaterials. 2015;51:238–249. doi: 10.1016/j.biomaterials.2015.02.026. [DOI] [PubMed] [Google Scholar]
- 3.Buwalda SJ, Boere KWM, Dijkstra PJ, Feijen J, Vermonden T, Hennink WE. Hydrogels in a historical perspective: From simple networks to smart materials. J Control Release. 2014;190:254–273. doi: 10.1016/j.jconrel.2014.03.052. [DOI] [PubMed] [Google Scholar]
- 4.Wang H, Chen Q, Zhou S. Carbon-based hybrid nanogels: a synergistic nanoplatform for combined biosensing, bioimaging, and responsive drug delivery. Chem Soc Rev. 2018;47(11):4198–4232. doi: 10.1039/C7CS00399D. [DOI] [PubMed] [Google Scholar]
- 5.Tao W, Ji X, Xu X, Islam MA, Li Z, Chen S, et al. Antimonene quantum dots: synthesis and application as nearinfrared photothermal agents for effective cancer therapy. Angew Chem Int Ed Engl. 2017;56(39):11896–11900. doi: 10.1002/anie.201703657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang Y, Sun S, Zhang Z, Shi D. Nanomaterials for cancer precision medicine. Adv Mater. 2018;30:1705660–1705681. doi: 10.1002/adma.201705660. [DOI] [PubMed] [Google Scholar]
- 7.Qiu M, Wang D, Liang W, Liu L, Zhang Y, Chen X, et al. Novel concept of the smart NIR-light–controlled drug release of black phosphorus nanostructure for cancer therapy. Proc Natl Acad Sci USA. 2018;115(3):501–506. doi: 10.1073/pnas.1714421115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wust P, Hildebrandt B, Sreenivasa G, Rau B, Gellermann J, Riess H. Hyperthermia in combined treatment of cancer. Lancet Oncol. 2002;3(8):487–497. doi: 10.1016/S1470-2045(02)00818-5. [DOI] [PubMed] [Google Scholar]
- 9.Qin L, Cao J, Shao K, Tong F, Yang Z, Lei T, et al. A tumor-to-lymph procedure navigated versatile gel system for combinatorial therapy against tumor recurrence and metastasis. Sci Adv. 2020;6:1–13. doi: 10.1126/sciadv.abb3116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gao Ge, Jiang Y-W, Jia H-R, Fu-Gen Wu. Near-infrared light-controllable on-demand antibiotics release using thermo-sensitive hydrogel-based drug reservoir for combating bacterial Infection. Biomaterials. 2019;188:83–95. doi: 10.1016/j.biomaterials.2018.09.045. [DOI] [PubMed] [Google Scholar]
- 11.Sautrot-Ba P, Razza N, Breloy L, Abbad Andaloussi S, Chiappone A, Sangermano M, et al. Photoinduced chitosan–PEG hydrogels with long-term antibacterial properties. J Mater Chem B. 2019;7:6526–6538. doi: 10.1039/C9TB01170F. [DOI] [PubMed] [Google Scholar]
- 12.Kumar CSSR, Mohammad F. Magnetic nanomaterials for hyperthermia-based therapy and controlled drug delivery. Adv Drug Deliv Rev. 2011;63:789–808. doi: 10.1016/j.addr.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jiating Xu, Kuang Ye, Lv R, Yang P, Li C, Bi H, et al. Charge convertibility and near infrared photon co-enhanced cisplatin chemotherapy based on upconversion nanoplatform. Biomaterials. 2017;130:42–55. doi: 10.1016/j.biomaterials.2017.03.041. [DOI] [PubMed] [Google Scholar]
- 14.Li Y, Lin T-Y, Luo Y, Liu Q, Xiao W, Guo W, et al. A smart and versatile theranostic nanomedicine platform based on nanoporphyrin. Nat Commun. 2014;5:4712–4727. doi: 10.1038/ncomms5712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martínez-Calvo M, Kotova O, Möbius ME, Bell AP, McCabe T, Boland JJ, Gunnlaugsson T. Healable luminescent self-assembly supramolecular metallogels possessing lanthanide (Eu/Tb) depended rheological and morphological properties. J Am Chem Soc. 2015;137(5):1983–1992. doi: 10.1021/ja511799n. [DOI] [PubMed] [Google Scholar]
- 16.Talebian S, Mehrali M, Taebnia N, Pennisi CP, Kadumudi FB, Foroughi J, et al. Self-healing hydrogels: the next paradigm shift in tissue engineering? Adv Sci. 2019;6(16):1801664–1801701. doi: 10.1002/advs.201801664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hervault A, Lim M, Boyer C, Dunn AE, Mott D, Maenosono S, Thanh NTK. Doxorubicin loaded dual pH- and thermo-responsive magnetic nanocarrier for combined magnetic hyperthermia and targeted controlled drug delivery applications. Nanoscale. 2016;8(24):12152–12161. doi: 10.1039/C5NR07773G. [DOI] [PubMed] [Google Scholar]
- 18.Gao F, Xie W, Miao Y, Wang D, Guo Z, Ghosal A, et al. Magnetic hydrogel with optimally adaptive functions for breast cancer recurrence prevention. Adv Healthcare Mater. 2019;8(14):1900203–1900217. doi: 10.1002/adhm.201900203. [DOI] [PubMed] [Google Scholar]
- 19.Häring M, Schiller J, Mayr J, Grijalvo S, Eritja R, Díaz DD. Magnetic gel composites for hyperthermia cancer therapy. Gels. 2015;1:135–161. doi: 10.3390/gels1020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wei Z, Xue F, Xin F, Ming Wu, Wang B, Zhang X, et al. A thieno-isoindigo derivative-based conjugated polymer nanoparticle for photothermal therapy at NIR-II bio-window. Nanoscale. 2020;12(38):19665–19672. doi: 10.1039/D0NR03771K. [DOI] [PubMed] [Google Scholar]
- 21.Shi B, Yan Q, Tang J, Xin K, Zhang J, Zhu Y, et al. Hydrogen sulfide-activatable second near-infrared fluorescent nanoassemblies for targeted photothermal cancer therapy. Nano Lett. 2018;18(10):6411–6416. doi: 10.1021/acs.nanolett.8b02767. [DOI] [PubMed] [Google Scholar]
- 22.Liu Y, Bhattarai P, Dai Z, Chen X. Photothermal therapy and photoacoustic imaging via nanotheranostics in fighting cancer. Chem Soc Rev. 2019;48(7):2053–2108. doi: 10.1039/C8CS00618K. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nam J, Son S, Ochyl LJ, Kuai R, Schwendeman A, Moon JJ. Chemo-photothermal therapy combination elicits anti-tumor immunity against advanced metastatic Cancer. Nat Commun. 2018;9(1):1074–1087. doi: 10.1038/s41467-018-03473-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lin H, Gao S, Dai C, Chen Y, Shi J. Correction to “A two-dimensional biodegradable niobium carbide (MXene) for photothermal tumor eradication in NIR-I and NIR-II biowindows. J Am Chem Soc. 2017;139(45):16235–16247. doi: 10.1021/jacs.7b07818. [DOI] [PubMed] [Google Scholar]
- 25.Bao X, Yuan Ye, Chen J, Zhang B, Li Di, Zhou D, et al. In vivo theranostics with near-infraredemitting carbon dots—highly efficient photothermal therapy based on passive targeting after intravenous administration. Light Sci Appl. 2018;7:91–102. doi: 10.1038/s41377-018-0090-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zou Q, Huang J, Zhang X. One-step synthesis of iodinated polypyrrole nanoparticles for CT imaging guided photothermal therapy of tumors. Small. 2018;14(45):1803101–1803112. doi: 10.1002/smll.201803101. [DOI] [PubMed] [Google Scholar]
- 27.Zhang H, Tian X-T, Shang Y, Li Y-H, Yin X-B. Theranostic Mn-porphyrin metal-organic frameworks for magnetic resonance imaging-guided nitric oxide and photothermal synergistic therapy. ACS Appl Mater Interfaces. 2018;10(34):28390–28398. doi: 10.1021/acsami.8b09680. [DOI] [PubMed] [Google Scholar]
- 28.Jiang Y, Qiongzheng Hu, Chen H, Zhang J, Chiu DT, McNeill J. Dual-mode superresolution imaging using charge transfer dynamics in semiconducting polymer dots. Angew Chem Int Ed Engl. 2020;59(37):16173–16180. doi: 10.1002/anie.202006348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wen G, Li X, Zhang Y, Han X, Xiayi Xu, Liu C, et al. Effective phototheranostics of brain tumor assisted by nearinfrared-II light-responsive semiconducting polymer nanoparticles. ACS Appl Mater Interfaces. 2020;12(30):33492–33499. doi: 10.1021/acsami.0c08562. [DOI] [PubMed] [Google Scholar]
- 30.Zhou W, Chen Y, Zhang Y, Xin X, Li R, Xie C, Fan Q. Iodine-rich semiconducting polymer nanoparticles for CT/fluorescence dual-modal imaging-guided enhanced photodynamic therapy. Small. 2020;16(5):1905641–1905650. doi: 10.1002/smll.201905641. [DOI] [PubMed] [Google Scholar]
- 31.Jiang Y, McNeill J. Light-harvesting and amplifified energy transfer in conjugated polymer nanoparticles. Chem Rev. 2017;117(2):838–859. doi: 10.1021/acs.chemrev.6b00419. [DOI] [PubMed] [Google Scholar]
- 32.Xiaoming Hu, Tang Y, Yuxuan Hu, Feng Lu, Xiaomei Lu, Wang Y, et al. Gadolinium-chelated conjugated polymer-based nanotheranostics for photoacoustic/magnetic resonance/NIR-II fluorescence imaging-guided cancer photothermal therapy. Theranostics. 2019;9(14):4168–4181. doi: 10.7150/thno.34390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li J, Kanyi Pu. Semiconducting polymer nanomaterials as near-infrared photoactivatable protherapeutics for cancer. Acc Chem Res. 2020;53(4):752–762. doi: 10.1021/acs.accounts.9b00569. [DOI] [PubMed] [Google Scholar]
- 34.Li J, Jiang R, Wang Qi, Li X, Xiaoming Hu, Yuan Y, et al. Semiconducting polymer nanotheranostics for NIR-II/photoacoustic imaging-guided photothermal initiated nitric oxide/photothermal therapy. Biomaterials. 2019;217:119304. doi: 10.1016/j.biomaterials.2019.119304. [DOI] [PubMed] [Google Scholar]
- 35.Xu H, Ohulchanskyy TY, Yakovliev A, Zinyuk R, Song J, Liu L, et al. Nanoliposomes co-encapsulating CT imaging contrast agent and photosensitizer for enhanced, imaging guided photodynamic therapy of cancer. Theranostics. 2019;9(5):1323–1335. doi: 10.7150/thno.31079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Men X, Chen H, Sun C, Liu Y, Wang R, Zhang X, et al. Thermosensitive polymer dot nanocomposites for trimodal computed tomography/photoacoustic/fluorescence imagingguided synergistic chemo-photothermal therapy. ACS Appl Mater Interfaces. 2020;12:51174–51184. doi: 10.1021/acsami.0c13252. [DOI] [PubMed] [Google Scholar]
- 37.Kubista B, Schoefl T, Mayr L, van Schoonhoven S, Heffeter P, Windhager R, et al. Distinct activity of the bone-targeted gallium compound KP46 against osteosarcoma cells-synergism with autophagy inhibition. Exp Clin Cancer Res. 2017;36(1):52–65. doi: 10.1186/s13046-017-0527-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu M, Zeng X, Ma C, Yi H, Ali Z, Mou X, et al. Injectable hydrogels for cartilage and bone tissue engineering. Bone Res. 2017;5:17014–17034. doi: 10.1038/boneres.2017.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bendtsen ST, Wei M. Synthesis and characterization of a novel injectable alginate–collagen–hydroxyapatite hydrogel for bone tissue regeneration. J Mater Chem B. 2015;3(15):3081–3090. doi: 10.1039/C5TB00072F. [DOI] [PubMed] [Google Scholar]
- 40.Luo S, Juan Wu, Jia Z, Tang P, Sheng J, et al. An injectable, bifunctional hydrogel with photothermal effects for tumor therapy and bone regeneration. Macromol Biosci. 2019;19(9):1900047–1900057. doi: 10.1002/mabi.201900047. [DOI] [PubMed] [Google Scholar]
- 41.Gizer M, Köse S, Karaosmanoglu B, Taskiran EZ, Berkkan A, Timuçin M, et al. The effect of boron-containing nano-hydroxyapatite on bone cells. Biol Trace Elem Res. 2020;193(2):364–376. doi: 10.1007/s12011-019-01710-w. [DOI] [PubMed] [Google Scholar]
- 42.Liu Y, Sui Y, Liu C, Liu C, Meiyan Wu, Li B, Li Y. A physically crosslinked polydopamine/nanocellulose hydrogel as potential versatile vehicles for drug delivery and wound healing. Carbohydr Polym. 2018;188:27–36. doi: 10.1016/j.carbpol.2018.01.093. [DOI] [PubMed] [Google Scholar]
- 43.Wang Z, Jia Z, Jiang Y, Pengfei Li Lu, Han XL, et al. Mussel-inspired nano-building block assemblies for mimicking extracellular matrix microenvironments with multiple functions. Biofabrication. 2017;9(3):035005. doi: 10.1088/1758-5090/aa7fdc. [DOI] [PubMed] [Google Scholar]
- 44.Li Y, Jiang C, Zhang D, Wang Y, Ren X, Ai K, et al. Targeted polydopamine nanoparticles enable photoacoustic imaging guided chemo-photothermal synergistic therapy of tumor. Acta Biomater. 2017;47:124–134. doi: 10.1016/j.actbio.2016.10.010. [DOI] [PubMed] [Google Scholar]
- 45.Gao X, Song J, Ji P, Zhang X, Li X, Xiao Xu, et al. Polydopamine-templated hydroxyapatite reinforced polycaprolactone composite nanofibers with enhanced cytocompatibility and osteogenesis for bone tissue engineering. ACS Appl Mater Interfaces. 2016;8(5):3499–3515. doi: 10.1021/acsami.5b12413. [DOI] [PubMed] [Google Scholar]
- 46.Thakor AS, Gambhir SS. Nanooncology: the future of cancer diagnosis and therapy. CA Cancer J Clin. 2013;63(6):395–418. doi: 10.3322/caac.21199. [DOI] [PubMed] [Google Scholar]
- 47.Yang R, Hou M, Gao Ya, Zhang L, Zhigang Xu, Kang Y, et al. Indocyanine green-modified hollow mesoporous prussian blue nanoparticles loading doxorubicin for fluorescence-guided tri-modal combination therapy of cancer. Nanoscale. 2019;11(12):5717–5731. doi: 10.1039/C8NR10430A. [DOI] [PubMed] [Google Scholar]
- 48.Wang X, Li F, Yan X, Ma Y, Miao Z, Dong L, et al. Ambient Aqueous synthesis of ultrasmall Ni0.85Se nanoparticles for non-invasive photoacoustic imaging and combined photothermal-chemo therapy of cancer. ACS Appl Mater Interfaces. 2017;9(48):41782–41793. doi: 10.1021/acsami.7b15780. [DOI] [PubMed] [Google Scholar]
- 49.Miao Z-H, Li K, Liu P-Y, Li Z, Yang H, Zhao Q, et al. Natural humic-acid-based phototheranostic agent. Adv Healthc Mater. 2018;7(7):1701202–1701211. doi: 10.1002/adhm.201701202. [DOI] [PubMed] [Google Scholar]
- 50.Yuan F, Li J-L, Cheng H, Zeng X, Zhang X-Z. A redox-responsive mesoporous silica based nanoplatform for in vitro tumor-specific fluorescence imaging and enhanced photodynamic therapy. Biomater Sci. 2017;6(1):96–100. doi: 10.1039/C7BM00793K. [DOI] [PubMed] [Google Scholar]
- 51.Deng J, Liu F, Wang L, An Y, Gao M, Wang Z, Zhao Y. Hypoxia- and singlet oxygen-responsive chemo-photodynamic Micelles featured with glutathione depletion and aldehyde production. Biomater Sci. 2018;7(1):429–441. doi: 10.1039/C8BM01042K. [DOI] [PubMed] [Google Scholar]
- 52.Oliva N, Conde J, Wang K, Artzi N. Designing Hydrogels For On-Demand Therapy. Acc Chem Res. 2017;50:669–679. doi: 10.1021/acs.accounts.6b00536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hou M, Liu W, Zhang L, Zhang L, Zhigang Xu, Cao Y, et al. Responsive agarose hydrogel incorporated with natural humic acid and MnO2 nanoparticles for effective relief of tumor hypoxia and enhanced photo-induced tumor therapy. Biomater Sci. 2020;8(1):353–369. doi: 10.1039/C9BM01472A. [DOI] [PubMed] [Google Scholar]
- 54.Xiang H, Lin H, Luodan Yu, Chen Yu. Hypoxia-irrelevant photonic thermodynamic cancer nanomedicine. ACS Nano. 2019;13(2):2223–2235. doi: 10.1021/acsnano.8b08910. [DOI] [PubMed] [Google Scholar]
- 55.Liang X, Ye X, Wang C, Xing C, Miao Q, Xie Z, et al. Photothermal cancer immunotherapy by erythrocyte membrane-coated black phosphorus formulation. J Control Release. 2019;296:150–161. doi: 10.1016/j.jconrel.2019.01.027. [DOI] [PubMed] [Google Scholar]
- 56.Márquez-Garbán DC, Deng G, Comin-Anduix B, Garcia AJ, Xing Y, Chen H-W, et al. Antiestrogens in combination with immune checkpoint inhibitors in breast cancer immunotherapy. J Steroid Biochem Mol Biol. 2019;193:105415. doi: 10.1016/j.jsbmb.2019.105415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Haoan Wu, Song L, Chen L, Huang Y, Yang Wu, Zang F, et al. Injectable thermosensitive magnetic nanoemulsion hydrogel for multimodal-imaging-guided accurate thermoablative cancer therapy. Nanoscale. 2017;9(42):16175–16182. doi: 10.1039/C7NR02858J. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.