Idiopathic normal pressure hydrocephalus (iNPH) is characterized clinically by degradation of gait, cognition, and urinary continence. INPH is progressive (Andrén et al, 2014), still probably underdiagnosed (Williams et al, 2019) but potentially treatable by CSF diversion (Kazui et al, 2015). Familial aggregation is a strong indicator of genetic regulation in the disease process iNPH (Fig 1). Enlargement of brain ventricles is associated with failed cerebrospinal (CSF) homeostasis by so far mostly unknown mechanisms. A mutation of the cilia gene CFAP43 in iNPH family, confirmed by a knocked‐out mouse model (Morimoto et al, 2019), allelic variation of NME8 (Huovinen et al, 2017), a segmental copy number loss in SFMBT1 in selected iNPH patients (Sato et al, 2016), and current results by Yang et al (2021) indicate that cilia dysfunction is one of the key mechanisms behind iNPH.
Subject Categories: Genetics, Gene Therapy & Genetic Disease; Neuroscience
T. Kuulasmaa, M. Hiltunen and V. Leinonen discuss novel genetic and functional findings related to two loss of function deletions in CWH43 gene in patients with Idiopathic normal pressure hydrocephalus by M. Johnson and colleagues, in this issue of EMBO Mol Med.

In this issue of EMBO Molecular Medicine, Yang et al (2021) report novel genetic and functional findings related to two loss of function deletions in CWH43 gene in patients with iNPH. This is one of the most important studies in the field of iNPH research so far, emphasizing the fact that eventually iNPH is not anymore considered as “idiopathic”. Furthermore, these results strongly support the existence of iNPH as an independent disease entity.
Figure 1.
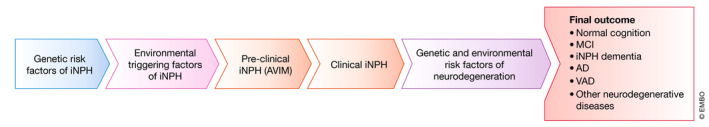
Hypothetical disease progress of iNPH
The discovery cohort used in the study of Yang et al is relatively small and thus, genetic studies in the larger patient cohorts are expected to identify new potential genetic loci related to iNPH. As with numerous other multifactorial diseases, international collaboration with large multicenter cohorts are needed to uncover the expected rare variants with large effect and more common variants with small effect.
Three out of the eight patients with CWH43 alteration had potential iNPH‐related family history, indicating that this variant can either be de novo mutation or that the familiar inheritance is underestimated due to the late onset of the clinical symptoms. Diagnostic criteria of iNPH need to be updated to include also prodromal iNPH, such as asymptomatic ventriculomegaly with features of iNPH on magnetic resonance imaging (AVIM, Kimihira et al, 2020). Identification of genetic variants similar to that now observed with CWH43 will open a window to decipher the underlying pathophysiological mechanisms further, paving the way to better treatments and novel prevention strategies in the future.
EMBO Mol Med (2021) 13: e13720.
See also: HW Yang et al (March 2021)
References
- Andrén K, Wikkelsø C, Tisell M, Hellström P (2014) Natural course of idiopathic normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry 85: 806–810 [DOI] [PubMed] [Google Scholar]
- Huovinen J, Helisalmi S, Paananen J, Laiterä T, Kojoukhova M, Sutela A, Vanninen R, Laitinen M, Rauramaa T, Koivisto AM et al (2017) Alzheimer's disease‐related polymorphisms in shunt‐responsive idiopathic normal pressure hydrocephalus. J Alzheimers Dis 60: 1077–1085 [DOI] [PubMed] [Google Scholar]
- Kazui H, Miyajima M, Mori E, Ishikawa M, SINPHONI‐2 Investigators (2015) Lumboperitoneal shunt surgery for idiopathic normal pressure hydrocephalus (SINPHONI‐2): an open‐label randomised trial. Lancet Neurol 14: 585–594 [DOI] [PubMed] [Google Scholar]
- Kimihira L, Iseki C, Takahashi Y, Sato H, Kato H, Kazui H, Kuriyama N, Nakajima M, Miyajima M, Endo K et al (2020) A multi‐center, prospective study on the progression rate of asymptomatic ventriculomegaly with features of idiopathic normal pressure hydrocephalus on magnetic resonance imaging to idiopathic normal pressure hydrocephalus. J Neurol Sci 419: 117166 [DOI] [PubMed] [Google Scholar]
- Morimoto Y, Yoshida S, Kinoshita A, Satoh C, Mishima H, Yamaguchi N, Matsuda K, Sakaguchi M, Tanaka T, Komohara Y et al (2019) Nonsense mutation in CFAP43 causes normal‐pressure hydrocephalus with ciliary abnormalities. Neurology 92: e2364–e2374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato H, Takahashi Y, Kimihira L, Iseki C, Kato H, Suzuki Y, Igari R, Sato H, Koyama S, Arawaka S et al (2016) A segmental copy number loss of the SFMBT1 gene is a genetic risk for shunt‐responsive, idiopathic normal pressure hydrocephalus (iNPH): a case‐control study. PLoS One 11: e0166615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams MA, Nagel SJ, Luciano MG, Relkin N, Zwimpfer TJ, Katzen H, Holubkov R, Moghekar A, Wisoff JH, McKhann GM et al (2019) The clinical spectrum of hydrocephalus in adults: report of the first 517 patients of the Adult Hydrocephalus Clinical Research Network registry. J Neurosurg 24: 1–12 [DOI] [PubMed] [Google Scholar]
- Yang HW, Lee S, Yang D, Dai H, Zhang Y, Han L, Zhao S, Zhang S, Ma Y, Johnson MF et al (2021) Deletions in CWH43 cause idiopathic normal pressure hydrocephalus. EMBO Mol Med 13: e13249 [DOI] [PMC free article] [PubMed] [Google Scholar]


