Abstract
Horizontal gene transfer facilitates the spread of antibiotic resistance genes, which constitutes a global challenge. However, the evolutionary trajectory of the mobile colistin resistome in bacteria is largely unknown. To investigate the coevolution and fitness cost of the colistin resistance genes in wild strains, different assays to uncover the genomic dynamics of mcr‐1 and mcr‐3 in bacterial populations are utilized. Escherichia coli strains harboring both mcr‐1 and mcr‐3.1/3.5 are isolated and mcr genes are associated with diverse mobile elements. Under exposure to colistin, the mcr‐1‐bearing resistome is stably inherited during bacterial replication, but mcr‐3 is prone to be eliminated in populations of certain strains. In the absence of colistin, the persistence rates of the mcr‐1 and mcr‐3‐bearing subclones varies depending on the genomic background. The decay of the mcr‐bearing bacterial populations can be mediated by the elimination of mcr‐containing segments, large genomic deletions, and plasmid loss. Mobile elements, including plasmids and transposons, are double‐edged swords in the evolution of the resistome. The findings support the idea that antibiotic overuse accounts for global spread of multidrug‐resistant (MDR) bacteria. Therefore, stringent regulation of antibiotic prescription for humans and animals should be performed systematically to alleviate the threat of MDR bacteria.
Keywords: coevolution, colistin resistance, mcr genes, plasmids
The evolutionary trajectory of mobile colistin resistance genes and the underlying genomic basis in bacteria are largely unknown after withdrawal of colistin from animal feed additives. This study comprehensively deciphers the genomic landscape after the elimination of mcr genes during bacterial growth under different conditions, highlighting the pivotal role of mobile elements in mediating resistance gene transmission.

1. Introduction
The emergence and persistence of novel antimicrobial resistance genes pose great concern for public health worldwide.[ 1 , 2 ] The misuse and abuse of antimicrobials play an important role in the emergence, transmission, and persistence of resistance genes among pathogens, although some resistance genes already existed in the pre‐antibiotic era.[ 3 ] There are still contrasting opinions concerning the role of clinical antibiotics in the evolution of antibiotic resistance genes, all of which are supported by different facts.[ 4 , 5 , 6 ] The actual correlation between these two factors may depend on the specific resistance mechanisms under investigation, and both ancient origin and post‐antibiotic evolution in different environments may account for the current severe problem of antibiotic resistance in human pathogens. Horizontal gene transfer conferred by plasmids or other mobile elements plays a key role in the transmission of antibiotic resistance among different pathogens.[ 7 ] Furthermore, the persistence of resistance genes is critical for bacteria to constitute a real ongoing threat. The fitness cost endowed by the acquired resistance genes or plasmids can determine differences in the persistence of resistance genes among bacteria.[ 8 , 9 ] However, the role of mobile elements and antibiotics in the persistence and evolution of multiple acquired resistance genes, such as different mcr genes, in the same bacterial population has not been extensively investigated.
The emergence of novel plasmid‐associated mcr genes (mcr‐1 to mcr‐10) conferring resistance to colistin, a last‐resort antibiotic used to treat severe bacterial infections caused by different pathogens, has evoked great concern for the coming post‐antibiotic era.[ 10 , 11 , 12 ] Co‐occurrence of identical or different mcr genes in the same strain was reported.[ 13 , 14 , 15 , 16 ] The archetypical mcr‐1‐bearing composite transposon Tn6330 was found to be unstable and could lose the mcr‐1 gene during bacterial replication.[ 17 , 18 ] However, the evolutionary trajectory of different mcr genes of the same strain during bacterial growth was not investigated systematically. Recently, one report found that plasmids carrying mcr‐3 were more stable than mcr‐1‐bearing plasmids, but the underlying genetic mechanisms were unknown.[ 19 ] In this study, we comprehensively characterized the genomic basis underlying resistance gene evolution in different Escherichia coli (E. coli) strains harboring mcr‐1 and mcr‐3 genes. Our findings indicate that the fitness cost of resistance genes and the corresponding plasmids are vital factors affecting the persistence of resistance genes in the bacterial population.
2. Results
2.1. Characterization of mcr‐Bearing E. coli Isolates
After bacterial isolation and identification, five E. coli strains were found to be positive for both mcr‐1 and mcr‐3 and resistant to colistin with minimum inhibitory concentrations ranging from 4 to 8 mg L−1. All of them were MDR strains resistant to multiple antimicrobials, including colistin, tetracycline, gentamycin, ampicillin, and chloramphenicol (Table S1, Supporting Information). Conjugation assay was successful for two (CP8‐3 and CP55) out of five strains. For CP8‐3, only the mcr‐1‐bearing transconjugant (CP8‐3‐T) was recovered. On the other hand, for CP55 two different transconjugants were obtained (CP55‐T1 harboring mcr‐1 and CP55‐T2 harboring both mcr‐1 and mcr‐3), indicating that co‐transfer of mcr‐1 and mcr‐3 occurred in CP55. The five mcr‐bearing strains belonged to different clones with different pulsed‐field gel electrophoresis (PFGE) profiles, implying that these strains descended from various separate ancestors. S1 nuclease digestion PFGE (S1‐PFGE) showed that plasmid profiles differed among strains, ranging from two to four plasmids with different sizes (Figures S1 and S2, Supporting Information). Notably, the plasmid harboring mcr‐3.19 and mcr‐1 was previously characterized in an isolate CP53 from the same slaughterhouse.[ 20 ]
2.2. Genomic Characterization of E. coli Strains Positive for mcr‐1 and mcr‐3
To assess the genomic features of strains harboring both mcr‐1 and mcr‐3, complete genome sequences were successfully obtained using a hybrid de novo assembly strategy. The distribution of resistance genes and basic information on the bacterial genomes are reported in Table 1 and Table S2, Supporting Information.
Table 1.
Genomic features of the five E. coli strains positive for the mcr‐1 and mcr‐3 genes
| Strain | Contigs a) | ST | Serotype | Resistance genes | Genetic context of mcr genes | Virulence genes | Size (bp) | Plasmid types |
|---|---|---|---|---|---|---|---|---|
| CP8‐3 | CP8‐3‐chromosome | ST34 | – | mcr‐1.1, mdf(A) | ISApl1‐mcr‐1‐Dpap2‐IS1294‐ISApl1; ISKpn19‐TnAs2‐mcr‐3.5‐dgkA‐IS15 | astA, gad | 4.7m | chromosome |
| pCP8‐3‐IncFII | aadA1, aac(3)‐VIa, qnrS1, floR, tet(M) | 87k | IncFII | |||||
| pCP8‐3‐IncFIB | aadA1, aadA2, mef(B), cmlA1, sul3, tet(A), dfrA12 | 75k | IncFIA(HI1), IncFIB(K), IncN | |||||
| pCP8‐3‐IncR | bla TEM‐1B, mcr‐3.5, qnrS1, tet(M) | 47k | IncR | |||||
| pCP8‐3‐IncX1 | – | 38k | IncX1 | |||||
| pCP8‐3‐IncQ | sul2 | 8k | IncQ1 | |||||
| CP55 | CP55‐chromosome | ST971 | O128:H27 | aac(3)‐IId, qnrS1, mdf(A), floR, catA1 | mcr‐1‐pap2; IS4321R‐TnAs2‐mcr‐3.5‐dgkA‐IS15 | capU, cma, gad, iha, ireA, iroN, iss, lpfA, mchF, subA | 4.9m | chromosome |
| pCP55‐IncFIB | aph(3″)‐Ib, aph(6)‐Id, bla TEM‐1B, sul2, tet(A) | 156k | IncFIB, IncFII | |||||
| pCP55‐141k | – | 141k | IncB/O/K/Z | |||||
| pCP55‐IncFII | mcr‐3.5, mph(A) | 70k | IncFII | |||||
| pCP55‐IncX4 | mcr‐1.1 | 33k | IncX4 | |||||
| CP61 | CP61‐chromosome | – | – | mcr‐1.1, mdf(A) | Tn6330; TnAs2‐mcr‐3.1‐dgkA‐ISKpn40 | gad | 4.5m | chromosome |
| pCP61‐IncN | aph(3′)‐Ia, qnrS2, tet(A) | 80k | ColE10, IncFIA(HI1), IncN,IncR | |||||
| pCP61‐IncFIB | aadA2, aadA1, aac(3)‐VIa, bla TEM‐1B, mcr‐3.1, mef(B), cmlA1, floR, sul3, tet(M), dfrA12 | 92k | IncFIB(K), IncN | |||||
| CP66‐6 | CP66‐6‐chromosome | ST5229 | – | mcr‐1.1, mdf(A) | ISApl1‐mcr‐1‐Dpap2‐IS1294‐ISApl1; bla TEM‐1B‐TnAs2‐mcr‐3.5‐dgkA‐IS26(IS15DI) | astA, gad, lpfA | 4.8m | chromosome |
| pCP66‐6‐IncFIC | aadA2, aph(3′)‐Ia, aadA17, aac(3)‐IId, aadA1, blaTEM‐215, lnu(F), cmlA1, floR, sul2, sul3, tet(A), tet(M), dfrA12 | 99k | IncFIB(AP001918), IncFIC(FII) | |||||
| pCP66‐6‐IncFII | bla TEM‐215, mcr‐3.5, fosA4, mph(A), dfrA12 | 74k | ColE10, IncFII | |||||
| pCP66‐6‐IncX3 | bla OXA‐181, qnrS1 | 50k | ColKP3, IncX3 | |||||
| pCP66‐6‐IncQ | sul2 | 8k | IncQ1 | |||||
| CP131 | CP131‐chromosome | ST48 | – | mcr‐1.1, mdf(A) | Tn6330 (ISApl1‐mcr‐1‐pap2‐ISApl1); TnAs2‐mcr‐3.1‐dgkA‐ISKpn40 | gad, lpfA | 4.5m | chromosome |
| pCP131‐IncHI1 | aph(3″)‐Ib, aac(3)‐IId, bla TEM‐1B, mcr‐3.1, qnrS1, mef(B), floR, sul3, tet(M) | 264k | IncFIA(HI1), IncHI1A, IncHI1B(R27) | |||||
| pCP131‐IncFIB | aadA2, bla TEM‐1B, tet(A), mph(A), floR, sul3, tet(M), dfrA12 | 116k | IncFIB(AP001918), IncFIC(FII) |
All contigs were circular plasmids and chromosomes. Plasmids smaller than 10 kb without resistance genes are not listed here. For the complete sequencing data, refer to the figshare database (https://doi.org/10.6084/m9.figshare.11825871). The dash symbols denote unidentified ST, serotypes, and resistance genes.
The genome of CP8‐3 consisted of one chromosome with the sequence type 34 (ST34) and four plasmids, namely pCP8‐3‐IncFII (87,125 bp), pCP8‐3‐IncFIB (75,733 bp), pCP8‐3‐IncR (47,220 bp), and pCP8‐3‐IncX1 (38,002 bp). The mcr‐1 gene was located on the chromosome within the genetic structure ISApl1‐mcr‐1‐∆pap2‐IS1294‐ISApl1 (Figure 1a). However, the mcr‐3.5 gene was located on the pCP8‐3‐IncR plasmid within the genetic structure ISKpn19‐TnAs2‐mcr‐3.5‐dgkA‐IS15, together with the resistance genes qnrS1, tet(M), and bla TEM‐1B. This mcr‐3.5‐bearing plasmid was similar to another mcr‐3‐bearing plasmid, pHN8 (MG780294), with 99% identity at 83% coverage. The most variable regions between these two plasmids were the MDR regions, showing great diversity mediated by mobile elements (Figure S3, Supporting Information). In addition, pCP8‐3‐IncFII was a typical MDR plasmid including aadA1, aac(3)‐VIa, floR, tet(M), and qnrS1, and most similar to pCC1410‐1 (KT725788) with 99% identity at 76% coverage. Moreover, pCP8‐3‐IncFIB was a multireplicon MDR plasmid harboring IncFIB and IncN replicons and including mef(B), sul3, cmlA1, aadA1, dfrA12, and tet(A), and was most similar to pSCE516‐4 (KX023259) with 99% identity at 96% coverage. Finally, pCP8‐3‐IncX1 did not harbor resistance genes, but another plasmid pCP8‐3‐IncQ (8,176 bp) harbored sul2 and czcD, which encoded a heavy metal ion transporter.
Figure 1.
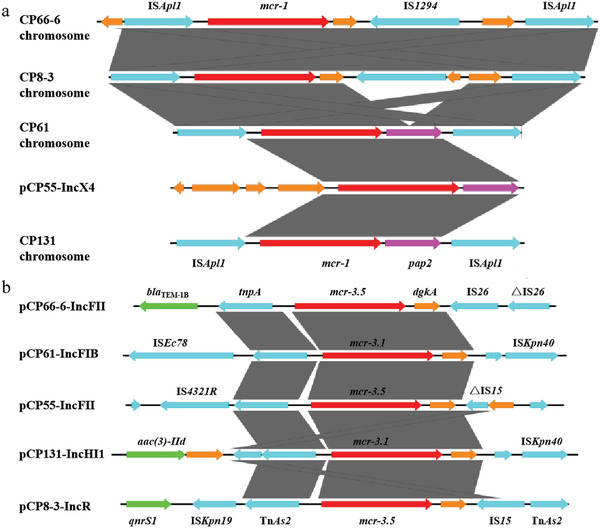
a) Alignment of mcr‐1‐bearing DNA segments from the five E. coli strains. Red arrows denote the mcr‐1 gene, while blue arrows represent insertion sequences; yellow and purple arrows are standard for other coding sequences. b) Alignment of mcr‐3‐bearing structures of various plasmids. Red arrows denote mcr‐3 genes, while blue arrows indicate insertion sequences; yellow arrows represent other coding sequences, and green arrows stand for other resistance genes.
The strain CP55 belonged to the ST971 family and carried one chromosome and four plasmids. The gene mcr‐1 was located on the IncX4‐type plasmid pCP55‐IncX4 (33,309 bp) within the genetic context mcr‐1‐pap2, without ISApl1 flanking mcr‐1 (Figure 1a). The gene mcr‐3.5 was located on the IncFII‐type plasmid pCP55‐IncFII (70,770 bp) within the genetic context IS4321R‐TnAs2‐mcr‐3.5‐dgkA‐IS15 (Figure 1b). Another plasmid, pCP55‐IncFIB (156,025 bp), contained multiple resistance genes, including tet(A), sul2, strAB, and bla TEM‐1B, and was most similar to pH2332‐166 (KJ484626) with 99% identity at 78% coverage.
Furthermore, the strain CP61 harbored one chromosome (untypable ST) and two plasmids, pCP61‐IncFIB (92,073 bp) and pCP61‐IncN (80,920 bp). The gene mcr‐1 was located on the chromosome in the form of Tn6330 (ISApl1‐mcr‐1‐pap2‐ISApl1). However, mcr‐3.1 was detected in pCP61‐IncFIB in the structure TnAs2‐mcr‐3.1‐dgkA‐ISKpn40, together with cmlA1, aadA1, mef(B), sul3, bla TEM‐1B, aac(3)‐VIa, floR, and tet(M). The backbone of pCP61‐IncFIB was similar to that of pSCE516‐4 (KX023259) and other reported plasmids (Figure S4, Supporting Information). Finally, the plasmid pCP61‐IncN, carrying multiple replicons, including IncN, IncFIA, IncX1, and IncR, harbored the genes tet(A), aph(3)‐Ia, and qnrS2.
Whole Genome Sequencing (WGS) results showed that in the CP66‐6 strain there was one chromosome (ST5229), harboring ISApl1‐mcr‐1‐∆pap2‐IS1294‐ISApl1, and four plasmids, namely pCP66‐6‐IncFIC (99,734 bp), pCP66‐6‐IncFII (74,817 bp), pCP66‐6‐IncX3 (50,481 bp), and pCP66‐6‐IncQ (8,197bp), invisible by S1‐PFGE. pCP66‐6‐IncFIC harbored IncFIC and IncFIB replicons and included the genes tet(M), aadA1, cmlA1, aadA1, dfrA12, floR, sul2, tet(A), aph(3′)‐Ia, sul3, bla TEM‐1B, lnu(F), aadA1, and aac(3)‐IId. In addition, pCP66‐6‐IncFII harbored mcr‐3.5 in the core structure bla TEM‐1B‐TnAs2‐mcr‐3.5‐dgkA‐IS26(IS15DI), together with mph(A), dfrA12, and fosA. This mcr‐3‐bearing plasmid was most similar to pCHL5009T‐102k‐mcr3 (CP032937), with 99% identity at 74% coverage (Figure S5, Supporting Information). The third plasmid, pCP66‐6‐IncX3, harbored bla OXA‐181, qnrS1, and was nearly identical to pM206‐OXA181(AP018831) at 100% coverage. Finally, pCP66‐6‐IncQ was nearly identical to pCP8‐3‐IncQ, with only a few SNPs.
The CP131 strain consisted of one chromosome (ST48) and two MDR plasmids, namely pCP131‐IncHI1 (264,177 bp) and pCP131‐IncFIB (121,655 bp). The mcr‐1 gene was located on the chromosome in the form of Tn6330. The mcr‐3.1 gene was found in pCP131‐IncHI1 in the structure TnAs2‐mcr‐3.1‐dgkA‐ISKpn40 (Figure 1), together with other resistance genes, including floR, aac(3)‐IId, strAB, mef(B), sul3, qnrS1, and bla TEM‐1B. Finally, pCP131‐IncFIB harbored tet(A), mph(A), floR, bla TEM‐1B, and tet(M).
2.3. Comparison of mcr‐Bearing Mobile Elements and Detection of Circular Intermediates
Across the five strains, mcr‐1 was found on the chromosomes of CP8‐3, CP61, CP66‐6, and CP131 and on a plasmid of CP55 (Table S3, Supporting Information). An intact Tn6330 structure was found in the chromosomes of CP61 and CP131, while a Tn6330 truncated by the insertion of IS1294 (ISApl1‐mcr‐1‐∆pap2‐IS1294‐ISApl1) was observed in both CP8‐3 and CP66‐6. However, the insertion sites of mcr‐1 on the chromosomes varied, consistent with previous reports.[ 21 ] In contrast, in CP55 the mcr‐1 gene was located on the IncX4‐type plasmid pCP55‐33k, which has a structure similar to that of other reported mcr‐1‐bearing IncX4 plasmids.
On the other hand, in the five strains, mcr‐3.1 or mcr‐3.5 was located on plasmids harboring IncFII, IncR, IncHI1, or IncFIB replicons, with sizes ranging from 47 to 264 kb. Although the plasmids and surrounding sequences were diverse, the core mcr‐3‐containing structure TnAs2‐mcr‐3‐dgkA, flanked by mobile elements or resistance genes, was conserved (Figure 1b). The mcr‐3.1‐bearing plasmid pCP131‐IncHI1 was an MDR IncHI1/IncFIA‐type plasmid containing multiple resistance genes (Figure 2 ). To the best of our knowledge, this is the largest mcr‐3.1‐bearing plasmid ever reported.
Figure 2.
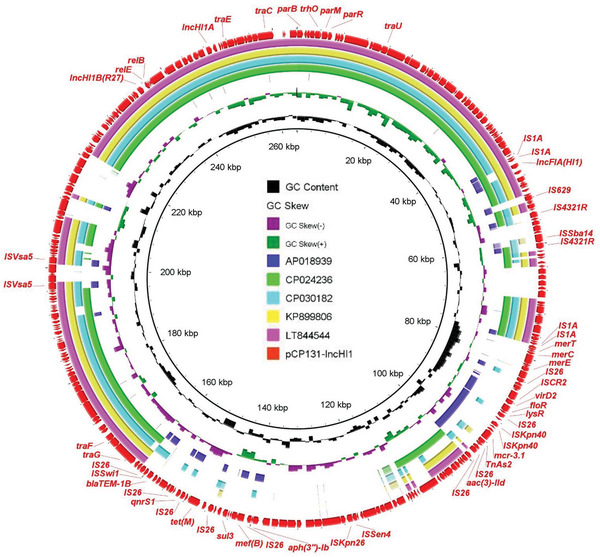
Alignment of the novel mcr‐3.1‐bearing plasmid pCP131‐IncHI1 with other similar plasmids. The outermost circle with arrows denotes the reference plasmid pCP131‐IncHI1.
To investigate the transmission of mcr genes, reverse PCR was used to detect potential circular intermediates according to published methods.[ 22 ] Samples positive for Tn6330 or its variant (ISApl1‐mcr‐1‐∆pap2‐IS1294‐ISApl1) were identified with the detection of two types of PCR products (2.5 and 4 kb, respectively). Sanger sequencing confirmed the existence of two types of circular forms, ISApl1‐mcr‐1‐pap2 and ISApl1‐mcr‐1‐∆pap2‐IS1294. In addition, two types of circular intermediates of mcr‐3.1, producing PCR products of 2 kb (CP66‐6) and 4.5 kb (CP131), were identified and sequencing analysis demonstrated that the two complete circular structures were ∆IS26‐TnAs2‐mcr‐3.5‐dgkA and ∆IS26‐∆TnAs2‐mcr‐3.1‐dgkA‐ISKpn40‐ble. These results imply that ISApl1 and IS26 play pivotal roles in the formation of circular intermediates of mcr‐1 and mcr‐3, respectively. It has been reported that mcr‐1‐bearing circular intermediates may be derived from an excision mechanism.[ 23 , 24 ] In contrast, mcr‐3 circular intermediates may be formed and translocated to other loci by a copy‐and‐paste mechanism, since with PCR primers targeting flanking sequences of the core mcr‐3‐bearing region we did not detect an excised region (data not shown).
2.4. Coevolution of mcr Genes and Underlying Genomic Dynamics
To investigate the coevolution of mcr‐1 and mcr‐3 genes in the same E. coli strain, we performed a stability assay of mcr genes in the five strains, as well as in the previously reported CP53 strain.[ 13 , 18 ] Under colistin pressure, the mcr‐1 gene was stable in all five strains and no mcr‐1‐negative subclones were detected during serial culture steps except for strain CP131, in which twelve subclones at the culture day 28 were found to be negative for mcr‐1 but still positive for mcr‐3 (Table S4, Supporting Information). After serial passages in medium with colistin, loss of mcr‐3 genes was detected in CP61 and CP66‐6, among which CP66‐6 lost mcr‐3 most easily, with 100% mcr‐3‐negative bacterial clones at passage 28 (Table S4, Supporting Information). No clone was observed to have lost both mcr‐1 and mcr‐3 under colistin pressure. However, loss of mcr‐1 and/or mcr‐3 in absence of colistin was common. Indeed, mcr‐1 was consistently stable only in CP55 along serial passages over 14 days. On the other hand, CP66‐6 and CP61 easily lost mcr‐1 and/or mcr‐3 after a number of passages. Intriguingly, all the mcr‐1‐negative clones of CP66‐6 were also negative for mcr‐3. To further investigate the genetic background and molecular mechanisms leading to loss of mcr‐1 and/or mcr‐3, we performed S1‐PFGE of subclones and obtained complete sequences of mcr‐bearing plasmids or chromosomes.
In CP66‐6, the extinction of mcr‐3 was caused by the loss of the mcr‐3‐bearing plasmid pCP66‐6‐IncFII, according to the S1‐PFGE profile (Figure 3a). However, it was impossible to assess the cause of the loss of chromosomal mcr‐1 by S1‐PFGE. To address the knowledge gap, the subclone CP66‐6‐C0_7‐3 was selected for WGS by MinION long‐read sequencing. Three circular contigs, including one chromosome and two plasmids (pCP66‐6‐IncFIC and pCP66‐6‐IncX3), were assembled. No mcr‐3‐bearing plasmid was identified, consistent with the S1‐PFGE results (Figure 3a). Detailed analysis of the mcr‐1‐bearing chromosomal segment indicated that an 18‐kb region including ISApl1‐mcr‐1‐pap2 was deleted in the chromosome of CP66‐6‐C0_7‐3 (Figure 3b). IS1294 may be involved in the deletion of this region. However, further research is required to reveal the underlying molecular mechanism. In conclusion, we propose that mcr‐1‐negative CP66‐6 subclones are derived from the deletion of chromosomal mcr‐1 during bacterial replication.
Figure 3.
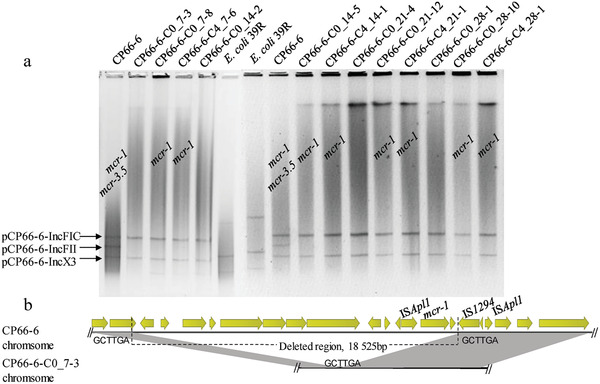
a) Results of S1‐PFGE for CP66‐6 and its subclones after serial passages in colistin and colistin‐free medium. The lanes of mcr‐positive clones are labeled. C0 denotes clones grown in medium without colistin, while C4 is used for clones grown with 2 mg L−1 colistin. The numbers 7, 14, 21, and 28 indicate the passage number (one passage per day) at which the clone is isolated. The last number indicates the clone number in the plates screened for mcr genes. b) Sequence alignment between the mcr‐1‐bearing chromosomal region of CP66‐6 and the corresponding chromosomic region of the subclone CP66‐6‐C0_7‐3.
Regarding the subclones of CP8‐3, the extinction of mcr‐3.5 in CP8‐3‐C0_1‐7 resulted from the loss of the mcr‐3.5‐bearing plasmid pCP8‐3‐IncR, as shown by S1‐PFGE and confirmed by MinION sequencing (Figure S4a, Supporting Information). In both CP8‐3‐C0_21‐5 and CP8‐3‐C0_28‐1, whose parent strain CP8‐3 displayed the same core mcr‐1‐bearing structure ISApl1‐mcr‐1‐∆pap2‐IS1294‐ISApl1 as CP66‐6, the loss of chromosomal mcr‐1 was due to the deletion of a long chromosomal region extending beyond the ISApl1 boundaries, similar to that observed in CP66‐6‐C0_7‐3. This was partially confirmed by the absence of PCR products when targeting the proximal genes of the core mcr‐1‐bearing structure.
No subclones losing mcr‐1 were found for the CP55 strain. However, mcr‐3.5 extinction in CP55 subclones may have resulted from the loss of the mcr‐3.5‐bearing segment of the pCP55‐IncFII plasmid, since the mcr‐3.5‐negative subclone CP55‐C0_28‐4 pCP55‐IncFII became smaller (Figure 4b). To confirm this hypothesis, the complete plasmids of CP55‐C0_28‐4 were sequenced by MinION sequencing. The comparison between the plasmids pCP55‐IncFII and pCP55‐C0_28‐4‐IncFII showed that an 8‐kb region including IS4321R‐TnAs2‐mcr‐3.5‐dgkA‐IS15‐mph(A) was deleted in pCP55‐C0_28‐4‐IncFII (Figure 4c). We speculate that the loss of the mcr‐3.5‐bearing region of pCP55‐IncFII may have also generated the other four mcr‐3.5‐negative subclones of CP55.
Figure 4.
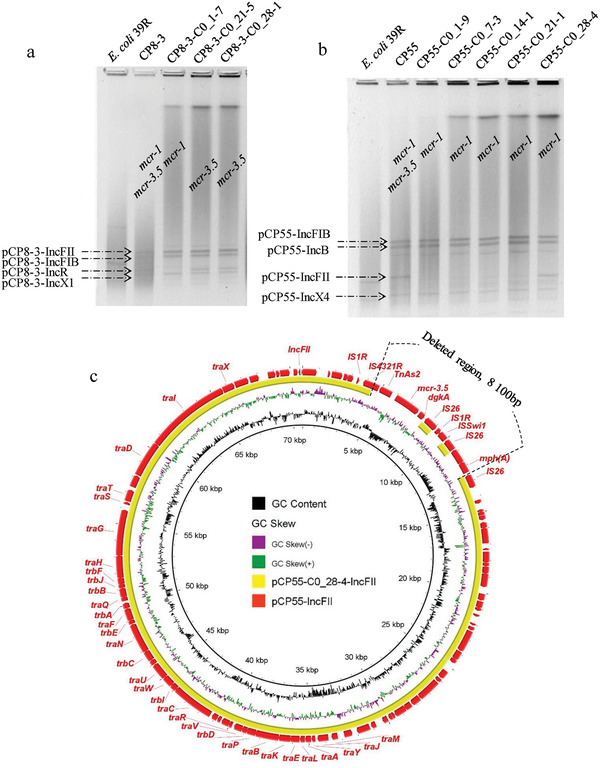
a,b) Results of S1‐PFGE of CP8‐3, CP55, and their respective subclones after serial passages in colistin and colistin‐free medium. c) Circular sequence alignment between the original mcr‐3.5‐bearing pCP55‐IncFII plasmid and its derivatives displaying loss of mcr‐3.5. The outermost circle represents the reference plasmid pCP55‐IncFII.
Furthermore, the loss of the mcr‐3.5‐bearing plasmid pCP61‐IncFIB accounted for the loss of mcr‐3.5 in CP61 subclones (Figure 5a). In addition, according to Nanopore long‐read data, chromosomal mcr‐1 loss in CP61 subclones was due to the loss of ISApl1‐mcr‐1‐pap2, resulting in one residual ISApl1 sequence (Figure 5b). This represents the typical decay process of Tn6330.[ 17 ] As for CP131, two subclones negative for mcr‐1 or mcr‐3.5 were analyzed by S1‐PFGE (Figure 6a). Notably, the extinction of mcr‐3.5 in CP131‐C0_28‐11 was due to the deletion of a large region in the pCP131‐IncHI1 plasmid mediated by IS15 (IS26‐like), as confirmed by the comparison between whole plasmid sequences (Figure 6b). In the CP131‐C0_21‐1 subclone, deletion of chromosomal mcr‐1‐pap2, leaving two residual ISApl1 sequences in the chromosome, accounted for the loss of mcr‐1 (Figure 6c). This was inconsistent with our results related to CP61 subclones and our previous report,[ 17 ] which found that Tn6330 decay would result in one residual ISApl1 sequence. The reason underlying this difference requires further research.
Figure 5.

a) Results of S1‐PFGE of CP61 and its subclones after serial passages in colistin and colistin‐free medium. b) Linear alignment between the mcr‐1‐bearing chromosomic region of CP61 and its truncated version from the subclone CP61‐C0_14‐10.
Figure 6.
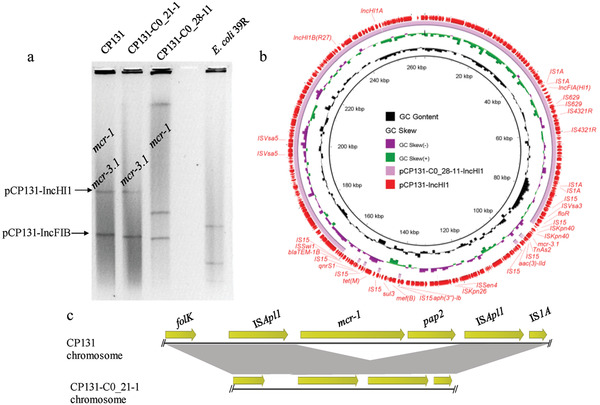
a) Results of S1‐PFGE of CP131 and its subclones after serial passages in colistin and colistin‐free medium. b) Comparison of pCP131‐IncHI1 and the respective plasmid from the subclone CP131‐C0_28‐11, without mcr‐3.1. c) Comparison of the mcr‐1‐bearing chromosome of CP131 and its evolved version from the subclone CP131‐C0_21‐1.
3. Discussion
The emergence of the mobile colistin resistance gene mcr was traced back to the 1980s,[ 25 ] indicating that the spread of mcr‐1 and its alleles among different pathogens is a long‐lasting evolutionary event. Mobile elements, antibiotic pressure, fitness cost, and compensatory mutations are pivotal factors for mcr gene transfer and persistence in the microbiome from different habitats, including animals, humans, and the environment. The expression of mcr‐1 could confer a biological fitness cost in different bacterial species, including E. coli and Klebsiella pneumoniae.[ 8 , 26 , 27 ] However, the fitness cost of other mcr genes has not been investigated.[ 19 ] Recently, co‐occurrence of different mcr genes was reported in single strains of E. coli.[ 13 , 14 , 19 , 28 ] Nevertheless, the possible coevolution of mcr‐1 and mcr‐3.1/3.5 has not been previously investigated.
In this study, we found five E. coli strains of different STs to be positive for mcr‐1 and mcr‐3.1/3.5. Three strains harbored mcr‐1 and mcr‐3.5, while two harbored mcr‐1 and mcr‐3.1. The co‐occurrence of mcr‐1 and mcr‐3.5 was consistent with previous reports.[ 19 , 29 ] The mcr‐1 gene could be found in both plasmids and chromosomes.[ 21 , 23 , 30 ] However, various mcr‐3 genes were only found in different Inc‐type plasmids in bacteria, except in Aeromonas species, which are potential reservoirs of mcr‐3 genes.[ 31 , 32 , 33 ] This phenomenon possibly explains the lower occurrence of mcr‐3 than mcr‐1 in field strains isolated from different sources.[ 29 ] Indeed, unlike the typical mcr‐1‐bearing Tn6330,[ 21 ] the core genetic context of mcr‐3 may also limit its transfer ability to the chromosomes of Enterobacteriaceae. The expression of mcr‐3 was reported to be less costly than that of mcr‐1 in the laboratory E. coli strain TOP10, with mcr‐3‐bearing plasmids outnumbering mcr‐1‐bearing plasmids in bacterial populations of this strain.[ 19 ] Although some strains in this study followed this paradigm, exceptional strains such as CP66‐6 showed the opposite trend, implying that the fitness cost of different mcr genes could depend on the bacterial genomic background rather than on the genes themselves. Furthermore, a previous study also demonstrated that the ratio of mcr‐3/mcr‐1 plasmids consistently increased over time in all three tested wild strains both in the presence and absence of colistin.[ 19 ] However, the data in this study showed that mcr‐3 genes were more prone to be eliminated than mcr‐1 during serial passages of certain bacterial strains (e.g., CP66‐6), with or without colistin. This indicated that, apart from the properties of mcr genes themselves, the genetic background, including diverse plasmids and chromosomes, may be important for determining their evolutionary trajectory. Therefore, the fitness cost of different mcr genes could depend on the genomic landscape, and direct comparison of fitness cost of resistance genes between different bacterial species, or even between various clones of the same species, should be conducted with caution. Indeed, plasmid‐host adaptation could influence the destiny of MDR plasmids in pathogens.[ 9 , 34 ] Moreover, in addition to single bacteria, biofilm formation is also a factor influencing the coevolution of resistance genes, plasmids, and their hosts.[ 35 ]
Certain widespread mcr‐1‐bearing plasmids (IncX4 and IncI2) did not confer fitness cost during bacterial growth under no colistin pressure.[ 36 ] However, although mcr‐1‐bearing plasmids could stably persist in bacteria, the mcr‐1‐bearing composite transposon Tn6330 was dynamic and loss of mcr‐1 mediated by ISApl1 could occur.[ 17 , 18 ] In our study, detailed genetic analysis of the passaged subclones showed that mcr‐1 was more stable than mcr‐3 in the strains harboring these two genes under antibiotic exposure, and loss of mcr‐1 was mediated by Tn6330 decay or deletion of large genomic regions. In contrast, loss of mcr‐3‐bearing plasmids and partial deletion of plasmid regions mediated by insertion sequences were two major reasons for mcr‐3.1/3.5 deletion. This indicates that mcr‐3‐bearing plasmids may confer greater fitness cost than mcr‐1‐bearing plasmids and chromosomes, which is consistent with the fact that mcr‐3‐bearing plasmids are less frequent than mcr‐1‐bearing plasmids among the mcr‐bearing strains.[ 37 ]
4. Conclusions
In conclusion, this study demonstrated that the presence of colistin provided the vital driving force for the retention of mcr genes in bacteria and that the co‐occurrence of multiple mcr genes was not an optimal evolutionary event under no exposure to colistin. Deletion of resistance regions and plasmid loss were two genetic events that the bacteria utilized to eliminate mcr‐3 genes during growth. On the other hand, DNA fragment deletion mediated by mobile elements was the major cause of mcr‐1 elimination. These results support the practices of banning the usage of colistin in veterinary feed additives and optimizing colistin deployment in clinical settings worldwide. This study expands the understanding of the coevolution of novel mobile resistance genes in bacterial populations. The long‐term coevolution of multiple mcr genes in bacterial communities containing different bacterial species or clones requires further detailed investigations.
5. Experimental Section
Isolation of Bacterial Strains
A pig slaughterhouse in Sichuan, China was selected to isolate colistin‐resistant E. coli strains in July 2016. Briefly, pig feces were collected in sterile sampling bags, stored at low temperature (4 °C), and transported to the laboratory for bacterial isolation. The feces (0.5 g) were mixed with 1 mL sterile saline solution (0.9% NaCl) and 50 µL of this fecal solution was spread on MacConkey agar supplemented with 4 µg mL−1 colistin. Putative E. coli strains appearing as red colonies were selected for bacterial identification (six colonies per sample). The VITEK2 COMPACT instrument and 16S rRNA gene sequencing were used to identify bacterial species. Pure bacterial cultures were stored in 15% glycerol at −80 °C.
Identification of mcr‐1‐ and mcr‐3‐Bearing Strains, Conjugation Assay, PFGE, and S1‐PFGE
Bacterial strains identified as E. coli were screened via PCR with primers targeting mcr‐1 and mcr‐3 (MCR‐1F, ATCAGCCAAACCTATCCTATCG; MCR‐1R, ATAGATGTTGCTGTGCGTCTGC; MCR‐3F, TATGGGTTACTATTGCTGG; MCR‐3R, CGATGAGCATCAGGGTAG). All strains harboring mcr‐1 and mcr‐3 were typed by the PFGE method for bacterial genomes after XbaI digestion, with the genome of the Salmonella Braenderup strain H9812 as standard marker. A conjugation assay through the filter mating method was conducted to test the transfer ability of colistin resistance genes with E. coli J53 (Azir) as the recipient strain. To visualize the plasmid profiles of the original isolates and their transconjugants, PFGE of bacterial genomes after S1 nuclease digestion (S1‐PFGE) was performed. Antimicrobial susceptibility testing with sixteen drugs was performed using the microbroth dilution method (Table S1, Supporting Information) and results were interpreted according to the CLSI Standard.[ 38 ] E. coli ATCC 25 922 was used as quality control.
WGS and Bioinformatic Analysis
Genome sequencing utilizing short‐read Illumina and long‐read MinION platforms were performed to obtain the complete genomic sequences of E. coli strains harboring mcr‐1 and mcr‐3 according to a published method.[ 39 ] Briefly, paired‐end short reads (2 × 150 bp) were obtained by Illumina Hiseq 2500 sequencing, long reads were generated with the Rapid Barcoding Kit (SQK‐RBK004) and flowcell R9.4 in a MinION sequencer, and hybrid de novo assembly was performed with Unicycler.[ 40 , 41 ] Total genomes or plasmids of passaged bacterial populations were sequenced with a long‐read MinION platform and assembled using the Flye or Canu tools.[ 42 , 43 ] Circular complete chromosome and plasmid sequences were annotated by Rapid Annotation using Subsystem Technology and edited manually.[ 44 ] Different databases, including ISFinder, PlasmidFinder, and ResFinder, were utilized to investigate the detailed structures of genomes.[ 45 , 46 , 47 ] The BRIG and Easyfig tools were used to perform genetic context comparisons.[ 48 , 49 ]
Coevolution Assay of mcr‐1 and mcr‐3 in E. coli Populations
To evaluate the stability and evolutionary dynamics of the colistin resistance genes mcr‐1 and mcr‐3, serial passages of the E. coli strains CP8‐3, CP55, CP61, CP66‐6, and CP131, harboring both mcr‐1 and mcr‐3 genes, were performed as follows: The five strains were grown on TSA agar plates supplemented with colistin (2 µg mL−1) and the same single colony from each strain was inoculated into 10 mL LB broth with colistin (2 µg mL−1) or without antibiotics and placed in an incubator at 37 °C with shaking at 100 rpm. Then, 20 µL bacterial cultures were transferred (passage 1) onto 10 mL fresh broth (1:500 dilution) with the same conditions and incubated overnight at 37 °C with shaking at 100 rpm. After incubation, these cultures were diluted (passage 2) and 100 µL of the dilutions were spread on TSA agar; after incubation, twelve colonies from a quarter region of a plate were selected to perform genomic DNA isolation and PCR‐based detection of mcr‐1 and mcr‐3 to investigate the frequency of mcr gene loss in the bacterial populations. The cultures were then passaged for seven days based on the method described above. After passage 7, the cultures were again used to investigate the frequency of mcr gene loss. The same procedure was then performed after passage (day) 14, 21, and 28. In addition, S1‐PFGE was utilized to investigate differences in plasmid profiles among subclones of the same strain during different stages of serial culture.
Detection of Circular Intermediates
To investigate the potential role of circular intermediates in mediating the transfer of mcr‐1 and mcr‐3 genes, reverse primers (MCR1‐RC‐F, ACGCACAGCAATGCCTATGA; MCR1‐R, CTTGGTCGGTCTGTAGGG; MCR3‐cF, CCGTGTTCCTATGCAGGTGT; MCR3‐cR, GAGAACTCCACGCCAGTTCA) were designed and long‐range PCR was performed to test the potential presence of circular DNA forms.[ 22 ] PCR products were then sequenced using the Sanger method.
Conflict of Interest
The authors declare no conflict of interest.
Availability of Data and Materials
The genome sequences generated in this study were deposited in NCBI with the BioProject number PRJNA633463. The data were also deposited in the figshare database (https://doi.org/10.6084/m9.figshare.11825871) for reference.
Supporting information
Supporting Information
Acknowledgements
R.L. and P.D. contributed equally to the work. This study was financially supported by the National Natural Science Foundation of China (grants no. 31872523, 31871899, and 31702294), the Natural Science Foundation of Jiangsu Province (grant no. BK20180900), and the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD). The authors acknowledge the reviewers for their insightful and constructive comments.
Li R., Du P., Zhang P., Li Y., Yang X., Wang Z., Wang J., Bai L., Comprehensive Genomic Investigation of Coevolution of mcr genes in Escherichia coli Strains via Nanopore Sequencing. Global Challenges 2021, 5, 2000014. 10.1002/gch2.202000014
References
- 1. Fair R. J., Tor Y., Perspect. Med. Chem. 2014, 6, PMC.S14459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Laxminarayan R., Duse A., Wattal C., Zaidi A. K., Wertheim H. F., Sumpradit N., Vlieghe E., Hara G. L., Gould I. M., Goossens H., Greko C., So A. D., Bigdeli M., Tomson G., Woodhouse W., Ombaka E., Peralta A. Q., Qamar F. N., Mir F., Kariuki S., Bhutta Z. A., Coates A., Bergstrom R., Wright G. D., Brown E. D., Cars O., Lancet Infect. Dis. 2013, 13, 1057. [DOI] [PubMed] [Google Scholar]
- 3. Bhullar K., Waglechner N., Pawlowski A., Koteva K., Banks E. D., Johnston M. D., Barton H. A., Wright G. D., PLoS One 2012, 7, e34953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Aminov R. I., Front. Microbiol. 2010, 1, 134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Davies J., Davies D., Microbiol. Mol. Biol. Rev. 2010, 74, 417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. D'Costa V. M., King C. E., Kalan L., Morar M., Sung W. W. L., Schwarz C., Froese D., Zazula G., Calmels F., Debruyne R., Golding G. B., Poinar H. N., Wright G. D., Nature 2011, 477, 457. [DOI] [PubMed] [Google Scholar]
- 7. Partridge S. R., Kwong S. M., Firth N., Jensen S. O., Clin. Microbiol. Rev. 2018, 31, e00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yang Q., Li M., Spiller O. B., Andrey D. O., Hinchliffe P., Li H., MacLean C., Niumsup P., Powell L., Pritchard M., Papkou A., Shen Y., Portal E., Sands K., Spencer J., Tansawai U., Thomas D., Wang S., Wang Y., Shen J., Walsh T., Nat. Commun. 2017, 8, 2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Porse A., Schonning K., Munck C., Sommer M. O., Mol. Biol. Evol. 2016, 33, 2860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bulman Z. P., Chen L., Walsh T. J., Satlin M. J., Qian Y., Bulitta J. B., Peloquin C. A., Holden P. N., Nation R. L., Li J., Kreiswirth B. N., Tsuji B. T., mBio 2017, 8, e00540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Carroll L. M., Gaballa A., Guldimann C., Sullivan G., Henderson L. O., Wiedmann M., mBio 2019, 10, e00853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wang C., Feng Y., Liu L., Wei L., Kang M., Zong Z., Emerging Microbes Infect. 2020, 9, 508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Li R., Zhang P., Yang X., Wang Z., Fanning S., Wang J., Du P., Bai L., J. Antimicrob. Chemother. 2019, 74, 1517. [DOI] [PubMed] [Google Scholar]
- 14. Creighton J., Anderson T., Howard J., Dyet K., Ren X., Freeman J., J. Antimicrob. Chemother. 2019, 74, 3113. [DOI] [PubMed] [Google Scholar]
- 15. Garcia V., Garcia‐Menino I., Mora A., Flament‐Simon S. C., Diaz‐Jimenez D., Blanco J. E., Alonso M. P., Blanco J., Int. J. Antimicrob. Agents 2018, 52, 104. [DOI] [PubMed] [Google Scholar]
- 16. Sun J., Li X. P., Fang L. X., Sun R. Y., He Y. Z., Lin J., Liao X. P., Feng Y., Liu Y. H., Int. J. Antimicrob. Agents 2018, 51, 842. [DOI] [PubMed] [Google Scholar]
- 17. Li R., Chen K., Chan E. W.‐C., Chen S., J. Antimicrob. Chemother. 2019, 74, 1807. [DOI] [PubMed] [Google Scholar]
- 18. Zhang P., Bai L., Li Y., Wang Z., Li R., Antimicrob. Agents Chemother. 2019, 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yang Q. E., MacLean C., Papkou A., Pritchard M., Powell L., Thomas D., Andrey D. O., Li M., Spiller B., Yang W., Walsh T. R., ISME J. 2020, 14, 861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yoshikawa T., Aoyama T., Tanabe K., Nishikawa K., Ito Y., Hayashi T., Cho H., Miyashita Y., Tsuburaya A., Sakamoto J., Dig. Surg. 2016, 33, 424. [DOI] [PubMed] [Google Scholar]
- 21. Li R., Yu H., Xie M., Chen K., Dong N., Lin D., Chan E. W.‐C., Chen S., Int. J. Antimicrob. Agents 2018, 51, 578. [DOI] [PubMed] [Google Scholar]
- 22. Li R., Xie M., Zhang J., Yang Z., Liu L., Liu X., Zheng Z., Chan E. W.‐C., Chen S., J. Antimicrob. Chemother. 2016, 72, 393. [DOI] [PubMed] [Google Scholar]
- 23. Li R., Xie M., Lv J., Wai‐Chi Chan E., Chen S., J. Antimicrob. Chemother. 2016, 72, 696. [DOI] [PubMed] [Google Scholar]
- 24. Snesrud E., He S., Chandler M., Dekker J. P., Hickman A. B., McGann P., Dyda F., Antimicrob. Agents Chemother. 2016, 60, 6973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shen Z., Wang Y., Shen Y., Shen J., Wu C., Lancet Infect. Dis. 2016, 16, 293. [DOI] [PubMed] [Google Scholar]
- 26. Nang S. C., Morris F. C., McDonald M. J., Han M. L., Wang J., Strugnell R. A., Velkov T., Li J., J. Antimicrob. Chemother. 2018, 73, 1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tietgen M., Semmler T., Riedel‐Christ S., Kempf V. A. J., Molinaro A., Ewers C., Gottig S., Int. J. Antimicrob. Agents 2018, 51, 554. [DOI] [PubMed] [Google Scholar]
- 28. Hadjadj L., Baron S. A., Olaitan A. O., Morand S., Rolain J. M., Front. Microbiol. 2019, 10, 2720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shen C., Zhong L.‐L., Yang Y., Doi Y., Paterson D. L., Stoesser N., Ma F., El‐Sayed M. A. E.‐G., Feng S., Huang S., bioRxiv 2020. [Google Scholar]
- 30. Wang Q., Sun J., Li J., Ding Y., Li X. P., Lin J., Hassan B., Feng Y., Microbiome 2017, 5, 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yin W., Li H., Shen Y., Liu Z., Wang S., Shen Z., Zhang R., Walsh T. R., Shen J., Wang Y., mBio 2017, 8, e00543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Xu Y., Zhong L. L., Srinivas S., Sun J., Huang M., Paterson D. L., Lei S., Lin J., Li X., Tang Z., Feng S., Shen C., Tian G. B., Feng Y., EBioMedicine 2018, 34, 139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Shen Y., Xu C., Sun Q., Schwarz S., Ou Y., Yang L., Huang Z., Eichhorn I., Walsh T. R., Wang Y., Zhang R., Shen J., Antimicrob. Agents Chemother. 2018, 62, e00404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hulter N., Ilhan J., Wein T., Kadibalban A. S., Hammerschmidt K., Dagan T., Curr. Opin. Microbiol. 2017, 38, 74. [DOI] [PubMed] [Google Scholar]
- 35. Stalder T., Cornwell B., Lacroix J., Kohler B., Dixon S., Yano H., Kerr B., Forney L. J., Top E. M., Mol. Biol. Evol. 2020, 37, 1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wu R. J., Yi L. X., Yu L. F., Wang J., Liu Y. Y., Chen X. J., Lv L. C., Yang J., Liu J. H., Front. Microbiol. 2018, 9, 10.3389/fmicb.2018.00331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wang Z., Fu Y., Schwarz S., Yin W., Walsh T. R., Zhou Y., He J., Jiang H., Wang Y., Wang S., Vet. Microbiol. 2019, 230, 56. [DOI] [PubMed] [Google Scholar]
- 38. CLSI. Performance Standards for Antimicrobial Susceptibility Testing. 28th ed. CLSI supplement M100 , Clinical & Laboratory Standards Institute, Wayne, PA, USA: 2018. [Google Scholar]
- 39. Li R., Chen K., Chan E. W. C., Chen S., J. Antimicrob. Chemother. 2018, 73, 2691. [DOI] [PubMed] [Google Scholar]
- 40. Wick R. R., Judd L. M., Gorrie C. L., Holt K. E., PLoS Comput. Biol. 2017, 13, e1005595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Li R., Xie M., Dong N., Lin D., Yang X., Wong M. H. Y., Chan E. W.‐C., Chen S., GigaScience 2018, 7, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Huang Y., Zheng N., Wang Z., Ying L., Huang F., Cao Y., Chem. Commun. 2017, 53, 1997. [DOI] [PubMed] [Google Scholar]
- 43. Koren S., Walenz B. P., Berlin K., Miller J. R., Bergman N. H., Phillippy A. M., Genome Res. 2017, 27, 722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Overbeek R., Olson R., Pusch G. D., Olsen G. J., Davis J. J., Disz T., Edwards R. A., Gerdes S., Parrello B., Shukla M., Vonstein V., Wattam A. R., Xia F. F., Stevens R., Nucleic Acids Res. 2014, 42, D206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Siguier P., Perochon J., Lestrade L., Mahillon J., Chandler M., Nucleic Acids Res. 2006, 34, D32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Carattoli A., Zankari E., Garcia‐Fernandez A., Larsen M. V., Lund O., Villa L., Aarestrup F. M., Hasman H., Antimicrob. Agents Chemother. 2014, 58, 3895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Zankari E., Hasman H., Cosentino S., Vestergaard M., Rasmussen S., Lund O., Aarestrup F. M., Larsen M. V., J. Antimicrob. Chemother. 2012, 67, 2640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Alikhan N. F., Petty N. K., Ben Zakour N. L., Beatson S. A., BMC Genomics 2011, 12, 402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sullivan M. J., Petty N. K., Beatson S. A., Bioinformatics 2011, 27, 1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information
Data Availability Statement
The genome sequences generated in this study were deposited in NCBI with the BioProject number PRJNA633463. The data were also deposited in the figshare database (https://doi.org/10.6084/m9.figshare.11825871) for reference.


