Abstract
Purpose:
Deeply embedded corneal foreign bodies and intrastromal foreign body removal can often be a challenge. The aim of this report was to describe the utility of endoscopy in visualization and removal of an embedded corneal bee stinger.
Methods:
A 44-year-old male patient developed toxic keratopathy after injury from a bee stinger. On examination, the bee stinger was noted to be deeply embedded in the corneal stroma. A superficial keratectomy was initially attempted; however, the stinger was noted to be intrastromal and protruding into the anterior chamber and could not be removed. An Endoscopy-assisted visualization was used to remove the stinger.
Results:
The bee stinger was successfully removed and the patient's vision improved to 20/100 from an initial CFCF (counting fingers close to face) at time of presentation. At the end of 3 months follow-up, there was residual corneal edema along with cataractous changes in the lens as a sequelae of the initial bee sting injury. The patient subsequently underwent an endothelial keratoplasty along with phacoemulsification with intraocular lens implantation and the final BCVA improved to 20/40.
Conclusion:
Endoscopyassisted visualisation of anterior chamber and angle structures can be valuable in removal of retained and deeply embedded corneal or intracameral foreign bodies.
Keywords: Bee sting injury, embedded corneal foreign body, endoscopy, toxic keratitis
Corneal bee sting injuries can lead to various ocular manifestations including conjunctival injury with or without retained stings, toxic keratitis, bullous keratopathy, anterior uveitis, iris atrophy, glaucoma, cataract, lens subluxation, optic neuritis, and panuveitis.[1,2,3,4,5,6] Bee venom is also known to incite a local toxic or immunologic reaction on cornea.[7,8] Management of corneal bee sting injuries in general is to control inflammatory reaction and to prevent secondary infections with conservative approach of topical steroids, antibiotics, and cycloplegics. However, removal of impacted and deeply embedded stingers remains controversial. In general removal of bee stinger depends on associated severity of inflammation/infiltration at presentation, the proximity of the injury site to the visual axis, depth of stinger and its external accessibility.[5]
Endoscopy-assisted visualization has become an invaluable tool in vitreoretinal surgeries where it has been used in management of ocular trauma, endophthalmitis, and in eyes with opaque anterior segment and media opacities.[9,10,11,12]
We describe in this case report an innovative approach where we utilized an endoscope which is used in vitreoretinal surgeries to visualize and remove the embedded bee stinger.
Case Report
A 44-year-old patient presented with pain, redness and diminution of vision since 10 days in his right eye after bee sting injury. Complete ophthalmic evaluation was done and his best-corrected visual acuity in the right eye was counting fingers close to face and 20/20 in the left eye. Slit-lamp examination of the right eye showed 1.8 × 2.1 mm sterile corneal infiltrate at 7-8 o clock adjacent to limbus along with a bee stinger embedded deep into the corneal stroma and diffuse corneal edema, descemet's folds, epithelial bullae and corneal scarring [Fig. 1a]. The left eye was essentially normal. He was started on topical steroids, antibiotics, cycloplegics and a debridement of necrotic surrounding corneal tissue was attempted initially to remove the stinger. However, only partial removal of stinger was achieved due to suboptimal visualisation under diffuse illumination of operating microscope. Postoperative anterior segment optical coherence tomography (AS-OCT) showed protrusion of retained stinger into anterior chamber [Fig. 1b and epithelial bullae [Fig. 1c]. Hence an endoscopy [Fig. 2a, 2b] probe was used to visualise the stinger and under endoscopy guided visualisation the stinger was removed.
Figure 1.
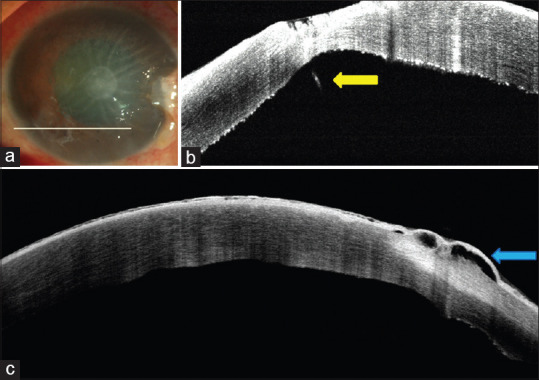
(a) Diffuse slit-lamp photograph at initial presentation showing infiltrates at 7–8 o clock with diffuse descemets folds and corneal edema. An AS OCT examination revealed the presence of a protruding stinger (yellow arrow) from cornea into anterior chamber (1b) and epithelial bullous edema (blue arrow) (1c)
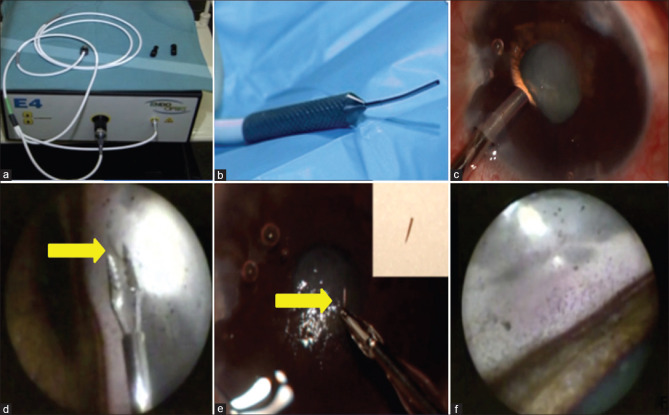
Figure 2.
(2a, 2b) Console and probe of E4 laser and Endoscopy system (2c) Insertion of endoscopic probe at diametrically opposite end of embedded bee sting (2d) Endoscopic view of the stinger (yellow arrow). A serrated 23 G forceps was used for grasping the stinger and it was subsequently removed and delivered out. The removed stinger (yellow arrow) can be seen clearly in inset (2e). (2f) show endoscopy images of anterior chamber angle clearly delineating structures of the angle
Surgical Technique
The endoscopy was performed under local anesthesia.The steps, in brief, included sterile draping of the eye, and subsequently, 2 corneal stab incisions were made. The first incision was exactly opposite to impacted stinger in the superonasal quadrant (SNQ) for insertion of endoscope and the second one was made superiorly at 11 o clock for insertion of the 23 guage forceps to retrieve the impacted stinger. Initially, pilocarpine was injected to constrict the pupil so as to prevent an inadvertent lens injury. Subsequently viscoelastic was injected to deepen the anterior chamber. The 23 gauge endoscope E4 Laser and Endoscopy System (EndoOptiks, Inc., Little Silver, NJ, USA) with light and video dual function was then introduced through the SNQ [Fig. 2a, 2b]. With the aid of the camera connected to the endoscope the bee stinger was visualised [Fig. 2c] and then under endoscopy guided visualisation, it was grasped with the 23 G serrated forceps and removed [Fig. 2d, 2e].
Endoscopy-assisted visualization also allowed for examination of the angle [Fig. 2f] for any remnant foreign bodies. The use of endoscopy guided visualisation reduced the maneuvering required to remove the stinger and thus ensured that the removal was less traumatic.
Results
After the removal of the bee sting, the patient was continued on topical steroids in tapering dose along with cycloplegics. At 3 month follow-up his vision had improved to 20/100 from an CFCF (counting fingers close to face) at time of initial presentation. However, there was residual corneal edema due to endothelial dysfunction along with cataractous changes as a sequelae of the initial bee sting injury. The patient subsequently underwent an endothelial keratoplasty and phacoemulsification with intraocular lens implantation and the final BCVA improved to 20/40.
Discussion
Corneal bee sting injuries are a relatively rare condition. Ocular surface is the first point of contact for all exogenous injuries apart from eyelids. After Bee sting, the bee loses its stinger and part of its abdomen leading to eventual death of bee.[1] In general removal of bee stinger depends on associated severity of inflammation/infiltration at presentation, the proximity of the injury site to the visual axis, depth of stinger and its external accessibility.[5]
Arcieri et al.[3] and Chuah et al.[9] had managed bee sting injury conservatively without removal of stinger however Jain et al.[10] have reported removing the retained stinger as it caused keratouveitis. In another report, Gudiseva et al.[11] have described the occurrence of secondary fungal infection in retained bee stinger
If the stinger is deeply embedded and associated with surrounding edema or infiltrate, it may lead to inadequate removal of stinger because of lack of proper visualization. Chauhan et al.[12] have described removal of an embedded bee sting with the help of an endoilluminator.
In our case, the initial attempt to remove stinger went in vain as it was deeply embedded and the associated diffuse corneal edema and corneal infiltration were impeding an adequate visualization under diffuse illumination of operating microscope and therefore we decided to remove the stinger with the help of an endoscopy-guided visualisation.
Ever since the introduction of the first ophthalmic endoscope by Thorpe[13] in 1934 for the extraction of non-magnetic intraocular foreign bodies, it has served a unique advantage of viewing the posterior segment with less surgical trauma, overcoming the problems of media opacity. In 1990, a 20- gauge endoscope with image projection on an electronic monitor was described.[14] An endoscope inserted via pars plana, with minimum manipulation of the eye gives a realistic picture of the posterior segment.[15,16]
Endoscopy-assisted removal of foreign body from angle of anterior chamber has also been described earlier.[17,18] An endoscopy-assisted visualisation will also help in precise localisation of the foreign body and therefore will help in minimising trauma to adjacent ocular structures and reduce the manipulations since we can now directly visualise the foreign body. This led us to use an endoscope to visualise the stinger and utilise endoscopy-assisted visualisation in removing the stinger
Conclusion
Endoscopic-assisted visualization can be a valuable tool in removing deeply embedded bee stingers or other foreign bodies. An endoscopy-assisted visualization also helps in minimizing trauma to adjacent ocular structures and can be useful in assessing the angle structures and in removing occult angle foreign bodies.
Financial support and sponsorship
Support provided by Hyderabad Eye Research Foundation, Hyderabad, India.
The funders had no role in the preparation, review or approval of the manuscript.
Conflicts of interest
There are no conflicts of interest.
Video available on: www.ijo.in
References
- 1.Semler-Collery A, Hayek G, Ramadier S, Perone JM. A case of conjunctival bee sting injury with review of the literature on ocular bee stings. Am J Case Rep. 2019;20:1284–9. doi: 10.12659/AJCR.917592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lin PH, Wang NK, Hwang YS, Ma DH, Yeh LK. Bee sting of the cornea and conjunctiva: Management and outcomes. Cornea. 2011;30:392–4. doi: 10.1097/ICO.0b013e3181f234a6. [DOI] [PubMed] [Google Scholar]
- 3.Arcieri ES, França ET, de Oliveria HB, De Abreu Ferreira L, Ferreira MA, Rocha FJ. Ocular lesions arising after stings by hymenopteran insects. Cornea. 2002;21:328–30. doi: 10.1097/00003226-200204000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Kim JM, Kang SJ, Kim MK, Wee WR, Lee JH. Corneal wasp sting accompanied by optic neuropathy and retinopathy. Jpn J Ophthalmol. 2011;55:165–7. doi: 10.1007/s10384-010-0912-z. [DOI] [PubMed] [Google Scholar]
- 5.Razmjoo H, Abtahi M-A, Roomizadeh P, Mohammadi Z, Abtahi S-H. Management of corneal bee sting. Clin Ophthalmol. 2011;5:1697–700. doi: 10.2147/OPTH.S26919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nakatani Y, Nishimura A, Sugiyama K. Successful treatment of corneal wasp sting-induced panuveitis with vitrectomy. J Ophthalmic Inflamm Infect. 2013;3:18. doi: 10.1186/1869-5760-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Teoh SCB, Lee J-J, Fam H-B. Corneal honeybee sting. Can J Ophthalmol. 2005;40:469–71. doi: 10.1016/S0008-4182(05)80008-0. [DOI] [PubMed] [Google Scholar]
- 8.Gürlü VP, Erda N. Corneal bee sting-induced endothelial changes. Cornea. 2006;25:981–3. doi: 10.1097/01.ico.0000226364.57172.72. [DOI] [PubMed] [Google Scholar]
- 9.Chuah G, Law E, Chan WK, Ang CL. Case reports and mini review of bee stings of the cornea. Singapore Med J. 1996;37:389–91. [PubMed] [Google Scholar]
- 10.Jain V, Shome D, Natarajan S. Corneal bee sting misdiagnosed as viral keratitis. Cornea. 2007;26:1277–8. doi: 10.1097/ICO.0b013e31814b8bae. [DOI] [PubMed] [Google Scholar]
- 11.Gudiseva H, Uddaraju M, Pradhan S, Das M, Mascarenhas J, Srinivasan M, et al. Ocular manifestations of isolated corneal bee sting injury, management strategies, and clinical outcomes. Indian J Ophthalmol. 2018;66:262–8. doi: 10.4103/ijo.IJO_600_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chauhan D. Corneal honey bee sting: Endoilluminator-assisted removal of retained stinger. Int Ophthalmol. 2012;32:285–88. doi: 10.1007/s10792-012-9553-1. [DOI] [PubMed] [Google Scholar]
- 13.Thorpe HE. Ocular endoscopy: An instrument for removal of intravitreous nonmagnetic foreign bodies. Trans Am Acad Ophthalmol. 1934;39:422–4. [Google Scholar]
- 14.Volkov VV, Danilov AV, Vassin LN, Frolov YA. Flexible endoscopes.Ophthalmoendoscopic techniques and case reports. Arch Ophthalmol. 1990;108:956–7. doi: 10.1001/archopht.1990.01070090058039. [DOI] [PubMed] [Google Scholar]
- 15.Reddy Pappuru RR, Tyagi M, Paulose RM, Dave VP, Das T, Chhablani J, et al. Role of diagnostic endoscopy in posterior segment evaluation for definitive prognostication in eyes with corneal opacification. Am J Ophthalmol. 2017;176:9–14. doi: 10.1016/j.ajo.2016.12.018. [DOI] [PubMed] [Google Scholar]
- 16.Dave VP, Pappuru RR, Tyagi M, Pathengay A, Das T. Endoscopic vitrectomy in endophthalmitis: initial experience of 33 cases at a tertiary eye care center. Clin Ophthalmol. 2019;13:243–51. doi: 10.2147/OPTH.S185716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xiao-Qiang L, Tian-Lin X, Zhen-Quan Z, Wen-Can W, Qin-Mei W, Jia Q, et al. Endoscopy-assisted removal of Nonmagnetic metallic foreign body in anterior chamber angle. Ophthalmic Surg Lasers Imaging. 2010:1–4. doi: 10.3928/15428877-20100215-39. doi: 10.3928/15428877-20100215-39. [DOI] [PubMed] [Google Scholar]
- 18.Nukala N, Pappuru RR, Dave VP. Endoscopy-assisted removal of angle foreign body presenting as persistent localised corneal oedema BMJ Case Rep. 2020;13:e233419. doi: 10.1136/bcr-2019-233419. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.