Abstract
Background:
Superior capsular reconstruction (SCR) represents a new option for the treatment of irreparable rotator cuff tears.
Purpose/Hypothesis:
This study aimed to evaluate the clinical and radiologic outcomes of SCR and compare them with the outcomes of partial repair (PR) of the infraspinatus tendon. The hypothesis was that there would be no significant differences between the clinical and radiologic outcome parameters of SCR and PR after a minimum follow-up of 2 years.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Of 21 patients who underwent SCR, 20 patients were matched in a 1:1 ratio according to sex, age, and tear configuration with 20 of 60 patients who had undergone PR; all patients were prospectively evaluated for a minimum follow-up of 2 years. The investigated outcome measures included the Constant score; Western Ontario Rotator Cuff (WORC) index; Disabilities of the Arm, Shoulder and Hand (DASH) score; and radiologic analysis of acromiohumeral distance (AHD) and humeral head centralization (HHC).
Results:
There were no differences in the demographic data between the SCR and PR groups. The mean age of both groups was 62.3 years (range, 47-79 years), the mean tear configuration was Bateman 3.0 and Patte 2.8, and the mean follow-up period was 29.4 months (range, 24-53 months). At final follow-up, no significant differences were seen between the SCR and PR groups with regard to Constant score (77.1 vs 82.7), age- and sex-adapted Constant score (85.5% vs 91.4%), DASH score (15.6 vs 7.8), or WORC index (81.1 vs 90.4). No significant differences in the AHD or HHC were seen between the groups. The reoperation rate was 4.8% (1/21) in the SCR cohort and 15% (9/60) in the PR cohort.
Conclusion:
Both SCR and PR resulted in significant improvements in patient-reported outcomes at 2-year follow-up, with no significant differences in clinical outcomes between the 2 techniques. Further follow-up is needed to determine whether there are long-term differences in HHC and development of cuff tear arthropathy. Further investigations should also focus on the cost-effectiveness of the respective procedures.
Keywords: shoulder rotator cuff, superior capsular reconstruction, partial rotator cuff repair, irreparable tears
Management of symptomatic, irreparable, posterosuperior rotator cuff tears (RCTs) is extremely challenging and controversial. Disruption and tendon retraction of the posterosuperior muscle-tendon units may result in superior humeral head migration on initial abduction. This may lead to impingement of the humeral head underneath the acromion.34,45 Therapeutic options for joint preservation include surgical and nonsurgical treatments. Numerous surgical options have been proposed to address this condition, including partial repair (PR) of the residual cuff and superior capsular reconstruction (SRC).2,23,32
PR was first described in 1994 by Burkhart,8 who arthroscopically performed a partial or “functional” repair, where the less retracted tendon edges restore the rotator cuff’s force couple and provide a stable fulcrum for the glenohumeral joint.6,11 PR has been shown to be a reliable option in patients with irreparable RCTs, with up to 70% good to excellent results.7,16,26 Moreover, PR was proven to provide superior results when compared with debridement alone in a level 1 study.4 SCR is a relatively new technique that has been developed to address posterosuperior irreparable RCTs and decrease the subsequent superior migration of the humeral head. SCR was first described by Mihata et al,31–33 who reconstructed the superior capsule with a fascia lata autograft. To decrease the morbidity of the donor site, recent literature has reported the use of synthetic patches, dermal allograft, xenograft, or long head of the biceps tendon autograft.5,12,21,28,43,51 An earlier series studying these techniques showed problems with graft healing and thereby altered results.14 Later, Lee and Min29 showed no significant differences in clinical scores but a decreased acromiohumeral distance (AHD) in cases of graft failure when comparing a group of patients with graft tears versus a group of patients with intact grafts. More recent results have been promising so far. Even in patients with severe functional deficits, improvements seem to be maintained for at least 2 years.10,23 However, it is difficult to compare outcomes of both techniques using the current literature because of inconsistencies in the description of tendon involvement, tear size, and repair techniques. The literature is limited concerning clinical results, and comparative studies are lacking.
Because both PR and SCR are performed arthroscopically using suture anchors to treat irreparable posterosuperior cuff tears in patients without glenohumeral arthritis and with an intact subscapularis, we decided to compare the outcomes of these 2 techniques. Thus, the purpose of this study was to evaluate clinical and radiologic outcomes of PR of the infraspinatus tendon compared with SCR using a xenograft. We hypothesized that there would be no significant differences in clinical and radiologic outcome parameters after a minimum follow-up of 2 years.
Methods
This study received ethics committee approval, and written informed consent was obtained from all study participants. The participants were 20 of 21 patients who had undergone arthroscopic SCR for irreparable, full-thickness, posterosuperior RCTs between October 2015 and May 2017.
The primary inclusion criteria were an irreparable tear that was classified on preoperative magnetic resonance imaging (MRI) scans as at least grade 3 according to Bayne and Bateman,3 showed an advanced retraction of grade 3 according to Patte,36 or demonstrated advanced fatty infiltration of at least grade 3 according to Goutallier et al19 and/or if during the operation, even after arthroscopic release, the tendons could not be advanced to their insertion at the greater tuberosity. We identified a group of 60 patients who satisfied the same inclusion criteria, had undergone PR of an irreparable posterosuperior RCT between January 2009 and December 2016, and consented to being clinically reevaluated and included in the present study. A total of 20 patients who had undergone SCR were matched 1:1 with 20 patients who had undergone PR according to age, sex, and tear configuration in the anteroposterior direction according to Bayne and Bateman3 and in the mediolateral direction according to Patte.36 Exclusion criteria included, among others, unwillingness to participate in the study, lack of 2-year follow-up, revision surgery after the index procedure, and subscapularis rupture. Moreover, patients with a decompensated posterior cuff function measured using the external rotation lag sign were excluded if the lag was >20° with the arm at the side (Table 1). Regarding the PR cohort, only patients without revision surgery at the time of the follow-up were eligible for matching.
Table 1.
Indications and Contraindications for Partial Repair and Superior Capsular Reconstruction
| Indications | Contraindications |
|---|---|
|
|
The decision to perform surgery was made after failure of nonoperative treatment and rehabilitation for at least 3 months. None of the patients in either group showed pseudoparalysis of the shoulder, and all patients had an external rotation lag sign of <20° with the arm at the side. The preoperative Constant score showed no significant difference between groups. All patients reported intolerable pain with pain scores on a visual analog scale of ≥5. Therefore, pain was the main indication for surgery. The indications and contraindications are shown in Table 1. All SCR surgeries were performed by one of the study authors (S.G.), and all PR surgeries were performed by another author (M.K.). The SCR group consisted of consecutive patients, and they were followed prospectively and reevaluated at a minimum of 2 years.
Surgical Technique
All patients initially underwent shoulder arthroscopy in the beach-chair position under general anesthesia and interscalene block. The arm was maintained comfortably at the patient’s side (“neutral abduction”) and in neutral rotation using a mechanical arm holder. Arthroscopic portals were used for complete arthroscopic evaluation, and the repairability of the tendon on its insertion was assessed. Partial resection of the subacromial bursa was performed in order to identify all relevant structures and remove inflamed tissue. Debridement of the tear and the insertion zone was performed. Reducibility of the rotator cuff was tested by grasping the tendon edges and attempting to advance them to the footprint. The supra- and infraspinatus tendons were then mobilized, and adhesions were divided in order to allow advancement of as much cuff tissue to the native footprint as possible. The supraspinatus tendon was not repairable in all cases. Once the irreparable nature of the tear was confirmed, a subacromial decompression and a tenotomy or tenodesis of the long head of the biceps tendon, if found to be intact, were performed.
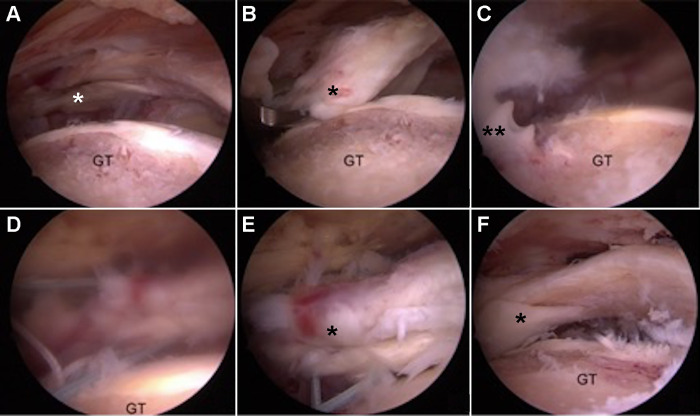
For the PR technique, the footprints of infraspinatus and supraspinatus tendons on the greater tuberosity were debrided and prepared. The lesion was then minimized as much as possible, and the superior part of the remaining infraspinatus tendon was shifted anterosuperiorly on the greater tuberosity. The optimal position for fixation and the amount of repair possible were determined. Tear size, retraction pattern, and tendon stiffness determined the amount of repair possible for each patient individually. According to the size of the remaining tissue, one or two 4.5-mm double-loaded suture anchors (Corkscrew FT; Arthrex GmbH) were placed. To fix the infraspinatus to the greater tuberosity, the tendon was penetrated using a suture passer (Scorpion; Arthrex GmbH), and a single-row fixation technique was used. Side-to-side sutures or margin convergence techniques were not performed in this series (Figure 1).
Figure 1.
Partial repair of the infraspinatus tendon. Intra-articular view from the anterolateral portal of a right shoulder. (A) Irreparable rotator cuff tear involving the supraspinatus and infraspinatus tendons. (B) The infraspinatus tendon is pulled using a grasper toward the greater tuberosity (GT). (C) Insertion of a 4.5-mm double-loaded suture anchor. (D) The sutures are passed through the tendon. (E) By pulling on the sutures, the infraspinatus tendon is attached to the greater tuberosity. (F) Final partial repair of the infraspinatus tendon. *Infraspinatus tendon. **4.5-mm suture anchor.
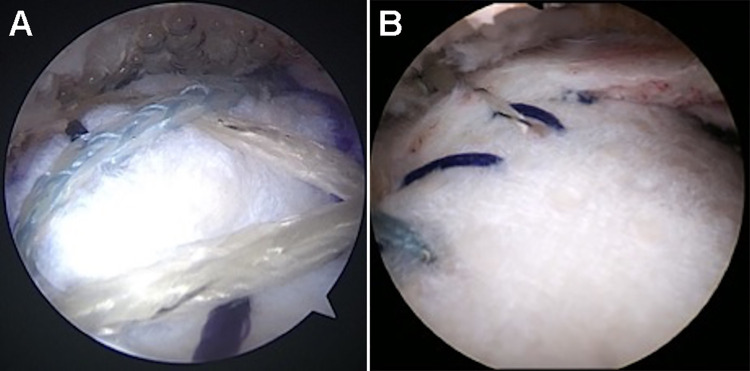
For the SCR technique, the surgeon debrided and prepared the superior scapular bone medial to the superior glenoid rim and the footprint on the greater tuberosity. Two double-loaded 3.0-mm anchors (SutureTak; Arthrex GmbH) were placed in the superior glenoid lateral to the base of the coracoid and at the upper border of the still-intact posterior part of the rotator cuff. Two 4.75-mm knotless anchors (SwiveLock; Arthrex GmbH) loaded with nonabsorbable suture tape and No. 2 sutures (Speed Bridge; Arthrex GmbH) were placed in the greater tuberosity at the cartilage bone junction of the debrided footprint. The No. 2 suture of the posterior anchor of the greater tuberosity was used to partially repair the infraspinatus tendon, thereby decreasing the size of the tear (Figure 2).
Figure 2.
Intra-articular view from the anterolateral portal of a left shoulder with all anchors in place and partial repair of the infraspinatus tendon. *Double-loaded No. 3.0 SutureTak anchors (Arthrex GmbH) in the superior glenoid. **Partially repaired infraspinatus tendon. ***Greater tuberosity with 2 No. 4.75 SwiveLock anchors (Arthrex GmbH) loaded with FiberTapes (Arthrex GmbH). G, glenoid; HH, humeral head.
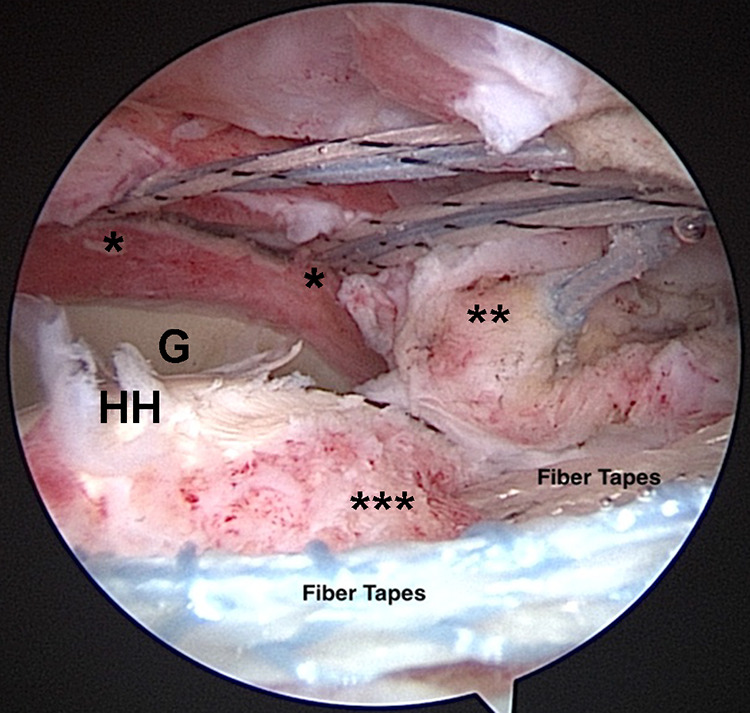
The individual anchors served as landmarks to determine the size of the patch. Measurement was performed using a flexible arthroscopic measurement probe, which enables measurement of arc distances that account for the curvature of the bones (AR-Scope measurement probe, 220 mm, 60°; Arthrex GmbH). According to the measurement, a double-layered, acellular, dermal porcine xenograft patch (DX Reinforcement Matrix; Arthrex GmbH) was sewn together resulting in a 3 mm--thick graft. The sutures and the tapes of the loaded anchors were passed through the patch while 1.0 cm of patch length was added laterally (Figure 3).
Figure 3.

Xenograft patch after suture passage, ready to be shuttled.
By means of a pulley, the graft was shuttled into the joint, and the medial sutures were each tied together. The shoulder was placed in neutral rotation and 15° of abduction, the graft was tensioned, and the FiberTapes (Arthrex GmbH) were crossed. Two additional 4.75-mm knotless anchors were used to fix the graft laterally at the greater tuberosity by using the FiberTapes as a suture bridge (Figure 3). Finally, the upper border of the infraspinatus tendon was fixed to the posterior border of the graft using side-to-side suturing, thereby closing the gap between the graft and the tendon and further shifting the infraspinatus tendon anterosuperiorly above the humeral head (Figure 4). The rotator interval was left open in every case to avoid inducing stiffness; for the same reason, no anterior side-to-side suturing to the subscapularis tendon was performed.
Figure 4.
(A) Intra-articular view of the lateral patch fixation. (B) Side-to-side patch fixation to the upper border of the infraspinatus tendon.
Postoperative Protocol
The postoperative rehabilitation for both techniques consisted of initial immobilization in a sling with 30° of shoulder abduction for 6 weeks, with limited passive mobilization allowed. This was followed by active assisted mobilization from week 7 and careful strengthening exercises from week 13. Unrestricted activity was allowed at 4 to 6 months after the operation according to the individual’s rehabilitation progress.
Clinical and Radiographic Evaluation
The Constant score was evaluated preoperatively, and the age- and sex-adapted Constant score as well as the Western Ontario Rotator Cuff (WORC) index and the Disabilities of the Arm, Shoulder and Hand (DASH) score were evaluated at final follow-up.13,20,50 Strength measurement for the Constant score was conducted with the arm in 90° of scapular abduction using a handheld dynamometer (microFET; Hoggan Health Industries) and was recorded as 0 if patients could not reach this position.
AHD was measured according to the literature as the shortest distance between the inferior cortex of the acromion and the top of the humeral head.18,35,38 AHD was assessed (in mm) from calibrated digital radiographs. To assess humeral head centralization (HHC) on the radiographs, a circle was drawn around the humeral head, incorporating both of its superior and medial contours. Then a horizontal line was drawn connecting the most medial and lateral points of the circle. The center of the glenoid cavity was measured by connecting the most superior and inferior landmarks of the anterior articular margin. The distance between the midpoint of this vertical line and the point where the horizontal line and vertical lines intersected was measured (Figure 5). Moreover, x-rays were evaluated according to the Hamada classification.
Figure 5.
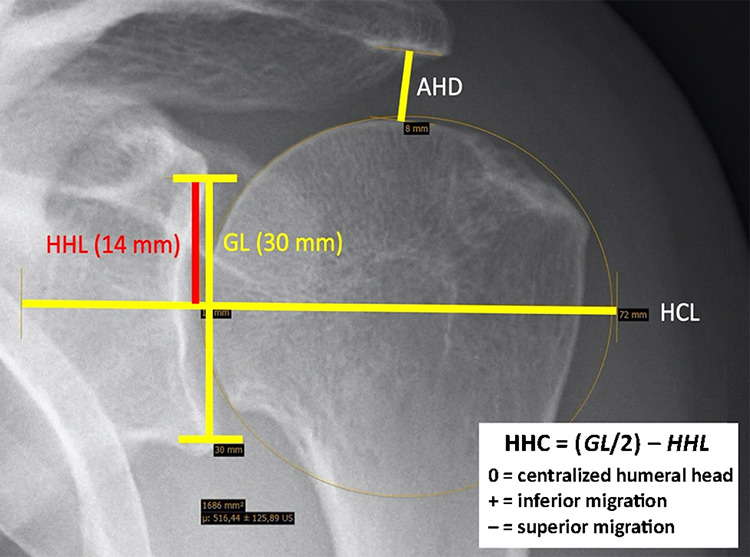
Measurement of humeral head centralization (HHC) on a true anteroposterior shoulder radiograph. AHD, acromiohumeral distance; GL, glenoid line; HCL, humeral head center line; HHL, humeral head line.
Statistical Analysis
An a priori sample size calculation was performed based on previously published data using the Constant score in rotator cuff surgery.27 Using α = .05, 1-β = .80, and a clinically significant difference in the Constant score of 10.4 points as input variables, we calculated that a minimum of 13 patients had to be included in each group.
Score data from the Constant, WORC index, and DASH are expressed as mean ± SD. The patients treated using the SCR technique were matched to patients treated using the PR technique according to sex, age, and type of RCT,25 which was classified according to the Bayne and Bateman3 and Patte36 classifications. For statistical analysis, the t test was used to compare means for the Constant, WORC index, and DASH results between the SCR and PR cohorts. The significance level was set to P < .05. All analyses were performed using SPSS Statistics (Version 25.0; IBM Corp).
Results
The 20 consecutive patients in the SCR group and the matched 20 patients in the PR group had a mean age of 62.3 years (range, 47-79 years) at the time of the operation. The mean follow-up time was 29.4 months (range, 24-53 months). The 4 female and 16 male patients of the SCR group and 4 female and 16 male patients of the PR group showed similar anthropometric data and were comparable with regard to RCT characteristics (Table 2). We found no significant differences in preoperative Constant score, AHD, or HHC (Table 3).
Table 2.
Anthropometric Data and Rotator Cuff Tear Classification Scoresa
| SCR Group (n = 20) |
PR Group (n = 20) |
P Value | |
|---|---|---|---|
| Dominant shoulder operated, n (%) | 13 (65) | 12 (60) | |
| Age at time of surgery, y, mean (range) | 62.1 (47-77) | 62.5 (48-79) | .47 |
| Follow-up, mo, mean (range) | 25.7 (24-30) | 34.0 (24-53) | .0058 |
| Bateman score, mean ± SD | 3.0 ± 0.4 | 3.0 ± 0.3 | .5 |
| Patte score, mean ± SD | 3.0 ± 0.2 | 2.6 ± 0.3 | .0003 |
aBolded P values indicate statistically significant between-group differences (P < .05). PR, partial infraspinatus repair; SCR, superior capsular reconstruction.
Table 3.
Outcome Measures for the SCR and PR Groups Preoperatively and at Minimum 2-Year Follow-upa
| SCR Group (n = 20) |
PR Group (n = 20) |
P Value | |
|---|---|---|---|
| CS | |||
| Preoperative | 49.7 | 50.7 | .76 |
| Postoperative | 77.1 ± 10.5 | 82.7 ± 8.4 | .07 |
| Age- and sex-adapted CS, % | 85.5 ± 11.4 | 91.4 ± 8.0 | .065 |
| DASH score | 15.6 ± 15.4 | 7.8 ± 11.1 | .074 |
| WORC index | 81.1 ± 17.8 | 90.4 ± 14.0 | .074 |
| AHD, mm | |||
| Preoperative | 7.1 ± 2.1 | 7.9 ± 1.7 | .21 |
| Postoperative | 7.8 ± 2.7 | 9.1 ± 2.2 | .26 |
| P value | .46 | .13 | |
| HHC, mm | |||
| Preoperative | 1.4 ± 4.3 | 1.8 ± 2.3 | .69 |
| Postoperative | 2.3 ± 3.2 | 0.9 ± 2.9 | .35 |
| P value | .56 | .39 |
aValues are expressed as mean ± SD. Bolded P value indicates statistically significant between-group difference (P < .05). AHD, acromiohumeral distance; CS, Constant score; DASH, Disabilities of the Arm, Shoulder and Hand; HHC, humeral head centralization; PR, partial infraspinatus repair; SCR, superior capsular reconstruction; WORC, Western Ontario Rotator Cuff.
At final follow-up, no significant differences were seen between the 2 groups with regard to Constant, age- and sex-adapted Constant, DASH, or WORC index scores (Table 3). As well, no between-group differences were noted in the Constant score subgroups for pain, activities of daily living, range of motion, or strength. The strength measurements were low for both groups (Table 4).
Table 4.
Constant Score Subgroup Outcomesa
| SCR Group (n = 20) |
PR Group (n = 20) |
P Value | |
|---|---|---|---|
| Pain (maximum 15 points) | 13.2 ± 2.3 | 13.8 ± 1.5 | .274 |
| Activities of daily living (maximum 20 points) | 17.2 ± 3.3 | 18.3 ± 2.1 | .199 |
| Range of motion (maximum 40 points) | 36.8 ± 3.6 | 37.0 ± 2.6 | .842 |
| Strength (maximum 25 points) | 10.7 ± 6.3 | 13.3 ± 5.7 | .176 |
aValues are expressed as mean ± SD. PR, partial infraspinatus repair; SCR, superior capsular reconstruction.
There were no cases of progression of osteoarthritis according to radiographic Hamada classification. No significant differences were seen between the groups regarding the AHD or HHC (Table 3).
In the described study period, 21 consecutive patients had SCR surgery; of these one patient reported persistent pain and dysfunction. A postoperative MRI scan demonstrated a clear tear of the patch (Figure 6). The patient underwent revision using latissimus dorsi transfer.
Figure 6.
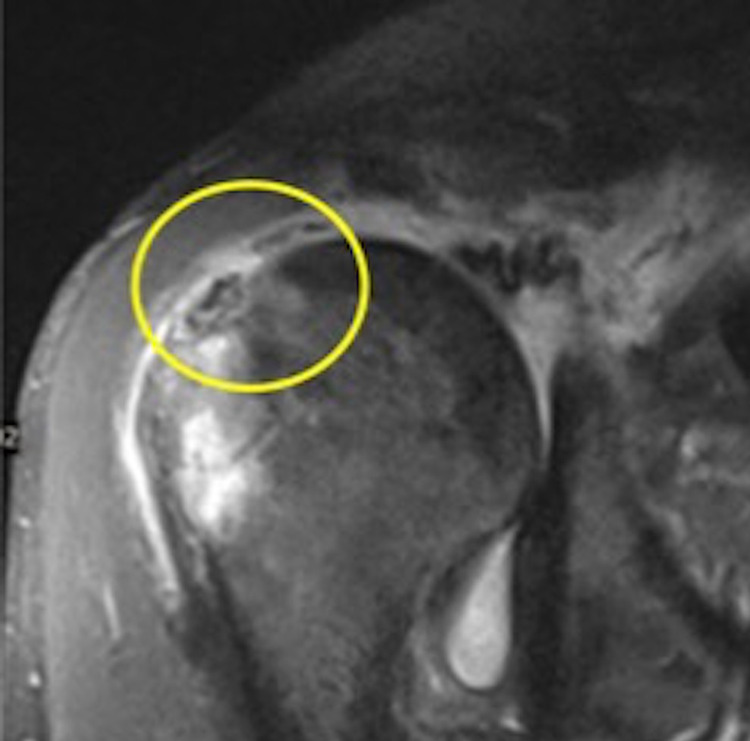
Magnetic resonance imaging scan showing lateral fixation failure after superior capsular reconstruction (yellow circle).
Discussion
The most important finding of this study was that partial infraspinatus repair and SCR both yielded positive outcomes for patients who had irreparable RCTs. However, no significant differences could be seen between these treatment groups according to the evaluated score results at a minimum 2-year follow-up in a matched cohort analysis. Pain, activities of daily living, and range of motion were nearly normal, but patients in both cohorts still had significant residual weakness.
The treatment of massive RCTs poses a challenge to orthopaedic surgeons. Many interventions are possible for patients with symptomatic, massive, irreparable RCTs, including nonoperative management, PR and SCR, implantation of a subacromial spacer, tendon transfers, and reverse shoulder arthroplasty, but there is no clear surgical guideline to treat this population.2,15,23,30–33,41,42,52
Biomechanical studies have shown that the superior capsule acts against superior humeral head migration.33 With the techniques of PR and SCR, either the posterosuperior cuff is partially repaired or an SCR is performed. Both techniques aim to recenter the humeral head in the glenoid fossa during shoulder movements and decrease superior humeral head migration and subsequent impingement. In the present study, the infraspinatus was also partially repaired in the SCR group, which might have increased the benefit achieved by that group.
Concerning the improvement of patient-reported functional outcome, the results of the SCR cohort are in agreement with findings by Mihata et al,32 who reported good clinical outcomes in 24 shoulders in 23 patients. Recent systematic reviews have reported significant improvements in clinical outcome scores and 14.2% graft failure on MRI.17,44 Inadequate AHD (<5 mm) and poor posterior remnant tissue have been proposed as predictive factors of retear.29 In the current study, 3 patients with SCR and 1 patient with PR had an AHD of ≤5 mm. This cutoff value was associated with a worse outcome according to Lee et al, which was confirmed in our groups.
PR has been shown to be a satisfactory therapeutic option for massive posterosuperior cuff tears. The results of this study were similar to those reported in the recent literature in this regard.16,23,40,49 Berth et al4 analyzed 21 patients at 2 years after PR for massive RCTs. The mean Constant score of this group was 58.2 ± 11, thereby lower in comparison with our finding. However, patients with subscapularis tears and complete infraspinatus tears were included in the study of Berth et al. Therefore, currently available data are difficult to compare because of a lack of comparative studies and inconsistent information about tear size and retraction.
In the current study, there were no cases of progression to cuff tear arthropathy in either group within the 2-year follow-up. Limited knowledge is available regarding how long the cuff tear treated using PR or SCR remains stable, at what point it might deteriorate, and whether patients develop cuff tear arthropathy in the long term. Porcellini et al,40 whose study entailed a follow-up of 5 years, reported that only 1 of 67 of patients with PR developed cuff tear arthropathy of Hamada grade 3.
Results beyond 2-year follow-up are currently unknown for SCR. The technique was introduced in 2012 and so far has not been evaluated in any medium- or long-term studies.32,33 Future investigation is required to understand whether this procedure can influence long-term centralization of the humeral head and/or the development of cuff tear arthropathy. Pennington et al37 analyzed pre- and postoperative AHD in a cohort of 88 patients with 1-year follow-up and found that AHD was significantly increased at 1 year; however, there are no data regarding whether this decrease can be maintained over time.
The operative technique used in the current study, which entails tear size reduction in combination with SCR and side-to-side suturing to the remnants of the posterior cuff, has been described before.1,9,22,46,47 Therefore, improvement after SCR may be due to the partial repair of the infraspinatus that is part of the procedure. There is still controversy regarding additional side-to-side suturing to the rotator interval or even the subscapularis tendon.1,9,22,39,48 To avoid the risk of shoulder stiffness, we did not perform any anterior side-to-side sutures in the present population, as recommended.46,47
Few data are available regarding use of acellular xenograft for SCR. The available data, however, show comparable results of SCR using a xenograft versus dermal allografts.14,23,24,37
The current study is the first to compare SCR versus PR in irreparable posterosuperior RCTs. One patient who underwent SCR had a revision using latissimus dorsi transfer because of patch failure. Regarding the PR cohort from which the pairs were matched, 9 of 60 patients underwent revision due to clinical failure by means of arthroscopic debridement, latissimus dorsi transfer, or reverse total shoulder arthroplasty. Although we found no significant differences in outcome scores between the matched groups, the lower revision rate of 4.8% (1/21) in the initially identified SCR cohort in comparison with 15% (9/60) in the initially identified PR cohort may favor increased use of the SCR technique in the future. However, worse prognostic preoperative factors in the unmatched PR cohort may have contributed to the higher revision rate. Further studies comparing these 2 cohorts with a larger sample size may demonstrate clinical and radiographic differences.
The strengths of this study are the high-quality comparison due to match-paired cohort groups and the follow-up of at least 2 years for a relatively new technique. The study has several limitations. First, the differences in functional outcome scores and graft materials used in this study versus other studies make it difficult to compare outcomes directly. Second, postoperative MRI was not routinely performed, and preoperative DASH and WORC index scores were not available for comparison. Third, because the PR group was drawn from a historic patient group, the follow-up time was longer for this group than for the SCR group. Fourth, the 2 cohorts underwent surgery by different surgeons. However, within each group, a single surgeon performed the operations, and both surgeons had trained in the same center and had a similar level of experience.
Conclusion
For irreparable posterosuperior RCTs, both SCR and PR techniques resulted in significant improvements in clinical outcomes after a minimum of 2 years of follow-up, with no significant differences in evaluated outcomes between the 2 techniques. Regarding long-term results including whether these techniques can prevent or delay decentralization of the humeral head and progression to RCT arthropathy, further studies are needed.
Acknowledgment
The authors thank all of the contributing patients.
Footnotes
Final revision submitted August 18, 2020; accepted September 4, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: S.G. and M.K. are medical advisors for Arthrex GmbH. A.V. is a consultant for DJO Global. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Regensburg (ref No. 17-657-101).
References
- 1. Adams CR, Denard PJ, Brady PC, Hartzler RU, Burkhart SS. The arthroscopic superior capsular reconstruction. Am J Orthop (Belle Mead NJ). 2016;45(5):320–324. [PubMed] [Google Scholar]
- 2. Anley CM, Chan SK, Snow M. Arthroscopic treatment options for irreparable rotator cuff tears of the shoulder. World J Orthop. 2014;5(5):557–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bayne O, Bateman J. Long-term results of surgical repair of full-thickness rotator cuff tears. In: Bateman J, Welsh R, eds. Surgery of the Shoulder. CV Mosby; 1984;167–171. [Google Scholar]
- 4. Berth A, Neumann W, Awiszus F, Pap G. Massive rotator cuff tears: functional outcome after debridement or arthroscopic partial repair. J Orthop Traumatol. 2010;11(1):13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Boutsiadis A, Chen S, Jiang C, et al. Long head of the biceps as a suitable available local tissue autograft for superior capsular reconstruction: “the Chinese way.” Arthrosc Tech. 2017;6(5):e1559–e1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Burkhart SS. Arthroscopic treatment of massive rotator cuff tears. Clin Orthop Relat Res. 2001;390:107–118. [DOI] [PubMed] [Google Scholar]
- 7. Burkhart SS. Partial repair of massive rotator cuff tears: the evolution of a concept. Orthop Clin North Am. 1997;28(1):125–132. [DOI] [PubMed] [Google Scholar]
- 8. Burkhart SS. Reconciling the paradox of rotator cuff repair versus debridement: a unified biomechanical rationale for the treatment of rotator cuff tears. Arthroscopy. 1994;10(1):4–19. [DOI] [PubMed] [Google Scholar]
- 9. Burkhart SS, Denard PJ, Adams CR, Brady PC, Hartzler RU. Arthroscopic superior capsular reconstruction for massive irreparable rotator cuff repair. Arthrosc Tech. 2016;5(6):e1407–e1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Burkhart SS, Hartzler RU. Superior capsular reconstruction reverses profound pseudoparalysis in patients with irreparable rotator cuff tears and minimal or no glenohumeral arthritis. Arthroscopy. 2019;35(1):22–28. [DOI] [PubMed] [Google Scholar]
- 11. Burkhart SS, Nottage WM, Ogilvie-Harris DJ, Kohn HS, Pachelli A. Partial repair of irreparable rotator cuff tears. Arthroscopy. 1994;10(4):363–370. [DOI] [PubMed] [Google Scholar]
- 12. Burkhart SS, Pranckun JJ, Hartzler RU. Superior capsular reconstruction for the operatively irreparable rotator cuff tear: clinical outcomes are maintained 2 years after surgery. Arthroscopy. 2020;36(2):373–380. [DOI] [PubMed] [Google Scholar]
- 13. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 14. Denard PJ, Brady PC, Adams CR, Tokish JM, Burkhart SS. Preliminary results of arthroscopic superior capsule reconstruction with dermal allograft. Arthroscopy. 2018;34(1):93–99. [DOI] [PubMed] [Google Scholar]
- 15. Deranlot J, Herisson O, Nourissat G, et al. Arthroscopic subacromial spacer implantation in patients with massive irreparable rotator cuff tears: clinical and radiographic results of 39 retrospectives cases. Arthroscopy. 2017;33(9):1639–1644. [DOI] [PubMed] [Google Scholar]
- 16. Duralde XA, Bair B. Massive rotator cuff tears: the result of partial rotator cuff repair. J Shoulder Elbow Surg. 2005;14(2):121–127. [DOI] [PubMed] [Google Scholar]
- 17. Ekhtiari S, Adili AF, Memon M, et al. Sources, quality, and reported outcomes of superior capsular reconstruction: a systematic review. Curr Rev Musculoskelet Med. 2019;12(2):173–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Flatow EL, Soslowsky LJ, Ticker JB, et al. Excursion of the rotator cuff under the acromion: patterns of subacromial contact. Am J Sports Med. 1994;22(6):779–788. [DOI] [PubMed] [Google Scholar]
- 19. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures: pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83. [PubMed] [Google Scholar]
- 20. Gummesson C, Atroshi I, Ekdahl C. The Disabilities of the Arm, Shoulder and Hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gupta AK, Hug K, Boggess B, Gavigan M, Toth AP. Massive or 2-tendon rotator cuff tears in active patients with minimal glenohumeral arthritis: clinical and radiographic outcomes of reconstruction using dermal tissue matrix xenograft. Am J Sports Med. 2013;41(4):872–879. [DOI] [PubMed] [Google Scholar]
- 22. Hirahara AM, Adams CR. Arthroscopic superior capsular reconstruction for treatment of massive irreparable rotator cuff tears. Arthrosc Tech. 2015;4(6):e637–e641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hirahara AM, Andersen WJ, Panero AJ. Superior capsular reconstruction: clinical outcomes after minimum 2-year follow-up. Am J Orthop (Belle Mead NJ). 2017;46(6):266–278. [PubMed] [Google Scholar]
- 24. Kalina R, Neoral P, Holibka R, Gallo J. Arthroscopic superior capsule reconstruction using the DX reinforcement matrix in patients with irreparable rotator cuff tears—pilot data. Article in Czech. Acta Chir Orthop Traumatol Cech. 2019;86(4):264–270. [PubMed] [Google Scholar]
- 25. Katolik LI, Romeo AA, Cole BJ, et al. Normalization of the Constant score. J Shoulder Elbow Surg. 2005;14(3):279–285. [DOI] [PubMed] [Google Scholar]
- 26. Kim SJ, Lee IS, Kim SH, Lee WY, Chun YM. Arthroscopic partial repair of irreparable large to massive rotator cuff tears. Arthroscopy. 2012;28(6):761–768. [DOI] [PubMed] [Google Scholar]
- 27. Kukkonen J, Kauko T, Vahlberg T, Joukainen A, Aarimaa V. Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. J Shoulder Elbow Surg. 2013;22(12):1650–1655. [DOI] [PubMed] [Google Scholar]
- 28. Lacheta L, Horan MP, Schairer WW, et al. Clinical and imaging outcomes after arthroscopic superior capsule reconstruction with human dermal allograft for irreparable posterosuperior rotator cuff tears: a minimum two year follow up. Arthroscopy. 2020;36(4):1011–1019. [DOI] [PubMed] [Google Scholar]
- 29. Lee SJ, Min YK. Can inadequate acromiohumeral distance improvement and poor posterior remnant tissue be the predictive factors of re-tear? Preliminary outcomes of arthroscopic superior capsular reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(7):2205–2213. [DOI] [PubMed] [Google Scholar]
- 30. Malahias MA, Brilakis E, Avramidis G, Antonogiannakis E. Satisfactory mid-term outcome of subacromial balloon spacer for the treatment of irreparable rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2019;27(12):3890–3896. [DOI] [PubMed] [Google Scholar]
- 31. Mihata T, Lee TQ, Hasegawa A, et al. Superior capsule reconstruction for reinforcement of arthroscopic rotator cuff repair improves cuff integrity. Am J Sports Med. 2019;47(2):379–388. [DOI] [PubMed] [Google Scholar]
- 32. Mihata T, Lee TQ, Watanabe C, et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29(3):459–470. [DOI] [PubMed] [Google Scholar]
- 33. Mihata T, McGarry MH, Kahn T, et al. Biomechanical role of capsular continuity in superior capsule reconstruction for irreparable tears of the supraspinatus tendon. Am J Sports Med. 2016;44(6):1423–1430. [DOI] [PubMed] [Google Scholar]
- 34. Nam D, Maak TG, Raphael BS, et al. Rotator cuff tear arthropathy: evaluation, diagnosis, and treatment: AAOS exhibit selection. J Bone Joint Surg Am. 2012;94(6):e34. [DOI] [PubMed] [Google Scholar]
- 35. Nove-Josserand L, Levigne C, Noel E, Walch G. The acromio-humeral interval: a study of the factors influencing its height. Article in French. Rev Chir Orthop Reparatrice Appar Mot. 1996;82(5):379–385. [PubMed] [Google Scholar]
- 36. Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990;254:81–86. [PubMed] [Google Scholar]
- 37. Pennington WT, Bartz BA, Pauli JM, Walker CE, Schmidt W. Arthroscopic superior capsular reconstruction with acellular dermal allograft for the treatment of massive irreparable rotator cuff tears: short-term clinical outcomes and the radiographic parameter of superior capsular distance. Arthroscopy. 2018;34(6):1764–1773. [DOI] [PubMed] [Google Scholar]
- 38. Petersson CJ, Redlund-Johnell I. The subacromial space in normal shoulder radiographs. Acta Orthop Scand. 1984;55(1):57–58. [DOI] [PubMed] [Google Scholar]
- 39. Petri M, Greenspoon JA, Millett PJ. Arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthrosc Tech. 2015;4(6):e751–e755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Porcellini G, Castagna A, Cesari E, et al. Partial repair of irreparable supraspinatus tendon tears: clinical and radiographic evaluations at long-term follow-up. J Shoulder Elbow Surg. 2011;20(7):1170–1177. [DOI] [PubMed] [Google Scholar]
- 41. Ricci M, Vecchini E, Bonfante E, et al. A clinical and radiological study of biodegradable subacromial spacer in the treatment of massive irreparable rotator cuff tears. Acta Biomed. 2017;88(4)(suppl):75–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Senekovic V, Poberaj B, Kovacic L, et al. The biodegradable spacer as a novel treatment modality for massive rotator cuff tears: a prospective study with 5-year follow-up. Arch Orthop Trauma Surg. 2017;137(1):95–103. [DOI] [PubMed] [Google Scholar]
- 43. Smolen D, Haffner N, Mittermayr R, et al. Application of a new polyester patch in arthroscopic massive rotator cuff repair–a prospective cohort study. J Shoulder Elbow Surg. 2020;29(1):e11–e21. [DOI] [PubMed] [Google Scholar]
- 44. Sochacki KR, McCulloch PC, Lintner DM, Harris JD. Superior capsular reconstruction for massive rotator cuff tear leads to significant improvement in range of motion and clinical outcomes: a systematic review. Arthroscopy. 2019;35(4):1269–1277. [DOI] [PubMed] [Google Scholar]
- 45. Su WR, Budoff JE, Luo ZP. The effect of anterosuperior rotator cuff tears on glenohumeral translation. Arthroscopy. 2009;25(3):282–289. [DOI] [PubMed] [Google Scholar]
- 46. Sutter EG, Godin JA, Garrigues GE. All-arthroscopic superior shoulder capsule reconstruction with partial rotator cuff repair. Orthopedics. 2017;40(4):e735–e738. [DOI] [PubMed] [Google Scholar]
- 47. Thorsness R, Romeo A. Massive rotator cuff tears: trends in surgical management. Orthopedics. 2016;39(3):145–151. [DOI] [PubMed] [Google Scholar]
- 48. Tokish JM, Beicker C. Superior capsule reconstruction technique using an acellular dermal allograft. Arthrosc Tech. 2015;4(6):e833–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wellmann M, Lichtenberg S, da Silva G, Magosch P, Habermeyer P. Results of arthroscopic partial repair of large retracted rotator cuff tears. Arthroscopy. 2013;29(8):1275–1282. [DOI] [PubMed] [Google Scholar]
- 50. Wessel RN, Lim TE, van Mameren H, de Bie RA. Validation of the Western Ontario Rotator Cuff index in patients with arthroscopic rotator cuff repair: a study protocol. BMC Musculoskelet Disord. 2011;12:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Woodmass JM, Wagner ER, Borque KA, et al. Superior capsule reconstruction using dermal allograft: early outcomes and survival. J Shoulder Elbow Surg. 2019;28(6)(suppl):S100–S109. [DOI] [PubMed] [Google Scholar]
- 52. Yallapragada RK, Apostolopoulos A, Katsougrakis I, Selvan TP. The use of a subacromial spacer-inspace balloon in managing patients with irreparable rotator cuff tears. J Orthop. 2018;15(3):862–868. [DOI] [PMC free article] [PubMed] [Google Scholar]