Abstract
Purpose
This study aimed to present our experience with failures in C-TDR and revision surgery outcomes.
Materials and Methods
We retrospectively examined patients who underwent revision surgery due to the failure of C-TDR between May 2005 to March 2019. Thirteen patients (8 males and 5 females) were included in this study. The mean age was 46.1 years (range: 22–61 years), and the average follow-up period was 19.5 months (range: 12–64 months). The outcome measures of pre- and post-operative neck and arm pain using a visual analogue scale (VAS) and functional impairment were assessed using a modified Japanese Orthopedic Association (JOA) scale and the Neck Disability Index (NDI).
Results
The main complaints of patients were posterior neck pain (77%), radiculopathy (62%), and/or myelopathy (62%). The causes of failure of C-TDR were improper indications for the procedure, osteolysis and mobile implant use, inappropriate techniques, and postoperative infection. The most common surgical level was C5–6, followed by C4–5. After revision surgery, the neck and arm pain VAS (preoperative vs. postoperative: 5.46 vs. 1.31; 4.86 vs. 1.08), a modified JOA scale (14.46 vs. 16.69), and the NDI (29.77 vs. 9.31) scores were much improved.
Conclusion
C-TDR is good surgical option. However, it is very important to adhere to strict surgical indications and contraindications to avoid failure of C-TDR. The results of reoperations were good regardless of the approach. Therefore, various reoperation options could be considered in patients with failed C-TDR.
Keywords: Artificial disc replacement, cervical, diskectomy, fusion, revision surgery
INTRODUCTION
Anterior cervical discectomy and fusion (ACDF) is an effective intervention for treating degenerative cervical spine disease.1 However, some problems may arise following ACDF. The procedure limits segmental motion at the fusion level and consequently results in subjective patient discomfort, increased biomechanical stresses, and accelerated degeneration of adjacent spinal motion segments.2,3,4 Total disc replacement of the cervical spine (C-TDR) has been developed to maintain an optimum range of motion in the operated segment to avoid the development of adjacent segment degeneration (ASD); equivalent outcomes may be achieved with C-TDR in terms of reduction in pain, improved neurological deficit, and earlier return-to-work times compared to the outcomes of ACDF.5,6,7 In addition, C-TDR prevents pseudoarthrosis or graft-related complications and adverse side effects caused by cervical fusion.2,8 The indications for and contraindications to C-TDR are shown in Table 1.9,10,11,12
Table 1. Indications for and Contraindications to Cervical Total Disc Replacement.
| Indications | |
| Symptomatic cervical disc disease at one or two vertebral levels between C3 and T1 confirmed by imaging (MRI, CT, or myelogram) showing herniated nucleus pulposus, spondylosis, or loss of disc height of at least 4 mm | |
| Failed ≥6 weeks of conservative management | |
| Between 20 and 70 years of age | |
| No contraindication | |
| Contraindications | |
| ≥3 vertebral levels requiring treatment | |
| Cervical fusion adjacent to tde level to be treated | |
| Cervical instability (translation >3 mm and/or >11 rotational difference to tdat or eitder adjacent level) | |
| Facet joint degeneration | |
| Severe spondylosis (bridging osteophytes, disc height loss >50%, and absence of motion <2°) | |
| Known allergy to implant materials (titanium, polyetdylene, cobalt, chromium, molybdenum) | |
| Posttraumatic vertebral body deficiency/deformity | |
| Prior surgery at tde treated level | |
| Neck or arm pain of unknown etiology | |
| Axial neck pain as tde solitary presenting symptom | |
| Osteoporosis/osteopenia | |
| Active malignancy | |
| Any patient witd history of invasive malignancy unless treated and asymptomatic for at least 5 years | |
| Systemic disease (AIDS, HIV, hepatitis B or C, and insulin-dependent diabetes) | |
| Metabolic bone disease (i.e., osteomalacia, osteogenesis imperfect, Paget's disease) | |
| Active local/systemic infection | |
| Presently on medications tdat can interfere witd bone/soft tissue healing (i.e., steroids) | |
| Autoimmune spondyloartdropatdies (i.e., rheumatoid artdritis) | |
| Pregnant or trying to become pregnant in tde next 3 years | |
AIDS, autoimmune deficiency syndrome; CT, computed tomography; HIV, human immunodeficiency virus; MRI, magnetic resonance imaging.
However, C-TDR may also lead to complications; several patients have required reoperation due to the persistence or recurrence of symptoms and complications.13 Some studies have reported that C-TDR had a higher reoperation rate compared to ACDF, which is unfortunate since reoperation is technically demanding regardless of the type and design used in the original C-TDR procedure.12,13,14,15 The reasons for reoperation include implant failure (typically due to a broken polyurethane sheath), inappropriate intraoperative techniques, subsidence with osteolysis, postoperative infection, wear debris and tissue reaction, and improper indications.12,15,16,17,18,19,20
Therefore, it is important to consider the indications for reoperation and how to improve the patients' radiologic and clinical outcomes. In this study, we investigated C-TDR failures and reoperations at our institute.
MATERIALS AND METHODS
Study design
We retrospectively reviewed the records of 111 patients at our hospital who underwent C-TDR or a hybrid procedure (C-TDR with ACDF) as well as those of patients who experienced postoperative complications after undergoing C-TDR at other medical centers from May 2005 to April 2019. We selected patients who underwent reoperation due to the failure of C-TDR. A total of 13 patients (8 males and 5 females) were analyzed. Among them, three had undergone initial C-TDR surgery at our hospital, indicating a 2.7% (3/111) prevalence. The other 10 patients in our sample were referred from outside clinics after they experienced postoperative complications. The mean age was 46.1 years (range: 22–61 years), and the average follow-up period was 19.5 months (range: 12–64 months). All 13 patients underwent radiography, computed tomography (CT) scans, and magnetic resonance imaging (MRI) of the cervical spine.
In terms of the location of surgery, nine patients underwent single-level C-TDR (1 at C4–5 and 8 at C5–6), two patients underwent hybrid surgery (C-TDR at C4–5 and ACDF at C6–7 in one patient and C-TDR at C4–5 and ACDF at C5–6 in the other), and two patients underwent a two-level C-TDR (one at C3–4 and C6–7 and the other at C5–7). Thirteen patients underwent surgery, and 15 total levels were included.
Failure of primary C-TDR was defined as persistence or recurrence of radiculopathy and/or myelopathy due to lingering or new pathology at the same level as the operation. Radiographically, problems with implants, such as broken polyurethane sheath or any movement of the devices from their initial location, were noted.
During clinical assessment, the patients reported pre- and postoperative 3, 6, 12-month neck and arm pain using a visual analogue scale (VAS) scored from 0–10 and functional impairment, which was assessed using a modified Japanese Orthopedic Association (JOA) scale and the Neck Disability Index (NDI).
The patients were analyzed to identify the type of implants, previous surgery levels, length of time from initial procedure to reoperation, surgical methods used during reoperation, neck and arm VAS, and modified JOA scale and NDI scores. The clinical data of patients including age, sex, medical history, radiographs, surgical methods, type of implants, and clinical outcomes were analyzed. We obtained the approval for this study from our Institutional Review Board (number: 3-2019-0431).
RESULTS
Patient characteristics
The main complaints of patients were posterior neck pain, radiculopathy, and/or myelopathy. Ten patients (77%) had posterior neck pain, 8 patients (62%) complained of radiculopathy, and other 8 patients (62%) reported myelopathy with motor weakness. All patients were followed-up for at least 12 months postoperatively (Table 2).
Table 2. Demographics and Preoperative Data of Patients.
| Case | Age | Sex | CC | Device | Surgical level | Follow-up (months) | Previous surgery |
|---|---|---|---|---|---|---|---|
| 1 | 60 | M | MP | Prodisc | C4–5 | 12 | Hybrid |
| PNP | |||||||
| 2 | 27 | M | PNP | Prestige | C4–5 | 12 | TDR |
| 3 | 35 | F | ShP | Prestige | C4–5 | 25 | Hybrid |
| AP | |||||||
| PNP | |||||||
| MP | |||||||
| 4 | 61 | F | ShP | Prestige | C5–6 | 12 | TDR* |
| AP | Prestige | C6–7 | |||||
| 5 | 53 | M | ShP | Mobi-C | C5–6 | 21 | TDR |
| AP | |||||||
| 6 | 61 | M | MP | Prestige | C3–4 | 64 | TDR* |
| PNP | Prestige | C6–7 | |||||
| 7 | 22 | M | MP | Mobi-C | C5–6 | 12 | TDR |
| PNP | |||||||
| 8 | 52 | M | PNP | Bryan | C5–6 | 22 | TDR |
| MP | |||||||
| 9 | 47 | F | PNP | Mobi-C | C5–6 | 26 | TDR |
| AP | |||||||
| 10 | 40 | M | AP | Prodisc | C5–6 | 12 | TDR |
| 11 | 56 | M | MP | Mobi-C | C5–6 | 12 | TDR |
| PNP | |||||||
| ShP | |||||||
| 12 | 44 | F | PNP | Mobi-C | C5–6 | 12 | TDR |
| AP | |||||||
| MP | |||||||
| 13 | 41 | F | PNP | Prodisc | C5–6 | 12 | TDR |
| AP | |||||||
| MP |
AP, arm pain; CC, chief complaint; ShP, shoulder pain; MP, myelopathy; Mo, months; TDR, total disc replacement.
*The patient who underwent two-level TDR.
The causes for failure of the initial C-TDR were as follows: 6 patients (46%) had improper indications for surgery, including severe spondylosis or cervical instability; four patients demonstrated osteolysis and implant subsidence; two patients experienced postoperative infection; and one patient's failure resulted from inappropriate technique selection and unstable implants. Among the devices, six were manufactured by Prestige LP (Medtronic Sofamor Danek, Memphis, TN, USA), five were obtained from Mobi-C (LDR Spine, Austin, TX, USA), three were purchased from ProDisc-C (Synthes, West Chester, PA, USA), and one came from Bryan (Medtronic Sofamor Danek).
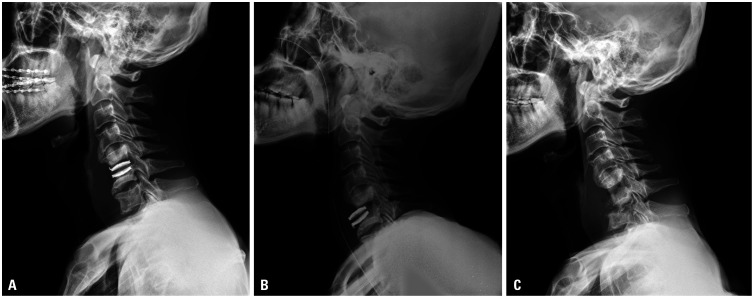
Of the seven patients with subsidence (54%), two had involvement at C4–5, and five had signs at C5–6. In these seven patients, three of the implanted devices were from Mobi-C, two were from Prestige LP, one was from Bryan, and one was from ProDisc-C. Four patients were affected by anterior migration of the superior portion of the implant, while two others experienced posterior migration of the superior portion and anterior migration of the inferior portion. The remaining one patient had anterior migration of both superior and inferior portions until the implant was no longer visible (Fig. 1).
Fig. 1. Missing Bryan device. (A) Postoperative lateral radiograph of the cervical spine showed anterior discectomy and implantation of artificial disc at C5–6. (B) Lateral radiographs after 6 months of follow-up showed subsidence of artificial disc. (C) Lateral radiographs at 1 year postoperatively showed disappearance of artificial disc.
Regarding the involved surgical levels, nine patients had implants at C5–6, three had implants at C4–5, two had implants at C6–7, and one had implants at C3–4. Two of these patients underwent hybrid surgery during primary operation (C-TDR at C4–5 and ACDF at C6–7 in one patient and C-TDR at C4–5 along with ACDF at C5–6 in the other patient). Two other patients underwent multilevel C-TDR procedures (C-TDR at C5–7 in one patient and C-TDR at both C3–4 and C6–7 in the other). The mean time from initial surgery until reoperation was 52.8 months (range: 0–126 months). The patients were divided into early and late reoperation groups based on a cutoff of 6 months after initial surgery. There were two patients in the early reoperation group; one of them was technically a failure, and the other showed improper indication of severe spondylosis. Both of these early group patients underwent reoperation with artificial disc removal and ACDF. In the late reoperation group, the causes of failure were improper surgical indications, osteolysis with subsidence, and spondylitis. Four of these patients (40%) underwent a posterior approach due to the presence of myelopathy (Table 3).
Table 3. Causes for Failure of Total Disc Replacement and Treatment.
| Case | Cause | Mobile direction | Duration (months) | Approach | Device removal | Reoperation |
|---|---|---|---|---|---|---|
| 1 | Improper indication (spondylosis), ASD | - | 89 | Post. | - | Laminectomy and LMSF |
| 2 | Inappropriate technique, mobile device | Sup-Ant | 0 | Ant. | + | ACDF (auto chip bone) |
| 3 | Osteolysis, mobile device | Sup-Ant | 15 | Ant. | + | ACDF (auto chip bone) |
| 4 | Improper indication (spinal instability) | - | 18 | Ant. | + | ACDF (allograft bone block) |
| 5 | Improper indication (spondylosis) | - | 5 | Ant. | + | ACDF (allograft bone block) |
| 6 | Improper indication (spinal instability) | - | 16 | Post. | - | Laminoplasty |
| 7 | Osteolysis, mobile device | Sup-Post | 60 | Ant. | + | ACDF (AIBG) |
| 8 | Postoperative infection, mobile device | Sup-Ant | 126 | Post. | * | Laminectomy and LMSF |
| Inf-Ant | ||||||
| 9 | Postoperative infection, mobile device | Sup-Post | 108 | Ant. | + | ACDF (AIBG) |
| Inf-Post | ||||||
| 10 | Improper indication (spondylosis) ASD | - | 101 | Ant. | + | ACDF (allograft bone block) |
| 11 | Osteolysis, mobile device | Sup-Post | 78 | Ant. | + | ACDF (allograft bone block) |
| Inf-Post | ||||||
| 12 | Improper indication (spondylosis) | - | 50 | Post. | - | Laminoplasty |
| 13 | Osteolysis, mobile device | Sup-Ant | 21 | Ant. | + | ACDF (AIBG) |
ASD, adjacent segment degeneration; Ant, anterior; Post, posterior; Sup, superior; Inf, inferior; LMSF, lateral mass screw fixation; ACDF, anterior cervical discectomy and fusion; AIBG, autogenous-tricortical iliac bone graft.
*The device was spontaneously disappeared steadily.
There was no difference in our approach to surgery in any patient based on the duration to reoperation. Instead, we chose either an anterior or a posterior approach, depending on whether the patient's symptoms were radiculopathy or myelopathy, respectively. However, the longer the reoperation period, the more difficult it was to remove the device, although the time length did not affect the choice of approach for reoperation.
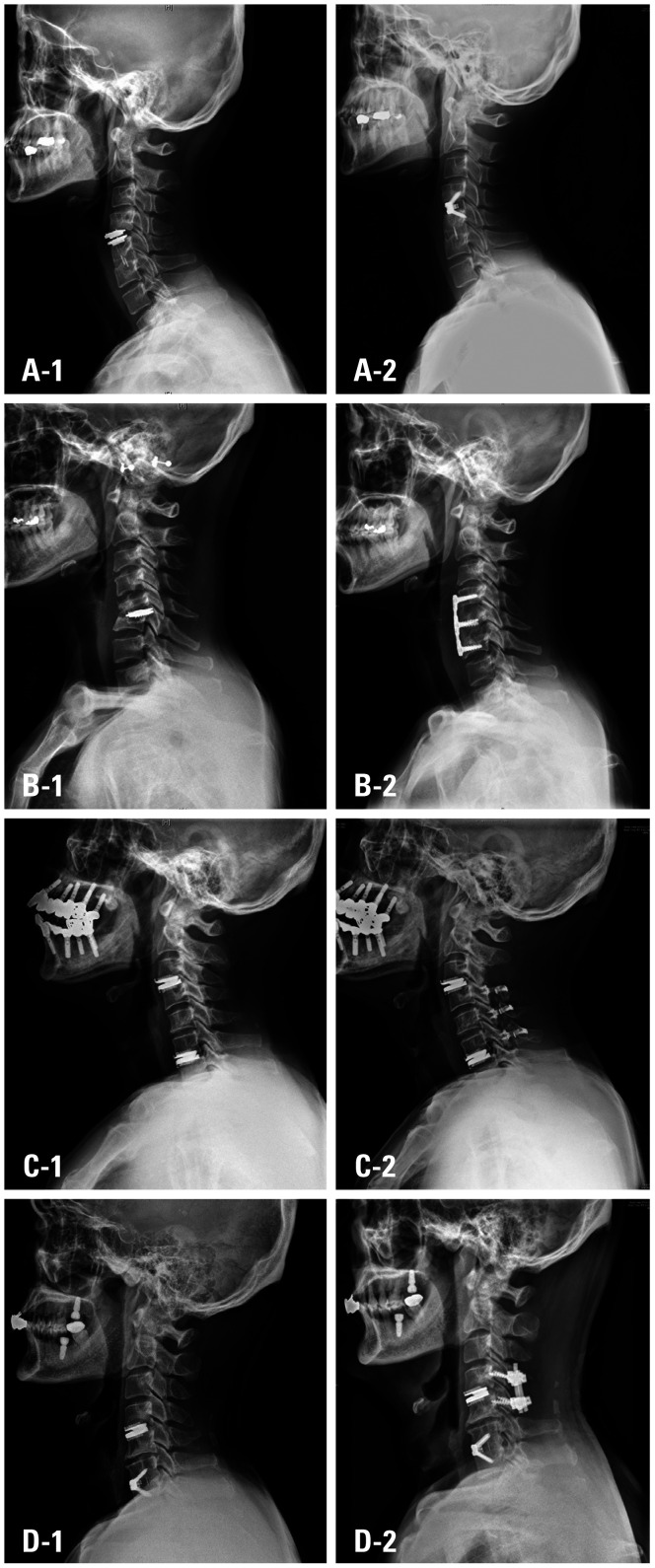
Nine patients underwent an anterior approach, and the remaining four were addressed with a posterior approach. Nine of the 13 patients (69%) underwent removal of the C-TDR device (four from Mobi-C, three from Prestige LP, and two from ProDisc-C), and one patient with a Bryan device experienced spontaneous disappearance (Fig. 1). Five patients underwent a one-level discectomy and fusion using a plate. Two other patients had a two-level discectomy and plate fusion. The types of bone grafts used in these patients were four freeze-dried allograft bone blocks, three autogenous tricortical iliac bone grafts, and two cages plus autogenous bone chips. Of the four patients being revised with a posterior approach, two underwent laminectomy and lateral mass screw fixation, and the other two underwent laminoplasty (Fig. 2, Table 3).
Fig. 2. Postoperative radiographs of patients underwent revision surgery. (A–1) Last follow-up lateral radiograph of the patient who underwent hybrid surgery with artificial disc at C4–5 and interbody fusion at C5–6. (A–2) Postoperative lateral radiograph of the patient who underwent removal of the implant and one-level discectomy and fusion using a cage plus autogenous bone chips at C4–5. (B–1) Last follow-up lateral radiograph of the patient who underwent artificial disc replacement at C5–6. (B–2) Postoperative lateral radiograph of the patient who underwent removal of the implant and two-level discectomy and fusion using freeze-dried allograft bone blocks with plate and screws at C4–5–6. (C–1) Last follow-up lateral radiograph of the patient who underwent multi-level artificial disc replacement at C3–4 and C6–7. (C–2) Postoperative lateral radiograph of the patient who underwent C3 laminectomy and open-door laminoplasty at C4–5–6 without the removal of previous implant. (D–1) Last follow-up lateral radiograph of the patient who underwent hybrid surgery with artificial disc at C4–5 and interbody fusion at C6–7. (D–2) Postoperative lateral radiograph of the patient underwent laminectomy and lateral mass screw fixation at C4–5 without the removal of previous implant.
Our clinical assessment compared patients' VAS, modified JOA, and NDI scores before and after surgery. The average change in VAS score for neck pain was −4.15, while that for arm pain was −3.77. Regarding functional improvement, the average change in modified JOA score was 2.23, while that for NDI was −20.46. Although no statistical significance was observed, both pain and functional disability resulted in postoperative improvement (Table 4).
Table 4. Clinical Assessment of the Patients Pain and Functional Disability.
| Case | Neck pain VAS | Arm pain VAS | ||||||
|---|---|---|---|---|---|---|---|---|
| Pre-operative | Post-operative 3 months | Post-operative 6 months | Post-operative 12 months | Pre-operative | Post-operative 3 months | Post-operative 6 months | Post-operative 12 months | |
| 5.46±1.51 | 2.31±1.49 | 1.38±1.61 | 1.31±1.38 | 4.85±1.63 | 2.08±1.26 | 1.54±1.27 | 1.08±1.26 | |
| 1 | 8 | 2 | 0 | 0 | 3 | 0 | 0 | 0 |
| 2 | 5 | 2 | 0 | 0 | 3 | 0 | 0 | 0 |
| 3 | 5 | 2 | 0 | 2 | 5 | 4 | 3 | 3 |
| 4 | 5 | 0 | 0 | 0 | 7 | 2 | 0 | 0 |
| 5 | 4 | 2 | 0 | 0 | 8 | 2 | 2 | 0 |
| 6 | 7 | 5 | 5 | 4 | 5 | 3 | 1 | 2 |
| 7 | 6 | 3 | 1 | 2 | 3 | 2 | 3 | 2 |
| 8 | 7 | 3 | 2 | 2 | 3 | 2 | 0 | 0 |
| 9 | 5 | 2 | 2 | 0 | 5 | 4 | 1 | 0 |
| 10 | 2 | 0 | 0 | 0 | 4 | 2 | 2 | 0 |
| 11 | 6 | 4 | 3 | 2 | 6 | 2 | 3 | 2 |
| 12 | 6 | 4 | 3 | 3 | 6 | 3 | 3 | 3 |
| 13 | 5 | 1 | 2 | 2 | 5 | 1 | 2 | 2 |
VAS, visual analogue scale; mJOA, modified Japanese Orthopaedic Association; NDI, Neck Disability Index.
DISCUSSION
The C-TDR technique showed at least the same or better results than ACDF in terms of ASD occurrence, pseudoarthrosis, and mechanical problems.2,8 In addition, this procedure demonstrated excellent clinical results similar to those of ACDF.
Patients who undergo C-TDR also may experience negative outcomes of implant failure, such as broken polyurethane sheath, subsidence with osteolysis, wear debris, and tissue reaction. Moreover, improper indications, inappropriate techniques, and movement due to the choice of device type can also lead to problems.12,15,16,17,18,19,20
A total of 13 patients (eight males and five females) underwent reoperation after C-TDR due to complications. Three of these patients underwent initial C-TDR at our hospital, a prevalence of 2.7% (3/111). Although the rate of reoperation due to complications was 2.7%, a detailed analysis was required to determine how to prevent and treat these outcomes.
Park, et al.13 found that the most common cause for failure of C-TDR was poor patient selection, followed by insufficient decompression, malpositioning, subsidence, osteolysis, and postoperative infection. In our study, the causes for failure of C-TDR procedures were as follows: improper indications in 6 patients (46%), including four for severe spondylosis and two for cervical instability. In addition, we found osteolysis with implant subsidence in four patients, postoperative infections in two patients, and inappropriate technique and unstable implant in one patient. The results of the current study were similar to those reported by Park, et al.13 Therefore, patient selection is the most important factor for a successful implantation.
The surgical indications and contraindications for C-TDR are shown in Table 1. In our study, six patients experienced failure due to improper indication; four had severe cervical spondylosis with osteophyte and disc height loss, and two suffered from cervical instability with spondylolisthesis. In the cases with improper indications, almost all patients complained of posterior neck pain and radiculopathy at the surgical levels. Three of them had myelopathy and underwent reoperation using a posterior approach. These patients should have initially been referred for fusion surgery with foraminotomy instead of C-TDR. Therefore, in order to properly perform C-TDR, clinicians must adhere to strict indications and technical care.
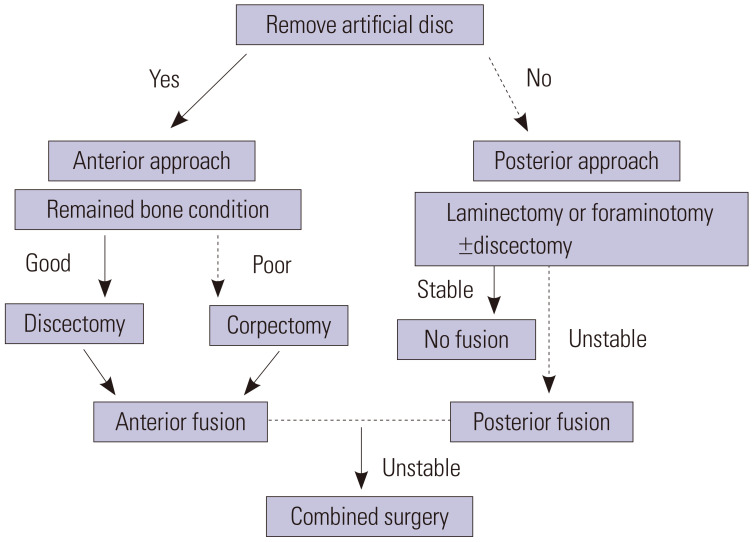
In our surgical strategy, the artificial disc was firmly fixed, and in the case of non-complication due to the implant, there was no reason to remove the implant, so we decided to use the posterior approach. In particular, in case of severe myelopathy, laminectomy with lateral mass screw fixation or laminoplasty was performed. In our case, each of the two cases was performed. In this part, surgeon difference clearly existed; and principally, it had a policy that enforced fusion, but in the other cases, it seems that the surgeon's will to maintain motion was reflected.
In the case of osteolysis or mobile implants, implant removal is required. In addition, when implant-related complications, such as sheath breakage occur, implant removal is also necessary. In addition, ACDF or corpectomy and fusion should be considered when the implant is removed. Reoperations were performed through the opposite side of previous surgical site, due to postoperative adhesions. Of course, the cases of reoperation due to early complications, such as cases 2 and 5, were performed with an existing wound. The implant was exposed, and the scar tissue and ossification were carefully removed from the endplates using high-speed drill, chisel, dissector, and forceps. Usually, the implant was removed in two pieces. When endplates were freed from bony spurs and granulation tissue, interbody fusion was considered.21 At this time, auto-iliac bone was used for infection such as spondylitis, and cervical interbody fusion cage was used for previous surgery at the peripheral level. Other than infection, allobone was used. However, osteolysis was very severe in our case, and although corpectomy could have been a good surgical option, we chose posterior fusion. Fortunaely, the patient is constantly on follow-up without any special problems.
When we divided the patients into early and late reoperation groups based on reoperation within 30 days after initial surgery, only one patient in the early reoperation group technically experienced failure. In failure cases, it is likely that the objective disc was not properly seated during surgery; in our case, the problem occurred as the upper part of the implant migrated to the anterior part, resulting in the need for reoperation.
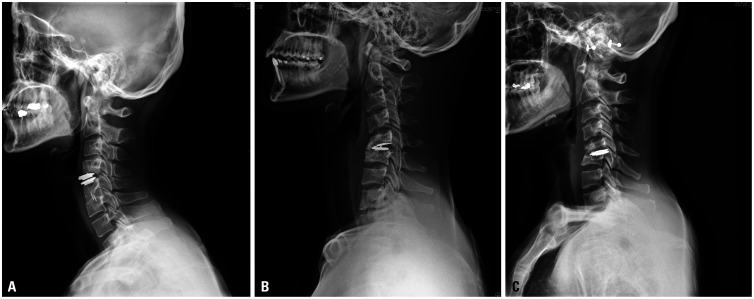
C-TDR failures are most likely to occur at levels C4–5 and C5–6,15 and we observed the same trend in our study. In their in vivo study, Skeppholm, et al.22 concluded that a larger range of motion might cause greater stress on the surface of fixation between the implant and the vertebra, leading to instability and migration of artificial discs. Since their study analyzed three-dimensional CT motion, it had a much higher chance of identifying developing mobility or subsidence with osteolysis in the upper endplate. Our study included seven patients with mobile implants, and C5–6 was the most common level of occurrence. Of the seven mobile implant patients in our study, five were at C5–6, and all seven had subsidence at the upper endplate; three also experienced subsidence in the lower endplate. Five of the upper endplate subsidence cases involved anterior migration, and two migrated toward the posterior (Fig. 3).
Fig. 3. Improper position of mobile artificial implant. (A) Migration of implant (Prestige) at the upper endplate with anterior migration without osteolysis at C4–5. (B) Subsidence of implant (Mobi-C) at the upper endplate with posterior migration with osteolysis and developed iatrogenic cervical kyphosis at C5–6. (C) Subsidence of implant (Mobi-C) at the upper and lower endplate with posterior migration with osteolysis due to spondylitis and bony destruction at C5–6.
Several studies have reported similar cases, as in our Bryan device patient, where the instruments were unable to be visualized after surgery (Fig. 1).23,24,25,26 An iatrogenic esophageal tear may possibly occur during an anterior cervical approach, with particularly higher likelihood in patients undergoing reoperation. Pompili, et al.25 reported delayed esophagus or pharyngeal perforation caused by chronic inflammation or infection, which may be associated with subsequent dislodgement and migration of implants. In contrast, dislodgement of implants may also cause chronic inflammation and lead to delayed esophageal perforation. The device could be located within the gastrointestinal tract, the mediastinum, or even the intraperitoneal space.23,24 Our case was represented in 126 months after the operation; during that period, no other symptoms, such as dysphasia, were reported by the patient, except posterior neck pain and myelopathy. As a result, endoscopic exploration was not performed, and the artificial disc was eliminated in the stool. As in the above cases, there is a high possibility that implants that move will produce chronic inflammation and lead to delayed esophageal perforation.
Some devices, including those manufactured by Prestige LP and Mobi-C, have been designed as keel types so that they can be embedded into the endplate. In our study, there were five keel-type devices (three by Mobi-C, two from Prestige LP) out of seven patients who experienced complications caused by infection or osteolysis. With the migrated Mobi-C devices, two showed posterior migration of the superior portion and anterior migration of the inferior component, and one showed anterior migration of the superior portion. The two patients with Prestige LP cases demonstrated anterior migration only in the superior portion. This result alone does not indicate that the keel type of implant is more mobile, but keel-type devices are not the firmest available. However, the removal of these keel-type artificial discs is difficult during reoperation, as most of them produce areas of heterotopic ossification around the device. Removal was performed by drilling through the ossified area and removing the implant from the bottom one piece at a time.
In our study, surgical strategies were mostly chosen based on patient symptoms and bone quality. Similarly, Park, et al.13 reported a summarized algorithm for reoperation strategy to manage failures in C-TDR. We slightly modified the algorithm for our study (Fig. 4). Several studies reported that implantation of an alternative cervical artificial disc is also a suitable option in consideration of the patient's integrity of facet, endplate, and presence of osteophytes.12,21 Unfortunately, in this study, most of the cases in which artificial disc had a complication and needed replacement were accompanied by osteolysis or infection, so we chose fusion rather than alternative artificial disc.
Fig. 4. A modified algorithm of revision strategy after total disc replacement of the cervical spine (C-TDR).
A limitation of our study was the relatively small number of reoperation cases. This number alone may not be enough to establish the cause of all complications and their associated treatments. However, we believe that our data will contribute to and help establish theories as more data are added by other groups. We will continue our research through long-term follow-up visits and further accumulation of data.
C-TDR is good surgical option, but it is also important to adhere to strict surgical indications and contraindications to avoid failure of C-TDR. In particular, if the surgical site shows severe spondylosis, such as instability, facet joint degeneration, and osteophytes, or the patient is allergic to the implant material or osteoporosis, the surgery is contraindicated. Careful preparation is needed to avoid damaging the endplate, and it is recommended that the implant be located in the third section of the front, and not in the front or the rear. The results of our reoperations were good regardless of the approach. Therefore, we conclude that various reoperation options can be considered in patients with failed C-TDR.
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: Kwang-Ryeol Kim, Dong-Kyu Chin, Keun-Su Kim, and Sung-Uk Kuh.
- Data curation: all authors.
- Formal analysis: Kwang-Ryeol Kim.
- Funding acquisition: Sung-Uk Kuh.
- Investigation: Kwang-Ryeol Kim and Keun-Su Kim.
- Methodology: all authors.
- Project administration: Kwang-Ryeol Kim, Keun-Su Kim, and Sung-Uk Kuh.
- Resources: Dong-Kyu Chin, Keun-Su Kim, Yong-Eun Cho, Dong-Ah Shin, Keung-Nyun Kim, and Sung-Uk Kuh.
- Software: Kwang-Ryeol Kim.
- Supervision: Dong-Kyu Chin, Keun-Su Kim, and Sung-Uk Kuh.
- Validation: Kwang-Ryeol Kim.
- Visualization: Kwang-Ryeol Kim.
- Writing—original draft: Kwang-Ryeol Kim.
- Writing—review & editing: Sung-Uk Kuh.
- Approval of final manuscript: all authors.
References
- 1.Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993;75:1298–1307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Lee JH, Kim JS, Lee JH, Chung ER, Shim CS, Lee SH. Comparison of cervical kinematics between patients with cervical artificial disc replacement and anterior cervical discectomy and fusion for cervical disc herniation. Spine J. 2014;14:1199–1204. doi: 10.1016/j.spinee.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 3.Matsumoto M, Okada E, Ichihara D, Watanabe K, Chiba K, Toyama Y, et al. Anterior cervical decompression and fusion accelerates adjacent segment degeneration: comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine (Phila Pa 1976) 2010;35:36–43. doi: 10.1097/BRS.0b013e3181b8a80d. [DOI] [PubMed] [Google Scholar]
- 4.Wigfield C, Gill S, Nelson R, Langdon I, Metcalf N, Robertson J. Influence of an artificial cervical joint compared with fusion on adjacent-level motion in the treatment of degenerative cervical disc disease. J Neurosurg. 2002;96(1 Suppl):17–21. doi: 10.3171/spi.2002.96.1.0017. [DOI] [PubMed] [Google Scholar]
- 5.Delamarter RB, Zigler J. Five-year reoperation rates, cervical total disc replacement versus fusion, results of a prospective randomized clinical trial. Spine (Phila Pa 1976) 2013;38:711–717. doi: 10.1097/BRS.0b013e3182797592. [DOI] [PubMed] [Google Scholar]
- 6.Park JY, Kim KH, Kuh SU, Chin DK, Kim KS, Cho YE. What are the associative factors of adjacent segment degeneration after anterior cervical spine surgery? Comparative study between anterior cervical fusion and arthroplasty with 5-year follow-up MRI and CT. Eur Spine J. 2013;22:1078–1089. doi: 10.1007/s00586-012-2613-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sasso RC, Best NM, Metcalf NH, Anderson PA. Motion analysis of Bryan cervical disc arthroplasty versus anterior discectomy and fusion: results from a prospective, randomized, multicenter, clinical trial. J Spinal Disord Tech. 2008;21:393–399. doi: 10.1097/BSD.0b013e318150d121. [DOI] [PubMed] [Google Scholar]
- 8.Park CK, Ryu KS. Are controversial issues in cervical total disc replacement resolved or unresolved?: a review of literature and recent updates. Asian Spine J. 2018;12:178–192. doi: 10.4184/asj.2018.12.1.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Auerbach JD, Jones KJ, Fras CI, Balderston JR, Rushton SA, Chin KR. The prevalence of indications and contraindications to cervical total disc replacement. Spine J. 2008;8:711–716. doi: 10.1016/j.spinee.2007.06.018. [DOI] [PubMed] [Google Scholar]
- 10.Buchowski JM, Riew KD. Primary indications and disc space preparation for cervical disc arthroplasty. In: Yue JJ, Bertagnoli R, MscAfee PC, An HS, editors. Motion preservation surgery of the spine: advanced techniques and controversies. Philadelphia: Elsevier, Saunders; 2008. pp. 185–192. [Google Scholar]
- 11.Leven D, Meaike J, Radcliff K, Qureshi S. Cervical disc replacement surgery: indications, technique, and technical pearls. Curr Rev Musculoskelet Med. 2017;10:160–169. doi: 10.1007/s12178-017-9398-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Skovrlj B, Lee DH, Caridi JM, Cho SK. Reoperations following cervical disc replacement. Asian Spine J. 2015;9:471–482. doi: 10.4184/asj.2015.9.3.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Park JB, Chang H, Yeom JS, Suk KS, Lee DH, Lee JC. Revision surgeries following artificial disc replacement of cervical spine. Acta orthop Traumatol Turc. 2016;50:610–618. doi: 10.1016/j.aott.2016.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nandyala SV, Marquez-Lara A, Fineberg SJ, Singh K. Comparison of revision surgeries for one- to two-level cervical TDR and ACDF from 2002 to 2011. Spine J. 2014;14:2841–2846. doi: 10.1016/j.spinee.2014.03.037. [DOI] [PubMed] [Google Scholar]
- 15.Skeppholm M, Henriques T, Tullberg T. Higher reoperation rate following cervical disc replacement in a retrospective, long-term comparative study of 715 patients. Eur Spine J. 2017;26:2434–2440. doi: 10.1007/s00586-017-5218-0. [DOI] [PubMed] [Google Scholar]
- 16.Anderson PA, Sasso RC, Rouleau JP, Carlson CS, Goffin J. The Bryan Cervical Disc: wear properties and early clinical results. Spine J. 2004;4:S303–S309. doi: 10.1016/j.spinee.2004.07.026. [DOI] [PubMed] [Google Scholar]
- 17.Lee SH, Kim KS. Ruptured artificial disc (Bryan Cervical Disc) Korean J Spine. 2011;8:232–235. [Google Scholar]
- 18.Malham GM, Parker RM, Ellis NJ, Chan PG, Varma D. Cervical artificial disc replacement with ProDisc-C: clinical and radiographic outcomes with long-term follow-up. J Clin Neurosci. 2014;21:949–953. doi: 10.1016/j.jocn.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 19.Wenger M, Markwalder TM. Heterotopic ossification associated with myelopathy following cervical disc prosthesis implantation. J Clin Neurosci. 2016;26:154–156. doi: 10.1016/j.jocn.2015.09.016. [DOI] [PubMed] [Google Scholar]
- 20.Yi S, Oh J, Choi G, Kim TY, Shin HC, Kim KN, et al. The fate of heterotopic ossification associated with cervical artificial disc replacement. Spine (Phila Pa 1976) 2014;39:2078–2083. doi: 10.1097/BRS.0000000000000640. [DOI] [PubMed] [Google Scholar]
- 21.Onken J, Reinke A, Radke J, Finger T, Bayerl S, Vajkoczy P, et al. Revision surgery for cervical artificial disc: surgical technique and clinical results. Clin Neurol Neurosurg. 2017;152:39–44. doi: 10.1016/j.clineuro.2016.10.021. [DOI] [PubMed] [Google Scholar]
- 22.Skeppholm M, Svedmark P, Noz ME, Maguire GQ, Jr, Olivecrona H, Olerud C. Evaluation of mobility and stability in the Discover artificial disc: an in vivo motion study using high-accuracy 3D CT data. J Neurosurg Spine. 2015;23:383–389. doi: 10.3171/2014.12.SPINE14813. [DOI] [PubMed] [Google Scholar]
- 23.Fountas KN, Kapsalaki EZ, Machinis T, Robinson JS. Extrusion of a screw into the gastrointestinal tract after anterior cervical spine plating. J Spinal Disord Tech. 2006;19:199–203. doi: 10.1097/01.bsd.0000164164.11277.49. [DOI] [PubMed] [Google Scholar]
- 24.Gazzeri R, Tamorri M, Faiola A, Gazzeri G. Delayed migration of a screw into the gastrointestinal tract after anterior cervical spine plating. Spine (Phila Pa 1976) 2008;33:E268–E271. doi: 10.1097/BRS.0b013e31816b8831. [DOI] [PubMed] [Google Scholar]
- 25.Pompili A, Canitano S, Caroli F, Caterino M, Crecco M, Raus L, et al. Asymptomatic esophageal perforation caused by late screw migration after anterior cervical plating: report of a case and review of relevant literature. Spine (Phila Pa 1976) 2002;27:E499–E502. doi: 10.1097/00007632-200212010-00016. [DOI] [PubMed] [Google Scholar]
- 26.Yeh MY, Huang WC, Kuo CH, Chang PY, Cheng H. Disappearance of anterior cervical corpectomy cage. Cureus. 2019;11:e3985. doi: 10.7759/cureus.3985. [DOI] [PMC free article] [PubMed] [Google Scholar]