Abstract
Background
Type 2 diabetes in the Gulf Cooperation Council countries, including Oman, is currently the fastest growing health crisis and is a significant cause of premature mortality and disability. There is currently insufficient up-to-date information available on prevalence of type 2 diabetes. This study aimed to assess the latest prevalence of type 2 diabetes mellitus and its associated demographic, behavioural, and clinical risk factors.
Methods
Using the WHO STEPwise approach to chronic disease surveillance, a nationally representative population-based survey was conducted from January to April 2017 of adults aged 18 years and above. A multi-stage, stratified, geographically clustered random sampling surveyed 9053 households including Omani nationals and non-Omani residents. Univariate and multiple logistic regression analysis was performed to determine the predictors of diabetes.
Results
Overall prevalence of diabetes among the population was 15.7% (95% CI: 14.0–17.5%) whereas prevalence of prediabetes was 11.8% (95% CI: 11.4–12.2%). Age, educational level, raised blood pressure, family history of diabetes, abnormal waist-to-hip ratio, and hypertriglyceridemia were found to be significantly associated with diabetes mellitus. Of the cases of diabetes mellitus, 17% were newly diagnosed and 13.2% were on medication and had an uncontrolled glucose level while 55.5% were not taking medication (although diagnosed) and had an uncontrolled blood glucose level.
Conclusions
The present study provides reliable information regarding the high prevalence of diabetes mellitus among the adult population in Oman with urgent attention needed to address this significant burden on the health system. The high proportion of uncontrolled cases warrants further research, awareness programmes, and community interventions.
Keywords: Diabetes mellitus, Prevalence, Risk factors, Diabetes, Prediabetes, Oman, STEPS, NCD, Non-communicable disease, Control status
Background
Around 463 million people had diabetes mellitus (DM) in 2019 based on International Diabetes Federation estimates, with a projection of 700 million by 2040. From this, it is evident that DM is one of the fastest growing health crises facing the twenty-first century. Type 2 diabetes, the most common form, accounts for about 90% of all global diabetes cases. The global economic burden of DM is massive, with an estimated annual expenditure of USD 760 billion in 2019, projected to grow by 11.2% to USD 845 billion by 2045 [1].
Recent literature revealed that the prevalence of type 2 diabetes in the Gulf Cooperation Council (GCC) is high with a dramatic increase in the past two decades, and is expected to increase by 96.5% by 2045 [2, 3]. Oman has been classified by the World Health Organization (WHO) as a country with low child and adult mortality rates (crude death rate: 2.4 per 1000). However, DM is currently the sixth leading cause of premature mortality in Oman and the fifth prominent cause of disability-adjusted life years lost [4].
Diabetes prevalence estimation and identification of high-risk groups is vital for surveillance, and development of policies and community-based interventions. There is currently insufficient, up-to-date information available on prevalence of type 2 diabetes and its correlates in the Sultanate of Oman. Previous community-based studies in Oman have been limited and do not truly represent all the risk factors and its relationships with diabetes in the Oman population [5–7]. This survey study, comprising the largest population-based survey in Oman so far, in collaboration with the WHO aimed to assess the latest prevalence of type 2 DM and its associated demographic, behavioural, and clinical risk factors.
Methods
Sampling
Briefly, and as previously described in the STEPS survey 2017 main paper [8], a nation-wide non-communicable disease (NCD) risk factor survey based on WHO STEPwise approach to chronic disease surveillance was undertaken in all the governorates (regions) in the Sultanate of Oman from January 2017 to April 2017. The survey adopted a multi-stage stratified, geographically clustered random sampling approach using the 2010 national census sampling frame. Cluster sampling (based on the 2010 census blocks) was used and symmetric equal number of blocks were chosen in each governorate. A total of 9053 households, 823 households chosen from each governorate‚ were selected (Omani nationals and non-Omani national residents) with one adult being selected from each household randomly. Adjustment of sample weight was done for non-response at the household level. The target age group was 18 years or older.
Data collection
A culturally adapted, Arabic translated, and pre-tested version of the WHO STEPS questionnaire (version 3.1) was used [8, 9]. As part of the household survey, sociodemographic and behavioural information on tobacco use, diet, physical activity, history of chronic diseases, family history of chronic conditions was collected in Step 1. Physical measurements such as height, weight, hip circumference, waist circumference, and blood pressure were collected in Step 2. Biochemical tests were conducted to measure fasting blood glucose, total cholesterol, and triglycerides in Step 3.
Data were collected by trained health professionals in the field. SECA adult portable stadiometers were used to measure height after removing shoes, socks, slippers and any head gear, with an accuracy up to 0.1 cm. SECA® digital weighing scales were used to measure the weight of the individuals. The scale was regularly calibrated against a standard weight. Waist circumference was measured using a SECA® constant tension tape to the nearest 0.1 cm. Blood pressure levels (both systolic blood pressure (SBP) and diastolic blood pressure (DBP)) were measured three times using the Omron M3 digital blood pressure device as recommended by WHO, with the average of the closest two readings taken as the final reading. Overnight fasting blood samples were drawn to assess the biochemical profile of participants. For blood glucose and lipid profile measurements, dry chemistry method was used (CardioChek® Plus Analyzer). The reference biomarker cut-off points are mentioned under the heading of operational definitions.
Data analysis
Categorical variables are summarized using proportions and continuous variables using mean, with 95% confidence intervals. Chi square test was used for comparison of proportions across groups. Univariate and multiple logistic regression analysis was performed to determine the predictors of diabetes. All variables were entered into the multiple regression model to ensure that the interaction of all variables and their effects with the presence of other variables were measured. Statistical analysis was done using STATA/IC version 16.1.
Ethical considerations
The survey was approved by the Central Research and Ethical Review & Approval Committee of the Ministry of Health, Sultanate of Oman. (Approval No: 26/2015). Written informed consent was obtained from participants for participation in the study separately during health history collection (STEP 1) and measurement of biophysiological parameters (STEP 2 & 3). The confidentiality of the data gathered was maintained through a secure server.
Operational definitions
Diagnostic criteria were based on WHO guidelines where diabetes was defined as individuals diagnosed by a physician and/or on antidiabetic medications and/or those who had fasting blood glucose ≥7 mmol/l (≥126 mg/dl), while prediabetes or impaired fasting glucose was defined as fasting blood glucose ≥6.1 mmol/l (≥110 mg/dl) and < 7 mmol/l (< 126 mg/dl). Current smoking included those individuals who were reported smoking in the month preceding the survey. Raised blood pressure was defined as individuals diagnosed by a physician and on antihypertensive medications (self-reported) and/or those who had systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg (WHO Criteria) [10, 11]. One serving or portion of vegetables was considered to be 80 g or 1 cup of raw green leafy vegetables or 1/2 cup of other cooked/chopped vegetables. One serving or portion of fruit was considered to be one whole medium-sized fruit or two smaller-sized fruits (WHO). Obesity was defined as Body Mass Index (BMI) ≥ 30. Hypertriglyceridemia was defined as serum triglyceride levels ≥150 mg/dl (≥1.7 mmol/l). Physical activity was assessed using the Global Physical Activity Questionnaire (GPAQ), which has been developed by the World Health Organization and used in the STEPS questionnaire [12, 13]. Participants were classified as sufficiently active when exceeding the minimum duration of physical activity per week recommended by WHO i.e. 150 min of moderate intensity physical activity or 75 min of vigorous intensity physical activity or an equivalent combination of moderate- and vigorous intensity physical activity [13]. Show cards (pictorial, adapted to the local context) were used to explain to the participants the type of physical activity, servings of fruits and vegetables and salty food intake [12].
Results
Table 1 shows the demographic characteristics of the respondents in the study. The overall response rate among survey participants was 75.5%, with the figure for Omani nationals being 73.5%. Majority of respondents were 30–39 years old (32.4%), Omani nationals (70.6%), had completed secondary school (34.3%), and were not currently engaged in any form of employment (44.9%).
Table 1.
Demographic characteristics of the participants
| Characteristics | n | Percentage |
|---|---|---|
| Age groups (years) | ||
| 18–29 | 1647 | 24.4 |
| 30–39 | 2187 | 32.4 |
| 40–49 | 1410 | 20.9 |
| 50–59 | 708 | 10.5 |
| 60 and above | 630 | 9.3 |
| Sex | ||
| Male | 3365 | 51.1 |
| Female | 3217 | 48.9 |
| Nationality | ||
| Omani | 4645 | 70.6 |
| Non-Omani | 1937 | 29.4 |
| Education Level | ||
| No formal education | 1772 | 26.9 |
| Preparatory or lower | 988 | 15.0 |
| Secondary completed | 2258 | 34.3 |
| University and above | 1558 | 23.7 |
| Employment status | ||
| Public sector employee | 1287 | 21.5 |
| Private sector employee | 1766 | 29.5 |
| Self-employed | 251 | 4.1 |
| Not currently working | 2692 | 44.9 |
Prevalence of DM
15.7% (95% CI: 14.0–17.5%) of the survey participants were found to have DM (Table 2). The prevalence was similar among women (16.1%) and men (15.4%). A lower prevalence of raised blood glucose was seen in Omani nationals (14.5%) as compared to non-Omani residents (18.8%). Impaired glycaemia was prevalent among 11.8% of the population. Higher prevalence’s were observed among women (12.6%) and non-Omani residents (12.5%) as compared to men (11.1%,) and Omani (11.5%), respectively.
Table 2.
Prevalence of diabetes mellitus (DM) and pre-diabetes by nationality and demographic characteristics
| Characteristics | Omani | Non-Omani | Total | |||
|---|---|---|---|---|---|---|
| Prevalence of pre-diabetes N (%, 95 CI) | Prevalence of diabetes N (%, 95 CI) | Prevalence of pre-diabetes N (%, 95 CI) | Prevalence of diabetes N (%, 95 CI) | Prevalence of pre-diabetes N (%, 95 CI) | Prevalence of diabetes N (%, 95 CI) | |
| Age group | ||||||
| 18–29 | 138 (8.6,(7.7–9.6)) | 55 (3.1,(2.1–4.4)) | 80 (11.8,(9.8–14.1)) | 34 (3.2,(1.9–5.2)) | 218 (9.3,(8.4–10.2)) | 89 (3.1,(2.3–4.2)) |
| 30–39 | 201 (12.8,(11.8–13.9)) | 119 (6.1,(4.7–7.8)) | 112 (13,(11.3–14.9)) | 99 (12.4,(9.2–16.5)) | 313 (12.9,(12.1–13.7)) | 218 (8.23,(6.7–10.0)) |
| 40–49 | 148 (14.6,(12.9–16.6)) | 166 (20.6,(14.7–28.1)) | 83 (11.3,(9.7–13)) | 105 (25.7,(20.0–32.2)) | 231 (13.5,(12.2–14.9)) | 271 (22.3,(17.9–27.5)) |
| 50–59 | 81 (10.5,(9.1–12)) | 162 (34.7,(26.6–3.7)) | 30 (15.3,(12.7–18.3)) | 81 (37.8,(27.5–49.3)) | 111 (11.7,(10.4–13)) | 243 (35.5,(28.8–42.8)) |
| 60 & above | 91 (12.6,(11.5–13.9)) | 205 (39.8,(31.7–48.4)) | 5 (11.2,(7.4–16.5)) | 28 (58.0,(38.5–75.2)) | 96 (12.4,(11.3–13.6)) | 233 (42.6,(35.1–50.5)) |
| Sex | ||||||
| Male | 249 (10.1,(9.4–10.8)) | 253 (13.5,(10.3–17.4)) | 261 (12.4,(11.1–13.9)) | 290 (18.4,(15.3–22.0)) | 510 (11,(10.3–11.7)) | 543 (15.4,(13.0–18.1)) |
| Female | 410 (12.6,(11.8–13.4)) | 454 (15.3,(13.0–18.1)) | 49 (12.3,(10.1–14.9)) | 57 (20.1,(14.3–27.5)) | 459 (12.6,(11.8–13.3)) | 511 (16.1,(13.8–18.6)) |
| Education level | ||||||
| No formal education | 230 (15.5,(14.4–16.8)) | 373 (31.8,(27.0–37.0)) | 76 (14.7,(13.3–16.3)) | 83 (23.6,(17.5–30.9)) | 306 (15.4,(14.4–16.4)) | 456 (30.3,(26.2–34.8)) |
| Preparatory or less | 80 (12.6,(10.9–14.4)) | 98 (23.4,(17.6–30.3)) | 75 (13.5,(12.2–14.9)) | 88 (20.4,(15.4–26.5)) | 155 (12.9,(11.8–14.1)) | 186 (22.2,(18.1–27.0)) |
| Secondary completed | 224 (10.3,(9.6–11.1)) | 156 (8.5,(5.7–12.2)) | 74 (10.5,(8.6–12.7)) | 96 (22.3,(15.5–31.0)) | 298 (10.4,(9.7–11.1)) | 252 (11.0,(8.4–14.2)) |
| University & above | 124 (9.7,(8.6–11)) | 80 (7.57,(4.7–11.9)) | 85 (12.5,(10.6–14.6)) | 79 (15.0,(11.1–19.9)) | 209 (10.8,(9.8–11.9)) | 159 (10.5,(8.0–13.6)) |
| Marital Status | ||||||
| Never married | 89 (8.3,(7.4–9.4)) | 42 (4.3,(2.1–8.5)) | 72 (12.1,(9.6–15.1)) | 33 (5.3,(2.8–9.8)) | 161 (9.1,(8.2–10.2)) | 75 (4.6,(2.6–7.7)) |
| Currently married | 496 (13,(12.3–13.7)) | 544 (17.3,(14.7–20.1)) | 233 (12.6,(11.3–13.9)) | 309 (22.2,(18.9–25.8)) | 729 (12.8,(12.3–13.4)) | 853 (18.8,(16.7–21.0)) |
| Divorced/Separated | 22 (12.3,(9.8–15.2)) | 91 (22.2,(8.8–45.5)) | 4 (16.2,(9.3–26.7)) | 2 (48.3,(12.5–85.9)) | 26 (12.5,(10.1–15.3)) | 103 (23.6,(10.4–5.3)) |
| Widowed | 52 (10.6,(9.1–12.3)) | 98 (34.7,(24.0–47.1)) | 1 (3.3,(1.7–6.2)) | 3 (30.5,(5.4–76.9)) | 53 (10.1,(8.7–11.7)) | 101 (34.4,(24.1–6.4)) |
| Work status | ||||||
| Public sector employee | 163 (13.7,(12.3–15.1)) | 124 (11.4,(8.2–15.7)) | 32 (11.2,(8.7–14.2)) | 27 (13.6,(7.8–22.6)) | 195 (13.4,(12.2–14.7)) | 151 (11.6,(8.6–15.5)) |
| Private sector employee | 60 (5.9,(5.2–6.7)) | 77 (13.9,(7.5–24.4)) | 244 (12.5,(11.3–13.9)) | 278 (17.8,(14.7–21.3)) | 304 (10.3,(9.4–11.3)) | 355 (16.5,(13.3–20.3)) |
| Not currently working | 435 (11.9,(11.3–12.6)) | 506 (15.9,(13.5–18.5)) | 34 (12.4,(10.2–14.9)) | 42 (24.6,(17.0–34.2)) | 469 (11.9,(11.3–12.6)) | 548 (16.8,(14.5–19.4)) |
| Total | 659 (11.5,(11.0–12.1)) | 707 (14.5,(12.5–16.8)) | 310 (12.5,(11.7–13.3)) | 347 (18.8,(16.0–22.0)) | 969 (11.8,(11.4–12.2)) | 1054 (15.7,(14.0–17.5)) |
Risk factors for DM
All demographic, lifestyle, and clinical variables were entered in a multivariate regression analysis model. In terms of demographic covariates, age group (p < .001) and educational level (p < .05) were found to be the risk factors significantly associated with DM (Table 3). In terms of lifestyle and clinical covariates, raised blood pressure (p < .05), family history of diabetes (p < .001), abnormal waist-to-hip ratio (p < .001), and hypertriglyceridemia (p < .001) were found to be significantly associated with DM (Table 4).
Table 3.
Multivariate analysis for demographic covariates associated with type 2 diabetes
| Covariate | Omani | Non-Omani | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total N | Prevalence of diabetes n (%) | Odds Ratio (P(95% CI)) | Multivariant Regression Analysis | Total N | Prevalence of diabetes N (%) | Odds Ratio (P(95% CI)) | Multivariant Regression Analysis | Total N | Prevalence of diabetes n (%) | Odds Ratio (P(95% CI)) | Multivariant Regression Analysis | |
| P(95% CI) | P(95% CI) | P(95% CI) | ||||||||||
| Age group | 0.000 | 0.000 | 0.000 | |||||||||
| 18–29 | 1102 | 55 (3.08) | Ref | 437 | 34 (3.22) | Ref | 1539 | 89 (3.1) | Ref | |||
| 30–39 | 1337 | 119 (6.11) | 0.08 (0.778) | 707 | 99 (12.44) | 1.14**(0.001) | 2044 | 218 (8.23) | 0.48*(0.036) | |||
| 40–49 | 856 | 166 (20.59) | 1.21***(0.000) | 465 | 105 (25.66) | 1.86***(0.000) | 1321 | 271 (22.33) | 1.40***(0.000) | |||
| 50–59 | 484 | 162 (34.69) | 1.85***(0.000) | 183 | 81 (37.8) | 2.23***(0.000) | 667 | 243 (35.48) | 1.99***(0.000) | |||
| 60 and above | 541 | 205 (39.76) | 2.11***(0.000) | 50 | 28 (57.96) | 3.26***(0.000) | 591 | 233 (42.64) | 2.37***(0.000) | |||
| Sex | 0.242 | 0.517 | 0.384 | |||||||||
| Male | 1665 | 253 (13.48) | Ref | 1518 | 290 (18.41) | Ref | 3183 | 543 (15.39) | Ref | |||
| Female | 2655 | 454 (15.38) | 0.31 (0.148) | 324 | 57 (20.11) | 0.28 (0.500) | 2979 | 511 (16.06) | 0.33 (0.075) | |||
| Education level | 0.048 | 0.003 | 0.022 | |||||||||
| No formal education | 1274 | 373 (31.77) | Ref | 387 | 83 (23.61) | Ref | 1661 | 456 (30.33) | Ref | |||
| Preparatory or less | 487 | 98 (23.38) | 0.29 (0.244) | 439 | 88 (20.41) | 0.04 (0.878) | 926 | 186 (22.22) | 0.26 (0.186) | |||
| Secondary completed | 1648 | 156 (8.45) | −0.31 (0.253) | 462 | 96 (22.34) | 0.047 (0.865) | 2110 | 252 (10.99) | −0.11 (0.597) | |||
| University and above | 908 | 80 (7.57) | −0.61 (0.073) | 552 | 79 (14.97) | −0.80**(0.007) | 1460 | 159 (10.48) | −0.48*(0.033) | |||
| Marital Status | 0.977 | 0.561 | 0.835 | |||||||||
| Never married | 742 | 42 (4.34) | Ref | 400 | 33 (5.32) | Ref | 1378 | 75 (4.55) | Ref | |||
| Currently married | 3161 | 544 (17.25) | 0.45 (0.145) | 1422 | 309 (22.19) | 0.57 (0.118) | 4895 | 853 (18.8) | 0.53*(0.035) | |||
| Divorced/Separated | 114 | 91 (22.17) | 0.49 (0.427) | 14 | 2 (48.25) | 0.92 (0.244) | 135 | 103 (23.63) | 0.48 (0.390) | |||
| Widowed | 303 | 98 (34.68) | 0.26 (0.541) | 6 | 3 (30.47) | −0.54 (0.716) | 335 | 101 (34.42) | 0.23 (0.542) | |||
| Work status | 0.371 | 0.459 | 0.532 | |||||||||
| Public sector employee | 1042 | 124 (11.41) | Ref | 175 | 27 (13.58) | Ref | 1217 | 151 (11.64) | Ref | |||
| Private sector employee | 465 | 77 (13.98) | 0.09 (0.798) | 1442 | 278 (17.79) | 0.007 (0.986) | 1907 | 355 (16.5) | 0.28 (0.202) | |||
| Not currently working | 2810 | 506 (15.88) | −0.23 (0.454) | 225 | 42 (24.63) | 0.18 (0.708) | 3035 | 548 (16.81) | −0.08 (0.743) | |||
CI Confidence interval; p values in parentheses, * p < 0.05 ** p < 0.01 *** p < 0.001
Table 4.
Multivariate analysis for behavioural and clinical covariates associated with type 2 diabetes
| Omani | Non-Omani | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total N | Diabetes n (%) | Odds Ratio (P(95% CI)) |
Multivariant Regression Analysis | Total N | Diabetes n (%) | Odds Ratio (P(95% CI)) |
Multivariant Regression Analysis | Total N | Diabetes n (%) | Odds Ratio (P(95% CI)) |
Multivariant Regression Analysis | |
| P(95% CI) | P(95% CI) | P(95% CI) | ||||||||||
| Smoking | 0.317 | 0.606 | 0.98 | |||||||||
| Yes | 224 | 38 (12.78) | Ref | 302 | 66 (21.21) | Ref | 526 | 104 (16.67) | Ref | |||
| No | 4096 | 669 (14.65) | −0.44 (0.223) | 1540 | 281 (18.42) | 0.12 (0.653) | 5636 | 950 (15.61) | −0.07 (0.747) | |||
| Raised Blood pressurea | 0.008 | 0.159 | 0.002 | |||||||||
| No | 2959 | 322 (8.65) | Ref | 1233 | 185 (13.3) | Ref | 4192 | 507 (9.84) | Ref | |||
| Yes | 1361 | 385 (26.84) | 0.56**(0.004) | 609 | 162 (28.14) | 0.33 (0.133) | 1970 | 547 (27.23) | 0.51***(0.001) | |||
| ≥ 5 servings of fruits and/or vegetable daily | 0.561 | 0.554 | 0.868 | |||||||||
| No | 2706 | 447 (13.2) | Ref | 1360 | 262 (18.43) | Ref | 4066 | 709 (14.85) | Ref | |||
| Yes | 1614 | 260 (16.22) | −0.07 (0.683) | 482 | 85 (19.71) | 0.17 (0.446) | 2096 | 345 (16.95) | 0.05 (0.753) | |||
| BMI ≥ 30 | 0.58 | 0.349 | 0.673 | |||||||||
| No | 2879 | 397 (12.18) | Ref | 1512 | 262 (17.17) | Ref | 4391 | 659 (13.73) | Ref | |||
| Yes | 1441 | 310 (19.26) | −0.19 (0.320) | 330 | 85 (25.74) | 0.22 (0.367) | 1771 | 395 (20.42) | −0.11 (0.453) | |||
| Family history of blood pressure | 0.938 | 0.902 | 0.976 | |||||||||
| No | 2591 | 425 (13.2) | Ref | 1281 | 227 (16.44) | Ref | 3872 | 652 (14.18) | Ref | |||
| Yes | 1729 | 282 (16.27) | −0.05 (0.819) | 561 | 120 (23.44) | 0.05 (0.832) | 2290 | 402 (17.89) | −0.002 (0.988) | |||
| Family history of diabetes | 0.000 | 0.01 | 0.000 | |||||||||
| No | 2787 | 402 (10.87) | Ref | 1317 | 219 (15.51) | Ref | 4104 | 621 (12.26) | Ref | |||
| Yes | 1533 | 305 (19.7) | 1.02***(0.000) | 525 | 128 (25.53) | 0.54*(0.015) | 2058 | 433 (21.04) | 0.83***(0.000) | |||
| Family history of total cholesterol | 0.677 | 0.309 | 0.285 | |||||||||
| No | 3210 | 526 (14.55) | Ref | 1542 | 290 (19.11) | Ref | 4752 | 816 (15.92) | Ref | |||
| Yes | 1110 | 181 (14.49) | −0.05 (0.829) | 300 | 57 (17.6) | −0.30 (0.320) | 1410 | 238 (15.1) | −0.16 (0.366) | |||
| Waist-to-Hip Ratiob | 0.001 | 0.126 | 0.000 | |||||||||
| Normal | 1365 | 115 (5.59) | Ref | 566 | 82 (10.74) | Ref | 1931 | 197 (6.88) | Ref | |||
| Abnormal | 2705 | 560 (20.18) | 0.68**(0.002) | 1256 | 265 (23.08) | 0.33 (0.184) | 3961 | 825 (21.02) | 0.57***(0.001) | |||
| Hypertriglyceridemiac | 0.002 | 0.009 | 0.000 | |||||||||
| No | 3365 | 481 (12.39) | Ref | 1132 | 166 (14.41) | Ref | 4497 | 647 (12.85) | Ref | |||
| Yes | 955 | 226 (22.5) | 0.56**(0.004) | 710 | 181 (25.75) | 0.51*(0.014) | 1665 | 407 (23.82) | 0.57***(0.000) | |||
| Physical activity | 0.755 | 0.36 | 0.943 | |||||||||
| Insufficient | 2177 | 386 (15.98) | Ref | 668 | 126 (21.39) | Ref | 2845 | 512 (17.13) | Ref | |||
| Sufficient | 2143 | 321 (13.51) | 0.05 (0.739) | 1174 | 221 (17.72) | 0.12 (0.561) | 3317 | 542 (14.81) | 0.06 (0.659) | |||
CI Confidence interval; p values in parentheses, * p < 0.05 ** p < 0.01 *** p < 0.001; aSBP ≥ 140 and/or DBP ≥ 90 and/or currently on medication; bAbnormal defined as > 0.85 for female & > 0.90 for male; c Serum triglycerides ≥1.7 mmol/L
Treatment and control status of DM
Among all the respondents with raised blood glucose or on medication for blood glucose, 83% were known cases of DM while 17% were newly diagnosed (Table 5). 14.3% of respondents were on a specific anti-diabetic medication and had a controlled glucose level (treatment success), 13.2% were on medication and a raised blood glucose level (treatment failure), and 55.5% were not taking medication (although diagnosed) and had a raised blood glucose level.
Table 5.
Prevalence of the population with raised blood glucose or on medication for blood glucose disaggregated by diagnosis and treatment status
| Category | On medication and glucose < 7 mmol/L | On medication and glucose ≥ 7 mmol/L | Not aware of raised glucose ≥ 7 mmol/L | Not taking prescribed medication and glucose ≥ 7 mmol/L | Total N |
|---|---|---|---|---|---|
| Age group | |||||
| 18–29 | 12.0 (0.7–2.3) | 10.3 (6.9–15.1) | 39.2 (34.3–44.3) | 49.2 (43.9–54.6) | 87 |
| 30–39 | 6.6 (4.9–8.9) | 6.5 (4.9–8.5) | 29.1 (25.9–32.3) | 57.8 (54.2–61.4) | 215 |
| 40–49 | 12.1 (10.3–14.2) | 10.1 (8.3–12.1) | 16.7 (14.4–19.2) | 61.1 (57.0–65.0) | 259 |
| 50–59 | 25.3 (21.8–29.1) | 11.3 (9.5–13.4) | 8.8 (7.5–10.3) | 54.6 (50.4–58.8) | 236 |
| 60+ | 14.2 (12.0–16.5) | 23.3 (19.9–27.1) | 12.8 (10.8–15.0) | 49.8 (45.2–54.4) | 226 |
| Sex | |||||
| Male | 13.0 (11.5–14.8) | 10.4 (8.9–12.2) | 20.8 (19–22.7) | 55.7 (52.6–58.7) | 526 |
| Female | 15.7 (13.9–17.6) | 16.0 (14.2–18) | 13.0 (11.5–14.6) | 55.3 (25.5–58.1) | 497 |
| Nationality | |||||
| Omani | 15.3 (13.8–17.0) | 14.9 (13.3–16.6) | 13.4 (12.1–14.7) | 56.5 (53.7–59.1) | 683 |
| Non-Omani | 12.3 (10.4–14.5) | 9.7 (7.9–11.7) | 24.5 (22.2–26.8) | 53.6 (50.6–56.6) | 340 |
| Overall | 14.3 (13.1–15.6) | 13.2 (12–14.5) | 17.0 (15.9–18.2) | 55.5 (53.4–57.6) | 1023 |
Small but significantly higher prevalence was observed for Omani nationals under medication and had controlled blood glucose status compared to non-Omani residents (15.3% vs 12.3%, p < 0.05), but no significant difference was found between male and females in this group. A majority of newly discovered cases with raised blood glucose level was observed in the 18–29 years age group (39.2%), males (20.8%) and non-Omani residents (24.5). Similarly, a majority of respondents not currently on medication and raised blood glucose level was found among 40–49 years old (61%), and Omani nationals (56.5%).
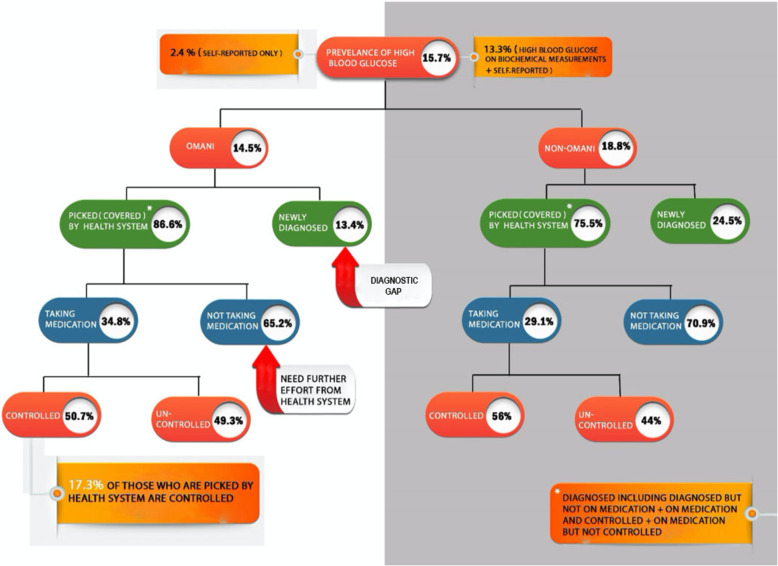
Figure 1 reveals that among the 14.5% Omani nationals, 86.6% were picked by the health system and 13.4% were newly diagnosed. Of those who were covered by the health system, only 34.8% were taking the prescribed medications and 65.2% were not. Of those who were taking their prescribed medication, only 50.7% were controlled for DM. This demonstrates that only 17.3% of those who were picked by the health system had controlled blood glucose status. Similarly, for the 18.8% of non-Omani residents, 75.5% were picked by the health system and 24.5% were newly diagnosed. Of those who were covered by the health system, only 29% were taking the medications. Of those who were taking medication, only 56% were controlled for DM.
Fig. 1.
Diabetes chart by nationality, diagnosis, treatment status, and control status
Discussion
This study represents the largest multistage stratified community-based national survey in Oman which included all the 11 governorates of Oman. A high response rate was achieved with the employment of the standardized STEPS questionnaire, robust methodology, and adherence to STROBE guidelines [14].
The results of this survey revealed a high prevalence of DM and prediabetes among the Oman population. Some national and regional surveys were conducted previously which showed the prevalence of diabetes between 1991 and 2010, with the last main national survey conducted in 2008 [5]. An increase in the prevalence of DM was found from the 2008 national survey (12.3%) when compared to our results in 2017 (15.7%) [15]. Strikingly, there has been a sharp increase in prevalence of prediabetes from 4.4% in 2008 to 11.8% in the current study. Our results for DM were similar to other STEPS studies conducted in the WHO Eastern Mediterranean (EMR) region, but higher than the prevalence reported in other Asian countries [16–19]. Omani nationals (14.5%) were found to have a significantly lower prevalence than non-Omani residents (18.8%) in this survey. This may be attributed to the universal healthcare system which provides free primary healthcare for Omani citizens and the difference in lifestyle between the two subgroups.
It has been reported that biological composition as well as obesity has an effect on sex differences associated with the burden and complication of DM [20]. In this present study, the prevalence of diabetes and prediabetes is slighter higher (though not significant) in females than in males as opposed to other studies globally which show a higher prevalence among males as compared to females [19, 21, 22]. Our results are corroborated by higher prevalence of overweight and obesity found among females than males in the survey [8]. Our results show that one third of the population with DM are under the age of 50. Based on these results, DM did increase with age although it is not limited to older subjects. This adds to the growing body of evidence suggesting that diabetes is also evolving among the younger population as well [18, 19, 23].
Different studies showed that both or either overall obesity or central obesity was associated with conferring risk of diabetes [18, 19]. This study found that an abnormal waist-hip ratio was independently associated with diabetes which is similar to the results in most of the other studies [24–26]. Literature has already shown the protective effects of physical activity against obesity [27]. It is well known that family history of DM is a strong, independent predictor of the disease which was confirmed in our study and supported by most other studies which can be used as a public health tool [28, 29]. Hypertriglyceridemia, but not family history of total cholesterol, was significantly associated with diabetes. Constant increments in serum triglyceride levels were found to be an independent risk factor for diabetes mellitus as well as associated with increased risk for CVD [30, 31]. The study results indicate that elderly individuals, hypertensive, or those with a family history of DM comprise an notable group for screening [5, 24, 27].
The ratio of newly diagnosed to total patients with DM (17%) was found to be considerably lower as compared to the 2008 national survey [15]. This proportion comes down to 13% for Omanis and could be attributed to the national non-communicable diseases screening program for those aged 40 years and above. The DM cases with controlled glucose level have also shown a slight reduction from 2008 (17% in 2008 vs 14% in 2017). However, most concerning is the bulk of uncontrolled cases which accounts for over two-thirds of the cases with raised blood glucose, out of which around 56% are not taking any medication to control their blood glucose level although they have been diagnosed with DM. It is this pool of cases of DM left uncontrolled which would become more prone to complications, and ultimately put a higher financial strain on the country. When assessing only the Omani national population who are served by free primary healthcare, about half of those taking medication were shown to have a controlled blood glucose status. This reveals that only 17% of the individuals who were picked by the health system had a controlled blood glucose status, which is an alarming figure. Challenges of health promotion as part of Oman’s Health Vision 2050 have to be tackled to address unsafe behaviours and subsequently health-related interventions [32]. It is of paramount importance that further research looks into understanding the underlying issues to be able to address them at the root level [33].
Study limitations
Firstly, due to the nature of the study design being cross-sectional, any casual inferences should be interpreted with caution. Secondly, blood glucose measurement was done by a spot analyser rather than venous blood glucose estimation due to logistical constraints. However, regular quality control checks on blood glucose measurement was done as per the manufacturer’s instructions. Thirdly, only fasting blood glucose level was used to measure for diabetes and prediabetes rather than the more sensitive oral glucose tolerance test (OGTT) or the HbA1c test due to financial and logistical constraints of a large-scale household community survey.
Conclusion
In conclusion, the current study provides reliable evidence regarding the high burden of DM among the adult population in Oman. With around 28% of the general population having either diabetes or prediabetes, urgent attention is needed to address this significant burden on the health system. The newly diagnosed cases of DM in the community should not be neglected and also be offered early treatment in order to avoid complications. The reasons for uncontrolled DM in Oman warrant further research and innovative strategies to address this population. Prevention of DM should have a high priority in public health development plans in Oman to prevent associated rising economic costs.
Acknowledgements
The authors acknowledge the support provided by the Director General of Planning and Studies, Ministry of Health, Oman, the WHO country office & WHO EMRO office for their contributions, and the data collectors for the execution of the survey.
Abbreviations
- DM
Diabetes mellitus
- USD
United States Dollars
- GCC
Gulf Cooperation Council
- WHO
World Health Organization
- MENA
Middle Eastern and North African
- BMI
Body Mass Index
- GPAQ
Global Physical Activity Questionnaire
- STROBE
Strengthening the Reporting of Observational Studies in Epidemiology
- EMR
Eastern Mediterranean Region
- NCD
Non-communicable Diseases
Authors’ contributions
AAM, AAH, MM, WAS, ADP, HAK, AAH, ZAB, JI contributed substantially to the acquisition. AAH & MM performed the data analysis. AAM, AAH, SKJ, ADP contributed to interpretation of data, drafted the work and substantively revised it. All authors have read and approved the final manuscript.
Funding
Special thanks to our funding agencies Omantel, Petroleum Development Oman (PDO), OQ, and SSW Group of companies who supported this national level survey. The funding bodies had no role in the design of the study and collection, analysis, interpretation of data, and writing the manuscript.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to data sharing policies but are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study protocol was approved by the Central Research and Ethical Review & Approval Committee of the Ministry of Health, Sultanate of Oman (Approval No: 26/2015). Written informed consent was obtained from the participants for participation in this study separately during health history collection and measurement of bio-physiologic parameters.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.International Diabetes Federation . IDF Diabetes Atlas. 2019. [Google Scholar]
- 2.Al Slamah T, Nicholl BI, Alslail FY, Melville CA. Self-management of type 2 diabetes in gulf cooperation council countries: a systematic review. PLoS One. 2017;12(12):e0189160. doi: 10.1371/journal.pone.0189160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morgan SA, Ali MM, Channon AA, Al-Sabahi S, Al Suwaidi H, Osman N, et al. Prevalence and correlates of diabetes and its comorbidities in four gulf cooperation council countries: evidence from the world health survey plus. J Epidemiol Community Health. 2019;73(7):630–636. doi: 10.1136/jech-2018-211187. [DOI] [PubMed] [Google Scholar]
- 4.Institute for Health Metrics and Evaluation . Oman. Global Burden of Disease Study 2017 (GBD 2017). 2018. [Google Scholar]
- 5.Al-Lawati JA, Panduranga P, Al-Shaikh HA, Morsi M, Mohsin N, Khandekar RB, et al. Epidemiology of diabetes mellitus in Oman results from two decades of research. Sultan Qaboos Univ Med J. 2015;15(2):e226–e233. [PMC free article] [PubMed] [Google Scholar]
- 6.Asfour MG, Samantray SK, Dua A, King H. Diabetes mellitus in the Sultanate of Oman. Diabet Med. 1991;8(1):76–80. doi: 10.1111/j.1464-5491.1991.tb01520.x. [DOI] [PubMed] [Google Scholar]
- 7.Majeed A, El-Sayed AA, Khoja T, Alshamsan R, Millett C, Rawaf S. Diabetes in the middle-east and North Africa: an update. Diabetes Res Clin Pract. 2014;103(2):218–222. doi: 10.1016/j.diabres.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 8.Al-Mawali A, Jayapal SK, Morsi M, Al-Shekaili W, Pinto AD, Al-Kharusi H, et al. Prevalence of Risk Factors of Non-Communicable Diseases in the Sultanate of Oman: STEPS Survey 2017. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.NCDs | The STEPS Instrument and Support Materials. [cited 2020 May 12]. Available from: https://www.who.int/ncds/surveillance/steps/instrument/en/.
- 10.Hypertension. [cited 2020 May 12]. Available from: https://www.who.int/health-topics/hypertension/#tab=tab_1.
- 11.WHO | The guideline development group for the diagnosis and pharmacological treatment of hypertension in adults. WHO. 2020. Available from: https://www.who.int/cardiovascular_diseases/guidelines/hypertension/en/
- 12.Global Physical activity Questionaire Analysis. World Health Organisations. [cited 2020 May 12]. Available from: https://www.who.int/ncds/surveillance/steps/resources/GPAQ_Analysis_Guide.pdf.
- 13.Global Physical Activity Questionnaire Analysis Guide GPAQ Analysis Guide Global Physical Activity Questionnaire (GPAQ) Analysis Guide.[cited 2020 May 12] Available from: https://www.who.int/ncds/surveillance/steps/resources/GPAQ_Analysis_Guide.pdf.
- 14.STROBE Statement. STROBE group. 2014 [cited 2020 May 12]. Available from: https://www.strobe-statement.org/index.php?id=strobe-home
- 15.Morsi M, Elaty A, Attia M, Al RA. Oman world health survey: part 1 methodology, sociodemographic profile and epidemiology of non-communicable diseases in Oman. Oman Med J. 2012;100(330):1–19. [PMC free article] [PubMed] [Google Scholar]
- 16.Tripathy JP, Thakur JS, Jeet G, Chawla S, Jain S, Pal A, et al. Prevalence and risk factors of diabetes in a large community-based study in North India: results from a STEPS survey in Punjab, India. Diabetol Metab Syndr. 2017;9(1):1–8. doi: 10.1186/s13098-017-0207-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization. Noncommunicable diseases and their risk factors. STEPS Country Reports. [cited 2020 Jul 1]. Available from: who.int/ncds/surveillance/steps/reports/en.
- 18.Akter S, Rahman MM, Abe SK, Sultana P. Prevalence of diabetes and prediabetes and their risk factors among Bangladeshi adults: a nationwide survey. Bull World Health Organ. 2014;92:204–213A. doi: 10.2471/BLT.13.128371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pham NM, Eggleston K. Prevalence and determinants of diabetes and prediabetes among Vietnamese adults. Diabetes Res Clin Pract. 2016;113:116–124. doi: 10.1016/j.diabres.2015.12.009. [DOI] [PubMed] [Google Scholar]
- 20.Peters SA, Woodward M. Sex differences in the burden and complications of diabetes. Curr Diab Rep. 2018;18(6):33. doi: 10.1007/s11892-018-1005-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Msyamboza KP, Mvula CJ, Kathyola D. Prevalence and correlates of diabetes mellitus in Malawi: population-based national NCD STEPS survey. BMC Endocr Disord. 2014;14(1):41. doi: 10.1186/1472-6823-14-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gaio V, Antunes L, Namorado S, Barreto M, Gil A, Kyslaya I, et al. Prevalence of overweight and obesity in Portugal: results from the first Portuguese health examination survey (INSEF 2015) Obes Res Clin Pract. 2018;12(1):40–50. doi: 10.1016/j.orcp.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 23.Hilawe EH, Chiang C, Yatsuya H, Wang C, Ikerdeu E, Honjo K, et al. Prevalence and predictors of prediabetes and diabetes among adults in Palau: population-based national STEPS survey. Nagoya J Med Sci. 2016;78(4):475. doi: 10.18999/nagjms.78.4.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al-Lawati JA, Jousilahti PJ. Prevalence and 10-year secular trend of obesity in Oman. Saudi Med J. 2004;25(3):346–351. [PubMed] [Google Scholar]
- 25.Al-Riyami AA, Afifi MM. Prevalence and correlates of obesity and central obesity among Omani adults. Saudi Med J. 2003;24(6):641–646. [PubMed] [Google Scholar]
- 26.Balhareth A, Meertens R, Kremers S, Sleddens E. Overweight and obesity among adults in the Gulf States: A systematic literature review of correlates of weight, weight-related behaviours, and interventions. Obesity Rev. Blackwell Publishing Ltd. 2019;20:763–793. doi: 10.1111/obr.12826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mabry R, Owen N, Eakin E. A National Strategy for promoting physical activity in Oman: a call for action. Sultan Qaboos Univ Med J. 2014;14(2):e170–e175. [PMC free article] [PubMed] [Google Scholar]
- 28.Hariri S, Yoon PW, Qureshi N, Valdez R, Scheuner MT, Khoury MJ. Family history of type 2 diabetes: a population-based screening tool for prevention? Genet Med. 2006;8(2):102–108. doi: 10.1097/01.gim.0000200949.52795.df. [DOI] [PubMed] [Google Scholar]
- 29.Consortium I. Others. The link between family history and risk of type 2 diabetes is not explained by anthropometric, lifestyle or genetic risk factors: the EPIC-InterAct study. Diabetologia. 2013;56(1):60–69. doi: 10.1007/s00125-012-2715-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ye X, Kong W, Zafar MI, Chen L-L. Serum triglycerides as a risk factor for cardiovascular diseases in type 2 diabetes mellitus: a systematic review and meta-analysis of prospective studies. Cardiovasc Diabetol. 2019;18(1):1–10. doi: 10.1186/s12933-019-0851-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beshara A, Cohen E, Goldberg E, Lilos P, Garty M, Krause I. Triglyceride levels and risk of type 2 diabetes mellitus: a longitudinal large study. J Investig Med. 2016;64(2):383–387. doi: 10.1136/jim-2015-000025. [DOI] [PubMed] [Google Scholar]
- 32.Al Hinai H, Al Mufarji K, Al Siyabi H, Al Anqoudi Z, Al Saadi R, Al Awaidy S. Health promotion strategy as part of Vision 2050 in Oman: the way forward. Global Health Promotion. 2020;27(4):145–9. 10.1177/1757975920909115. [DOI] [PubMed]
- 33.Al Mawali AHN, Al Qasmi AM, Al Sabahi SMS, Idikula J, Abd Elaty MA, Morsi M, et al. Oman vision 2050 for health research: a strategic plan for the future based on the past and present experience. Oman Med J. 2017;32(2):86. doi: 10.5001/omj.2017.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due to data sharing policies but are available from the corresponding author on reasonable request.