Abstract
In England patients aged 65 years and over experience a delay of more than 4 months between onset of symptoms and diagnosis of pulmonary TB. This report examines three cases of patients experiencing significant delays in both diagnosis and treatment. Each case had a background of bronchiectasis. Symptoms were initially believed to be secondary to their pre-existing lung disease. Immunosenescence, atypical presentation and pre-existing lung disease mean there is often a significant delay in diagnosis in this population at both a primary care and specialist level.
Keywords: tuberculosis, TB and other respiratory infections, global health, long term care
Background
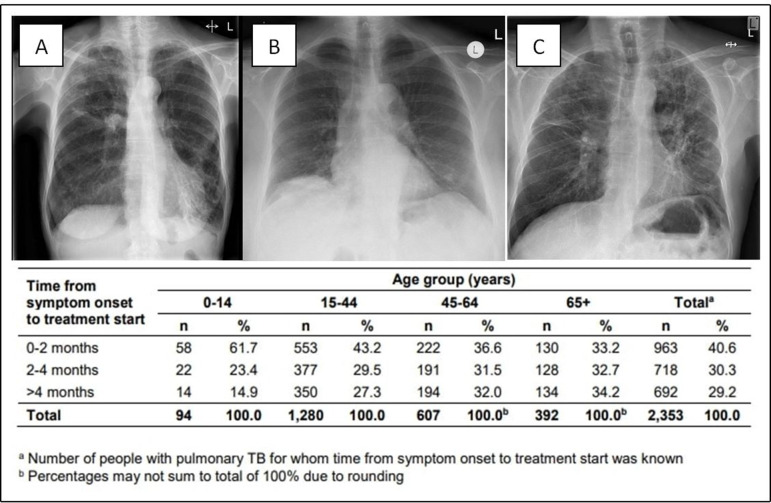
In the report ‘Tuberculosis in England 2019’, data from 2018 showed that 38.69% of patients aged 65 years and over experienced delays of more than 4 months between onset of symptoms and diagnosis (figure 1).1 In this report, we will discuss three patients from the London area who on average experienced a 6-month delay. They each had a background of bronchiectasis. These delays should be seen in the context of an increasingly older population in a city and indeed a nation which has one of the highest rates of pulmonary tuberculosis (pTB) in Western Europe.2 The international community uses the expression ‘underserved community’1 2 to describe individuals who, at each stage of their pTB management, from diagnosis to treatment, suffer a disadvantage due to social circumstances. This expression currently does not refer to the older generation who are often overlooked and undertreated. The medical community also expects to see increased cases of latent TB reactivation in the elderly population given the degree of exposure this population had in their younger years. Older patients with pTB are harder to identify, at increased risk if institutionalised and have a higher burden of comorbidities. Together these factors make older patients with pTB extremely vulnerable.1–5 Patients with bronchiectasis have some of the key symptoms of active pTB as part of their usual disease burden. For the purposes of this case series, we have identified the start of active pTB symptoms as the worsening of their usual symptoms despite courses of standard antibiotics or the addition of extra symptoms. We have taken data directly from patient records and compared it with the data recorded by the London TB Register (LTBR).
Figure 1.
Pretreatment chest radiograph from Mrs A (A), Mrs B (B) and Mr C (C), and 2018 data from Public Health England: time of symptom onset to treatment start by age.1 TB, tuberculosis.
Case presentation
Case 1 Mrs A: symptoms: 14 April 2017; diagnosis: 30 November 2017
Mrs A was diagnosed at the age of 82 years. She was born in Hastings in the south of England. Her mother died of TB when she was 7 years old. She has a history of hypertension and hypercholesterolaemia and was being treated as an outpatient in a respiratory clinic in London for a longstanding history of left lower lobe bronchiectasis. On review in clinic in October 2016, Mrs A reported well-controlled symptoms and good concordance with prophylactic azithromycin. Shortly after her clinic review, she was admitted to Charing Cross Hospital with pneumonia which was successfully treated with doxycycline. She then reported recurrent chest infections from April 2017 onwards despite azithromycin, with symptoms of increasing productive cough and shortness of breath. Mrs A also described significant weight loss which she had linked to a recent period of bereavement. In November 2017, a sputum sample was sent for mycobacterial culture and she was diagnosed with smear positive pTB confirmed on PCR on 30 November 2017. Subsequent drug susceptibility testing identified resistance to izoniazid and she was admitted for initial TB treatment given her severe symptoms and frailty at the time of diagnosis. On review of her imaging (figure 1), it was noted that the right apical changes had been present on images from her admission in October along with the longstanding bronchiectasis and emphysematous changes noted in the left lower lobe. She started treatment as an inpatient and completed therapy in October 2018. Of note, Mrs A is a lifelong non-smoker, she had no significant travel history and lived at home alone following the loss of her husband. According to the LTBR, this woman had a delay of 230 days between worsening of her symptoms in April 2017 and initiation of appropriate treatment at the end of November.
Case 2 Mrs B: symptoms: 20 January 2017; diagnosis: 18 July 2017
Mrs B was diagnosed at the age of 70 years. She was born in France but has been a UK resident since 1967. She has a history of whooping cough as a child, hypertension and gout. She was originally investigated by her general practitioner (GP) in January 2017 for an ongoing cough productive of brown-coloured sputum and lethargy. Chest X-ray (CXR) at the time showed bilateral multilobar pneumonia for which she had multiple courses of antibiotics and several X-rays in February and March. Mrs B was subsequently reviewed in the respiratory clinic in May when it was noted that sputum cultures had thus far been negative (but not tested for acid-fast bacillus). CXR in July prior to diagnosis (figure 1) showed resolution of the early infective changes outlined above with only persistent right lower lobe atelectasis and a left lower lobe nodule. A non-contrast CT of the chest showed right upper lobe consolidation and bronchiectasis, and a bronchoscopy was performed suspecting non-tuberculous mycobacterial infection. After this, Mrs B noted drenching night sweats and a general deterioration in symptoms. She was admitted on 17 July 2017 to hospital, with smear and culture positive on bronchoalveolar lavage. Mrs B is a lifelong non-smoker with no recent significant travel or TB contacts and no other risk factors. HIV and hepatitis serology were both negative. Culture confirmed full sensitivity and she completed treatment in February 2018. This patient had a delay between reporting her first symptoms and diagnosis of 179 days.
Case 3 Mr C: symptoms: 30 August 2017; diagnosis: 30 December 2017
Mr C was aged 65 years at the time of diagnosis in December 2017. He is originally from Tanzania but has been a UK resident since 1962. His medical background is unremarkable, he has a 20 cigarette pack-year history but stopped over 25 years ago. He was referred by the GP with increasing breathlessness, episodes of haemoptysis and recurrent episodes of productive cough requiring multiple courses of antibiotics between January 2017 and review in clinic in December 2017. A CXR in October showed marked interstitial shadowing in the left and right upper lobe in keeping with bronchiectasis (figure 1). A preclinic CT scan in November confirmed marked cylindrical bronchiectasis in the left upper lobe with associated fibrosis. Following review in clinic, sputum was sent and confirmed a smear positive sample and later was culture positive for fully sensitive TB. He was HIV and hepatitis negative and had no other risk factors. According to the LTBR, Mr C had a delay between symptom presentation and diagnosis of 122 days.
Outcome and follow-up
All three patients were followed up by the local TB service throughout the course of their treatment. Each patient successfully completed their therapy without complication. They continue to be followed up by the respiratory services who continue to manage their underlying bronchiectasis.
Discussion
Despite Mrs B and Mr C not being born in the UK, all three patients had no significant recent travel history, had been in the country from birth or for the last 50 years, and had no local TB contacts. None had risk factors such as homelessness, drug abuse, immunosuppression or recent institutionalisation. Apart from a brief history of depression in one patient, none of them suffered significant mental health issues. Two of the three were lifelong non-smokers and there was no history of occupational exposures. All three were smear positive and highly infectious, and had significant symptoms of weight loss, haemoptysis and productive cough at the time of diagnosis. Mrs A and Mrs B were admitted to hospital for the start of treatment due to the severity of their symptoms secondary to delays in diagnosis. Principally, all three patients had a history of bronchiectasis which presented with recurrent chest infections and weight loss over the preceding months. They also all had significant radiological abnormalities seen early on CXR or cross-sectional imaging. What is striking about these cases is that because of the perceived likelihood that these symptoms were due to bronchiectasis, there was extensive delay between the start of worsening of their usual symptoms and diagnosis. Mrs B also had a relatively normal CXR immediately before diagnosis which may have delayed diagnosis. TB was not uncommon in the earlier part of the previous century meaning that older people today may have been exposed to a significant extent in earlier life and may have had latent TB for many years.1 2 While we believe TB reactivation is most common within 2 years of initial exposure, there is a reducing but significant risk of reactivation that persists over a lifetime.1 Immunosenescence means the elderly are at risk of reactivation presenting with typical or atypical findings.4 A retrospective cohort review from Abbara et al concluded that patients 65 years and over were less likely to present with the ‘classic’ clinical or radiological features of active pTB and therefore were more likely to have delays between symptoms and diagnosis.5 Internationally the average age at diagnosis with TB is rising, for example, in Hong Kong where reactivation of TB in senior populations is thought to be largely responsible for halting the earlier decline in TB incidence.4 These three cases indicate the way that the index of suspicion at both primary care and specialist level can be obscured in elderly people with and without comorbid lung disease. A failure to suspect and diagnose pTB in old age risks allowing progression to more advanced disease in a vulnerable population, in addition to the ongoing transmission of disease potentially in their peer group.
Learning points.
This report reflects the value of considering a diagnosis of pulmonary tuberculosis (pTB) in symptomatic patients within this vulnerable patient group both with and without radiological changes.
Immunosenescence should be considered a separate risk factor when considering the investigation of this age group for pTB.
Reactivation of latent TB in the elderly population will become an increasing issue internationally as older age groups, exposed in childhood and with pre-existing lung disease, become unwell with active TB. It is in this vulnerable group were prompt diagnosis and treatment will be most important.
Footnotes
Contributors: CRM compiled the case reports and discussion with GKR and OMK, advising on direction of the discussion, overall review and the identification cases for the report. All three named authors contributed to the response following initial review of the case report.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Public Health England . Tuberculosis in England, 2019. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/821335/Tuberculosis_in_England_executive_summary_2019 [Accessed 1 Jul 2020].
- 2.Public Health England . Collaborative tuberculosis strategy for England 2015-2020. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/403231/Collaborative_TB_Strategy_for_England_2015_2020_.pdf [Accessed 1 Jul 2020].
- 3.Byng-Maddick R, Noursadeghi M. Does tuberculosis threaten our ageing populations? BMC Infect Dis 2016;16:1–5. 10.1186/s12879-016-1451-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tam G, Yang H, Meyers T. Mixed methods study on elimination of tuberculosis in Hong Kong. Hong Kong Med J 2018;24:400–7. 10.12809/hkmj177141 [DOI] [PubMed] [Google Scholar]
- 5.Abbara A, Collin SM, Kon OM, et al. Time to diagnosis of tuberculosis is greater in older patients: a retrospective cohort review. ERJ Open Res 2019;5:00228-2018. 10.1183/23120541.00228-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]